Abstract
Despite new approaches in adjuvant chemotherapy, colorectal cancer metastasis is still a major health concern worldwide. Herbal medications with anti-tumor effects are considered a suitable alternative for the treatment of malignancies. Auraptene, an abundant natural coumarin, exhibits anti-cancer activity against various types of cancer. However, the mechanisms by which auraptene impacts cancer invasion and metastasis remain unknown. The current study aimed to assess a possible inhibitory role of auraptene in colorectal cancer metastasis in a mouse model. The anti-proliferative and anti-migratory effects of auraptene were evaluated by 3–4,5-dimethylthiazol-2-yl-2,5 diphenyltetrazolium bromide (MTT) and cell migration assays, respectively. The quantitative reverse transcription polymerase chain reaction (qRT-PCR) technique was used to determine the gene expression levels of matrix metalloproteinase (MMP)-2, MMP-9, E-cadherin, and vascular endothelial growth factor A (VEGF-A) and its cognate receptor (vascular endothelial growth factor receptor 1, VEGFR1) in tumor samples. Moreover, the western blot analysis was conducted to examine the expression of MMP-2 and MMP-9 proteins. According to the in vitro results, auraptene inhibited the proliferation and migration of CT26 cells. Furthermore, auraptene decreased the rate of metastasis by modulating the expression of MMP-2, MMP-9, E-cadherin, VEGF-A, and VEGFR1 genes. Accordingly, the expression levels of MMP-2 and MMP-9 proteins were significantly reduced. In addition, the pathological analysis revealed a marked degree of necrosis in tumor cells treated with auraptene. Based on our results, auraptene is likely to be a potent therapeutic agent for the treatment of metastatic colorectal cancer and may be a suitable candidate for adjuvant therapy due to its anti-metastatic effects.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is the second leading cause of cancer death and the third most commonly diagnosed cancer worldwide (Sung et al. 2021). Despite the rapid development of chemotherapeutic compounds over the past decade, metastasis is still a serious challenge in the treatment of colorectal cancer (CRC) (Valderrama-Treviño et al. 2017). 5-Fluorouracil (5-FU), which is the gold standard medication for the treatment of CRC, possesses numerous therapeutic effects; however, some obstacles, such as the high recurrence rate, have enhanced the need for alternative therapies (Fong et al. 1999). The rate of cell division is very high in cancer cells and these cells have the ability to escape from cell death (i.e., apoptosis). Metastasis is more likely to occur when the size of the primary tumor grows. Therefore, inhibiting cancer cell proliferation seems to be the critical first step in the progression of metastatic cancer (Weinberg and Weinberg 2013). Moreover, it is now established that a number of proteins are involved in the metastasis and invasion of cancer cells. Matrix metalloproteinases (MMPs) are a group of enzymes that digest the extracellular matrix and are responsible for the metastasis and invasion of cancer cells (Hooper et al. 2002). In addition to their proteolytic functions in physiological processes, MMP-2 and MMP-9 are also highly expressed in CRC, and some studies suggest that these two serum MMPs could be used as biomarkers of CRC invasion (Tutton et al. 2003; Said et al. 2014). It is worth noting that these two MMPs could be applied to predict the recurrence and invasion of CRC (Tutton et al. 2003; Araújo et al. 2015). E-cadherin is another key protein involved in cell-cell adhesion and tissue integrity (Deryugina and Quigley 2006). According to research, MMP-9 is closely related to E-cadherin since MMP-9 can cleave the ectodomain of E-cadherin, allowing cancer cells to migrate to other distant tissues/organs (Symowicz et al. 2007).
Angiogenesis or vascularization is one of the significant stages of cancer metastasis, and it has been shown that targeting this biological process could improve the treatment course of patients with CRC (Lopez et al. 2019). Vascular endothelial growth factor A (VEGF-A) and its cognate receptor (vascular endothelial growth factor receptor 1, VEGFR1) serve a crucial function in the survival of endothelial cells and the regulation of angiogenesis (Bhattacharya et al. 2017). Studies have indicated that VEGF-A is the most critical member of the VEGF family involved in the dissemination of tumor cells (George et al. 2001; Onogawa et al. 2004).
