Abstract
Study design
Three imaging techniques were compared using porcine spines.
Objectives
To compare image acquisition time, radiation exposure, pedicle width measurement, assessment of screw breach, and image artifact between cone-beam tomosynthesis (CBT) single mode, CBT dual mode (stereotactic CBT), and computed tomography (CT) imaging with and without spinal implants.
Summary of background data
CT is the standard for axial imaging of orthopedic procedures. CBT technology is being developed, allowing real-time intraoperative imaging and 3D surgical guidance. CBT may deliver useful axial imaging quicker with less radiation than current technologies.
Methods
Six porcine spines were instrumented with bilateral pedicle screws at six levels connected with 5.5 mm rods. Dosimeters were attached to four surfaces of spines. CT, CBT single and CBT dual images were acquired pre-implant and post-implant. Image acquisition and 3D reconstruction times were recorded. Pedicle widths were measured before and after instrumentation. Screw medial breaches were graded (0: no breach, 1: < 2 mm, 2: 2–4 mm, 3: > 4 mm). Artifact and/or distortion of each image was ranked (0 = none, 1 = mild, 2 = moderate, 3 = large). Image acquisition and reconstruction times, radiation dose, pedicle width, screw breach and artifact were compared between techniques.
Results
Total image acquisition and reconstruction times of CBT was significantly less (single: 9.9 ± 0.2 s, p < 0.001; dual: 60.0 ± 8.7 s, p < 0.001) than CT (250.3 ± 36.7 s). CBT had significantly less radiation exposure than CT (CT: 0.7 ± 0.1 rad, single: 0.03 ± 0.02 rad, dual: 0.07 ± 0.03 rad; p < 0.001). No difference in pedicle width change pre-implant to post-implant was found (CT: p = 0.449, single: p = 0.430, dual: p = 0.528). Pedicle width (pre-implant: p > 0.5, post-implant: p > 0.9) and pedicle width change (p > 0.4) was similar amongst all techniques. Breach assessment was not different between groups (p = 0.257). CBT images had consistently lower artifact grades than CT.
Conclusions
Although CBT axial image quality appeared subjectively inferior to CT, it enabled consistent assessment of pedicle width and screw breach, at half time and 10× lower radiation exposure. With continued refinements, CBT technology may allow for adequate intra-operative axial imaging using low radiation exposure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Currently, the gold standard to obtain axial imaging for bony procedures is computed tomography (CT). This involves a separate visit for the patient as it is not yet available in most hospital operating rooms. Despite substantial improvement in recent years, CT gives a high radiation exposure that may be especially concerning in children [1,2,3]. Alternatively, there is an increase in the amount of fluoroscopic imaging used during spine deformity cases, and concern of radiation exposure to both the patient and the surgical staff in the operating room merits attention [4, 5]. Intra-operative axial imaging is becoming more commonly used to assess pedicle screw position in adolescent scoliosis surgery.
Ideally, to allow for the most accurate and safe surgical procedures, intra-operative imaging would provide perfect three-dimensional (3D) visualization of the spine with no artifact or radiation exposure and would not require an interruption in the surgical procedure to acquire imaging. However, reality dictates that technical capability, imaging quality and radiation exposure to all persons in the operating room must strike a balance. Fluoroscopy allows for immediate 2D intra-operative imaging, with slight interruption of the surgical case, but no axial visualization is possible. Intra-operative CT navigation, such as the O-arm, provides intra-operative 3D visualization, and has been found to be comparably as effective for pedicle screw placement as using standard freehand technique or robotic guidance [6]. But CT requires substantial radiation and a pause in the surgical case to acquire imaging. Novel intraoperative three-dimensional (3D) cone-beam tomosynthesis technology (CBT, nView medical, Salt Lake City, UT) capable of real-time intraoperative image guidance technology has been developed, allowing visualization of the spine in the axial plane which has previously not been possible with the standard intraoperative fluoroscopy [7,8,9]. CBT technology was designed to deliver segmental images (axial, coronal, sagittal) and projection images (Anterior–Posterior, Medial–Lateral) in less time and with less radiation than currently available intra-operative technologies.
This study was an evaluation of CBT imaging using porcine spine specimens. The purpose was to assess spinal imaging using CBT single mode and CBT dual mode (stereotactic CBT images) compared to the current clinical 3D imaging gold standard of CT. Image acquisition time, radiation exposure, and pedicle width measurement with and without implants were compared between the three techniques. Pedicle screw breach and amount of artifact were assessed post-implant. The null hypothesis tested was that CBT imaging provides images allowing the same spinal anatomical measurements compared with the gold standard of CT imaging.
