Abstract
Study design
A prospective study.
Objective
To investigate the paravertebral and lower extremity muscle activities using surface electromyography (S-EMG) in patients with adult spinal deformity (ASD) comparing with those of age-matched controls.
Summary of background data
Although the paravertebral muscle is greatly involved in ASD pathology, little is known about the contribution of lower extremity muscle on maintaining standing posture.
Methods
Fourteen patients with ASD (1 man, 13 women; mean age, 67.1 years) who underwent corrective fusion surgery with at least 2 years of follow-up and age-matched controls (1 men, 7 women; mean age, 69.3 years) were enrolled. The muscle activities of the thoracic and lumbar erector spinae (TES and LES), external oblique (EO), gluteus maximus (GM), rectus femoris (RF), and biceps femoris (BF) were recorded in the upright and anterior flexion positions using S-EMG pre-operatively and 1 year post-operatively.
Results
Compared with controls, patients showed a significantly higher muscle activity in the LES and BF at rest in a standing position. After corrective fusion surgery, the muscle activity of LES decreased and that of RF increased (p < 0.05), and the changes reached the level of the controls. When the posture changed from upright to anterior flexion, the controls showed increased muscle activity of the BF, whereas the patients showed decreased muscle activity of the TES and RF and increased muscle activity of the BF. Post-operatively, muscle activity of the TES, LES, GM, and BF increased and that of the RF decreased.
Conclusions
ASD patients required a higher activity of the lower extremity and trunk muscles to maintain a standing position compared to the age-matched controls. Significant increase of the GM, BF, and TES muscle activities during anterior bending suggest the presence of mechanical stress concentration caused by fixed lumbar spine.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although various factors, such as disc degeneration, osteoporosis-related vertebral fracture, and impairments in strength and function of the trunk muscles, affect the development and deterioration of spinal alignment, the etiology of adult spinal deformity (ASD) is still unclear [1, 2]. Many authors reported that the paravertebral muscles are greatly involved in the development and progression of spinal deformity [2,3,4,5]. Takemitsu et al. [6] revealed that patients with lumbar degenerative kyphosis had a significantly lower lumbar extensor strength and marked atrophy of the paraspinal muscles with fatty infiltration than individuals with no history of degenerative lumbar spine disease. According to the ‘‘cone of economy’’ theory proposed by Dubousset et al. [7], anterior tilting of the trunk would increase the work of the paravertebral extensor muscles in maintaining an upright posture. We previously reported that trunk tilting during standing and walking was significantly correlated with the cross-sectional area of the paravertebral muscles [8]. Hanada et al. [9] evaluated the paravertebral muscle activation amplitudes during walking using surface electromyography (S-EMG) in elderly patients with low back pain and demonstrated that the back extensor muscles were significantly activated to higher amplitudes compared to the asymptomatic control group, indicating the important role of these muscles in stabilizing the spine. Hyun et al. [10] reported that the patients with proximal junctional failure (PJF) after a long spinal fusion surgery had lower thoracolumbar muscularity and higher fatty degeneration than patients without PJF, indicating that the paravertebral muscles were also crucial for maintaining the postoperative sagittal alignment and preventing junctional failure. On the other hand, the pelvis and lower extremity cooperatively compensated for spinal kyphosis to prevent anterior translation of the axis of gravity, with the extent of compensation depending on spine stiffness and musculature status [11]. Therefore, the lower extremity muscles also play an important role in maintaining the standing posture. Understanding the function of these muscles is fundamental to prevent or slow down the progression of deformity in these patients. To the best of our knowledge, the specific contribution of the paravertebral and lower extremity muscles in maintaining the standing posture for patients with sagittal malalignment has not been evaluated.
Measuring the cross-sectional area is a simple and effective way of assessing muscle; many authors have therefore used this method to investigate the relationship between spinal deformity and the paravertebral muscles [10, 12]. However, a multi-faceted analysis of the important parameters, such as the quality of the muscle tissue (measured using histological analysis), muscle strength (measured using isokinetic muscle power), and muscle activity (measured using electromyography), should be considered when evaluating the muscular pathologies. Among them, measurement of muscle activity using S-EMG is a less invasive method that enables real-time assessment of multiple muscles in conjunction with motion.
