Abstract
Objective
Adjacent segment disease, junctional kyphosis/failure and pseudarthrosis can negatively impact the mid to long-term outcome in spinal deformity surgery. These complications might be influenced by upper instrumented vertebra (UIV) fixation techniques. In this study we analyze key biomechanical properties of three different UIV fixation techniques and define their ideal clinical use based on patient-specific risk profiles using a finite element analysis (FEA) model.
Methods
A T9-pelvis posterior instrumented spinal fusion was assumed. Three different FEA models were created based on the UIV fixation technique: T9 pedicle screws (PS); T9 cortical bone screws (CBS); T9 transverse process hooks (TPH). The three FEA models consisted of T8–T10 bone and ligamentous anatomy derived from a CT scan of a healthy patient as well as spinal implants consisting of either pedicle screws, cortical bone screws or transverse process hooks as well as cobalt chromium rods. The FEA models were constrained at T10, axial load as assumed for a healthy 80 kg male during flexion, extension and lateral bending were applied. As surrogate markers for risk of proximal junctional kyphosis, proximal junctional failure, adjacent segment disease and pseudarthrosis the following biomechanical parameters were calculated: UIV range of motion (ROM); intradiscal stress at UIV/UIV + 1; UIV intravertebral stress and screw pull out forces. One-way ANOVA analyses have been performed to compare biomechanical outcome parameters between the three construct variants under investigation.
Results
UIV-ROM was restricted during flexion/extension/lateral bending by: PS: 73%/80%/86%, CBS: 71%/81%/85% and TPH: 62%/76%/85%. Average intradiscal stress at UIV/UIV + 1 during flexion/extension/lateral bending was (Mega Pascal, MPa): PS 0.42/0.44/0.38, CBS 0.49/0.4/0.44, TPH 0.66/0.51/0.58; average intravertebral stress of the UIV superior endplate during flexion/extension/lateral bending was (MPa): PS 2.23/2.12/2.21, CBS 1.87/1.98/1.8, TPH 1.67/0.98/1.53. Screw pull-out forces (N) at UIV during flexion/extension/lateral bending were: PS 476/320/375, CBS 444/245/308. Statistically significant differences were found for intradiscal stress as well as vertebral body average stress (p = 0.02 and p = 0.02).
Conclusion
Different UIV fixation techniques carry different biomechanical properties. Pedicle screw fixation is the most rigid, leading to the highest UIV stress and UIV screw pull out forces. Cortical bones screw fixation is similarly rigid; however, UIV stress and UIV screw pull out is significantly lower. Transverse process hook fixation is the least rigid, with the lowest UIV stress, however highest intradiscal stress at UIV/UIV + 1. Thus, these biomechanical differences may help select optimal UIV fixation techniques according to patient specific risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mid and long-term outcomes following spinal deformity surgery can be negatively influenced by possible secondary alterations at the transition between fused and unfused spine. These secondary changes are on a clinical spectrum ranging from more benign degenerative changes of discs and facet joints, termed adjacent segment disease (ASD) to structural failure patterns in terms of junctional kyphosis (JK) or junctional failure (JF). A variety of patient specific factors are known to influence the incidence of JK and JF, mainly bone quality, patient age and body weight [1, 2]. Further surgery-specific factors such as length of fusion, choice of upper and lower instrumented vertebra (UIV and LIV) and postoperative alignment influence the incidence of JK/JF [3]. Previous clinical research suggests that less rigid UIV-fixation, such as transverse process hooks (TPH) might decrease the risk of JK/JF in patients who are not at high risk for pseudarthrosis [4]. Lately another fixation technique has been introduced in the lumbar spine, the so-called cortical bone screw (CBS) trajectory, which comprises of an upward and outwardly direct pedicle screw. This technique requires less soft tissue dissection to expose the entry point and engages more of the corresponding lamina, which is rich in dense cortical bone. The choice of UIV fixation technique has a profound impact on the biomechanical characteristics of the junctional area with resulting clinical implications.
This study investigates the properties of three different UIV fixation devices: conventional pedicle screw fixation (PS), CBS and TPH. CBS is a novel technique which we compare to the two established techniques, PS and TPH. The biomechanical profile of each device is correlated with possible clinical correlations to facilitate surgical decision making.
