Abstract
Purpose
To define the risk of curve progression of idiopathic scoliosis (IS) to 35°, 40°, 45°, and 50° based on current curve magnitude and Sanders stage for boys and girls, using a large cohort of patients and encounters, to improve granularity and allow more accurate estimations to guide treatment.
Methods
Retrospective analysis of a prospectively collected scoliosis database. Generalized estimation equation logistic regression models estimated probabilities of curve progression to 35°, 40°, 45°, and 50° based on starting curve size and Sanders stage. Probabilities and their 95% confidence intervals were calculated for each combination of variables to each endpoint separately for boys and girls.
Results
A total of 309 patients (80% girls) were included. Starting curve size and Sanders stage were significant predictors for progression in both sexes (all P ≤ 0.04). Higher starting curve sizes and lower Sanders stages were associated with greater odds of progression. Risk of progression was still present even at higher Sanders stages.
Conclusion
IS curves follow a predictable pattern, having more risk for progression when curves are larger and Sanders stages are smaller. Risk of curve progression is a spectrum based on these factors, indicating some risk of progression exists even for many smaller curves with higher Sanders stages. The improved granularity of this analysis compared to prior efforts may be useful for counseling patients about the risks of curve progression to various curve size endpoints and may aid shared decision-making regarding treatments.
Level of evidence or clinical relevance
Level III: retrospective cohort study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The most important factors which predict the risk of idiopathic scoliosis (IS) progression are curve size and remaining growth [1]. The major risk of curve progression happens during peak height velocity of the adolescent growth spurt [2]. Predictors of peak height velocity can include chronologic age, Tanner staging, serial height measurements, hormone levels, and various radiographic markers, with the most accurate being a modification of the Tanner-Whitehouse-III RUS (radius, ulna, short bones) score, also known as the Sanders score (SS) [3].
Sanders et al. assessed the risk of progression of IS to 50° or larger based on the current curve size and SS for girls [4]. They used regression analysis on a longitudinal series of 22 patients who had 161 encounters with radiographs throughout their adolescent growth spurt and created a predictive model for the risk of progression to 50° based on the SS. Despite their important work, the small sample size, exclusion of male patients, and limitation of their cohort to Lenke I and III curves, may make their risk calculator less applicable to the general population. Sitoula et al. performed a similar analysis, but included a cohort of 161 patients, including boys and girls with all Lenke type curves [5]. However, both studies only assessed the risk of progression to 50° since there is general agreement that curves greater than 50° after skeletal maturity are more likely to progress and lead to surgical intervention.
This study seeks to improve on the accuracy of the previous regression analyses of Sanders et al. [4] and Sitoula et al. [5] by including a larger cohort of patients and encounters and to distinguish risk separately for boys and girls. Additionally, because curves less than 50° at skeletal maturity still have some risk of progression [1, 6, 7], this study also seeks to define the risk of curve progression to various curve endpoints 35°, 40°, 45°, and 50°, based on current curve magnitude and Sanders stage, which may have implications for the goals of treatment and protocols for bracing.
Methods
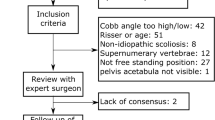
Institutional review board approval was obtained to retrospectively analyze data from a preexisting, prospectively collected, institutional nonoperative IS database. The database included all IS scoliosis patient encounters from a single practice from 2014 to 2021 and had over 3500 encounters at the time of data analysis. Patients included in this analysis had an initial visit with a scoliosis radiograph and a left-hand radiograph, and subsequent follow-up either to skeletal maturity or to documentation of progression to the desired ending curve size. Maturity was accepted when patients reached SS7 when a left-hand radiograph was available or Risser 4 when a hand radiograph was not obtained. Similar to Sanders et al.’s methodology, patients could have several encounters as they naturally progressed through the Sanders stages, and all encounters were eligible for inclusion in our analysis [4]. Separate data sets were created for boys and girls, and separate analyses were performed for progression to 35°, 40°, 45°, and 50°. All curve size, Risser, and SS measurements in the database were performed by a single surgeon. Similar to prior studies, patients were not separated based on treatment, and were braced according to surgeon and patient preference, guided by routine Scoliosis Research Society protocols [8].