Patients with spinal deformity require more muscle activity in their trunk and lower extremities to maintain the standing position compared to healthy individuals. This increased activity leads to muscle fatigue and pain, making it difficult to maintain a standing position for a long time. Restoring the correct posture with surgery reduces the muscle activity. After surgery, we instruct patients to refrain from bending forward to prevent PJF, but the scientific basis is unclear. Therefore, this study aimed to evaluate the muscle activity of the paravertebral and lower extremity muscles using S-EMG in patients with ASD and to compare the data with those of individuals without spinal deformity. The changes in muscle activity after corrective fusion surgery and forward bending were evaluated as well.
Materials and methods
Enrollment of participants
This study was approved by the institutional review board of our institution, and informed written consent was obtained from all patients. Patients with ASD who underwent corrective fusion surgery using long constructs from the lower thoracic spine to the pelvis between April 2016 and April 2018 in our department with at least 2 years of follow-up were eligible for our study. We excluded patients with a history of spinal surgery, infection, and/or neuromuscular diseases, such as Parkinson’s disease, who could not undergo assessment with S-EMG, and those who experienced postoperative complications requiring revision surgery during the follow-up period. We also excluded patients with hip or knee arthroplasty. The control population consisted of elderly patients with osteoarthritis who did not have spinal disease based on their history and radiographic findings. Furthermore, degenerative changes found in these subjects were attributed to their age. However, they did not have scoliosis or vertebral fractures.
Assessment using S-EMG
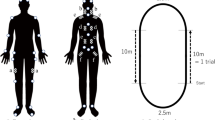
Prior to the application of S-EMG electrodes, all sites were cleaned with alcohol to ensure low impedance (typically < 5 kOhm). The pairs of 38-mm surface electrodes (Blue sensor SP-00-S, METS, Chiba, Japan) were attached in the following muscles in only the right side of the participants: thoracic and lumbar erector spinae (TES and LES), external oblique (EO), gluteus maximus (GM), rectus femoris (RF), and biceps femoris (BF) (Fig. 1a). These active electrodes were placed 2 cm apart and parallel to the following muscle fibers: TES (7th thoracic and 2 cm lateral to the spinous process), LES (4th lumbar level and 4 cm lateral to the spinous process), EO (2 cm anterior from the line connecting between the tip of the iliac crest and rib), GM (midpoint between the lateral aspect of the sacrum and greater trochanter), RF (midpoint between the anterior superior iliac spine and tip of patella), and BF (midpoint between the ischial tuberosity and head of fibula).
a The attachment of surface electrodes; ① thoracic erector spinae (TES); ② lumbar erector spinae (LES); ③ external oblique (EO); ④ gluteus maximus (GM); ⑤ rectus femoris (RF); ⑥ biceps femoris (BF). Measurement of maximum voluntary contraction using a fixed trunk dynamometer (b flexion, c extension); Measurement of maximum voluntary contraction by manual resistance; (d gluteus maximus, e rectus femoris, f biceps femoris)
Then, the EMG signals were recorded with a telemetric EMG system (TeleMyo™ DTS, Noraxon USA Inc, Scottsdale, AZ) with a bandpass filter between 5 and 500 Hz and sampled at 1500 Hz. The S-EMG signals were received from six channels and transmitted to the personal computer wirelessly.
Participants were asked to maintain the posture during the 3-s recording of S-EMG data. The muscle electrical activity was determined by calculating the mean value of the amplitude over a stable period. These data were obtained at rest in a standing position and maximum anterior flexion position with 10 s rest in between. The results were normalized to the maximum activity observed during the maximum voluntary contraction (MVC). For the determination of MVC of these muscles, the participants were asked to perform a maximum isometric movement against resistance. For trunk muscles (TES, LES, and EO), MVC was measured using a fixed trunk dynamometer (Takei Scientific Instruments Co., JPN) (Fig. 1b, c), and for lower extremity muscles (GM, RF, and BF), MVC was measured by the manual resistance applied by the investigator (Fig. 1d–f). The mean amplitude for the three trials was calculated to obtain the MVC value.