Materials and methods
Specimens and preparation
Thoracolumbar spines were harvested from six 12-month-old female Yucatan mini-pigs (weight 40–45 kg at 9 months old). Dosimeters were attached to the spines at four locations by placing them onto gauze secured in place with rubber bands: anteriorly (A, placed 10 cm distal to most proximal rubber band marker), right side (R), left side (L), posteriorly (P, placed 10 cm proximal to the most distal rubber band marker) (Fig. 1). Dosimeter placement was documented using digital photography. Optical simulated luminescent dosimeters (InLight® nanoDots™, Landauer Inc., Glenwood, IL) were chosen to determine radiation exposure because of their small size, 5 mrad lower limit detection and an accuracy of ± 10% over a clinically relevant voltage range (70–140 kVp) [10,11,12].
Pre-implant imaging
CT imaging (0.625 mm slice thickness, General Electric 64-Slice LightSpeed VCT, Chicago, IL) was performed of each spine placed prone with the cephalic end entering the scanner first (Fig. 2). The clinical small body thoracolumbar spine imaging protocol used at our pediatric institution (internal protocol 7.4) was used: 100 kVp with length set to 30 cm and width to 20 cm. Time of acquisition was recorded from the scanning machine. Time for the technician to create 2D and 3D reconstructions from scanned images was measured using a stopwatch. Following CT imaging, dosimeters were replaced with unexposed dosimeters at the identical locations.
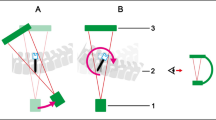
CBT Imaging was performed on a custom radiolucent table with spines positioned prone. First, the single mode (pediatric mode, 60 kVp, single CBT acquisition) was used for each spine. Spines were centered under the detection side of the device using the acquisition length marked by rubber bands (Fig. 3), and acquisition width set to 20 cm. Distance between the detection panel and table top was 12.8 to 13.3 cm. Time of acquisition and time to create 3D reconstructions from scanned images was recorded directly from the scanning machine. After the single mode scan was complete, dosimeters were removed and replaced with unexposed dosimeters at the identical locations. CBT imaging was then performed using the dual mode (pediatric mode, 60 kVp, dual stereotactic CBT acquisition); one image taken at 30° clockwise and another at 30° counter-clockwise (Fig. 4). Time of acquisition was recorded directly from the scanning machine. Time to create 3D reconstructions from scanned images was measured using a stopwatch. Times were compared between three techniques using ANOVA, and if Alpha was p < 0.05, pairwise comparisons were performed. Alpha was set at p < 0.05 to declare significance.
Implant details
Muscle was removed from the posterior spine over six vertebral levels. Bilateral pedicle screws (4.0 or 5.0 mm diameter, 20, 25, 30 or 35 mm long, uniaxial or polyaxial, Titanium (Ti), OrthoPediatrics, Warsaw, IN) were placed in the six levels using anatomic landmarks with a total of 12 screws per spine. 5.5 mm diameter rods (Ti or cobalt chromium (CoCr)) connected the screws via Ti set screws (OrthoPediatrics) on each side (Fig. 5).
Post-implant imaging
CT and CBT single and dual imaging was repeated identically to the pre-implant scans (Figs. 6 and 7), reconstructions were performed and the timing was recorded.
Radiation exposure analysis
Control dosimeters were supplied with each group of dosimeters used and were kept with the specimens as they were moved between imaging devices, but not exposed. All dosimeters were returned to the manufacturer (Landauer Inc.) within 24 h of exposure and exposure report was provided by the company. Control values were subtracted from the exposure reading for each group to account for background radiation.
Friedman nonparametric test for related samples was used to compare exposure time and reconstruction times between CT, CBT single and CBT dual. A linear mixed effects model was used to evaluate differences in exposure based on dosimeter placement within each modality, with dot position as a repeated effect. Bonferroni post hoc comparisons were used to compare the four positions. Then, for supplemental evaluation, repeated measures ANOVA was performed to evaluate differences in exposure based on dosimeter placement within each modality, with dot position as a repeated effect. Bonferroni post hoc comparisons were used to compare the four positions. Similar analysis was performed for radiation exposure based on technique, followed by a separate mixed model analysis for single versus dual without CT, which accounted for dot position as a repeated factor. Wilcoxon signed ranks test was utilized for post hoc comparison among the three techniques. Alpha was set at p < 0.05 to declare significance (IBM SPSS Statistics for Windows, Version 25.0, Armonk, NY).
Pedicle width measurement
All CT and CBT images were imported into the publically available Medical Imaging Interaction Toolkit (MITK 2018.4.0, developed by the German Cancer Research Center, Division of Medical Image Computing, Heidelberg, Germany). Pedicle widths of each of the six spines were measured at the six instrumented vertebral levels, on both the right and left sides from CT, CBT single mode and CBT dual mode both before and after implants were placed.
All vertebral levels with visible pedicles were included to a maximum of 72 measurements per technique (6 spines × 6 vertebral levels × 2 pedicles per vertebra). Linear mixed effects models were utilized to compare pre to post changes within each technique for pedicle width, comparing pre to post-instrumentation. Pre pedicle width, post pedicle width, and difference in pedicle width (post minus pre) were compared between techniques. For between group comparisons, analyses utilized only vertebral levels that had measurements for all techniques being compared. Sidedness and vertebral level were included in the models as subject effects to account for non-independence. CT scan was set as reference within the fixed effects factorial model. Bonferroni post hoc comparisons were used to compare among the three techniques. Alpha was set at p < 0.05 to declare significance.