Statistical analysis
Summary statistics were performed for variables corresponding to the first patient visit. Continuous variables were summarized as median (range) and mean (standard deviation), while categorical variables were reported as frequency (percentage). Since there were patients with multiple encounters documented, generalized estimation equation logistic regression models were used to estimate probabilities of curve progression to 35°, 40°, 45°, and 50°. Variables used in the models were starting curve size (°) and SS1 to SS8. Odds ratio (OR) estimates and 95% confidence intervals (CI) were calculated from the fitted models and can be interpretated as the multiplicative increase in the odds of curve progression for the given curve size outcome. Probabilities and their 95% CIs were calculated for the different levels of progression for each combination of starting curve size and SS. All analyses were performed separately for boys and girls. P values less than 0.05 were considered as statistically significant, and all statistical tests were two sided. Statistical analyses were performed using R Statistical Software (version 4.0.3; R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 309 patients, 246 girls (80%) and 63 boys (20%), were included in this retrospective cohort study. Patient characteristics from the first visit are summarized in Table 1. The median age for girls was 12.4 years and the median age for boys was 13.5 years. The median follow-up time until skeletal maturity was 23.5 months for girls and 23 months for boys.
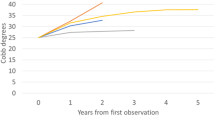
Odds ratios corresponding to curve progression to 35°, 40°, 45°, and 50° are displayed by sex in Table 2. Starting curve size and SS were statistically significant predictors for all progression outcomes in both sexes (all P ≤ 0.04). Higher values of starting curve size were associated with greater odds of curve progression, whereas higher values for SS were associated with lower odds of curve progression. The estimated probabilities of curve progression are shown in Table 3 for girls and Table 4 for boys.
Discussion
Predicting curve progression based on current curve size and remaining growth has been the primary method to guide treatment for patients with IS, with supporting evidence strengthened by the natural history studies of Weinstein et al. and Lonstein et al. [1, 6]. Though they clearly showed an association of curve progression with larger curves and younger patients, determining risk for individual patients has remained difficult due to inconsistent methods for determining the curve acceleration phase (CAP) of growth. Multiple radiographic markers are useful to assess skeletal maturity, including scoring systems from the pelvis and proximal humerus [9, 10]. Sanders et al. demonstrated excellent accuracy of the left-hand X-Ray for determining the CAP compared to chronologic age, the Risser sign, menarche, and various hormones, and since then, the SS has been a commonly used method [3, 4]. Despite Sanders’ important contribution, the predictive ability of the SS was developed using data from a small series of patients, making accurate prediction more difficult. Additionally, his data included only girls with primary thoracic scoliosis (Lenke I and III curves).
Several other studies have expanded on Sanders’ work. Sitoula et al. used similar methodology using a cohort of 116 patients and included boys and girls with all curve types [5]. They confirmed the general pattern of larger curves with lower SS having more risk of progression. However, instead of using regression analysis to predict progression for all categories, they reported curve size/SMS combinations only for categories where they had data, many with small numbers of patients.
Dolan et al. created a predictive calculator based on SS and curve size using 115 untreated patients from the BrAIST study [11, 12]. They also differentiated between lumbar/thoracolumbar curves (Lenke 5) and all other curves that included a thoracic component. They analyzed the risk of progression to 45° for patients in three categories: SMS 1–2, SMS 3, and SMS 4 + . Their conclusions agreed with our study and with previous work, noting a higher risk of progression in less mature patients with larger curves, but did not have granularity based on the specific stage of the SS. Their ability to report on an untreated population is somewhat unique and is a methodology that is difficult to repeat. We did not have the option to include untreated patients in our study. Similar to the Sanders [4] and Sitoula [5] studies, our patients were typically treated according to standard bracing algorithms and did not include any randomization into a nontreatment group. Because we did not withhold treatment, several combinations of curve sizes and SS in our study included only treated or untreated patients. For example, all SS3 patients with 30° curves were treated with braces, while all SS7 patients with 15° curves were observed. Considering the results of the BrAIST study [12] which showed less risk of progression to surgery for patients treated with braces, it is unlikely that a study with untreated controls could be feasible and receive approval from an institutional review board. Additionally, compliance data were not available in our study for patients who were braced. Despite these limitations, we feel that our analysis of all patients regardless of treatment may be more generalizable.