The EMG data were analyzed using myoRESEARCH® 3 (Noraxon, Scottsdale, USA). After rectification and smoothing, the EMG signals were amplitude normalized to the average MVC value (%MVC). The average MVC value was the average of 0.5 s before and after the maximum muscle activity. In patients with ASD, the muscle activity was assessed pre-operatively and at 1 year post-operatively.
Radiographic measurements
A standardized lateral view of the entire spine in the standing position was obtained for all participants at each measurement time point; they were asked to relax their heads while looking straight ahead, without pulling in the chin, with their hands placed on their clavicles, and with a 1.5-m distance between the radiographic tube and the patient. The following alignment parameters were measured from the radiographs: sagittal vertical axis (SVA), pelvic tilt (PT), pelvic incidence (PI), lumbar lordosis (LL), and thoracic kyphosis (TK).
Data analysis
Among controls, we compared the muscle activity measured pre-operatively with that measured at post-operatively. Moreover, the muscle activity changes depending on the posture (at rest in a standing position versus maximum anterior flexion) were assessed. The spinopelvic parameters (SVA, PT, PI, LL, and TK) were compared between the patients and controls.
To compare the muscle activity and radiographic parameters, paired t test and Wilcoxon test were used for intragroup changes and Mann–Whitney U test for inter-group changes. The Spearman correlation coefficient was calculated to evaluate the correlations between muscle activity and radiographic parameters. To verify the accuracy of a fixed trunk dynamometer, trunk muscle strength (flexion and extension) was measured 3 times in 11 healthy volunteers, and the infraclass correlation coefficient (ICC) was determined.
All statistical analyses were performed using SPSS version 23.0 (SPSS Inc., Chicago, IL). A P value < 0.05 was considered significant.
Results
We examined 14 patients with ASD (1 man, 13 women) and 8 elderly volunteers (1 men, 7 women). The mean age and range of the patients and elderly volunteers were 67.1 (standard deviation [SD]: 7.9) and 69.3 (SD: 9.3) years, respectively. The mean body mass index was 21.4 (SD: 2.6) and 22.0 (SD: 1.7) kg/m2, respectively. There were no differences in demographic data between the patients and controls. The mean follow-up period of the patients with ASD was 43.9 months (range, 28–45) months.
Regarding ASD pathologies, out of 14 patients with ASD, 13 had de novo scoliosis and 1 had progressed idiopathic scoliosis. There were no cases of post-traumatic fractures or iatrogenic deformity. The mean number of levels fused was 8.4 segments, with an upper instrumented vertebra (UIV) of T7 in 1 patient, T9 in 3, and T10 in 10 patients. All patients underwent sacroiliac fusion using bilateral S1 and iliac screws. Sagittal alignment, as represented by the spinopelvic parameters, in the patients with ASD that was significantly worse at baseline compared with controls, improved significantly at 2-year post-operatively (Table 1, Fig. 2).
The fixed trunk dynamometer showed high reliability, with ICC values for trunk flexion and extension muscle strength of 0.944 and 0.864, respectively. Regarding the S-EMG of the trunk and lower extremity, at rest in a standing position, the patients with ASD showed a significantly higher muscle activity in LES and BF than the controls (p < 0.05) (Table 2 and Fig. 3). After corrective fusion surgery, a decrease in LES muscle activity and an increase in RF muscle activity were observed (p < 0.05), and the changes reached the level of the controls (Table 2). On the other hand, on anterior flexion, there was no significant difference between the ASD patients and controls. However, a significant increase in TES muscle activity was observed after corrective fusion surgery (p < 0.05) (Table 3).
