Abstract
Aluminium is one of the most widely distributed elements of the Earth’s crust. Its routine use has resulted in excessive human exposure and due to the potential neurotoxic effects has attained a huge interest in recent years. Despite its ubiquitous abundance, aluminium has no crucial biological functions in the human body. Oxidative stress and neuroinflammatory effects are attributed to its neurotoxic manifestations implicated in Alzheimer’s disease. In this review, we have discussed the neuroinflammatory and neurodegenerative events in the brain induced by aluminium exposure. We have highlighted the neurotoxic events caused by aluminium, such as oxidative stress, apoptosis, inflammatory events, calcium dyshomeostasis, Aβ deposition, and neurofibrillary tangle formation in the brain. In addition, the protective measures needed for prevention of aluminium-induced neuronal dysregulations have also been discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metals are naturally occurring elements, continuously released to the environment by natural events, that easily bioaccumulate in living organisms [1]. Due to the various anthropogenic interventions, such as industrial, domestic and agricultural use of the metal-containing compounds, its human exposure has significantly increased in various regions of the world [2]. Aluminium is the third most abundant element present on the Earth’s terrestrial crust and is widely distributed in the environment. Several salt forms of aluminium such as chloride, hydroxide, phosphide, nitrite, silicate, and sulfate are used across different industries. These include the petroleum industry, glassware and ceramics, fireworks and explosives, the cosmetics industry, the pharmaceutical industries, vaccines, and water purification [3]. Thus, the human population across the world is significantly exposed to aluminium and its bioaccumulation in the brain has been linked to adverse neuroinflammatory and neurodegenerative effects.
Aluminium exposure in Alzheimer’s disease: epidemiological and clinical data
Aluminium has gained substantial attention because of its potential neurotoxic effects. It is redox inactive due to its single oxidation state (+3). Its exposure occurs mainly via drinking water, food, and air [4]. The toxicity of aluminium mainly takes place due to the increasing use of aluminium-containing compounds via dialysates, parenteral nutrition, and vaccines. Due to such diverse exposure, its bioaccumulation may occur in various body tissues, such as the liver, kidney, bones, and brain [5]. Aluminium does not significantly attribute any physiological role, but its chronic exposure may lead to neurodegeneration [6]. It accumulates in various brain regions including the prefrontal cortex, hippocampus, corpus striatum, cerebellum, and brain stem [7]. Aluminium dysregulates the level of essential metals and forms insoluble precipitates, which gets accumulated in the exposed tissues resulting into molecular structural damage and aggregation of cellular proteins, lipids, and DNA. Thus, chronic aluminium exposure may cause neurobehavioral alterations along with pathological and biochemical changes in the brain [8]. Various epidemiological studies have shown that aluminium has been etiologically linked to several neurological diseases including Alzheimer's disease (AD) [9, 10]. AD is the most debilitating, progressive form of neurodegenerative disorders leading to cognitive loss and dementia, particularly in the elderly population. According to World Health Organization (WHO), over fifty million populations are affected with dementia worldwide with around ten million new cases each year. The disease is characterized by a gradual decline in cognitive functions and progressive memory loss, visual–spatial disturbances, confusion, and disorientation. The main pathological hallmarks of AD are extracellular Aβ accumulation and aggregation of neurofibrillary tangles (NFTs) leading to loss of synaptic function and neuronal aberration [11].
Existing pieces of evidence have provided a link between gradual aluminium accumulation in brain tissue and progression of AD pathology. In addition, a few clinical studies have also reported significantly increased levels of aluminium in brain tissue of AD patients [12]. However, a few other groups have failed to find significant differences between aluminium levels in the AD brain as compared to the age-matched controls [13]. It has been shown that the circulatory aluminium level in cerebrospinal fluid (CSF) and serum are higher in AD patients as compared to healthy control subjects [12]. The neurotoxic effects of aluminium have also been shown in dialysis patients in clinical studies. The aluminium salts added as a phosphate binder to the dialysate have shown elevated levels of aluminium in plasma and brain tissue [14] and these individuals exhibited progressive cognitive impairments and dementia [15]. This was mainly due to the slow removal of aluminum from the brain tissue and, the various biological processes affected by aluminum deposition in the brain [16]. Another study showed a positive correlation between cognitive impairment and aluminium intake in elderly subjects, suggesting its exposure as a risk factor for AD [17].
Pharmacokinetics and blood–brain barrier (BBB) transport of aluminium
The accumulation of aluminium in human body tissues occurs primarily through various food and dietary items. It has been found that the bioavailability of aluminium from food and beverages is about 0.1% and from drinking water is about 0.3%. The absorption of aluminium from the gastrointestinal tract primarily occurs in the duodenum [18] and it depends upon the salt ingested, pH, and levels of calcium and iron. The aluminium uptake is enhanced by citrate, lactate, and fluoride salts and is diminished due to the presence of phosphates, silicates, phytate, and polyphenols [19, 20].
The pharmacokinetic distribution of aluminium occurs unequally in various tissues in humans and animals [21]. The actual accumulation of aluminium depends on the aluminium salt administered, species and route (i.e., intravenous, intraperitoneal, or subcutaneous), and kidney function [22]. In healthy human subjects, the total aluminium content ranges from 30 to 50 mg/kg of body weight. The normal serum concentration is- 1–3 μg/L. The skeletal system and lungs have 50% and 25% of the 30–50 mg of total aluminium body burden, respectively. The primary route of aluminium excretion are kidney. The excretion through urine constitutes more than 95% of excreted aluminium [23]. The kidneys can eliminate all the absorbed aluminium unless there is an excess load. The complete elimination of aluminium from other organs and body tissues takes more time. Aluminium can be also marginally excreted through the bile. The unabsorbed aluminium is eliminated through gastrointestinal tract in feces, and the elimination half-life varies in the range of days to years, depending on the body storage compartment, from which it has to be eliminated [24].
Aluminium enters the brain through systemic circulation via three different routes, such as blood–brain barrier (BBB), choroid plexus, and the nasal cavity. However, only a very small amount of aluminium can enter the brain through the nasal cavity and choroid plexus [25]. The entry into the brain through BBB can occurs by diffusion or carrier-mediated process. The transport of aluminium in the brain through BBB occurs by transferrin receptor (Tf–Tfr) complex-mediated endocytosis. Transferrin is the primary iron (Fe) binding protein (Tf–Fe3+) present in the plasma. Around 81% of the circulating aluminium can bind with transferrin and can get transported to the brain through Tf–Tfr complex to cross BBB.