Natural or synthetic products that inhibit the function of these proteins with minimal side effects may be useful in limiting the metastatic spread of CRC. Auraptene (1,7-geranyloxycoumarin, 1) is a monoterpene coumarin found in Rutaceae and Apiaceae families, especially in Citrus species, which is native to South and East Asia (Genovese and Epifano 2011; Kumar et al. 2012). In animal models of various cancers, including gastric, prostate, breast, and liver malignancies, auraptene appears to have numerous therapeutic effects (Derosa et al. 2016). With its antioxidant and chemopreventive properties, auraptene suppresses superoxide formation, reduces lipid peroxidation, and modulates glutathione S-transferase activity in mice (Tanaka et al. 1998). It was shown that the oral administration of auraptene prevented the metastasis of melanoma cells to the lungs and inhibited the growth of the metastatic tumor in mice (Tanaka et al. 2000). Hayashi et al. (2007) reported that auraptene reduced the risk of colon cancer in mice through the suppression of cyclooxygenase-2 (COX-2) and nitric oxide synthase (iNOS) and induced apoptosis in colon epithelial cells.

The present study aimed to examine the inhibitory function of auraptene isolated from Citrus fruits in the proliferation and migration of CT26 cells as well as evaluate the anti-metastatic effects of this compound on the expression levels of MMP-2, MMP-9, E-cadherin, VEGF-A, and VEGFR1. To the best of our knowledge, this is the first report assessing the impacts of auraptene on metastasis in CT26 tumor-bearing mice.
Materials and Methods
Chemicals and Reagents
Auraptene was purchased from Tinab Shimi (purity of 96%; Mashhad, Iran; Lot number: T49500203). Dimethyl sulfoxide (DMSO), penicillin-streptomycin, and trypsin-EDTA were procured from Sigma-Aldrich (St. Louis, MO, USA). Fetal bovine serum (FBS) and RPMI 1640 medium were obtained from Gibco (Grand Island, NY, USA). The total RNA extraction kit was purchased from Yekta Tajhiz Azma (Tehran, Iran). The ExcelRT™ Reverse Transcription Kit II for the synthesis of cDNA was obtained from SMOBIO Technology, Inc. (Taiwan). For western blot analysis, all primary antibodies against MMP-2, MMP-9, and β-actin were acquired from ZellBio GmbH (Germany).
Cell Culture
The CT26 cell line was procured from the National Cell Bank of Iran (the Pasteur Institute, Tehran, Iran). The cells were cultured in RPMI 1640 medium containing 10% heat-inactivated FBS and 1% streptomycin/penicillin at 37 °C in 5% CO2 atmosphere. The cells were passaged utilizing trypsin-EDTA in their exponential phase.
Growth Inhibition Assay
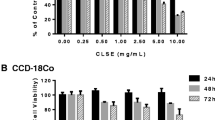
The inhibitory effect of auraptene on cell growth was assessed by the 3–4,5-dimethylthiazol-2-yl-2,5 diphenyltetrazolium bromide (MTT) assay (Mosmann 1983). For this purpose, CT26 cells (10 × 103 cells/well) were incubated overnight. Then, the cells were treated with auraptene (12.5–500 μM) for 48 h. After that, 10 μl of the MTT reagent stock (5 mg/ml) was added to each well. The respective supernatants were removed after 3 h, and 100 μl of DMSO was added to each well to dissolve the formazan crystals. The microplates were shaken gently for 40 min in the dark at room temperature, and the absorbance was measured at 545 and 630 nm (background) using a Stat FAX303 plate reader. The IC50 value was determined using GraphPad Prism software. All treatments were carried out in triplicate.
Cell Migration Assay
The wound healing assay was conducted to determine the effect of auraptene against the migration of CT26 cells according to the method described previously (Khorsand et al. 2022). A total of 2.5 × 105 cells/well were treated with auraptene at a concentration of 200 μM in a 24-well plate. The process of cell migration assay was monitored, and the cells were imaged under a microscope secured with a digital camera (CAMV1200SC, Canada). The imaging procedure was carried out at various time intervals (0, 6, 10, 20, and 24 h). The experiment was performed in triplicate and then repeated three times. In this method, cells were treated with 5-FU as the positive control.
