Abstract
Introduction
The combination of posterior elbow dislocation, radial head fracture, and coronoid fracture has been named “terrible triad” as this injury is difficult to treat and yield poor outcomes. Some studies compared the results of radial head fixation to replacement in isolated radial head fractures, very few reports have tried to compare both treatment modalities in the setting of a terrible triad injury.
The aim of this study was to compare the functional outcome of radial head fixation vs replacement in terrible triad injuries of the elbow.
Methods
A single-center, prospective cohort study was conducted at an academic Level 1 Trauma Center from April 2016 to April 2019.
A total of 30 patients with terrible triad injury of the elbow were enrolled. The primary outcome was the Quick Disability of Arm, Shoulder and Hand (Quick-DASH) at 1 year. The secondary outcomes were to report the Mayo Elbow Performance Score (MEPS) at 1 year and elbow range of motion.
Results
At final follow up for each patient (13.4 ± 1.2 months) The Quick-DASH score at 1 year for fixation group was 5 ± 2.3, for the replacement group it was 7.1 ± 7.1. The MEPS at 1 year for fixation group was 93.6 ± 8.4, for the replacement group it was 90.9 ± 9.4.
Loss of elbow extension at 1 year for fixation group was 17.1° ± 10.7°, for replacement group it was 18.75° ± 11.5°.
Conclusion
A systematic approach to address the bony and soft tissue components of terrible triad elbow injury is crucial to obtain satisfactory outcome. Our study shows that radial head repair and replacement, in the setting of terrible triad injury, yields comparable results.
Level of evidence
Level II, Therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combination of posterior elbow dislocation, radial head fracture, and coronoid fracture has been named “terrible triad” as this injury is difficult to treat and yield poor outcomes [1]. In this uncommon injury, there is loss of the anterior buttress of the coronoid, the valgus buttress of the radial head, and the posterolateral stabilization of the lateral ulnar collateral ligament (LUCL) which results in elbow instability [2].
High rates of complications (e.g., contractures, instability, and pain) has been reported by historical studies [3,4,5]. However, the improved understanding of elbow constraints, as well as the improvements in fixation options; lead to significant improvements in the treatment of this injury. The adoption of algorithmic approach and standardized surgical protocols by recent studies [6,7,8,9] in treating this difficult injury resulted in improved patient outcomes. While some studies compared the results of radial head fixation to replacement in isolated radial head fractures [10], very few reports have tried to compare both treatment modalities in the setting of a terrible triad injury.
The aim of this study was to compare the functional outcome of radial head fixation vs replacement in terrible triad injuries of the elbow. The primary outcome was to report the Quick Disability of Arm, Shoulder and Hand (Quick-DASH) at 1 year. The secondary outcomes were to report the Mayo Elbow Performance Score (MEPS), elbow flexion/extension arc and complications (e.g., infection, heterotrophic ossification).
Our null hypothesis was that functional results are the same for fixation vs replacement of radial head fractures in treating terrible triad injury of the elbow.
Methods
Study Design
An Institutional Review Board (IRB) approved, single-center, prospective follow-up study.
Setting
An academic Level 1 Trauma Center. The study was conducted from April 2016–April 2019 (patient enrollment continued for 2 years, then study was terminated when a minimum of 12 months follow-up was achieved for all patients).
Participants
All patients above 18 years who presented to our service with elbow dislocation were registered and assessed for eligibility, patients with terrible triad injury were eligible for enrollment.
Radiographic evaluation included plain radiographs as well as CT scan of the elbow to assess fractures pattern and articular surfaces involvement.
Exclusion criteria for enrollment in the study were as follows: pure elbow dislocation without associated elbow fractures; open dislocation/fracture; patients with compartment syndrome; concomitant injury (e.g., multiple fractures); patients with concomitant upper extremity injury (e.g., humerus fracture) and fractures older than 14 days.
Data on age, gender, mode of trauma, fracture type (for radial head and coronoid), and complications (e.g., stiffness, infection) were registered.
Radial head fractures were graded according to Mason classification [11], coronoid fractures were graded according to Regan–Morrey classification [12].
Intervention
Elbow dislocation was reduced closed in the emergency department under conscious sedation or in the operating room under general anesthesia. Then the limb was supported in a posterior splint awaiting definitive surgery.
Our institution uses the widely accepted algorithmic approach to guide surgical intervention of terrible triad injury [8, 9].
The decision of operative management was taken by the senior investigator (SG).
We adopted the operative technique described by Pugh [8].
Patients were put in the supine position with a tourniquet on the proximal arm. The arm was placed over a hand table to allow easy access to the C-arm. A lateral incision was used in all patients and deep structures were approached through the Kocher interval. A typical finding was disruption of the lateral collateral ligament (LCL) complex from the lateral epicondyle.