Methods
The CT scan of a 20-year-old male without pathologic structural changes of the entire spine and no known disease of bone metabolism was used as a template for this study. Thin sectioned (0.625 mm) DICOM files were used to extract the spinal segment T8–T10 and then converted to a “computer-aided design” (CAD) model, which then was used for the FEA Simulation[5]. Three different surgical scenarios have been modelled, differing by the mode of UIV fixation: variant 1: UIV, UIV-1 PS, variant 2: UIV CBS and UIV-1 PS, variant 3 UIV TPH and UIV-1 PS; Virtual placement of hardware was performed using 3D surface rendered views in correlation with cross sectional views according to common surgical practice [6,7,8], see Fig. 1.
Pedicle screws as well as TPH were titanium based and dimensions chosen according to local anatomy, while rods were cobalt chromium based [9].
Each vertebra consisted of a cancellous core model using 3D tetra element surrounded by a cortical shell which is modelled using 2D elements. The intervertebral disc was modelled as nucleus pulposus and annulus fibrosus as a hyper-elastic material using the Mooney–Rivlin material model [10]. Facet joints of each level were modeled as a tetra element and major ligaments (anterior longitudinal ligament, ALL, interspinous ligament, ISL and supraspinous ligament, SSL) as shell elements [11]. Figure 2 outlines biomechanical material properties of all simulated implant and anatomical elements.
Pedicle screw placement was performed on the 3D models using a conventional trajectory, as described in the literature [7, 12]. Cortical bone screw placement has been performed as described by Hosogane et al. [8]. Friction coefficient between the bone and the pedicle screw has been considered according to previous studies [13].
Considering an estimated total body weight of 75 kg, in which 65% constitutes to upper body weight, a load of 480 Newton (N) was applied on the FEA models vertically. Moments required for flexion, extension and lateral bending were derived using an intact model based on the maximum range of motion (ROM) of T9, which was then applied to the instrumented FEA models. All degrees of freedom were constrained at the T10 endplate. Each FEA model of the corresponding variant under investigation has been subjected to flexion, extension and lateral bending loads. During each simulation the following parameters have been calculated: ROM T9, intradiscal von Mises stress UIV/UIV + 1, intravertebral von Mises stress UIV, implant associated von Mises stress, screw pull out force.
Biomechanical outcome parameters were compared between the three variant models using one-way ANOVA analysis (Graphpad Software, La Jolla, San Diego, USA).
Results
Rigidity of a fixation technique was investigated by comparing the UIV-ROM of each variant to a native, intact FEA model of T8–T10. Table 1 outlines ROM restrictions under the above outlined loading conditions, showing that TPH-variant, particularly during flexion, allowed for the most residual movement when compared to the other two variants.
PS and CBS variants showed comparable reduction in UIV-ROM in relation to the TPH-variant of 81%, 83% and 89% and 76%, 80%, and 98% (flexion, extension, and lateral bending) for PS and CBS, respectively.
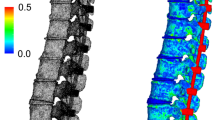
Intradiscal pressures at UIV + 1/UIV (measured in mega Pascal, MPa) were calculated after loading conditions were applied and are outlined in Table 1. Figure 3 shows mid discal axial sections (UIV/UIV + 1) demonstrating von Mises stress zones for each variant, while Table 1 shows average von Mises stress values calculated for a single mid disc axial section. While PS and CBS resulted in comparable mean stress values (relative values for PS and CBS during flexion/extension/lateral bending: 100%/100%/86% and 117%/91%/100%), TPH showed significantly higher stresses 157%/116%/131%).