Johnson et al. used the largest series of patients available to predict the chances of nonoperative treatment success [13]. They followed 609 boys and girls with scoliosis and defined success as reaching skeletal maturity with a curve < 50°. They divided their categories into skeletal immaturity (SMS 1–2), peak height velocity (SMS 3–4), late adolescence (SMS 5–6), and early maturity (SMS 7–8). Their findings also corroborated the general pattern of older patients with smaller curves having a greater chance of successful nonoperative management. Our study differs from Johnson, et al. by including separate analyses of the results for boys and girls and by defining endpoints other than 50°. Unlike their study, our study did not consider other factors which might contribute to curve progression, such as curve classifications or body mass index.
Our study agrees with these previous efforts, and again demonstrates the clear pattern of an increased risk of curve progression for less mature patients with larger curves. We were able to expand on prior efforts by including predictive models for multiple endpoints (35°, 40°, 45°, and 50°) and by including separate models for boys and girls. Despite these advances, our study still has some limitations. Though we included larger cohorts of encounters for boys and girls, we still did not have enough patients in each category to completely minimize the 95% CI. In his original study, Sanders predicted that 36 patients would need to be followed through maturity for each category to decrease all 95% CI to ± 10%, which would require more than 2000 encounters for the table with a 50° endpoint [4]. This is likely beyond the scope of even multicenter efforts. Because many of the predicted risks for progression continue to have wide 95% CI, it is important that this information is shared transparently with patients and their families when discussing treatment options. All measurements were done by a single surgeon, so there was no analysis of intra-observer error. Although Cobb angles and SS both have some inherent measurement error, it is unlikely that some variability would change the overall pattern seen in the regression analysis that reinforces the findings seen in prior studies.
We followed patients through their CAP until they reached Risser 4 or SS7, but did not require minimum 2-year follow-up. We feel this was practical in most cases, as patients who progressed significantly in a shorter time period would be valuable to include. Similarly, patients with smaller curves who reach skeletal maturity were often not be required to follow-up for additional radiographs. For example, a patient followed for 12 months with a nonprogressive 15° curve who achieved Risser 4, Sanders 7 status would likely not return for another appointment, but it would still be reasonable to project that they would never progress to 35° and include them in the data. If followed long after skeletal maturity, some patients with larger curves might have progressed further. Grothaus et al. showed 58% of the patients who were 40° or larger at SS7 progressed to at least 50° [7]. Therefore, our limited follow up could have underestimated the actual risk of progression for some categories. We were not able to separate patients based on treatment, curve type, or body mass index because recommendations for bracing were based on traditional indications, so most patients with significant curves and growth remaining were braced. Our institution also does not routinely employ temperature sensors in braces, so our results can only be interpreted as the risk of progression regardless of treatment or compliance.
We used the original Sanders classification, but more recently subclassifications have been proposed including Sanders 3A, 3B, and 7b categories [14, 15]. Our data did not account for these subclassifications, which might provide even more granularity for prediction of curve progression. Our study evaluated progression based only on curve size and SS. A more accurate model might be achieved by including other factors, such as treatment, the Risser sign, height velocity, curve classification, body mass index, and menarche (girls). Finally, because idiopathic scoliosis likely represents a polygenic disorder, our study has the same limitation of multiple previous studies that have attempted to predict curve progression based on phenotypic markers. Predicting curve progression for any individual patient may not correspond to the means and confidence intervals predicted by regression analysis, and so these models should be used with appropriate caution.
Adolescent IS curves follow a predictable pattern, having more risk for progression when curves are larger, and the Sanders stage is smaller. Considering curve progression risk as a spectrum based on these factors indicates some small risk of progression exists even for many smaller curves with higher SS. This analysis may be useful for counseling patients about the risks of curve progression to various curve size endpoints and may aid shared decision-making regarding treatments.
Data availability
The data that support the findings of this study are available upon reasonable request from the authors.
