Abstract
Introduction
Asymmetry in pedicle anatomy is most distinctly noted around the apex of the curve. The correlation of pedicle dysmorphia with apical vertebral rotation (AVR) and coronal Cobb angle (CCA) has not been studied.
Objective
To establish whether pedicle dysmorphism is linked to curve magnitude CCA and the AVR in adolescent idiopathic scoliosis (AIS).
Methodology
Preoperative plain whole spine standing radiographs and non-contrast computed tomography (CT) scans of 25 AIS patients that were operated at a single centre from 2013 to 2019 were retrospectively reviewed by 3 independent co-investigators. CCA was noted on the standing radiograph, whereas the AVR was measured on the axial cuts of CT scan. Pedicle morphometric measurements were performed for apical and periapical pedicles. These included apical vertebra (when present), 2 vertebrae above (U1 and U2) and below (B1 and B2) the apex vertebra/disc. The pedicle morphometric measurements were performed on CT scans. We assessed the transverse pedicle diameter, transverse cancellous channel diameter, sagittal pedicle diameter, pedicle length and pedicle axis length. Correlation tests between various pedicle morphometric measurements, AVR and the curve magnitude (Cobb angle) was performed by the Pearson correlation test.
Results
The apex of the major curve was in the thoracic spine in 20 patients, thoracolumbar in three patients and in the lumbar spine in two patients. The mean Cobb angle was 61.5 ± 9.3° and the mean AVR was 28.4 ± 17.8°. A positive correlation was noted with the AVR for U1 concave pedicle length (r = 0.45, p = 0.03), pedicle axis length of the U2 concave pedicle (r = 0.6, p = 0.04), transverse pedicle diameter of the convex apical vertebrae (r = 0.82, p = 0.00009) and the convex apical transverse pedicle diameter (r = 0.80, p = 0.002). A negative correlation with the AVR was noted for U2 convex pedicle length (r = − 0.51, p = 0009), transverse cancellous channel diameter of the U2 concave pedicle (r = − 0.42, p = 0.04) and apical concave pedicle (r = − 0.78, p = 0.002) and the sagittal pedicle diameter for the convex pedicle of U2 (r = − 0.45, p = 0.03) and apex(r = − 0.59, p = 0.04). The Cobb angle did not show a significant correlation with any of the pedicle measurements at any of the levels on the convex and the concave sides.
Conclusion
Pedicle asymmetry and dysmorphism demonstrate a morphometric association with the apical vertebral rotation than the curve magnitude. The pedicle length and the pedicle axis length increase on the concave apical and periapical region with increase in AVR. The transverse cancellous channel diameter significantly decreases on the concave apical region with the increase in AVR. The sagittal pedicle diameter decreases on the convex side with the increase in AVR.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is associated with morbidity not only due to back pain and cardiopulmonary issues but also the cosmetic deformity with the associated psychosocial problems in adolescents [1]. The use of pedicle screw constructs for correction of these deformities is now considered standard [2, 3]. However, pedicle screw fixation is limited by the anatomy of the pedicle. Diameter, trajectory and length of pedicle can vary significantly from the normal [4]. It has been established that asymmetry exists between concave and convex pedicles of structural curves in AIS [5]. These differences are more pronounced at the apex and the periapical region of the curve [5]. However, it is not clear how the pedicle dysmorphism and asymmetry correlate with Cobb angle and apical vertebral rotation which are both considered markers of the 3-dimensional deformity. Though pedicle types have been described based on the differences in the cancellous channels, there is no study that quantifies the morphology of the apical pedicles. In the present study, we aim to correlate the coronal Cobb angle and the apical vertebral rotation with various pedicle measurements made on both the convex and the concave side in apical and periapical region in patients with AIS.
Materials and methods
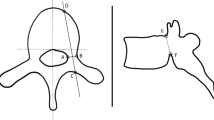
A total of 25 AIS patients that had been operated at our centre from 2013 to 2019 were included. The patients with deformity due to other causes or with incomplete radiological records were excluded. All patients underwent a posterior spinal fusion with pedicle screw constructs and preoperative low-dose CT scans were obtained in these patients for preoperative planning and pedicle screws sizing. The scans were done in supine position from T1 to S1 (Somatom Definition FLASH, Siemens Healthcare, Forchheim, Germany). The highest estimated radiation dose for the scans in the present study was 2.4–3.6 mSV. For each patient, age, gender, apex of the deformity, coronal Cobb angle, and apical vertebral rotation were recorded. Pedicle morphology was assessed by measuring transverse outer cortical pedicle diameter, transverse cancellous channel diameter, sagittal pedicle diameter, pedicle length and pedicle axis length. The parameters were recorded at the apical vertebra (when present) and 2 vertebrae above (apex-2 = U1 and apex-1 = U2) and 2 vertebrae below (apex + 1 = B1 and apex + 2 = B2) on both the convex and the concave sides. The coronal Cobb was measured on standing anteroposterior radiographs between the two end vertebrae. The vertebral rotation was measured by the Aaro–Dahlborn method on computed tomography scan [6]. Transverse outer cortical pedicle diameter, transverse cancellous channel diameter, sagittal pedicle diameter, pedicle length and pedicle axis length or chord length were measured as described previously by Vaccaro et al. and Liljenqvist et al. [5, 7, 8]. Representative images for measurements are presented in Fig. 1. All measurements were performed by three independent co-investigators and average of the three values was used.