Intravertebral von Mises stress at the UIV under loading conditions are illustrated in Figs. 4 and 5. In each FEA simulation the UIV was divided into a superior and inferior half in a sagittal plane. Average von Mises stress values under loading conditions are detailed in Table 1. Except for extension loading in variant 3, average stresses were higher in the superior half of the vertebral body for all variants. Upon flexion the highest average stress was encountered in the PS variant (2.23 MPa versus 1.87 and 1.67 MPa, for PS, CBS and TPH, respectively). The PS variant also had the highest average stress in extension (2.12 MPa versus 1.98 and 0.98 MPa, respectively) and in lateral bending (2.21 MPa versus 1.8 MPa versus 1.53 MPa). Table 1 also outlines maximal von Mises stress values for each variant and loading condition. Correlating these results with Fig. 4 show that the engagement site of the TPH are high stress areas (5.06 MPa, 5.41 MPa, and 5.72 MPa during flexion, extension and lateral bending, respectively). Moreover, the cortical area directly caudal to the entry point of the cortical bone screw trajectory is subject to higher stresses (flexion, extension and lateral bending: 3.29 MPa, 2.68 MPa and 2.95 MPa respectively). Actual implant related stresses are outlined in Fig. 6, showing that high stress zones are located at the UIV screw head/ shaft interface in case of PS and CBS variants, particularly upon flexion. In the case of CBS, an additional high stress zone is located in the rods between UIV and UIV-1 and in the TPH variant high stress zones are located in the actual transverse process hooks (Table 1). Lastly screw pull out forces were calculated for each variant upon loading with PS having greater pull out forces in flexion, extension, and lateral bending when compared to CBS (Table 1). A statistical comparison of outcome parameter has been performed and is outlined in Fig. 7 and Table 2. Statistical significance was found for vertebral body stress values (MPa) as well as intradiscal stress (MPa). For the remaining parameters the sample size in terms of measurements has not been sufficient.
Discussion
The results of this biomechanical study indicate that the three different UIV fixation techniques (PS, CBS, TPH) have different biomechanical properties, potentially translating to a different risk profile for pseudarthrosis rate, ASD, and JK/JF. We find that while PS induces high UIV stress, it also is the most rigid mode of fixation. CBS is similarly rigid as PS, however UIV stress as well as screw pull out forces are lower when compared to CPS. TPH fixation showed the least rigid fixation, the lowest UIV stress however UIV/UIV + 1 intradiscal stress was highest. In a clinical setting the choice of UIV fixation technique based on these biomechanical results should be influenced by patient specific factors.
Different approaches have been proposed in the past to improve the biomechanical profile at the junctional area of a fusion, such as polyester or mersilene tethering. As shown by Bess et al. [14] posterior polyester tethers at UIV to UIV + 1,2,3 create a gradual increase in ROM at the junctional zone as well as decrease of intradiscal pressures. In clinical trials junctional tethering has shown promising results with lower rates of PJF of 4% versus 18% [15, 16].
Pseudarthrosis following adult deformity surgery negatively impacts patient outcomes and has been reported in up to 24% of cases, with the thoracolumbar and lumbosacral junction being at highest risk [17]. Generally, risk factors for pseudarthrosis are advance age, incomplete sacropelvic fixation (LIV S1 versus pelvis), residual postoperative global imbalance, thoracolumbar kyphosis (> 20°) and osteoarthritis of the hip joint. In this study, we demonstrated, that ROM restriction, which can potentially influence fusion rate, was highest for the PS and CBS-variant when compared to TPH fixation. In cadaveric studies it has been shown that in the native spine ROM at T1/2 is almost 50% higher than that of any other thoracic level[18]. Overall UIV-TP hook fixation may increase risk for pseudarthrosis, particularly if T2 is the UIV.