Mechanistic understanding of the neurological effects of aluminium exposure in AD
Aluminium is recognized as a potential neurotoxin, as it is reported to adversely affect several important biological reactions in the brain including neurotransmitter biosynthesis, synaptic transmission, oxidative stress, inflammatory responses, and neuronal development [26]. Aluminium has shown a strong affinity for phosphate groups of DNA leading to conformational changes of DNA [27]. Aluminium may alter expressions of neurofilament-producing gene, neuron-specific enolase, transferrin receptor, RNA polymerase I, antioxidant genes (SOD1, glutathione reductase, etc.), amyloid precursor protein (APP), and β-secretase [28]. Aluminium may also tightly bind to several amino acids such as histidine, tyrosine, and arginine and promotes their phosphorylation, and oligomerization of proteins due to its ionic structure. These structural and conformational changes may prevent their biological degradation. The cross-linking of aluminium to phosphorylated amino acids may also accelerate its accumulation resulting in neuronal and glial apoptosis [26]. Several studies have reported aluminium-induced neuroinflammation and neurodegenerative changes in the brain tissue of animals (Table 1).
Aluminium-induced amyloid-beta (Aβ) aggregation
Aluminium may alter conformational changes in beta-sheet structure of amyloid, which promotes its aggregation and fibril formation [47]. The long term administration of aluminium salts in drinking water to double transgenic mice has shown amyloid–precursor protein (APP) and tau protein over-expression; however, there was no significant alteration of Aβ levels or pro-oxidant activity observed in these animals [48]. Practico et al. have shown that aluminium exposure through drinking water to APP transgenic mice promotes gradual accumulation of Aβ plaques and oxidative stress in the cortex [49]. In addition, it has also been demonstrated in-vitro that aluminium salts may promote Aβ aggregation [50].
Aluminium-induced tau aggregation
A higher level of environmental aluminium has been related to the pathological alterations in CNS, such as NFTs and neuronal dysfunctions [4]. Protein phosphatase 2A (PP2A), a major phosphate-removing enzyme in the brain, may prevent tau aggregation and formation of NFT [51]. During the progression and development of AD, the activity and expression of PP2A are shown to be decreased [52]. Another study found that 14-3-3ζ protein has a high affinity for aluminium in hippocampal tissue. The 14-3-3ζ protein forms complex with tau protein and can prevent its hyperphosphorylation. However, this is destabilized due to aluminium exposure leading to binding of 14-3-3ζ with aluminium (Fig. 1). In addition, the level of tau hyperphosphorylation is induced in aluminium-exposed dendrites and may lead to synaptic dysfunction. This explanation may provide one of the mechanistic evidence for aluminium-induced neurotoxicity in AD [53].
Aluminium and cholinergic dysfunction
The cholinergic functions in the brain are primarily dependent on the modulation of the neurotransmitter acetylcholine (ACh). ACh is degraded in the synaptic cleft by acetylcholine esterase (AChE) after its release from the presynaptic nerve terminals [54]. Therefore, any alterations in AChE levels may result in the modulation of neurobehavioral changes [55]. Aluminium is shown to affect the cholinergic changes by altering the synthesis and degradation of ACh [56]. It also interferes with the binding of ACh to the muscarinic acetylcholine receptors (mAChRs) and nicotinic acetylcholine receptors (nAChRs) [46]. Aluminium exposure has shown distinct cholinergic dysfunction in different regions of brain tissue and induction of neurobehavioral alteration in male albino rats [57].
Aluminium-induced apoptosis
Aluminium activates caspase-3 and DNA fragmentation by inducing the release of mitochondrial cytochrome-c, decreased expression of Bcl-2 in mitochondria and endoplasmic reticulum, and mitochondrial Bax translocation. The cytochrome-c may bind to apoptosis protease activating factor-1 to induce caspase-9 and caspase-3 activation [58]. The cytochrome-c may also lead to Bax translocation to mitochondria through modulation of the transition pores. These cytotoxic stimuli trigger the mitochondrial changes responsible for the initiation of the primary events in apoptosis [59]. Moreover, it has also been shown that aluminium can induce neuronal apoptosis through stress-activated protein kinase or c-Jun N-terminal kinase activation (Fig. 2) [60]. Aluminium exposure has also caused cellular shrinkage, hyper-condensed and damaged chromatin, characteristic features of apoptosis [61].
Fe2+/Ca2+ dyshomeostasis
Aluminium competes with iron for iron-binding proteins, such as ferritin, transferrin, and iron regulatory protein (IRP). The IRP regulates and prevents free Fe2+ formation, which further causes free radical generation [62]. Aluminium influences the expression of iron-binding proteins leading to elevated iron concentration [63]. It also increases the uptake of iron by the glial cells [64]. Thus, aluminium may affect the expression and homeostasis of iron, IRPs, and IREs. The APP mRNA contains IRE as well as ferritin regulated by iron [65], which exhibit ferroxidase activity [66]. Aluminium exposure also induces iron-mediated lipid peroxidation and oxidative stress in-vitro and in-vivo [67].
Aluminium can also cause neuronal damage by disrupting calcium homeostasis. It can delay the closure of voltage-dependent calcium channels and may block calmodulin (CaM)-dependent Ca2+/Mg2+-ATPase. It helps in the extrusion of excess intracellular calcium and protects against excitotoxicity. In-vivo exposure of aluminium was shown to elevate glutamate and decrease γ-aminobutyric acid (GABA) levels in the brain, leading to excitotoxic damage [68]. Aluminium induces an elevation in the level of resting and peak Ca2+ concentrations in neuronal cytoplasm, inhibition of phosphoinositide 4,5-biphosphate (PIP2) hydrolysis. This may result in less inositol triphosphate (IP3) availability for downstream signaling and protein kinase C (PKC) activation; and a slower rate of Ca2+ removal from the cytoplasm. Thus, Ca2+ dyshomeostasis and alteration of Ca2+ signaling could result due to neuronal aluminium accumulation (Fig. 3) leading to neuronal dysfunction [69].