SPSS 20 software was used to perform statistical analysis. Mean and standard deviation were calculated for parameters following normal distribution, whilst the other was described using median and interquartile range. Inter-class correlation (ICC) coefficient was used to measure reliability across radiological measurements. A Pearson correlation coefficient (r) was calculated for Cobb angle and AVR with various pedicle morphometric measurements for the apical/peri-apical pedicles. A p value < 0.05 was considered significant. The value of r ≥ 0.7 was considered a strong correlation, 0.7 > r ≥ 0.3 was considered a moderate correlation and r < 0.3 was considered a weak correlation [9]. The interclass correlation coefficient (ICC) was used to measure reliability across radiographic measurements. ICC > 0.9 was considered excellent, 0.9 > ICC > 0.75 was considered good [10].
Results
A total of 25 patients were analysed in this study. These included 23 females and 2 males. The mean age was 14.4 ± 2.1 years. The apex of major curve was T9–T10 disc in 4 cases, T8 in 3 cases and T7, T7–T8, T8–T9, T9, T10–T11, T12 in 2 cases each. One case each had an apex at T5–T6, T12–L1, L2, L2–L3 levels. The apex of the major curve was in the thoracic spine in 20 patients, thoracolumbar in 3 patients and in the lumbar spine in 2 patients. The mean Cobb angle was 61.5 ± 9.3 (CI95% -57.8–65.1). The mean apical vertebral rotation was 28.4 ± 17.8 (CI 95% 22.7–34.1). The interclass correlation coefficient for all radiographic measurements showed good to excellent reliability (0.80–0.96).
The mean measurements along with standard deviation for transverse outer cortical pedicle diameter, sagittal pedicle diameter, pedicle length and pedicle axis length for U1, U2, apex B1 and B2 pedicles are represented in Table 1.
The Pearson correlation coefficient and the p values for the comparison of Cobb angle and apical vertebral rotation with various pedicle measurements are represented in Table 2. The Cobb angle did not show a significant correlation with any of the pedicle measurements in any of the apical and the periapical vertebrae. The pedicle length showed a significant positive correlation at U1 concave pedicle (r = 0.45 p = 0.03) and a negative correlation at U2 convex pedicle (r = − 0.51, p = 0009) with apical vertebral rotation (AVR). The pedicle axis length showed a positive correlation with AVR at U2 concave pedicle (r = 0.6, p = 0.04). The transverse pedicle diameter significantly correlated with AVR at convex apical vertebrae (r = 0.82, p = 0.00009). The transverse cancellous channel diameter showed a significant negative correlation at U2 concave pedicle (r = − 0.42, p = 0.04) and apical concave pedicle (r = − 0.78, p = 0.002) and positive correlation at convex apex pedicle (r = 0.80, p = 0.002) with AVR. A representative case is presented in Fig. 2. A diagrammatic representation of the statically significant results is presented in Fig. 3. The sagittal pedicle diameter showed a significant negative correlation with AVR at convex pedicle of U2 (r = − 0.45, p = 0.03) and apex (r = − 0.59, p = 0.04). The AVR did not correlate significantly with any pedicle measurements for periapical vertebrae below the apex (Table 2).
Discussion
An increased acceptance of the pedicle screw-based constructs has led to an increased popularity of the posterior approach for the treatment of AIS. The three-dimensional control afforded by the pedicle screws has provided a superior biomechanical control and led to more powerful corrections. However, placement of the pedicle screws can be difficult in dysplastic pedicles. Liljenqvist et al. in their MRI-based study on patients with AIS were the first to establish that distinctive morphology in the form of thinner pedicles in the concavity along with shifting of the dural sac to the concavity occurred in the apical region and it normalised significantly near the neutral vertebrae [5]. A CT-based study compared AIS patients with healthy controls and noted a significantly narrower pedicle on the concave side. They also noted that the highest prevalence of dysplastic pedicles was at the apex of the structural curve [4]. Davis et al. reported a CT-based assessment of pedicles in AIS patients, noting that the apical concave pedicles had a smaller height and width compared with the convex pedicles. They also noted a more ‘acute trajectory’ of the convex pedicles in comparison to the concave pedicles [11]. The dysmorphic pedicles in our study are noted to be more commonly located in the thoracic spine, in the concavity, at or near the apex of the curve. This could be linked to the incidence of misplaced screws being nearly three times higher in these pedicles [12]. In an MRI-based study, the progressive changes in pedicle parameters were compared in AIS patients with non-scoliotic patients. It was seen that the dural sac was more closely approximated to the medial wall of the pedicle on the concave side in the AIS group. The chord lengths and the transverse pedicle angle increased more on the concave side in the AIS group creating further asymmetries. This study emphasised that asymmetrical growth of posterior vertebral elements occurs in AIS [13].