Surgical repair and stabilization were carried out from deep to superficial. All coronoid fractures were fixed (using non-absorbable suture lasso, passed through drill holes and tied over the dorsum of the olecranon). A decision of radial head fixation (using headless screws and/or small proximal radial plate) was made when there were ≤ 3 articular fragments, with no traumatic delamination of the articular cartilage and no comminution of the radial neck. If these criteria were not met, the radial head was replaced (using a modular prosthesis). There was no radial head excision without replacement. With radial head replacement, aggregation of the excised head fragments was done to select the implant head size (with a preference to slight under-sizing). Neck length was determined by ensuring that the implanted head was flush with the proximal edge of the lesser sigmoid notch when the joint is reduced as well as ensuring there was no gapping in the medial ulno-humeral joint.
Finally, the LCL complex was repaired back to the isometric point at the lateral epicondyle, using either non-absorbable sutures passed through drill holes in the epicondyle if bone quality was good, or using suture anchors if bone quality was poor.
Stability of the elbow was tested intra-operatively using the hanging arm test [13], which was performed before and after the LCL was addressed.
All surgeries were performed by the same surgeon (AL), who is fellowship trained in hand surgery.
Postoperative regimen included the use of an arm sling for arm support in the early postoperative period (held in 70° flexion and slight pronation to protect LCL repair), that was converted to a hinged elbow brace 1 week after surgery and physical therapy was initiated to recover elbow range.
Outcomes
Patients were followed at 2 weeks, 6 weeks, 3 months, and 1 year for radiological and functional evaluations.
The Quick-DASH score [14, 15] at 1 year was selected as the primary outcome measure, it was also collected at inclusion (recall baseline function).
Secondary outcome measures were MEPS [16, 17] at 1 year, elbow flexion/extension arc and complications (e.g., infection, heterotrophic ossification).
Statistics
The statistical analysis was performed using the statistical package SPSS (Statistical Package for the Social Sciences) version 25.
Mean and standard deviation (SD) were used to express continuous data while frequency (count) and relative frequency (percentage) were used to express categorical data.
Continuous variables were age, functional score, length of follow-up period, and elbow range of motion. Categorical variables were sex, side of injury, fracture pattern, and complications.
The statistical difference was calculated using Student’s t test for continuous variables which followed a normal distribution and Mann–Whitney U test for those not following a normal distribution. For comparing categorical data, Chi-squared (χ2) test was performed, Fisher’s exact test was used instead when the expected frequency was less than 5.
P values less than 0.05 were considered as statistically significant.
Ethics
No funding was received for this study. Authors declare that they have no conflict of interest. The study was conducted in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration. Informed consent was obtained from all patients who participated in the study.
Results
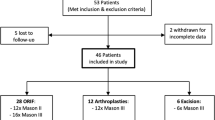
A total of 67 patients were assessed for eligibility, 32 patients were excluded as they did not meet the inclusion criteria, five patients refused to participate in the study, so a final number of 30 patients were enrolled. No patients were lost to follow up at time of final data analysis.
The study included 17 males (56.7%) and 13 females (43.3%), the mean age at time of enrollment was 40.4 ± 14.9 years. The mean follow-up period was 13.4 ± 1.2 months.
Dominant side was affected in 11 patients (36.7%), non-dominant side was affected in 19 patients (63.3%).
The mode of injury was falling to the ground (FTG) in 22 patients (73.3%), road traffic accident (RTA) in eight patients (26.7%).
Radial head fracture type (according to Mason classification) was type I in one patient, type II in 15 patients and type III in 13 patients. One patient has radial neck fracture.
Coronoid fractures type (according to Regan–Morrey classification) was type I in 10 patients and type II in 20 patients.
Fixation of radial head fractures was done in 14 patients and replacement was done for 16 patients.
The Quick-DASH score at 1 year for fixation group was 5 ± 2.3, for the replacement group it was 7.1 ± 7.1. The difference was not found to be statistically significant.
The MEPS at 1 year for fixation group was 93.6 ± 8.4, for the replacement group it was 90.9 ± 9.4. The difference was not found to be statistically significant.
Loss of elbow extension at 1 year for fixation group was 17.1° ± 10.7°, for replacement group it was 18.75° ± 11.5°. The difference was not found to be statistically significant.
Table 1 shows functional results for both groups.
The classification of radial head fractures was found to have no impact on the functional outcome (Table 2).
Three patients required secondary procedures; one patient developed significant pain over the lateral aspect of the elbow due to capitellar erosion by radial head prosthesis. Removal of prosthesis was done after 6 months. Pain was relieved. At final follow up, flexion degree was 145°, extension loss was 20°, pronation was 80° and supination was 60°, MEPS was 95 and Quick-DASH was 2.3. Another patient (who had radial head fixation) developed deep wound infection, which resolved after debridement without the need for any hardware removal. Another patient developed heterotopic ossification for which surgical excision was done after 6 months when maturation of ossification was confirmed on radiographs, that was followed by 3 weeks course of Indomethacin to prevent recurrence; at final follow-up, flexion degree was 120°, extension loss was 10°, pronation–supination arc was 165°, MEPS was excellent and Quick-DASH score was 4.5. A clincial example of radial head fixation case is shown in Fig. 1, a clinical example of radial head replacment case is shown in Fig. 2.