Aluminium-induced neuronal oxidative stress
Oxidative stress is one of the major contributing factors involved in the progression of several neurodegenerative diseases including AD [49]. Despite redox-inactive status, many studies have suggested that aluminium has strong pro-oxidant activity [70]. Aluminium salts may cause oxidative stress-related changes, such as enhanced lipid peroxidation, increased 4-HNE formations. Exposure to aluminium chloride (50 mg/kg/day, oral for 30 days) showed alterations in antioxidant enzymes and increased lipoprotein tissue damage in the brain [71]. Aluminium promotes mitochondrial damage through generation of toxic free radicals (OH−) and may lead to decrease in the activity of glutathione peroxidase, catalase, and SOD, aggravating neuronal damage through oxidative stress in AD [72]. Aluminium may potentiate an increase in glutamate-induced excitotoxicity in neurons [73]. These devastating cellular and impaired mitochondrial alterations have an additive effect on excitotoxicity [74], and are responsible for the disturbances of tissue-protective mechanisms against excitotoxicity [75].
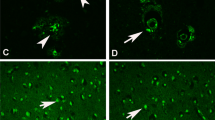
Mechanism of neuroinflammation due to aluminium exposure
The neuroinflammatory response is primarily triggered by the activation of the microglial cells in the brain. This aggravates the accumulation of Aβ and NFTs, the core pathological features of AD [76]. The proinflammatory effects of aluminium exposure are initiated by oxidative stress and the generation of free radicals [77]. Aluminium upregulates pro-inflammatory signaling encoding genes [78]. It has been shown that aluminium exposure increases transcription and translation of pro-inflammatory cytokine TNFα, IL-1β and macrophage inflammatory protein-1α (MIP-1α) in a concentration-dependent manner resulting in exacerbation of neuroinflammation [77]. Chronic exposure of aluminium sulfate in drinking water in mice has been shown to induce systemic inflammation characterized by increased serum IL-6, TNFα, C-reactive protein (CRP), and pro-inflammatory microRNAs (miRNA-9, miRNA-125b, and miRNA-146a) triads. These elevated levels of biomarkers indicate progressive chronic inflammation in exposed animals [3]. The prolonged exposure to low aluminium concentration may also induce glial fibrillary astrocytic protein (GFAP) in the frontal cortex of the brain, which is an indicator of astrocytic immune activation [79]. In brain injury, aluminium has been shown to induce proinflammatory cytokines, TNF-α, IL-1β, intracellular Ca2+, and oxidative stress [78].
Approaches used to alleviate aluminium-induced neurotoxicity in AD
Several approaches aiming to ameliorate aluminium-induced oxidative stress, mitochondrial dysfunction, and neuroinflammation have been reported in the literature. These approaches include chelation therapy and supplementation of antioxidants or pharmaceutical agents (Fig. 4).
Chelation therapy
A chelator is a molecule that possesses electron-donating functional groups for the formation of a bond with the metal ion [80]. The metal toxicity can be efficiently treated with the therapeutic use of a suitable chelator. Such an agent must be able to form a stable complex with a toxic metal, and should facilitate its elimination from its biological targets to reduce the associated toxic effects of its bioaccumulation [81].
Deferoxamine (DFO) is one of the iron chelators, used in aluminium toxicity, because it can form a stable DFO–Al complex [82]. The Kidney Disease Outcomes Quality Initiative (KDOQI) has recommended DFO for aluminium overload in the treatment of dialysis patients [83]. It has been shown that the treatment with DFO in rabbits lead to a partial reversal of aluminium-induced neurofibrillary degeneration [84]. Another study showed that DFO and 1,2-dimethyl-3-hydroxypyrid-4-one (L1) and 1-(p-methyl benzyl)-2-ethyl-3-hydroxypyrid-4-one (MeBzEM) were most effective in enhancing the urinary aluminium excretion in rats through chelation [85]. Ascorbate and Feralex-G, either alone or in combination with DFO, have successively been introduced as a molecular shuttle chelation therapy for aluminium intoxication [86].
Antioxidant therapy in aluminium toxicity
Vitamin C is one of the common antioxidants, that helps to scavenge reactive oxygen species by the rapid electron transfer mechanism. Hence, vitamin C has a protective effect against age-related cognitive deterioration in AD [87]. It has also exhibited tissue-protective properties in aluminium-induced toxicity in-vivo [88]. Vitamin E is another lipid-soluble antioxidant, and its dietary supplementation decreased the levels of GFAP, S100B, and proinflammatory markers (TNF-α and IL-1β) in the hippocampus and cortex of male Wistar rats. The co-treatment of vitamin E with aluminium lactate (10 mg/kg for 4 weeks by intraperitoneal route) decreased aluminium burden across different regions of brain tissues and an increase in glutathione and catalase levels [89, 90].
Melatonin prevents the damage of cell membrane caused by lipid peroxidation through free radical scavenging activity. It prevents Aβ generation, fibril formation and protects against Aβ-mediated neuronal toxicity through its antioxidant activity. Melatonin efficiently attenuates tau hyperphosphorylation in AD [91]. In aluminium exposed isolated synaptosomes, melatonin supplementation lowers protein and lipid peroxidation in a concentration-dependent manner [92].
Curcumin has demonstrated potent anti-inflammatory, antioxidant and anticancer activities in-vitro and in-vivo [28, 93, 94]. It can inhibit aluminium-induced Aβ42 fibrillation and neurotoxicity [93]. It has been shown to alleviate aluminium-induced neurotoxicity at electrophysiological, biochemical, and behavioral levels [94]. Another known antioxidant, alpha-lipoic acid (α-LA) is a well-known fatty acid, used as a supplement in neurodegenerative disorders and peripheral neuropathies. α-LA alleviates the neurotoxic effects of reactive oxygen species in the brain due to its antioxidant properties. α-LA improves learning and memory by increasing the expression of choline acetyltransferase (ChAT), M1, and M2 genes in the hippocampus and amygdala in mice [95, 96]. N-acetyl cysteine (synthetic GSH precursor) has been shown to restore the elevated lipid peroxidation levels and antioxidant defence system in brain tissues of rats, exposed to aluminium chloride (100 mg/kg, oral) [97].
Furthermore, several plant constituents such as flavonoids have been found to exert a protective effect against aluminium-induced neurotoxicity. Fisetin can attenuate aluminium chloride-induced modulation of lipid peroxidation, glutathione, and antioxidant enzyme status in mice [98]. Naringin, a flavanone glycoside protects against aluminium chloride (100 mg/kg, oral, 6 weeks) induced oxidative mitochondrial damage in rat brain [99]. Hesperidin, a flavoglycone attenuates aluminium-induced neurotoxicity by decreasing proinflammatory markers such as TNF-α, IL-6, IL-1β, IL-4 and prevents microglial activation in the hippocampus and cortex [100].