Animal Model of CRC
Female Balb/C mice (6–8 weeks old, n = 50) were purchased from the Razi Institute (Karaj, Iran) and kept under standard laboratory conditions (constant humidity, room temperature of 20–25 °C, and a 12-h light/dark cycle). All animal experiments were performed according to the guidelines provided by the Ethics Committee of Mashhad University of Medical Sciences (IR.MUMS.MEDICAL.REC.1399.744). CT26 colon adenocarcinoma cells (1 × 106) were implanted subcutaneously (s.c.) into the right flank of 18–20-week-old female Balb/c mice (weight range: 19–21 g). The size of the tumor was calculated using the formula 1/2 × length × width2, and when it reached around 85 ± 50 mm3, the animals were randomly divided into five groups (n = 8 per group): (i) the control group (sham control) with intratumoral injection of 100 μl of normal saline and DMSO as an auraptene solvent, (ii) the positive group subjected to the intraperitoneal injection (i.p.) of 5 mg/kg 5-FU, and (iii, iv, v) auraptene groups with intratumoral injection of auraptene at the concentrations of 50, 100, and 200 μM. The injection process was conducted every other day for 14 days. After this time period, the animals were sacrificed, and whole tumors were collected and kept at −80 °C for further analyses (Fig. 1).
Anti-proliferative and anti-migratory effects of auraptene on CT26 cells. A The graph indicates the percentage of the cell-free area at certain time points during the in vitro migration assay. B Representative images from the migration assays of CT26 cells. C Growth suppression after 48 h of treatment with auraptene. Data are expressed as the mean ± SEM of three independent experiments (*p < 0.05)
Quantitative Real-Time Polymerase Chain Reaction (PCR)
According to the manufacturer’s instructions, total RNA was isolated and converted into cDNA using the RNA extraction kit. The expression of all genes was examined by real-time PCR (Table 1). All PCR were performed on Applied Biosystems (ABI) with the following cycling conditions: 95 °C for 15 min followed by 30–40 cycles of 95 °C for 30 s and 55–60 °C for 60 s (Mogharrabi et al. 2020). The relative expression of the genes was normalized against β-actin as an endogenous control. The relative fold change of these mRNAs was determined by the Pfaffl method, as described previously (Pfaffl 2001).
Western Blot
The protein levels of MMP-2 and MMP-9 were assessed using the western blot method according to the study by Mohammadi et al. (2020). Tumor samples were homogenized in ice-cold RIPA buffer, and the bicinchoninic acid method (BCA kit, Pars Tous, Iran) was applied to determine the protein concentration. Electrophoresis was carried out on equal amounts of proteins. The immunoblotting bands were visualized using a Pars Tous chemiluminescence detection kit (Pars Tous Biotechnology, Iran). The relative expression was compared to the β-actin protein expression using ImageJ software (NIH, Bethesda, Rockville, MD, USA).
Histological Analysis
Tumor samples were fixed in freshly prepared 4% formalin. Then, tumor tissues were processed in a graded alcohol series and paraffin-embedded at 56 °C. All tissue blocks were sectioned at a thickness of 5–7 µm and then stained with hematoxylin and eosin (H&E) (Abcam, USA). Finally, samples were evaluated under a light microscope (Cardiff et al. 2014).
Statistical Analysis
Data are expressed as the means and standard error of the mean (mean ± SEM). The differences between the groups were analyzed by one-way analysis of variance (one-way ANOVA), followed by Dunnett’s post hoc test. The migration assay results were statistically compared using repeated measures of ANOVA. A p-value of less than 0.05 was considered statistically significant. The obtained values were statistically analyzed using GraphPad Prism version 8.0. All experiments were performed in triplicate and independently.