When the posture changed from standing to anterior flexion, the control subjects showed minimal changes in muscle activity, with only the BF showing a significant increase (Fig. 4). However, the patients with ASD showed a significant decrease in TES and RF and a significant increase in BF (Fig. 5). After corrective fusion surgery, TES showed a significant increase in muscle activity at the anterior flexion position compared to that pre-operatively. Moreover, a significant increase in LES, GM, and BF, and a significant decrease in RF were observed (Fig. 6).
Discussion
Several reports have investigated the paravertebral muscle activity using S-EMG for patients with spinal disease [13, 14]. However, few reports have investigated the paravertebral muscle activity in patients with spinal kyphosis. Enomoto et al. [15] demonstrated that the patients with lumbar degenerative kyphosis had a higher muscle activity of the paravertebral muscles at rest in a standing position than age-matched patients with lumbar spinal canal stenosis and healthy volunteers. Our results are consistent with the findings of the previous report. We also showed that when maintaining the upright posture, the lower extremity muscles, such as GM, RF, and BF, and trunk muscles, including TES, LES, and EO, required a higher muscle activity in patients with ASD than in health young participants (Table 2). Prior et al. [16] revealed that a significant increase in the BF muscle activity was observed when the pelvis moved from a normal position to retroversion. Patients with ASD maintained the standing posture through pelvis retroversion (high pelvic tilt) [11]. Therefore, not only trunk anterior tilting but also pelvic retroversion could contribute to an increase in BF muscle activity in patients with ASD. Spinal kyphosis could also be compensated by the lower extremity through hip extension and knee bending to maintain global alignment [11, 17]. Therefore, the lower extremity muscles need higher muscle activity during standing in patients with ASD than in healthy young individuals who require minimal muscle activity to maintain the standing posture.
On the other hand, after corrective fusion surgery, the muscle activity of LES decreased and that of RF increased significantly (Table 2). The fixed lumbar spine using an instrument and muscle denervation could be affect the decrease of LES muscle activity after operation. Although the BF showed higher activity than the RF pre-operatively, after the operation, the RF showed higher activity (Table 2). These results suggested that during a forward trunk tilt, the BF requires more effort compared to RF to maintain the standing posture; however, sagittal spinal realignment through corrective surgery would facilitate the use of RF with knee extension to reduce the load on the BF. Despite involving healthy individuals as the study subjects, Wang et al. [18] revealed that with anterior trunk tilting, an increase in BF and erector spinae activation was observed, accompanied by a decrease in RF activity, with the opposite pattern being observed in posterior trunk tilting. In fact, an increase in BF activity and a decrease in RF activity in the flexion position than at rest in a standing position were observed in both controls and patients (Figs. 4 and 5). Although sagittal alignment was corrected through surgery, every muscle still required a higher activity to maintain the standing posture in the patients than in controls, because the fixed spine is different from the flexible spine, with the former possibly increasing the load on the non-fixed area such as the thoracic spine, pelvis, and lower extremity.
In patients with ASD, the muscle activity of the lower extremity muscles (GM, RF, and BF) were significantly changed during anterior bending after surgery compared to that pre-operatively (Figs. 5 and 6). A fixed spine that has lost its ability to compensate might place a load on the GM and BF to maintain an anterior flexion posture. Regarding the proximal junction, the patients with ASD showed a decrease in TES activity during anterior flexion (Fig. 5); on the contrary, a significant increase in TES activity was observed after fusion surgery (Fig. 6). The thoracic spine has a compensatory mechanism to maintain standing posture by reducing thoracic kyphosis [11], which results in an increase in the TES activity in the standing position. Taking the anterior flexion position seemed to cancel this compensation mechanism and reduce the muscle activity. However, after surgery, mechanical stress was concentrated on the proximal junction due to the fixed lumbar spine, thereby causing a proximal junctional failure, which was reported as one of the major complications after long spinal fusion surgery [19]. Proximal junctional failure has been reported to be caused by multiple factors, including age, fusion to the pelvis, preoperative thoracic kyphosis, low bone mineral density, lower muscularity, and excessive correction [19,20,21,22]. We showed that, after corrective fusion surgery, TES required a high muscle activity to maintain the anterior flexion position. Greater trunk extensor muscle activation, which may increase the spinal load, was reported to contribute to vertebral fracture [13]. Our finding may partly help to explain the mechanisms of vertebral fracture around the upper instrumented vertebra, leading to proximal junctional failure after long fusion surgery. Therefore, after corrective fusion surgery, patients should be prohibited to perform anterior flexion to prevent the concentration of mechanical stress on the proximal junction.