Drug therapy
Meloxicam is a cyclooxygenase (COX) inhibitor used as a non-steroidal anti-inflammatory drug (NSAID) and prevents cerebral neuronal damage by decreasing lipid peroxidation, malondialdehyde (MDA) level [101] through modulation of COX-2 mRNA expression in aluminium-exposed mice [101]. Another COX inhibitor, ibuprofen has been shown to attenuate aluminium-induced neurite loss and synaptic dysfunction [102]. Ginkgo biloba has shown protection against neurotoxic effects by regulation of MDA and GSH in brain tissue in a sub-chronic aluminium-exposed rat model [103]. However, it has been demonstrated that co-administration of vitamins or antioxidants with a chelator may produce more beneficial therapeutic effects [47]. The oral administration of either hydroxyethylenediaminetriacetic acid (HEDTA) or citric acid prior to aluminium nitrate exposure showed moderate therapeutic efficacy by the alteration of oxidative stress in the brain. Although, their combination exerted better therapeutic protection in the same model [4].
Discussion and future perspectives
Aging is one of the major risk factors for the accumulation of aluminium in the brain and may lead to the progression of several neurodegenerative diseases, such as AD. Aluminium is one of the proven and incontrovertible neurotoxins. Aluminum has been shown to produce neurotoxicity by diverse mechanisms such as it promotes the formation and accumulation of insoluble Aβ and hyperphosphorylated tau. Excess of insoluble Aβ contributes to the development and progression of AD. In addition, aluminium also mimics the deficit of cortical cholinergic neurotransmission in AD. Furthermore, aluminium induces iron and calcium dyshomeostasis in the brain, and thereby facilitates oxidative stress, neuronal injury, and apoptotic cell death. Thus, disruption of basic cell processes in the brain may mediate primary molecular mechanisms of aluminium-induced neurotoxicity.
To minimize the risk of aluminium-induced neurotoxicity, it is necessary to clearly understand the mechanism by which the burden of aluminium significantly increases in the brain. Thus, approaches for the avoidance of continuous repeated exposure of aluminium seem to be more prudent. However, the approaches to reduce the consequent oxidative stress, neuronal damage, molecular, structural, and functional biomarkers seem to be more viable, if significant bioaccumulation of aluminium in brain tissue has occurred. In addition, the facilitation of accumulated aluminium excretion to reduce the total body burden of aluminium may also offer some therapeutic hope to halt the progression of AD. These approaches may prove to be clinically significant to improve the manifestations of the risk of aluminium-induced neurotoxicity in AD.
Conclusion
Aluminium is one of the widely recognized neurotoxicants and exerts its neurotoxic effects through exacerbation of oxidative stress and neuroinflammation due to its accumulation in brain tissue. Several mechanistic pieces of evidence related to the aluminium-induced toxicity have been discussed in the literature; however, the exact mechanism for neurotoxicity is a matter of further debate. Neuronal inflammation and oxidative stress are thought to be the causative factors for aluminium-induced neurotoxicity in the pathogenesis of AD. Specific therapeutic targeting of various neuroinflammatory mechanisms and oxidative stress parameters could be effective for the treatment of aluminium induced neurodegenerative disorders. The therapeutic use of several natural antioxidant products either alone or with other drugs/disease-modifying agents may provide significant beneficial effects. However, the molecular mechanisms of the neuroprotective effect of these agents remain to be elucidated. Further studies are required to understand the exact mechanisms and development of better therapeutic strategies for aluminium-induced neurotoxicity.
References
Jaishankar M, Tseten T, Anbalagan N, Mathew BB, Beeregowda KN. Toxicity, mechanism and health effects of some heavy metals. Interdiscip Toxicol. 2014;7:60–72. https://doi.org/10.2478/intox-2014-0009.
Anyanwu BO, Ezejiofor AN, Igweze ZN, Orisakwe OE. Heavy metal mixture exposure and effects in developing nations: an update. Toxics. 2018;6:1–32. https://doi.org/10.3390/toxics6040065.
Igbokwe IO, Igwenagu E, Igbokwe NA. Aluminium toxicosis: a review of toxic actions and effects. Interdiscip Toxicol. 2020;12:45–70. https://doi.org/10.2478/intox-2019-0007.
Kumar V, Gill KD. Oxidative stress and mitochondrial dysfunction in aluminium neurotoxicity and its amelioration: a review. Neurotoxicology. 2014;41:154–66. https://doi.org/10.1016/j.neuro.2014.02.004.
Exley C. Human exposure to aluminium. Environ Sci Process Impacts. 2013;15:1807–16. https://doi.org/10.1039/c3em00374d.
Exley C. The aluminium-amyloid cascade hypothesis and Alzheimer’s disease. Subcell Biochem. 2005;38:225–34. https://doi.org/10.1007/0-387-23226-5_11.
Julka D, Vasishta RK, Gill KD. Distribution of aluminum in different brain regions and body organs of rat. Biol Trace Elem Res. 1996;52:181–92. https://doi.org/10.1007/bf02789460.
Kaur A, Joshi K, Minz RW, Gill KD. Neurofilament phosphorylation and disruption: a possible mechanism of chronic aluminium toxicity in Wistar rats. Toxicology. 2006;219:1–10. https://doi.org/10.1016/j.tox.2005.09.015.
Santibañez M, Bolumar F, García AM. Occupational risk factors in Alzheimer’s disease: a review assessing the quality of published epidemiological studies. Occup Environ Med. 2007;64:723–32. https://doi.org/10.1136/oem.2006.028209.
Solfrizzi V, Colacicco AM, D’Introno A, Capurso C, Del PA, Capurso SA, et al. Macronutrients, aluminium from drinking water and foods, and other metals in cognitive decline and dementia. J Alzheimer’s Dis. 2006;10:303–30. https://doi.org/10.3233/JAD-2006-102-314.
Gupta VB, Anitha S, Hegde ML, Zecca L, Garruto RM, Ravid R, et al. Aluminium in Alzheimer’s disease: are we still at a crossroad? Cell Mol Life Sci. 2005;62:143–58. https://doi.org/10.1007/s00018-004-4317-3.
Exley C, Clarkson E. Aluminium in human brain tissue from donors without neurodegenerative disease: a comparison with Alzheimer’s disease, multiple sclerosis and autism. Sci Rep. 2020;10:1–7. https://doi.org/10.1038/s41598-020-64734-6.
Mcdermott JR, Smith AI, Iqbal K, Wisniewski HM. Brain aluminum in aging and Alzheimer disease. Neurology. 1979;29:809–14. https://doi.org/10.1212/wnl.29.6.809.