Discussion
The stability of the elbow joint is provided by a complex interaction between the articular surfaces and soft tissue stabilizers, making it a very congruous joint. When elbow dislocation is associated with articular surface disruption surgical treatment is usually mandated for recurrent instability, and the risk of subsequent arthrosis increases substantially [18,19,20,21].
As the understanding of the functional anatomy of the elbow and how this influences its stability, the outcome of surgical management of terrible triad injuries became more predictable as shown by recently published literature [7, 21, 22].
In a review article [23], the results of 137 terrible triad injuries in five studies were analyzed. Treatment included coronoid fixation, repair or replacement of radial head, and repair of LCL complex, reserving MCL repair and hinged external fixation for residual instability. That treatment strategy appeared effective in the majority of cases. Mean follow-up was 31 months. Overall flexion–extension arc was 111.4° and the average MEPS was 85.6 points.
In another review article [24] of 21 studies on terrible triad injuries of the elbow, it was found that the prosthetic replacement was the most common method for treating radial head fractures, trans-osseous suture was the most common method for coronoid fixation, and repair of the LCL complex was always done. The mean age was 45.9 years (range 13–79 years). Mason type III was the most common, Morrey type II was the most common. Those with radial head fixation had an average elbow flexion/extension arc of 115.5° ± 19.7°, had an average MEPS of 86.1 ± 12.9; while those with radial head replacement had an average elbow flexion/extension arc of 116.6° ± 25.3° and an average MEPI score of 85.8 ± 13.8. Those in which the coronoid process was fixed using trans-osseous sutures had the highest functional score (MEPS of 91.5 ± 9.1) compared to those in which the coronoid was fixed using suture anchors (MEPS of 73.3 ± 29.1).
From our data and other collected data, the most common approach to radial head management was by prosthetic replacement followed by ORIF (we think that was driven by the nature of the fracture pattern) with no role for excision alone. Functional results of prosthesis were comparable with that of fixation. In our study, trans-osseous sutures for coronoid repair were the standard managed as this method was found to yield the best functional outcomes. The LCL had been routinely repaired throughout our study as a necessary step. We did not perform MCL repair in our series as all elbows in our study became stable after reconstruction of the lateral and central stabilizers. The scientific literature [23, 24] recommend repairing the MCL only when there was persistent instability after repair of other elbow stabilizers.
In a retrospective review [2] that included 39 patients with terrible triad injuries who were managed with repair (n = 9) or replacement (n = 30) of the radial head, repair of the LUCL, and repair of the coronoid fracture. The mean elbow flexion/extension arc was 115° (75°–140°). The mean DASH score was 16 (0–34).
Another retrospective study [25] reviewed the difference between radial head replacement vs fixation. They included 23 patients with terrible triad injury and found comparable functional results between the two groups with only higher rate of re-operation in the fixation group.
In light of the previously mentioned literature, the authors wanted to compare radial head fixation vs replacement in treating terrible triad injuries of the elbow, as the only available literature on that matter was only retrospective studies.
Our results were not different than those shown in similar retrospective studies [2, 25].
One of the limitations to this study is that to generalize the results, longer follow up would be needed to evaluate the long-term effect of prosthesis and its longevity.
In conclusion, the authors believe that using a systematic approach to address the bony and soft tissue components of this difficult injury pattern is crucial to obtain satisfactory outcome. Satisfactory outcome is usually achieved in most patients following that systematic approach, and MCL repair or the application of a hinged external fixator is seldomly required. Our study shows that radial head repair yields comparable results to replacement in the setting of terrible triad injury.
References
Hotchkiss, R. N. (1996). Fractures and dislocations of the elbow. In C. A. Rockwood, D. P. Green, R. W. Bucholz, & J. D. Heckman (Eds.), Rockwood and green’s fractures in adults (4th ed., pp. 980–981). Philadelphia: Lippincott-Raven.
Watters, T. S., Garrigues, G. E., Ring, D., & Ruch, D. S. (2014). Fixation versus replacement of radial head in terrible triad: is there a difference in elbow stability and prognosis? Clinical Orthopaedics and Related Research, 472(7), 2128–2135.
Josefsson, P. O., Gentz, C. F., Johnell, O., & Wendeberg, B. (1989). Dislocations of the elbow and intraarticular fractures. Clinical Orthopaedics and Related Research, 246, 126–130.
Johnston, G. W. (1962). A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Medical Journal, 31, 51–56.