This study has several limitations. First, participants were asked to maintain the posture during surface electromyography measurements. The patients maintaining their position due to pain were excluded because accurate measurement was not possible. However, these actions could be limited due to pain in ASD patients. Second, we normalized the muscle activity using %MVC. Although this method is the most widely used reference point for normalization, it is often subjective and potentially limited by sensation of pain in injured individuals [23]. Third, we evaluated trunk muscles only in one side. These muscle activities could be different in patients with scoliosis. Finally, the sample size was relatively small, and these results might diminish the statistical relevance of the inter-group comparisons.
In conclusion, patients with ASD required a higher activity of the lower extremity and trunk muscles to maintain a standing position than normal controls. After corrective fusion surgery, a significant increase in the muscle activity of the lower extremity muscles (GM, BF) and TES was observed during anterior bending, suggesting the presence of mechanical stress concentration caused by the fixed lumbar spine.
Key points
-
We assessed the paravertebral and lower extremity muscle activities using surface electromyography in patients with adult spinal deformity (ASD) and compared the results with those of controls.
-
The patients with ASD required a higher activity of the lower extremity and trunk muscles to maintain a standing position, compared with age-matched controls.
-
After corrective fusion surgery, the muscle activity of lumbar erector spinae decreased and that of rectus femoris increased.
-
The muscle activity of gluteus maximus, biceps femoris, and thoracic erector spinae significantly increased during anterior bending after surgery.
References
Banno T, Togawa D, Arima H et al (2016) The cohort study for the determination of reference values for spinopelvic parameters (T1 pelvic angle and global tilt) in elderly volunteers. Eur Spine J 25:3687–3693
Hongo M, Miyakoshi N, Shimada Y et al (2012) Association of spinal curve deformity and back extensor strength in elderly women with osteoporosis in Japan and the United States. Osteoporos Int 23:1029–1034
Miyakoshi N, Hongo M, Maekawa S et al (2007) Back extensor strength and lumbar spinal mobility are predictors of quality of life in patients with postmenopausal osteoporosis. Osteoporos Int 18:1397–1403
Yagi M, Hosogane N, Watanabe K et al (2016) The paravertebral muscle and psoas for the maintenance of global spinal alignment in patient with degenerative lumbar scoliosis. Spine J 16:451–458
Banno T, Yamato Y, Hasegawa T et al (2017) Assessment of the cross-sectional areas of the psoas major and multifidus muscles in patients with adult spinal deformity: a case-control study. Clin Spine Surg 30:E968–E973
Takemitsu Y, Harada Y, Iwahara T et al (1988) Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine (Phila Pa 1976) 13:1317–1326
Dubousset J (2011) Reflections of an orthopaedic surgeon on patient care and research into the condition of scoliosis. J Pediatr Orthop 31:S1-8
Banno T, Arima H, Hasegawa T et al (2019) The effect of paravertebral muscle on the maintenance of upright posture in patients with adult spinal deformity. Spine Deform 7:125–131
Hanada EY, Johnson M, Hubley-Kozey C (2011) A comparison of trunk muscle activation amplitudes during gait in older adults with and without chronic low back pain. PM&R 3:920–928
Hyun SJ, Kim YJ, Rhim SC (2016) Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J 16:1095–1101
Barrey C, Roussouly P, Le Huec JC et al (2013) Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 22(Suppl 6):S834–S841
Yagi M, Kaneko S, Yato Y et al (2017) Drop body syndrome: a distinct form of adult spinal deformity. Spine (Phila Pa 1976) 42:E969-e77