Parkinson IS, Ward MK, Kerr DNS. Dialysis encephalopathy, bone disease and anaemia: the aluminium intoxication syndrome during regular haemodialysis. J Clin Pathol. 1981;34:1285–94. https://doi.org/10.1136/jcp.34.11.1285.
Alfrey AC, LeGendre GR, Kaehny WD. The dialysis encephalopathy syndrome. N Engl J Med. 1976;294:184–8. https://doi.org/10.1056/nejm197601222940402.
Klotz K, Weistenhöfer W, Neff F, Hartwig A, Van Thriel C, Drexler H. The health effects of aluminum exposure. Dtsch Arztebl Int. 2017;114:653–9. https://doi.org/10.3238/arztebl.2017.0653.
Rondeau V, Jacqmin-Gadda H, Commenges D, Helmer C, Dartigues JF. Aluminum and silica in drinking water and the risk of Alzheimer’s disease or cognitive decline: findings from 15-year follow-up of the PAQUID cohort. Am J Epidemiol. 2009;169:489–96. https://doi.org/10.1093/aje/kwn348.
Steinhausen C, Kislinger G, Winklhofer C, Beck E, Hohl C, Nolte E. Investigation of the aluminium biokinetics in humans: a 26Al tracer study. Food Chem Toxicol. 2004;42(3):363–71. https://doi.org/10.1016/j.fct.2003.09.010.
Kandimalla R, Vallamkondu J, Corgiat EB, Gill KD. Understanding aspects of aluminum exposure in Alzheimer’s disease development. Brain Pathol. 2016;26(2):139–54. https://doi.org/10.1111/bpa.12333.
Tietz T, Lenzner A, Kolbaum AE, Zellmer S, Riebeling C, Gürtler R, et al. Aggregated aluminium exposure: risk assessment for the general population. Arch Toxicol. 2019;93:3503–21. https://doi.org/10.1007/s00204-019-02599-z.
Novaes RD, Mouro VGS, Gonçalves RV, Mendonça AAS, Santos EC, Fialho MCQ, et al. Aluminum: a potentially toxic metal with dose-dependent effects on cardiac bioaccumulation, mineral distribution, DNA oxidation and microstructural remodeling. Environ Pollut. 2018;242:814–26. https://doi.org/10.1016/j.envpol.2018.07.034.
Krewski D, Yokel RA, Nieboer E, Borchelt D, Cohen J, Kacew S, et al. Human health risk assessment for aluminium, aluminium oxide, and aluminium hydroxide. J Toxicol Environ Health B Crit Rev. 2007;10:1–269. https://doi.org/10.1080/10937400701597766.
Yokel RA. Aluminium toxicokinetics: an updated minireview. Pharmacol Toxicol. 2001;88:159–67. https://doi.org/10.1111/j.1600-0773.2001.880401.x.
Nie J. Exposure to aluminum in daily life and Alzheimer’s disease. Adv Exp Med Biol. 2018;1091:99–111. https://doi.org/10.1007/978-981-13-1370-7_6.
Wang L. Entry and deposit of aluminum in the brain. Adv Exp Med Biol. 2018;1091:39–51. https://doi.org/10.1007/978-981-13-1370-7_3.
Kawahara M, Kato-Negishi M. Link between aluminum and the pathogenesis of Alzheimer’s disease: the integration of the aluminum and amyloid cascade hypotheses. Int J Alzheimers Dis. 2011;2011: 276393. https://doi.org/10.4061/2011/276393.
Bharathi SG, Rao KSJ, Stein R. First evidence on induced topological changes in supercoiled DNA by an aluminium d-aspartate complex. J Biol Inorg Chem. 2003;8:823–30. https://doi.org/10.1007/s00775-003-0484-1.
Lin R, Chen X, Li W, Han Y, Liu P, Pi R. Exposure to metal ions regulates mRNA levels of APP and BACE1 in PC12 cells: blockage by curcumin. Neurosci Lett. 2008;440:344–7. https://doi.org/10.1016/j.neulet.2008.05.070.
Taïr K, Kharoubi O, Taïr OA, Hellal N, Benyettou I, Aoues A. Aluminium-induced acute neurotoxicity in rats: treatment with aqueous extract of Arthrophytum (Hammada scoparia). J Acute Dis. 2016;5:470–82. https://doi.org/10.1016/j.joad.2016.08.028.
Kumar V, Bal A, Gill KD. Aluminium-induced oxidative DNA damage recognition and cell-cycle disruption in different regions of rat brain. Toxicology. 2009;264:137–44. https://doi.org/10.1016/j.tox.2009.05.011.
Cao Z, Yang X, Zhang H, Wang H, Huang W, Xu F, et al. Aluminum chloride induces neuroinflammation, loss of neuronal dendritic spine and cognition impairment in developing rat. Chemosphere. 2016;151:289–95. https://doi.org/10.1016/j.chemosphere.2016.02.092.
Olajide OJ, Yawson EO, Gbadamosi IT, Arogundade TT, Lambe E, Obasi K, et al. Ascorbic acid ameliorates behavioural deficits and neuropathological alterations in rat model of Alzheimer’s disease. Environ Toxicol Pharmacol. 2017;50:200–11. https://doi.org/10.1016/j.etap.2017.02.010.
Ahmad Rather M, Justin-Thenmozhi A, Manivasagam T, Saravanababu C, Guillemin GJ, Essa MM. Asiatic acid attenuated aluminum chloride-induced tau pathology, oxidative stress and apoptosis via AKT/GSK-3β signaling pathway in wistar rats. Neurotox Res. 2019;35:955–68. https://doi.org/10.1007/s12640-019-9999-2.
Chakrabarty M, Bhat P, Kumari S, D’Souza A, Bairy KL, Chaturvedi A, et al. Cortico-hippocampal salvage in chronic aluminium induced neurodegeneration by Celastruspaniculatus seed oil: neurobehavioural, biochemical, histological study. J Pharmacol Pharmacother. 2012;3:161–71. https://doi.org/10.4103/0976-500X.95520.
Iglesias-González J, Sánchez-Iglesias S, Beiras-Iglesias A, Méndez-Álvarez E, Soto-Otero R. Effects of aluminium on rat brain mitochondria bioenergetics: an in vitro and in vivo study. Mol Neurobiol. 2017;54:563–70. https://doi.org/10.1007/s12035-015-9650-z.
Prema A, Justin Thenmozhi A, Manivasagam T, Mohamed Essa M, Guillemin GJ. Fenugreek seed powder attenuated aluminum chloride-induced tau pathology, oxidative stress, and inflammation in a rat model of Alzheimer’s disease. J Alzheimer’s Dis. 2017;60:S209–20. https://doi.org/10.3233/JAD-161103.