Results
Auraptene Inhibited Cell Proliferation and Migration in CT26 Cells
In order to investigate the anti-proliferative effects of auraptene, the MTT assay was carried out. The results revealed that auraptene suppressed cell growth in a dose-dependent manner (Fig. 1C). According to the scratch mobility results, auraptene significantly reduced cell migration into the cell-free area after 24 h compared to the control cells (Fig. 1A, B, p < 0.05).
Auraptene Suppressed Colorectal Xenograft Tumor Growth In Vivo
As shown in Fig. 2B, C, the size of tumors in mice treated with 200 μM auraptene and 5-FU was significantly smaller than that of the control mice (p < 0.05).
Administration of Auraptene Decreased the Expression Levels of MMP-2, MMP-9, E-cadherin, VEGF-A, and VEGFR Genes
The results obtained from the real-time PCR method demonstrated that treatment with 100 and 200 μM auraptene led to the greatest reduction in the expression levels of MMP-2 and VEGF-A genes, by 0.009 and 0.012 times for MMP-2 (p < 0.0001) and 0.8 (p < 0.01) and 0.6 times (p < 0.0001) for VEGF compared with the control group, respectively (Fig. 3A, C). Moreover, the expression levels of MMP-9 and VEGFR genes declined in a dose-dependent manner (Fig. 3B, D). Auraptene at concentrations of 100 and 200 μM elevated the expression level of E-cadherin by 19.5 (p < 0.05) and 115 (p < 0.0001) times in comparison with the control group, respectively (Fig. 3E).
The impact of auraptene on the expression of anti-metastatic and anti-angiogenic genes. The expression rates of A MMP-2, B MMP-9, C VEGF-A, D VEGFR, and E E-cadherin genes; data are represented as the mean ± SEM of three independent experiments. *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001 denote significant differences compared with the control group
Intratumoral Administration of Auraptene Reduced the Protein Expression of MMP-2 and MMP-9
As displayed in Fig. 4A, the protein expression of MMP-2 in the control group was high and visualized as an intense band. Protein bands were also observed in samples treated with 50 μM and 100 μM auraptene, whereas no bands were detected in samples treated with 5-FU or 200 μM auraptene. Consistent with our findings in gene expression analysis, the protein expression level of MMP2 was diminished by 0.63 times in samples treated with 50 µM auraptene (p < 0.001) and by 0.13 times in those treated with 100 µM auraptene (p < 0.0001) compared with the control group (Fig. 4B).
According to Fig. 4A, auraptene at the concentration of 200 μM and 5-FU significantly reduced the expression of the MMP-9 protein by 0.17 and 0.04 times compared with the control group (p < 0.0001, Fig. 4B). These results suggested that auraptene had a higher impact on the expression of MMP-2 than MMP-9.
Pathological Findings
The stained slides were evaluated by an expert pathologist. There was detectable tumor calcification and necrosis in the tumor tissue in groups treated with 100 and 200 µM auraptene, as well as 5-FU, compared to the control group, whereas tumor cells in other groups did not exhibit morphological changes. These findings indicated that auraptene can inhibit tumor growth and induce necrosis in colorectal tumor cells (Fig. 5).