Besides the differences in the pedicle morphology, the vertebral body morphology has also been compared between AIS patients and controls. It was noted that patients with AIS have significant differences in apical vertebral rotation, axial vertebral body asymmetry and frontal vertebral body rotation compared to controls which was most pronounced at the apical vertebrae [14]. Whilst the occurrence of pedicle asymmetry and dysmorphism has been established, various studies as discussed above the factors associated with or leading to this are not yet established. Hence, in the present study, we tried to investigate the correlation of Cobb angle and apical vertebral rotation with various pedicular parameters in the apical and periapical region of major curve in patients with AIS.
Coronal Cobb angle of the major structural curve in AIS is a radiographic marker of the curve severity. Larger curves are associated with larger Cobb angles, longer surgical duration, higher blood loss and increased hospital costs [15]. However, there are no studies which have correlated Cobb angle with pedicle dysmorphism parameters. Our study was designed to compare the correlation of Cobb angle with various pedicular parameters of concave and convex pedicles in apical and periapical region. We did not find any significant correlation between the Cobb angle and the various pedicle parameters. Whilst increasing Cobb angle denotes increasing severity of the curve in AIS, it does not correlate with abnormal pedicle morphology.
Scoliotic deformities being three-dimensional deformities are associated with significant vertebral rotation besides coronal and sagittal plane deformities. The apical vertebra is often the most rotated vertebra also for the majority of major curves in AIS [16]. The AVR significantly correlated with various pedicle parameters in the apical and the periapical region in the present study indicating that the pedicle dysmorphism may be more a function of vertebral rotation than the magnitude of the curve. In the present study, we found that pedicle length and pedicle axis length significantly increased on the concave side with increase in in AVR. It was also noticed that the pedicle length showed a negative correlation with periapical convex pedicle (U2) with respect to AVR.
The narrow diameter of transverse cancellous channels in patients with AIS especially on the concave side has been well documented in various studies [8, 12, 17]. It has been seen that the abnormal pedicles with narrow cancellous channel are significantly more in the concavity, the apical and the periapical region [12]. In the present study, we noticed the cancellous channel diameter at concave apical and upper periapical vertebrae (U2), which showed a significant moderate negative correlation with the AVR. It indicates that the cancellous channel becomes narrower as the AVR increases in the apical and the periapical region. Another interesting finding in the present study was that sagittal pedicle diameter correlated negatively at the convex upper periapical (U2) and apical region with AVR. The above findings indicate that the caution must be exercised during pedicle screw insertion on the apical and the periapical concave side in cases of high apical vertebral rotation due to increased risk of medial and lateral breach. Similar caution must be exercised on the convex apical and the periapical region in the cranio-caudal direction in case of high AVR due to decreased sagittal pedicle diameter.
Small sample size, heterogeneity of the patient population and data acquisition from a single centre are some of the limitations of the present study. However, this is the first study that has studied the correlation of coronal Cobb angle and AVR with the various pedicle measurements in the periapical region of the major curve. Our study shows that the AVR correlates well with various pedicle measurements and may be one of the main drivers of pedicle dysmorphism in AIS.
Conclusion
Pedicle asymmetry and dysmorphism are better linked to the apical vertebral rotation than to the curve magnitude. The pedicle length and the pedicle axis length increase on the concave apical and periapical region with the increase in AVR. The transverse cancellous channel diameter significantly decreases on the concave apical region with the increase in AVR. The sagittal pedicle diameter decreases on the convex side with the increase in AVR. Further studies in different patient populations and larger sample size are required to validate these results.
Data availability
Available.
Code availability
Not applicable.