Knirk, J. L., & Jupiter, J. B. (1986). Intra-articular fractures of the distal end of the radius in young adults. Journal of Bone and Joint Surgery: American Volume, 68(5), 647–659.
Egol, K. A., Immerman, I., Paksima, N., Tejwani, N., & Koval, K. J. (2007). Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bulletin of the NYU Hospital for Joint Diseases, 65(4), 263–270.
Forthman, C., Henket, M., & Ring, D. C. (2007). Elbow dislocation with intraarticular fracture: the results of operative treatment without repair of the medial collateral ligament. Journal of Hand Surgery: American Volume, 32(8), 1200–1209.
Pugh, D. M., Wild, L. M., Schemitsch, E. H., King, G. J., & McKee, M. D. (2004). Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. Journal of Bone and Joint Surgery: American Volume, 86(6), 1122–1130.
Zeiders, G. J., & Patel, M. K. (2008). Management of unstable elbows following complex fracture-dislocations—the “terrible triad” injury. Journal of Bone and Joint Surgery: American Volume, 90(4), 75–84.
Ring, D., Quintero, J., & Jupiter, J. B. (2002). Open reduction and internal fixation of fractures of the radial head. Journal of Bone and Joint Surgery: American Volume, 84(10), 1811–1815.
Mason, M. L. (1954). Some observations on fractures of the head of the radius with a review of one hundred cases. British Journal of Surgery, 42(172), 123–132.
Regan, W., & Morrey, B. (1989). Fractures of the coronoid process of the ulna. Journal of Bone and Joint Surgery: American Volume, 71(9), 1348–1354.
Garrigues, G. E., Wray, W. H., 3rd, Lindenhovius, A. L., Ring, D. C., & Ruch, D. S. (2011). Fixation of the coronoid process in elbow fracture-dislocations. Journal of Bone and Joint Surgery: American Volume, 93(20), 1873–1881.
Beaton, D. E., Wright, J. G., & Katz, J. N. (2005). Upper extremity collaborative group: development of the QuickDASH: comparison of three item-reduction approaches. Journal of Bone and Joint Surgery: American Volume, 87(5), 1038–1046.
Gummesson, C., Ward, M. M., & Atroshi, I. (2006). The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskeletal Disorders, 7, 44.
Morrey, B. F., An, K. N., & Chao, E. Y. S. (1993). Functional evaluation of the elbow. In B. F. Morrey (Ed.), The Elbow and Its Disorders (2nd ed., pp. 86–97). Philadelphia: WB Saunders Co.
Cusick, M. C., Bonnaig, N. S., Azar, F. M., Mauck, B. M., Smith, R. A., & Throckmorton, T. W. (2014). Accuracy and reliability of the Mayo elbow performance score. The Journal of Hand Surgery, 39(6), 1146–1150.
Ring, D., Jupiter, J. B., & Zilberfarb, J. (2003). Roles of the medial collateral ligament and the coronoid in elbow stability. Journal of Bone and Joint Surgery: American Volume, 85(3), 568–569.
O’Driscoll, S. W., Jupiter, J. B., King, G. J., Hotchkiss, R. N., & Morrey, B. F. (2001). The unstable elbow. Instructional Course Lectures, 50, 89–102.
O’Driscoll, S. W., Morrey, B. F., Korinek, S., & An, K. N. (1992). Elbow subluxation and dislocation: a spectrum of instability. Clinical Orthopaedics Related Research, 280, 186–197.
Pugh, D. M., & McKee, M. D. (2002). The “terrible triad” of the elbow. Techniques in Hand and Upper Extremity Surgery, 6(1), 21–29.
Mathew, P., Athwal, G. S., & King, G. J. W. (2009). Terrible triad injury of the elbow: current concepts. Journal of American Academy of Orthopaedic Surgeons, 17(3), 137–151.
Rodriguez-Martin, J., Pretell-Mazzini, J., Andres-Esteban, E. M., & Larrainzar-Garijo, R. (2011). Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. International Orthopaedics, 35(6), 851–860.
Ebrahim, N. A., Raberding, C. J., & Liu, J. (2012). A review of terrible triad injury of the elbow. Techniques in Shoulder Elbow Surgery, 13(3), 101–106.
Leigh, W., & Ball, C. (2012). Radial head reconstruction versus replacement in the treatment of terrible triad injuries of the elbow. Journal of Shoulder and Elbow Surgery, 21(10), 1336–1341.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Disclosure
The author, their immediate family, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Ethical standard statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Afifi, A., Lymona, A.M. & Galal, S. Radial Head Fixation vs Replacement in Terrible Triad: Preliminary Results of a Prospective Cohort Study with Patient Reported Outcome. JOIO 54 (Suppl 2), 254–259 (2020). https://doi.org/10.1007/s43465-020-00090-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-020-00090-x