Discussion
In CRC, as in many types of cancer, metastasis has a significant impact on patient survival and reduces the effectiveness of treatment (Engstrand et al. 2018). In the current study, the anti-metastatic properties of auraptene were evaluated. It was found that auraptene dramatically reduced the tumor size in mice bearing CT26 cells. Moreover, auraptene inhibited the growth and migration of colon cancer cells in monolayer cells. Afshari et al. (2019) showed that the anti-proliferative potential of auraptene was because of its ability to induce cell cycle arrest and apoptosis. In their study, auraptene inhibited the migration of human malignant glioblastoma cells. Another study reported that auraptene prevents the proliferation of MCF-7 cells by targeting genes related to the S-phase of the cell cycle, such as cyclin D1 and insulin-like growth factor 1 (IGF-1) as the stimulators of this phase (Krishnan and Kleiner-Hancock 2012). The results of the study by Jamialahmadi et al. (2018) indicated that the anti-migratory effects of auraptene were due to its ability to suppress the activity of MMP-2 and MMP-9. In order to determine the anti-metastatic potential of auraptene, we evaluated the effects of auraptene on the expression of MMP-2 and MMP-9 in tumor samples. Our study demonstrated that auraptene diminished metastasis by decreasing the expression of MMP-2 and MMP-9 at both gene and protein levels. Our findings showed that the suppression of MMP-2 mRNA was more pronounced than MMP-9 suppression at both gene and protein levels. These results corroborated those of previous studies suggesting that the dysregulation of MMP-2 could be the first sign of CRC tumorigenesis, while MMP-9 dysregulation could be attributed to neovascularization (Araújo et al. 2015). According to the study by Kawabata et al. (2006), when mice received dextran sulfate sodium (DSS), which causes ulcerative colitis, the activity of MMP-2, MMP-9, and MMP-7 was decreased in the mucosa in response to auraptene treatment. In their study, the relative activity of MMPs was assessed by gelatin zymography. They indicated that in mice receiving auraptene for 2 weeks, the activity of MMP-2 and MMP-9 was decreased by 100 and 80%, respectively. In addition, they showed that DSS administration increased MMP-2 and MMP-9 activities by 13 and 31 times, respectively. They also reported that auraptene might have anti-metastatic properties and be beneficial in the treatment of CRC. In another study, the effect of auraptene on the invasion and metastasis of cervical (HeLa) and ovarian (A2780) cancer cells was assessed. In that study, auraptene suppressed the activity of MMP-2 and MMP-9 in a dose-dependent manner at all concentrations (Jamialahmadi et al. 2018). Similar to the results of our study, Charmforoshan et al. (2019) observed that auraptene downregulated the mRNA expression of MMP-2 and MMP-9 in the human breast cancer cell line MCF-7. Moreover, they reported that auraptene had anti-metastatic effects and could be used as adjuvant chemotherapy.
E-cadherin is a vital protein in cell-cell adhesion, and its downregulation results in the invasion of tumor cells (Christou et al. 2017). Based on our results, the mRNA expression of E-cadherin was increased by auraptene at concentrations of 100 and 200 μM (p < 0.05). Our findings were in line with the results reported by Chen et al. (2013), which showed that curcumin inhibited metastasis in a mouse model of CRC by increasing E-cadherin expression. During tumor progression, in addition to metastasis, there is a huge formation of blood vessels around and within tumors. VEGF and its cognate receptor (VEGFR) are essential regulators of angiogenesis (Melincovici et al. 2018). Our results showed that auraptene reduced the gene expression of VEGFR in a dose-dependent manner. Moreover, the expression of VEGF was markedly diminished in response to auraptene treatment at the concentrations of 100 and 200 µM. In a similar study, Jang et al. (2015) found that auraptene inhibited neovascularization in nude mice with renal cancer by lowering VEGF mRNA expression by 70% under hypoxic conditions. In mice treated with 100 μM auraptene subcutaneously, new vessels had a five-fold lower hemoglobin content, and the degree of neovascularization was decreased in comparison with the control group. Pathological findings from the H&E staining of the vessels in tumor tissues were consistent with their results. Nevertheless, Toliver et al. (2011) revealed the ability of VEGF to induce angiogenesis by tube formation in human umbilical vein endothelial cells (HUVEC) and assessed the impact of auraptene on the prevention of this function. According to their results, auraptene exhibited angiogenic activity by targeting VEGF. On the contrary, our results showed that auraptene inhibited colorectal tumor metastasis by decreasing the expression levels of VEGF and VEGFR genes.
As revealed by H&E staining, there were morphological changes and necrosis in the samples treated with 100 and 200 μM auraptene. Furthermore, notable tissue calcification was observed in these two groups, which is related to extensive tumor cell death. Typically, intratumoral calcification results from degenerative changes in the tissue, such as necrosis or hemorrhage, except in a few cases of bone-forming tumors (Karwowski et al. 2012; Yu et al. 2017). In one study, H&E staining results indicated that the rate of renal tumor cell growth was about one-third lower in mice receiving 100 μM auraptene (s.c.) compared with the control mice (Jang et al. 2015). The use of auraptene as an adjunctive therapy and achieving the optimum therapeutic efficacy in CRC patients is a complex issue requiring further in vivo and clinical research in the future. There are several limitations to the current research including the use of an angiogenic CRC model and the evaluation of factors involved in angiogenesis. However, further studies including the simultaneous use of auraptene and 5-FU or immunohistochemical analysis of these proteins are needed to clarify the precise mechanism of action of auraptene in metastasis. It would also be beneficial to study the angiogenesis model in the future.