References
Weiss HR, Karavidas N, Moramarco M, Moramarco K (2016) Long-term effects of untreated adolescent idiopathic scoliosis: a review of the literature. Asian Spine J 10(6):1163–1169. https://doi.org/10.4184/asj.2016.10.6.1163
Chen Z, Rong L (2016) Comparison of combined anterior–posterior approach versus posterior-only approach in treating adolescent idiopathic scoliosis: a meta-analysis. Eur Spine J 25(2):363–371. https://doi.org/10.1007/s00586-015-3968-0
Shufflebarger HL, Geck MJ, Clark CE (2004) The posterior approach for lumbar and thoracolumbar adolescent idiopathic scoliosis: posterior shortening and pedicle screws. Spine 29(3):269–276. https://doi.org/10.1097/01.BRS.0000109881.63411.48
Gao B, Gao W, Chen C et al (2017) What is the difference in morphologic features of the thoracic pedicle between patients with adolescent idiopathic scoliosis and healthy subjects? A CT-based case-control study. Clin Orthop 475(11):2765–2774. https://doi.org/10.1007/s11999-017-5448-9
Liljenqvist UR, Allkemper T, Hackenberg L, Link TM, Steinbeck J, Halm HFH (2002) Analysis of vertebral morphology in idiopathic scoliosis with use of magnetic resonance imaging and multiplanar reconstruction. J Bone Jt Surg Am 84(3):359–368. https://doi.org/10.2106/00004623-200203000-00005
Aaro S, Dahlborn M, Svensson L (1978) Estimation of vertebral rotation in structural scoliosis by computer tomography. Acta Radiol Diagn (Stockh) 19(6):990–992. https://doi.org/10.1177/028418517801900614
Vaccaro AR, Rizzolo SJ, Allardyce TJ et al (1995) Placement of pedicle screws in the thoracic spine. Part I: morphometric analysis of the thoracic vertebrae. J Bone Jt Surg Am 77(8):1193–1199. https://doi.org/10.2106/00004623-199508000-00008
Akazawa T, Kotani T, Sakuma T, Minami S, Tsukamoto S, Ishige M (2015) Evaluation of pedicle screw placement by pedicle channel grade in adolescent idiopathic scoliosis: should we challenge narrow pedicles? J Orthop Sci Off J Jpn Orthop Assoc 20(5):818–822. https://doi.org/10.1007/s00776-015-0746-0
Akoglu H (2018) User’s guide to correlation coefficients. Turk J Emerg Med 18(3):91–93. https://doi.org/10.1016/j.tjem.2018.08.001
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Davis CM, Grant CA, Pearcy MJ et al (2017) Is there asymmetry between the concave and convex pedicles in adolescent idiopathic scoliosis? A CT investigation. Clin Orthop 475(3):884–893. https://doi.org/10.1007/s11999-016-5188-2
Sarwahi V, Sugarman EP, Wollowick AL, Amaral TD, Lo Y, Thornhill B (2014) Prevalence, distribution, and surgical relevance of abnormal pedicles in spines with adolescent idiopathic scoliosis vs. no deformity: a CT-based study. JBJS 96(11):e92. https://doi.org/10.2106/JBJS.M.01058
Davis CM, Grant CA, Izatt MT et al (2020) Characterization of progressive changes in pedicle morphometry and neurovascular anatomy during growth in adolescent idiopathic scoliosis versus adolescents without scoliosis. Spine Deform 8(6):1193–1204. https://doi.org/10.1007/s43390-020-00160-y
Vavruch L, Forsberg D, Dahlström N, Tropp H (2018) Vertebral axial asymmetry in adolescent idiopathic scoliosis. Spine Deform 6(2):112-120.e1. https://doi.org/10.1016/j.jspd.2017.09.001
Tarrant RC, Queally JM, O’Loughlin PF, Sheeran P, Moore DP, Kiely PJ (2016) Preoperative curves of greater magnitude (>70°) in adolescent idiopathic scoliosis are associated with increased surgical complexity, higher cost of surgical treatment and a delayed return to function. Ir J Med Sci 1971 185(2):463–471. https://doi.org/10.1007/s11845-015-1391-5
Labaki C, Otayek J, Massaad A et al (2019) Is the apical vertebra the most rotated vertebra in the scoliotic curve? J Neurosurg Spine 31(6):873–879. https://doi.org/10.3171/2019.6.SPINE19203
Watanabe K, Lenke LG, Matsumoto M et al (2010) A novel pedicle channel classification describing osseous anatomy: how many thoracic scoliotic pedicles have cancellous channels? Spine 35(20):1836–1842. https://doi.org/10.1097/BRS.0b013e3181d3cfde
Funding
There is no funding source for this publication/study.
Author information
Authors and Affiliations
Contributions
Concept and design: BG, TB, NM, JM. Data acquisition: BG, TB, JM. Data analysis: BG, TB, NM. Manuscript preparation: TB, JM. Manuscript editing: BG, TB, NM, JM. Approval of final version of manuscript: BG, TB, NM, JM.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Approval was obtained from the ethics committee of All India Institute of Medical Sciences, New Delhi. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garg, B., Bansal, T., Mehta, N. et al. Is the morphology of the apical pedicles influenced by apical rotation or the coronal curve magnitude in adolescent idiopathic scoliosis?: a radiographic assessment. Spine Deform 12, 341–348 (2024). https://doi.org/10.1007/s43390-023-00773-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00773-z