Initially JK has been defined as sagittal Cobb angle UIV/UIV + 2 of more than 10° plus an increase between pre- and postop of at least 10° [19]. More recently, a novel definition of at least 15° increase between pre- and postop, measured between UIV and UIV + 1 [20] has been suggested. Mechanisms implicated in JK involve chronic endplate fractures of the UIV [21] in the lower thoracic spine and subluxation in the upper thoracic spine case of proximal thoracic UIV [22]. The observations of our study support these results, since the upper half of the UIV represents the highest stress zone. Instrument related factors have been suggested to increase risk of JK include pedicle versus transverse process hook fixation, rod diameter (transitional rod), sagittal rod bend, and intraoperative violation of UIV facet joints [23]. Previous studies have found the incidence of JK in adults following deformity correction to be at 22%, even though outcome measures seem to not be impacted. Eventually only 11% of all PJF patients required revision surgery. Surgery related risk factors are posterior fusion (in contrast to anterior fusion), fusion to the sacrum, postoperative under- or overcorrection, total amount of alignment change [24], while patient specific risk factors include obesity [25]. In the case of JF, which manifests more seriously, in addition to UIV fracture, usually hardware failure is implicated as well. The incidence of JF has been found to be as high as 35%, with a revision rate of 21% [26] and risk factors include lower thoracic spine instrumentation and overcorrection. In this study we showed that TPH fixation led to the lowest UIV intravertebral stresses, which might decrease the risk for endplate fractures, related to JF. Clinical studies on the utility of transverse process hooks came to varying conclusions. In a series of 39 adult patients, undergoing deformity correction, Matsumara et al. [4] found similar JK rates in patients with UIV-PS and TPH fixation, however the rate of JF was lower in patients with TPH fixation. In another study on 53 adult patients a significantly higher JK rate was found in patients with UIV-TPH fixation when compared to UIV-PS (36% vs 8%) [21].
As outlined in Table 1 the downsides of TPH are increased UIV/UIV + 1 intradiscal stress and lower rigidity of fixation. CBS, which demonstrate similar rigidity when compared to PS, induced less UIV endplate stresses and screw pull out, both of which are implicated in JF. Biomechanically it seems, that CBS might be a potential alternative to CPS fixation, however clinical experience with this trajectory in the thoracic spine is limited. Moreover, the entry point of CBS are not in line with CPS. Because of the upward/outward directed trajectory of CBS, less soft tissue damage might be necessary at the UIV/UIV + 1 junctional area in clinical practice, further decreasing the risk for JK/JF. AS shown in this study the rods between UIV/UIV-1 is at particular stress in the case of cortical bone screw fixation, since the entry point for this trajectory is not in line with the entry point of classical pedicles screws. In clinical practice this fact would need to be addressed, for instance by appropriate rod contouring or the use of offset connectors.
Classical ASD is a significant burden in the lumbar spine. Even though less prevalent in the thoracic spine, due to its increased rigidity and decreased discal ROM, it should also be considered in certain scenarios. As this study showed, TP hook fixation leads to the highest discal stresses at UIV/UIV + 1, which could have implications in the case of preexisting discal degeneration or congenital spinal stenosis.
Conclusion
The choice of UIV fixation technique (PS, CBS or TPH) has profound biomechanical implications, with instrumentation choice depending on individual patient risk profiles. PS and CBS are equally rigid modes of fixation; however, CBS induces less intravertebral stresses and less screw pull out forces thus potentially reducing the risk for JF. Our results suggest that TPH fixation might have the lowest risk for JF, however the risk for pseudarthrosis and adjacent segment disc degeneration might be high. The use of TPH might be less beneficial in cases with preexisting discal degeneration or congenital spinal stenosis at UIV/UIV + 1 or in cases with increased risk for pseudarthrosis.