Conclusion
Our findings showed that auraptene can prevent metastasis by reducing the protein levels of MMP-2 and MMP-9 as well as the gene expression levels of VEGF-A, E-cadherin, and VEGFR1 in CRC and this compound might be considered an alternative medication in adjuvant therapy.
References
Afshari AR, Jalili-Nik M, Soukhtanloo M, Ghorbani A, Sadeghnia HR, Mollazadeh H, Roshan MK, Rahmani F, Sabri H, Vahedi MM, Mousavi SH (2019) Auraptene-induced cytotoxicity mechanisms in human malignant glioblastoma (U87) cells: role of reactive oxygen species (ROS). Excli J 18:576–590. https://doi.org/10.17179/excli2019-1136
Araújo RF Jr, Lira GA, Vilaça JA, Guedes HG, Leitão MCA, Lucena HF, Ramos CCO (2015) Prognostic and diagnostic implications of MMP-2, MMP-9, and VEGF-α expressions in colorectal cancer. Pathol Res Prac 211:71–77. https://doi.org/10.1016/j.prp.2014.09.007
Bhattacharya R, Fan F, Wang R, Ye X, Xia L, Boulbes D, Ellis LM (2017) Intracrine VEGF signalling mediates colorectal cancer cell migration and invasion. Brit J Cancer 117:848–855. https://doi.org/10.1038/bjc.2017.238
Cardiff RD, Miller CH, Munn RJ (2014) Manual hematoxylin and eosin staining of mouse tissue sections. Cold Spring Harb Protoc 2014:655–658. https://doi.org/10.1101/pdb.prot073411
Charmforoshan E, Karimi E, Oskoueian E, Es-Haghi A, Iranshahi M (2019) Inhibition of human breast cancer cells (MCF-7 cell line) growth via cell proliferation, migration, and angiogenesis by auraptene of Ferula szowitsiana root extract. J Food Meas Charact 13:2644–2653. https://doi.org/10.1007/s11694-019-00185-6
Chen CC, Sureshbabul M, Chen HW, Lin YS, Lee JY, Hong QS, Yang YC, Yu SL (2013) Curcumin suppresses metastasis via Sp-1, FAK inhibition, and E-cadherin upregulation in colorectal cancer. Evid-Based Complement Altern Med 2013:541695. https://doi.org/10.1155/2013/541695
Christou N, Perraud A, Blondy S, Jauberteau MO, Battu S, Mathonnet M (2017) E‑cadherin: a potential biomarker of colorectal cancer prognosis. Oncol lett 13:4571–7456. https://doi.org/10.3892/ol.2017.6063
Derosa G, Maffioli P, Sahebkar A (2016) Auraptene and its role in chronic diseases. In: Gupta S, Prasad S, Aggarwal B (eds) Drug discovery from mother nature. Adv Exp Med Biol, Springer, Cham. 929:399–407. https://doi.org/10.1007/978-3-319-41342-6_19
Deryugina EI, Quigley JP (2006) Matrix metalloproteinases and tumor metastasis. Cancer Metastasis Rev 25:9–34. https://doi.org/10.1007/s10555-006-7886-9
Engstrand J, Nilsson H, Strömberg C, Jonas E, Freedman J (2018) Colorectal cancer liver metastases–a population-based study on incidence, management and survival. BMC Cancer 18:78. https://doi.org/10.1186/s12885-017-3925-x
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230:318. https://doi.org/10.1097/00000658-199909000-00004
Genovese S, Epifano F (2011) Auraptene: a natural biologically active compound with multiple targets. Curr Drug Targets 12:381–386. https://doi.org/10.2174/138945011794815248
George ML, Tutton MG, Janssen F, Arnaout A, Abulafi AM, Eccles SA, Swift RI (2001) Vegf-a, vegf-c, and vegf-d in colorectal cancer progression. Neoplasia 3:420–427. https://doi.org/10.1038/sj.neo.7900186
Hayashi K, Suzuki R, Miyamoto S, Shin-Ichiroh Y, Kohno H, Sugie S, Takashima S, Tanaka T (2007) Citrus auraptene suppresses azoxymethane-induced colonic preneoplastic lesions in C57BL/KsJ-db/db mice. Nutr Cancer 58:75–84. https://doi.org/10.1080/01635580701308216