Prakash D, Gopinath K, Sudhandiran G. Fisetin enhances behavioral performances and attenuates reactive gliosis and inflammation during aluminum chloride-induced neurotoxicity. NeuroMolecular Med. 2013;15:192–208. https://doi.org/10.1007/s12017-012-8210-1.
Wang H, Ye M, Yu L, Wang J, Guo Y, Lei W, et al. Hippocampal neuronal cyclooxygenase-2 downstream signaling imbalance in a rat model of chronic aluminium gluconate administration. Behav Brain Funct. 2015;11:1–12. https://doi.org/10.1186/s12993-015-0054-z.
Khan KA, Kumar N, Nayak PG, Nampoothiri M, Shenoy RR, Krishnadas N, et al. Impact of caffeic acid on aluminium chloride-induced dementia in rats. J Pharm Pharmacol. 2013;65:1745–52. https://doi.org/10.1111/jphp.12126.
Yu H, Zhang J, Ji Q, Yu K, Wang P, Song M, et al. Melatonin alleviates aluminium chloride-induced immunotoxicity by inhibiting oxidative stress and apoptosis associated with the activation of Nrf2 signaling pathway. Ecotoxicol Environ Saf. 2019;173:131–41. https://doi.org/10.1016/j.ecoenv.2019.01.095.
Singh NA, Bhardwaj V, Ravi C, Ramesh N, Mandal AKA, Khan ZA. EGCG nanoparticles attenuate aluminum chloride induced neurobehavioral deficits, beta amyloid and tau pathology in a rat model of Alzheimer’s disease. Front Aging Neurosci. 2018;10:1–13. https://doi.org/10.3389/fnagi.2018.00244.
Fernandes J, Mudgal J, Rao CM, Arora D, Basu Mallik S, Pai KSR, et al. N-acetyl-l-tryptophan, a substance-P receptor antagonist attenuates aluminum-induced spatial memory deficit in rats. Toxicol Mech Methods. 2018;28:328–34. https://doi.org/10.1080/15376516.2017.1411412.
Ekong MB, Ekpo MM, Akpanyung EO, Nwaokonko DU. Neuroprotective effect of Moringa oleifera leaf extract on aluminium-induced temporal cortical degeneration. Metab Brain Dis. 2017;32:1437–47. https://doi.org/10.1007/s11011-017-0011-7.
Bihaqi SW, Sharma M, Singh AP, Tiwari M. Neuroprotective role of Convolvulus pluricaulis on aluminium induced neurotoxicity in rat brain. J Ethnopharmacol. 2009;124:409–15. https://doi.org/10.1016/j.jep.2009.05.038.
Lakshmi BVS, Sudhakar M, Anisha M. Neuroprotective role of hydroalcoholic extract of Vitis vinifera against aluminium-induced oxidative stress in rat brain. Neurotoxicology. 2014;41:73–9. https://doi.org/10.1016/j.neuro.2014.01.003.
Farhat SM, Mahboob A, Ahmed T. Oral exposure to aluminum leads to reduced nicotinic acetylcholine receptor gene expression, severe neurodegeneration and impaired hippocampus dependent learning in mice. Drug Chem Toxicol. 2021;44(3):310–8. https://doi.org/10.1080/01480545.2019.1587452.
Crisponi G, Nurchi VM, Bertolasi V, Remelli M, Faa G. Chelating agents for human diseases related to aluminium overload. Coord Chem Rev. 2012;256:89–104. https://doi.org/10.1016/j.ccr.2011.06.013.
Akiyama H, Hosokawa M, Kametani F, Kondo H, Chiba M, Fukushima M, et al. Long-term oral intake of aluminium or zinc does not accelerate Alzheimer pathology in AβPP and AβPP/tau transgenic mice. Neuropathology. 2012;32:390–7. https://doi.org/10.1111/j.1440-1789.2011.01274.x.
Praticò D, Uryu K, Sung S, Tang S, Trojanowski JQ, Lee VMY. Aluminum modulates brain amyloidosis through oxidative stress in APP transgenic mice. FASEB J. 2002;16:1138–40. https://doi.org/10.1096/fj.02-0012fje.
Bolognin S, Messori L, Drago D, Gabbiani C, Cendron L, Zatta P. Aluminum, copper, iron and zinc differentially alter amyloid-Aβ 1–42 aggregation and toxicity. Int J Biochem Cell Biol. 2011;43:877–85. https://doi.org/10.1016/j.biocel.2011.02.009.
Liu F, Grundke-Iqbal I, Iqbal K, Gong CX. Contributions of protein phosphatases PP1, PP2A, PP2B and PP5 to the regulation of tau phosphorylation. Eur J Neurosci. 2005;22:1942–50. https://doi.org/10.1111/j.1460-9568.2005.04391.x.
Walton JR. An aluminum-based rat model for Alzheimer’s disease exhibits oxidative damage, inhibition of PP2A activity, hyperphosphorylated tau, and granulovacuolar degeneration. J Inorg Biochem. 2007;101:1275–84. https://doi.org/10.1016/j.jinorgbio.2007.06.001.
Wang X, Cheng D, Jiang W, Ma Y. Mechanisms underlying aluminum neurotoxicity related to 14-3-3ζ protein. Toxicol Sci. 2018;163:45–56. https://doi.org/10.1093/toxsci/kfy021.
Maya S, Prakash T, Madhu KD, Goli D. Multifaceted effects of aluminium in neurodegenerative diseases: a review. Biomed Pharmacother. 2016;83:746–54. https://doi.org/10.1016/j.biopha.2016.07.035.
Saiyed SM, Yokel RA. Aluminium content of some foods and food products in the USA, with aluminium food additives. Food Addit Contam. 2005;22:234–44. https://doi.org/10.1080/02652030500073584.
Stevanović ID, Jovanović MD, Čolić M, Jelenković A, Bokonjić D, Ninković M. Nitric oxide synthase inhibitors protect cholinergic neurons against AlCl3 excitotoxicity in the rat brain. Brain Res Bull. 2010;81:641–6. https://doi.org/10.1016/j.brainresbull.2010.01.004.
Yellamma K, Saraswathamma S, Kumari BN. Cholinergic system under aluminium toxicity in rat brain. Toxicol Int. 2010;17:106–12. https://doi.org/10.4103/0971-6580.72682.