References
Wang H, Ma L, Yang D et al (2017) Incidence and risk factors of adjacent segment disease following posterior decompression and instrumented fusion for degenerative lumbar disorders. Medicine 96:e6032
Liu F-Y, Wang T, Yang S-D et al (2016) Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J 25:2376–2383
Kim JS, Phan K, Cheung ZB et al (2019) Surgical, radiographic, and patient-related risk factors for proximal junctional kyphosis: a meta-analysis. Global Spine J 9:32–40
Matsumura A, Namikawa T, Kato M et al (2018) Effect of different types of upper instrumented vertebrae instruments on proximal junctional kyphosis following adult spinal deformity surgery: pedicle screw versus transverse process hook. Asian Spine J 12:622
Wang T, Cai Z, Zhao Y et al. Development of a three-dimensional finite element model of thoracolumbar kyphotic deformity following vertebral column decancellation. Applied bionics and biomechanics 2019; 2019:
Xuan J, Chen J, He H et al (2017) Cortical bone trajectory screws placement via pedicle or pedicle rib unit in the pediatric thoracic spine (T9–T12): a 2-dimensional multiplanar reconstruction study using computed tomography. Medicine 96:e5852
Kim YJ, Lenke LG, Bridwell KH et al (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine 29:333–342
Matsukawa K, Yato Y, Hynes RA et al (2017) Cortical bone trajectory for thoracic pedicle screws: a technical note. Clin Spine Surg 30:E497–E504
Jendoubi K, Khadri Y, Bendjaballah M et al (2018) Effects of the insertion type and depth on the pedicle screw pullout strength: a finite element study. Appl Bionics Biomech 2018:1–9
Huang J, Xie G, Liu Z (2008) FEA of hyperelastic rubber material based on Mooney-Rivlin model and Yeoh model. China Rubber Ind 8:22–26
Kurutz M (2010) Finite element modelling of human lumbar spine. Finite Element Analysis. IntechOpen, London
Kim YJ, Lenke LG (2005) Thoracic pedicle screw placement: free-hand technique. Neurol India 53:512
Rancourt D, Shirazi-Adl A, Drouin G et al (1990) Friction properties of the interface between porous-surfaced metals and tibial cancellous bone. J Biomed Mater Res 24:1503–1519
Bess S, Harris JE, Turner AW et al (2017) The effect of posterior polyester tethers on the biomechanics of proximal junctional kyphosis: a finite element analysis. J Neurosurg Spine 26:125–133. https://doi.org/10.3171/2016.6.SPINE151477
Rodnoi P, Le H, Hiatt L et al (2021) Ligament Augmentation with mersilene tape reduces the rates of proximal junctional kyphosis and failure in adult spinal deformity. Neurospine 18:580–586. https://doi.org/10.14245/ns.2142420.210
Safaee MM, Deviren V, Dalle Ore C et al (2018) Ligament augmentation for prevention of proximal junctional kyphosis and proximal junctional failure in adult spinal deformity. J Neurosurg Spine 28:512–519. https://doi.org/10.3171/2017.9.SPINE1710
Kim YJ, Bridwell KH, Lenke LG et al (2006) Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine 31:2329–2336
Wilke H-J, Herkommer A, Werner K et al (2017) In vitro analysis of the segmental flexibility of the thoracic spine. PLoS ONE 12:e0177823
Glattes RC, Bridwell KH, Lenke LG et al (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine 30:1643–1649
Helgeson MD, Shah SA, Newton PO et al (2010) Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine 35:177–181
Tsutsui S, Hashizume H, Yukawa Y et al (2021) Optimal anchor at the uppermost instrumented vertebra in long fusion from the pelvis to the lower thoracic spine in elderly patients with degenerative spinal deformity: hook versus pedicle screw. Clin Spine Surg 35:E280–E284
Ha Y, Maruo K, Racine L et al (2013) Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine 19:360–369
Cammarata M, Aubin C-É, Wang X et al (2014) Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine 39:E500–E507
Yagi M, King AB, Boachie-Adjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine 37:1479–1489
Wang H, Ding W, Ma L et al (2017) Prevention of proximal junctional kyphosis: are polyaxial pedicle screws superior to monoaxial pedicle screws at the upper instrumented vertebrae? World Neurosurg 101:405–415
Smith MW, Annis P, Lawrence BD et al (2015) Acute proximal junctional failure in patients with preoperative sagittal imbalance. Spine J 15:2142–2148
Funding
Funding for this study was received by EN and MM from Medtronic.
Author information
Authors and Affiliations
Contributions
EN, MM, ND, BY, LGL, MF, VA, SKC: conception, drafting, data analysis, manuscript preparation. AS: conception, drafting (original draft and final approval), data collection, manuscript preparation.
Corresponding author
Ethics declarations
Ethical approval
Approval by IRB and informed consent were not required for this study.
Conflict of interest
None of the authors have a conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nevzati, E., Moser, M., Dietz, N. et al. Clinically relevant biomechanical properties of three different fixation techniques of the upper instrumented vertebra in deformity surgery. Spine Deform 10, 1017–1027 (2022). https://doi.org/10.1007/s43390-022-00506-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00506-8