Hooper NM, Itoh Y, Nagase H (2002) Matrix metalloproteinases in cancer. Essays Biochem 38:21–36. https://doi.org/10.1042/bse0380021
Jamialahmadi K, Salari S, Alamolhodaei NS, Avan A, Gholami L, Karimi G (2018) Auraptene inhibits migration and invasion of cervical and ovarian cancer cells by repression of matrix metalloproteinasas 2 and 9 activity. J Pharmacopuncture 21:177–184. https://doi.org/10.3831/kpi.2018.21.021
Jang Y, Han J, Kim SJ, Kim J, Lee MJ, Jeong S, Ryu MJ, Seo KS, Choi SY, Shong M, Lim K (2015) Suppression of mitochondrial respiration with auraptene inhibits the progression of renal cell carcinoma: involvement of HIF-1α degradation. Oncotarget 6:38127–38. https://doi.org/10.18632/oncotarget.5511
Kawabata K, Murakami A, Ohigashi H 2(006) Auraptene decreases the activity of matrix metalloproteinases in dextran sulfate sodium-induced ulcerative colitis in ICR mice. Biosci Biotechnol Biochem 70:3062–3065. https://doi.org/10.1271/bbb.60393
Khorsand M, Khajeh S, Eslami M, Nezafat N, Ghasemi Y, Razban V, Mostafavi-Pour Z (2022) Telmisartan anti-cancer activities mechanism through targeting N-cadherin by mimicking ADH-1 function. J Cell Mol Med 26:2392–2403. https://doi.org/10.1111/jcmm.17259
Kumar D, Arya V, Kaur R, Bhat ZA, Gupta VK, Kumar V (2012) A review of immunomodulators in the Indian traditional health care system. Microbiol Immunol Infect 45:165–184. https://doi.org/10.1016/j.jmii.2011.09.030
Lopez A, Harada K, Vasilakopoulou M, Shanbhag N, Ajani JA (2019) Targeting angiogenesis in colorectal carcinoma. Drugs 79:63–74. https://doi.org/10.1007/s40265-018-1037-9
Melincovici CS, Boşca AB, Şuşman S, Mărginean M, Mihu C, Istrate M, Moldovan IM, Roman AL, Mihu CM (2018) Vascular endothelial growth factor (VEGF)-key factor in normal and pathological angiogenesis. Rom J Morphol Embryol 59:455–467
Melincovici CS, Boşca AB, Şuşman S, Mărginean M, Mihu C, Istrate M, Moldovan IM, Roman AL, Mihu Mogharrabi M, Rahimi HR, Hasanzadeh S, Dastani M, Kazemi-Oskuee R, Akhlaghi S, Soukhtanloo M (2020) The effects of nanomicelle of curcumin on the matrix metalloproteinase (MMP-2, 9) activity and expression in patients with coronary artery disease (CAD): a randomized controlled clinical trial. ARYA Atheroscler 16:136. https://doi.org/10.22122/arya.v16i3.1938
Mohammadi F, Javid H, Afshari AR, Mashkani B, Hashemy SI (2020) Substance P accelerates the progression of human esophageal squamous cell carcinoma via MMP-2, MMP-9, VEGF-A, and VEGFR1 overexpression. Mol Biol Rep 47:4263–4272. https://doi.org/10.1007/s11033-020-05532-1
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65:55–63. https://doi.org/10.1016/0022-1759(83)90303-4
Onogawa S, Kitadai Y, Tanaka S, Kuwai T, Kimura S, Chayama K (2004) Expression of VEGF-C and VEGF-D at the invasive edge correlates with lymph node metastasis and prognosis of patients with colorectal carcinoma. Cancer Sci 95:32–39. https://doi.org/10.1111/j.1349-7006.2004.tb03167.x
Pfaffl MW (2001) A new mathematical model for relative quantification in real-time RT–PCR. Nucleic Acids Res 29:e45–e45. https://doi.org/10.1093/nar/29.9.e45