Ghribi O, Herman MM, Forbes MS, DeWitt DA, Savory J. GDNF protects against aluminum-induced apoptosis in rabbits by upregulating Bcl-2 and Bcl-XL and inhibiting mitochondrial Bax translocation. Neurobiol Dis. 2001;8:764–73. https://doi.org/10.1006/nbdi.2001.0429.
Vasudevaraju BP, Govindaraju M, Palanisamy AP, Sambamurti K, Rao KSJ. Molecular toxicity of aluminium in relation to neurodegeneration. Indian J Med Res. 2008;128:545–56.
Fu HJ, Hu QS, Lin ZN, Ren TL, Song H, Cai CK, et al. Aluminum-induced apoptosis in cultured cortical neurons and its effect on SAPK/JNK signal transduction pathway. Brain Res. 2003;980:11–23. https://doi.org/10.1016/S0006-8993(03)02833-6.
Maroney AC, Glicksman MA, Basma AN, Walton KM, Knight E, Murphy CA, et al. Motoneuron apoptosis is blocked by CEP-1347 (KT 7515), a novel inhibitor of the JNK signaling pathway. J Neurosci. 1998;18:104–11. https://doi.org/10.1523/jneurosci.18-01-00104.1998.
Muckenthaler MU, Galy B, Hentze MW. Systemic iron homeostasis and the iron-responsive element/iron-regulatory protein (IRE/IRP) regulatory network. Annu Rev Nutr. 2008;28:197–213. https://doi.org/10.1146/annurev.nutr.28.061807.155521.
Crichton RR, Wilmet S, Legssyer R, Ward RJ. Molecular and cellular mechanisms of iron homeostasis and toxicity in mammalian cells. J Inorg Biochem. 2002;91:9–18. https://doi.org/10.1016/S0162-0134(02)00461-0.
Oshiro S, Kawahara M, Kuroda Y, Zhang C, Cai Y, Kitajima S, et al. Glial cells contribute more to iron and aluminum accumulation but are more resistant to oxidative stress than neuronal cells. Biochim Biophys Acta Mol Basis Dis. 2000;1502:405–14. https://doi.org/10.1016/S0925-4439(00)00065-X.
Cho HH, Cahill CM, Vanderburg CR, Scherzer CR, Wang B, Huang X, et al. Selective translational control of the Alzheimer amyloid precursor protein transcript by iron regulatory protein-1. J Biol Chem. 2010;285:31217–32. https://doi.org/10.1074/jbc.M110.149161.
Duce JA, Tsatsanis A, Cater MA, James SA, Robb E, Wikhe K, et al. Iron-export ferroxidase activity of β-amyloid precursor protein is Inhibited by zinc in Alzheimer’s disease. Cell. 2010;142:857–67. https://doi.org/10.1016/j.cell.2010.08.014.
Kaneko N, Sugioka T, Sakurai H. Aluminum compounds enhance lipid peroxidation in liposomes: insight into cellular damage caused by oxidative stress. J Inorg Biochem. 2007;101:967–75. https://doi.org/10.1016/j.jinorgbio.2007.03.005.
Blaylock RL. Aluminum induced immunoexcitotoxicity in neurodevelopmental and neurodegenerative disorders. Curr Inorg Chem. 2012;2:46–53. https://doi.org/10.2174/1877944111202010046.
Walton JR. Aluminum disruption of calcium homeostasis and signal transduction resembles change that occurs in aging and Alzheimer’s disease. J Alzheimer’s Dis. 2012;29:255–73. https://doi.org/10.3233/JAD-2011-111712.
Yuan CY, Lee YJ, Hsu GSW. Aluminum overload increases oxidative stress in four functional brain areas of neonatal rats. J Biomed Sci. 2012;19:1–9. https://doi.org/10.1186/1423-0127-19-51.
Jyoti A, Sharma D. Neuroprotective role of Bacopa monniera extract against aluminium-induced oxidative stress in the hippocampus of rat brain. Neurotoxicology. 2006;27:451–7. https://doi.org/10.1016/j.neuro.2005.12.007.
Johri A, Beal MF. Mitochondrial dysfunction in neurodegenerative diseases. J Pharmacol Exp Ther. 2012;342:619–30. https://doi.org/10.1124/jpet.112.192138.
Nayak P, Chatterjee AK. Effects of aluminium exposure on brain glutamate and GABA systems: an experimental study in rats. Food Chem Toxicol. 2001;39:1285–9. https://doi.org/10.1016/S0278-6915(01)00077-1.
Blaylock R, Maroon J. Immunoexcitotoxicity as a central mechanism in chronic traumatic encephalopathy—a unifying hypothesis. Surg Neurol Int. 2011;2:107. https://doi.org/10.4103/2152-7806.83391.
Exley C. A molecular mechanism of aluminium-induced Alzheimer’s disease? J Inorg Biochem. 1999;76:133–40. https://doi.org/10.1016/S0162-0134(99)00125-7.
Weng MH, Chen SY, Li ZY, Yen GC. Camellia oil alleviates the progression of Alzheimer’s disease in aluminum chloride-treated rats. Free Radic Biol Med. 2020;152:411–21. https://doi.org/10.1016/j.freeradbiomed.2020.04.004.
Milnerowicz H, Ściskalska M, Dul M. Pro-inflammatory effects of metals in persons and animals exposed to tobacco smoke. J Trace Elem Med Biol. 2015;29:1–10. https://doi.org/10.1016/j.jtemb.2014.04.008.
Lukiw WJ, Percy ME, Kruck TP. Nanomolar aluminum induces pro-inflammatory and pro-apoptotic gene expression in human brain cells in primary culture. J Inorg Biochem. 2005;99:1895–8. https://doi.org/10.1016/j.jinorgbio.2005.04.021.
Yokel RA, O’Callaghan JP. An aluminum-induced increase in GFAP is attenuated by some chelators. Neurotoxicol Teratol. 1998;20:55–60. https://doi.org/10.1016/S0892-0362(97)00069-X.
Kontoghiorghes GJ. Comparative efficacy and toxicity of desferrioxamine, deferiprone and other iron and aluminium chelating drugs. Toxicol Lett. 1995;80:1–18. https://doi.org/10.1016/0378-4274(95)03415-H.
Andersen O. Principles and recent developments in chelation treatment of metal intoxication. Chem Rev. 1999;99:2683–710. https://doi.org/10.1021/cr980453a.
Day JP, Ackrill P. The chemistry of desferrioxamine chelation for aluminum overload in renal dialysis patients. Ther Drug Monit. 1993;15:598–601. https://doi.org/10.1097/00007691-199312000-00026.