Greig AM, Briggs AM, Bennell KL et al (2014) Trunk muscle activity is modified in osteoporotic vertebral fracture and thoracic kyphosis with potential consequences for vertebral health. PLoS ONE 9:e109515
Wang YJ, Li JJ, Zhou HJ et al (2016) Surface electromyography as a measure of trunk muscle activity in patients with spinal cord injury: a meta-analytic review. J Spinal Cord Med 39:15–23
Enomoto M, Ukegawa D, Sakaki K et al (2012) Increase in paravertebral muscle activity in lumbar kyphosis patients by surface electromyography compared with lumbar spinal canal stenosis patients and healthy volunteers. J Spinal Disord Tech 25:E167–E173
Prior S, Mitchell T, Whiteley R et al (2014) The influence of changes in trunk and pelvic posture during single leg standing on hip and thigh muscle activation in a pain free population. BMC Sports Sci Med Rehabil 6:13
Obeid I, Hauger O, Aunoble S et al (2011) Global analysis of sagittal spinal alignment in major deformities: correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J 20(Suppl 5):681–685
Wang Y, Asaka T, Zatsiorsky VM et al (2006) Muscle synergies during voluntary body sway: combining across-trials and within-a-trial analyses. Exp Brain Res 174:679–693
Lau D, Clark AJ, Scheer JK et al (2014) Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 39:2093–2102
Liu FY, Wang T, Yang SD et al (2016) Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J 25:2376–2383
Hyun SJ, Kim YJ, Rhim SC (2016) Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J 16(9):1095–1101
Maruo K, Ha Y, Inoue S et al (2013) Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 38:E1469-1476
Marras WS, Davis KG (2001) A non-MVC EMG normalization technique for the trunk musculature: part 1. Method development. J Electromyogr Kinesiol 11:1–9
Acknowledgements
No other person aside from the authors made substantial contributions to conception, design, acquisition of data, or analysis and interpretation of data, or was involved in drafting the manuscript or revising it critically for important intellectual content. No funding was received for the design, in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication. No language editor or scientific (medical) writer was involved in the preparation of the manuscript.
Funding
YY and SO belong to the division as follows; Donated Fund Laboratory (Division of Geriatric Musculoskeletal Health, Hamamatsu University School of Medicine, Shizuoka, Japan). Meitoku medical institute Jyuzen memorial hospital, Shizuoka, Japan. Japan Medical Dynamic Marketing Inc, Tokyo, Japan. Medtronic Sofamor Danek Inc., Memphis, United States.
Author information
Authors and Affiliations
Contributions
TB, YY, ON, TH, GY, HA, SO, HU, TY, KI, YW, KY, and YM: conception or design of the work; TB, YY, and ON: acquisition of data for the work; TB, YY, and ON: analysis of data for the work; TB, YY, and ON: interpretation of data for the work; TB, YY, ON, TH, GY, HA, SO, HU, TY, KI, YW, KY, and YM: drafting the work or revising it critically for important intellectual content; TB, YY, ON, TH, GY, HA, SO, HU, TY, KI, YW, KY, and YM: final approval of the version to be published; TB, YY, ON, TH, GY, HA, SO, HU, TY, KI, YW, KY, and YM: agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
TB, ON, TH, GY, HA, HU, TY, KI, YW, KY and YM have nothing to disclose.
Ethical approval
All study participants provided informed consent, and the study design was approved by the appropriate ethics review boards in Hamamatsu University School of Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Banno, T., Yamato, Y., Nojima, O. et al. Comparison of the postoperative changes in trunk and lower extremity muscle activities between patients with adult spinal deformity and age-matched controls using surface electromyography . Spine Deform 10, 141–149 (2022). https://doi.org/10.1007/s43390-021-00396-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00396-2