Said AH, Raufman J-P, Xie G (2014) The role of matrix metalloproteinases in colorectal cancer. Cancers 6:366–375. https://doi.org/10.3390/cancers6010366
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Symowicz J, Adley BP, Gleason KJ, Johnson JJ, Ghosh S, Fishman DA, Hudson LG, Stack MS (2007) Engagement of collagen-binding integrins promotes matrix metalloproteinase-9–dependent E-cadherin ectodomain shedding in ovarian carcinoma cells. Cancer Res 67:2030–2039. https://doi.org/10.1158/0008-5472.can-06-2808
Tanaka T, Kawabata K, Kakumoto M, Hara A, Murakami A, Kuki W, Takahashi Y, Yonei H, Maeda M, Ota T, Odashima S (1998) Citrus auraptene exerts dose-dependent chemopreventive activity in rat large bowel tumorigenesis: the inhibition correlates with suppression of cell proliferation and lipid peroxidation and with induction of phase II drug-metabolizing enzymes. Cancer Res 58:2550–2556
Tanaka T, Kohno H, Murakami M, Kagami S, El-Bayoumy K (2000) Suppressing effects of dietary supplementation of the organoselenium 1, 4-phenylenebis (methylene) selenocyanate and the Citrus antioxidant auraptene on lung metastasis of melanoma cells in mice. Cancer Res 60:3713–3716
Toliver T, Chintalapati M, Losso JN (2011) Anti-angiogenic activity of auraptene. J Young Investigat 22:67–75
Tutton MG, George ML, Eccles SA, Burton S, Swift RI, Abulafi AM (2003) Use of plasma MMP-2 and MMP-9 levels as a surrogate for tumour expression in colorectal cancer patients. Inter J Cancer 107:541–550. https://doi.org/10.1002/ijc.11436
Valderrama-Treviño AI, Barrera-Mera B, Ceballos-Villalva JC, Montalvo-Javé EE (2017) Hepatic metastasis from colorectal cancer. Euroasian J Hepatogastroenterol 7:166–175. https://doi.org/10.5005/jp-journals-10018-1241
Weinberg RA, Weinberg RA (2013) The biology of cancer. WW Norton & Company, New York. https://doi.org/10.1201/9780429258794
Acknowledgements
This study was extracted from the Ph.D. dissertation of Sepideh Ebrahimi (Grant No. 981098) and was financially supported by Mashhad University of Medical Sciences, Mashhad, Iran.
Funding
This study is based on the Ph.D. dissertation of Sepideh Ebrahimi (Grant No. 981098) and was financially supported by Mashhad University of Medical Sciences, Mashhad, Iran.
Author information
Authors and Affiliations
Contributions
MS, ZMP, SE, and MK contributed to the study conception and design. SE, SEN, and MK carried out all the animal experiments. SE performed all the molecular experiments and contributed to the interpretation of the results. STJ carried out the pathological study. Drafts of the manuscript were prepared by SE, and revisions were completed by SK and ZM for publication in the journal. The corresponding author declares that all the listed authors meet the criteria.
Corresponding author
Ethics declarations
Ethics Approval
All animal experiments were performed in accordance with the guidelines of the NIH and the Ethics Committee of Mashhad University of Medical Sciences (IR.MUMS.MEDICAL.REC.1399.744).
Conflict of Interest
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ebrahimi, S., Mostafavi-Pour, Z., Khazaei, M. et al. Suppression of Metastasis by Citrus Auraptene in a Mouse Model of Colorectal Cancer. Rev. Bras. Farmacogn. 33, 182–190 (2023). https://doi.org/10.1007/s43450-022-00351-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43450-022-00351-w