Kan WC, Chien CC, Wu CC, Su SB, Hwang JC, Wang HY. Comparison of low-dose deferoxamine versus standard-dose deferoxamine for treatment of aluminium overload among haemodialysis patients. Nephrol Dial Transplant. 2010;25:1604–8. https://doi.org/10.1093/ndt/gfp649.
Savory J, Herman MM, Erasmus RT, Boyd JC, Wills MR. Partial reversal of aluminium-induced neurofibrillary degeneration by desferrioxamine in adult male rabbits. Neuropathol Appl Neurobiol. 1994;20:31–7. https://doi.org/10.1111/j.1365-2990.1994.tb00954.x.
Gómez M, Esparza JL, Domingo JL, Singh PK, Jones MM. Chelation therapy in aluminum-loaded rats: influence of age. Toxicology. 1999;137:161–8. https://doi.org/10.1016/S0300-483X(99)00077-3.
Kruck TP, Cui JG, Percy ME, Lukiw WJ. Molecular shuttle chelation: the use of ascorbate, desferrioxamine and Feralex-G in combination to remove nuclear bound aluminum. Cell Mol Neurobiol. 2004;24:443–59. https://doi.org/10.1023/B:CEMN.0000022773.70722.b2.
Harrison FE. A critical review of vitamin C for the prevention of age-related cognitive decline and alzheimer’s disease. J Alzheimer’s Dis. 2012;29:711–26. https://doi.org/10.3233/JAD-2012-111853.
Yousef MI. Aluminium-induced changes in hemato-biochemical parameters, lipid peroxidation and enzyme activities of male rabbits: protective role of ascorbic acid. Toxicology. 2004;199:47–57. https://doi.org/10.1016/j.tox.2004.02.014.
Nedzvetsky VS, Tuzcu M, Yasar A, Tikhomirov AA, Baydas G. Effects of vitamin e against aluminum neurotoxicity in rats. Biochem (Moscow). 2006;71:239–44. https://doi.org/10.1134/S0006297906030023.
Abubakar MG, Taylor A, Ferns GAA. Regional accumulation of aluminium in the rat brain is affected by dietary vitamin E. J Trace Elem Med Biol. 2004;18:53–9. https://doi.org/10.1016/j.jtemb.2004.02.001.
Lin L, Huang QX, Yang SS, Chu J, Wang JZ, Tian Q. Melatonin in Alzheimer’s disease. Int J Mol Sci. 2013;14:14575–93. https://doi.org/10.3390/ijms140714575.
Albendea CD, Gómez-Trullén EM, Fuentes-Broto L, Miana-Mena FJ, Millán-Plano S, Reyes-Gonzales MC, et al. Melatonin reduces lipid and protein oxidative damage in synaptosomes due to aluminium. J Trace Elem Med Biol. 2007;21:261–8. https://doi.org/10.1016/j.jtemb.2007.04.002.
Jiang T, Zhi XL, Zhang YH, Pan LF, Zhou P. Inhibitory effect of curcumin on the Al(III)-induced Aβ42 aggregation and neurotoxicity in vitro. Biochim Biophys Acta Mol Basis Dis. 2012;1822:1207–15. https://doi.org/10.1016/j.bbadis.2012.04.015.
Sethi P, Jyoti A, Hussain E, Sharma D. Curcumin attenuates aluminium-induced functional neurotoxicity in rats. Pharmacol Biochem Behav. 2009;93:31–9. https://doi.org/10.1016/j.pbb.2009.04.005.
Mahboob A, Farhat SM, Iqbal G, Babar MM, Zaidi NusSS, Nabavi SM, et al. Alpha-lipoic acid-mediated activation of muscarinic receptors improves hippocampus- and amygdala-dependent memory. Brain Res Bull. 2016;122:19–28. https://doi.org/10.1016/j.brainresbull.2016.02.014.
Dos Santos SM, Romeiro CFR, Rodrigues CA, Cerqueira ARL, Monteiro MC. Mitochondrial dysfunction and alpha-lipoic acid: beneficial or harmful in Alzheimer’s disease? Oxid Med Cell Longev. 2019. https://doi.org/10.1155/2019/8409329.
Prakash A, Kumar A. Effect of N-Acetyl cysteine against aluminium-induced cognitive dysfunction and oxidative damage in rats. Basic Clin Pharmacol Toxicol. 2009;105:98–104. https://doi.org/10.1111/j.1742-7843.2009.00404.x.
Belaïd-Nouira Y, Bakhta H, Bouaziz M, Flehi-Slim I, Haouas Z, Ben CH. Study of lipid profile and parieto-temporal lipid peroxidation in AlCl3 mediated neurotoxicity modulatory effect of fenugreek seeds. Lipids Health Dis. 2012;11:1–8. https://doi.org/10.1186/1476-511X-11-16.
Prakash A, Shur B, Kumar A. Naringin protects memory impairment and mitochondrial oxidative damage against aluminum-induced neurotoxicity in rats. Int J Neurosci. 2013;123:636–45. https://doi.org/10.3109/00207454.2013.785542.
Justin-Thenmozhi A, Dhivya Bharathi M, Kiruthika R, Manivasagam T, Borah A, Essa MM. Attenuation of aluminum chloride-induced neuroinflammation and caspase activation through the AKT/GSK-3β pathway by hesperidin in wistar rats. Neurotox Res. 2018;34:463–76. https://doi.org/10.1007/s12640-018-9904-4.
Jun-Qing Y, Bei-Zhong L, Bai-Cheng H, Qi-Qin Z. Protective effects of meloxicam on aluminum overload-induced cerebral damage in mice. Eur J Pharmacol. 2006;547:52–8. https://doi.org/10.1016/j.ejphar.2006.07.031.
Jamil A, Mahboob A, Ahmed T. Ibuprofen targets neuronal pentraxins expresion and improves cognitive function in mouse model of AlCl3-induced neurotoxicity. Exp Ther Med. 2016;11:601–6. https://doi.org/10.3892/etm.2015.2928.
Abd-Elhady RM, Elsheikh AM, Khalifa AE. Anti-Amnestic properties of Ginkgo biloba extract on impaired memory function induced by aluminum in rats. Int J Dev Neurosci. 2013;31:598–607. https://doi.org/10.1016/j.ijdevneu.2013.07.006.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dey, M., Singh, R.K. Neurotoxic effects of aluminium exposure as a potential risk factor for Alzheimer’s disease. Pharmacol. Rep 74, 439–450 (2022). https://doi.org/10.1007/s43440-022-00353-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-022-00353-4