References
Lonstein JE, Carlson JM (1984) The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am 66:1061–1071
Little DG, Song KM, Katz D et al (2000) Relationship of peak height velocity to other maturity indicators in idiopathic scoliosis in girls. J Bone Joint Surg Am 82:685–693. https://doi.org/10.2106/00004623-200005000-00009
Sanders JO, Browne RH, McConnell SJ et al (2007) Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Joint Surg Am 89:64–73. https://doi.org/10.2106/JBJS.F.00067
Sanders JO, Khoury JG, Kishan S et al (2008) Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am 90:540–553. https://doi.org/10.2106/JBJS.G.00004
Sitoula P, Verma K, Holmes L Jr et al (2015) Prediction of curve progression in idiopathic scoliosis: validation of the sanders skeletal maturity staging system. Spine (Phila Pa 1976) 40:1006–1013. https://doi.org/10.1097/BRS.0000000000000952
Weinstein SL, Ponseti IV (1983) Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 65:447–455
Grothaus O, Molina D, Jacobs C et al (2020) Is it growth or natural history? Increasing spinal deformity after sanders stage 7 in females with AIS. J Pediatr Orthop 40:e176–e181. https://doi.org/10.1097/BPO.0000000000001415
Richards BS, Bernstein RM, D’Amato CR et al (2005) Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS committee on bracing and nonoperative management. Spine (Phila Pa 1976) 30:2068–2077. https://doi.org/10.1097/01.brs.0000178819.90239.d0
Risser JC (2010) The classic: The iliac apophysis: an invaluable sign in the management of scoliosis. 1958. Clin Orthop Relat Res 468:643–653. https://doi.org/10.1007/s11999-009-1096-z
Li DT, Linderman GC, Cui JJ et al (2019) The proximal humeral ossification system improves assessment of maturity in patients with scoliosis. J Bone Joint Surg Am 101:1868–1874. https://doi.org/10.2106/JBJS.19.00296
Dolan LA, Weinstein SL, Abel MF et al (2019) Bracing in adolescent idiopathic scoliosis trial (BrAIST): development and validation of a prognostic model in untreated adolescent idiopathic scoliosis using the simplified skeletal maturity system. Spine Deform 7:890-898.e4. https://doi.org/10.1016/j.jspd.2019.01.011
Weinstein SL, Dolan LA, Wright JG et al (2013) Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 369:1512–1521. https://doi.org/10.1056/NEJMoa1307337
Johnson MA, Flynn JM, Anari JB et al (2021) Risk of scoliosis progression in nonoperatively treated adolescent idiopathic scoliosis based on skeletal maturity. J Pediatr Orthop 41:543–548. https://doi.org/10.1097/BPO.0000000000001929
Sanders JO, Howell J, Qiu X (2011) Comparison of the Paley method using chronological age with use of skeletal maturity for predicting mature limb length in children. J Bone Joint Surg Am 93:1051–1056. https://doi.org/10.2106/JBJS.J.00384
Cheung PWH, Cheung JPY (2021) Sanders stage 7b: using the appearance of the ulnar physis improves decision-making for brace weaning in patients with adolescent idiopathic scoliosis. Bone Joint J 10:141–147. https://doi.org/10.1302/0301-620X.103B1.BJJ-2020-1240.R1
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Conceptualization: Kevin M. Neal. Methodology: Kevin M. Neal, Gary M. Kiebzak. Formal analysis and investigation: Kevin M. Neal, Emily C. Craver, Julia E. Crook. Writing–original draft preparation: Kevin M. Neal. Writing—review and editing: Kevin M. Neal, Melanie Boeyer, Emily C. Craver, Julia E. Crook, Gary M. Kiebzak. Resources: Gary M. Kiebzak. Supervision: Kevin M. Neal. All authors have read and approved the final manuscript. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have none to declare. Financial interests: Kevin M. Neal receives royalties and consulting fees, and stock less than $5,000 from Company A. Melanie Boeyer receives research support unrelated to this work from Zimmer Biomet and ZimVie, and consulting fees less than $5,000 per year from ZimVie. The remaining authors have no relevant financial interests to disclose. Non-financial interests: Kevin M. Neal is on committees for AAOS, SRS, and POSNA. Dr. Neal also serves as a journal reviewer for Journal of Pediatric Orthopaedics. The remaining authors have no relevant non-financial interests to disclose.
Ethical approval
This research study was conducted retrospectively from data obtained for clinical purposes. The Nemours Children’s Health Institutional Review Board determined our study did not need ethical approval.
Informed consent
As part of the Nemours Children’s Health IRB exemption, the requirement for obtaining informed consent was waived based on the applicable federal regulation.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Neal, K.M., Boeyer, M., Craver, E.C. et al. Improving prediction of progression of idiopathic scoliosis based on curve size and skeletal maturity. Spine Deform (2024). https://doi.org/10.1007/s43390-024-00939-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43390-024-00939-3