Screw breach assessment
Each image taken following pedicle screw placement was accessed at each level, right and left sides, for pedicle screw breach of the medial spinal canal. The criteria were: Grade 0 is completely in, Grade 1 is < 2 mm breach, Grade 2 was 2–4 mm, and Grade 3 was > 4 mm [13].
McNemar–Bowker test for paired proportions was utilized to evaluate the proportion of pedicle breach grades across the three techniques. All vertebral levels with visible pedicles were included to a maximum of 72 assessments per technique. A secondary sensitivity/specificity analysis using CT as the gold standard was performed which combined Grades 1, 2 and 3 into a “yes” category and Grade 0 was “no” category. Alpha was set at p < 0.05 to declare significance.
Artifact assessment
Qualitative assessment was made of the artifact and distortion of each imaging modality. A single orthopedic surgeon ranked the artifact presence in each image as Grade 0 = none, Grade 1 = mild, Grade 2 = moderate, Grade 3 = large. For example, in Fig. 7 (CoCr rod) the CT image (left) is Grade 3 bilaterally and the single CBT image (middle) and dual CBT image (right) are both Grade 1 bilaterally; Fig. 7 (Ti rod), the CT image (left) is Grade 2 bilaterally, and the single and dual CBT images are Grade 1 bilaterally.
Results
Post-implant imaging times are presented (Table 1), allowing for training during pre-implant acquisition. The radiology technician performed an initial scan to identify the sample length on the CT scanner (mean ± stdev, 51.0 ± 21.1 s), then returned to the CT console, performed a scout scan and selected the region of interest (74.2 ± 11.3 s), before the actual scan was acquired. All CT scans had an exposure time of 3.3 s. Following exposure, it took the technician 29.3 ± 6.3 s to create 2D (coronal and sagittal) reconstructions and an additional 92.5 ± 29.8 s for a 3D reconstruction (Fig. 6). CBT image acquisition did not require a scout scan and selection of a region of interest. The exposure time was 3.0 s for single mode and 6.0 s for dual mode, both significantly different (p = 0.002; p = 0.014 for each pairwise comparison) from the 3.3 s CT scan exposure time. Reconstruction time for single mode was 6.9 ± 0.2 s (significantly less than for CT scans, p = 0.028) and for dual mode was 54.0 ± 8.7 s.
Radiation exposure
Dosimeter reading
Each of the three control dosimeters recorded 0.003 rad of background radiation exposure. One of the spines required re-imaging (CBT dual) so the dosimeters were replaced; however only three dosimeters were available, so for between group comparisons, n = 23 dosimeters was used. For CT scan, dosimeters placed anteriorly had significantly less exposure than the left side and posteriorly (p = 0.029 and p = 0.044, respectively). For both CBT modes, dosimeters placed posteriorly received significantly less exposure than in all other locations (p ≤ 0.003 in all cases, Fig. 8). Both CBT modes had significantly lower exposure than CT (20× lower radiation for CBT single and 10× lower for CBT dual) regardless of dosimeter position (p < 0.05), with no difference between CBT single and dual (p = 0.41, Fig. 9). When single was compared to dual (without CT), dual had significantly more exposure than single (p < 0.001). RM ANOVA analysis followed by pairwise comparisons resulted in all three techniques with significantly different radiation exposure than each of the other (p < 0.001).
Pedicle width
Positioning was very sensitive for CBT single mode. Images were not clear along the full 30 cm acquisition length. Pedicle anatomy visualization was adequate of the vertebral levels directly in the middle of the acquisition length, but became more difficult at the most proximal and distal ends of the spine. For this reason, pedicle widths were measured for 2 or 3 of the 6 levels from each of these images only, resulting in 28 measurements for the CBT single group and 72 measurements for the CT and CBT dual groups.
No significant difference in pedicle width change from pre to post-instrumentation was found for CT (72 measurements, p = 0.449), CBT single (28 measurements, p = 0.430) or CBT dual (72 measurements, p = 0.528). When comparing all three groups (28 measurements each), there were no differences between pedicle width pre-implant (all p > 0.5) and post-implant (all p > 0.9). In addition, the change in pedicle width from pre to post was not different between the three techniques (all p > 0.4, Table 2). When comparing only CT and CBT dual (72 measurements each), there were no differences in pedicle width pre-implant (p = 0.483), post-implant (p = 0.247) and no difference in the change between pre and post (p = 0.786).
Screw breach
There was no significant difference in breach count (Grades 0, 1, 2, 3) between the three groups when evaluating the 28 assessments included in all three techniques (p = 0.257). When comparing only CT and CBT dual (72 assessments each) no statistical difference was observed (p = 0.1). Of these 72 assessments, 61 (84.7%) had perfect agreement. Of the remaining 11, all were off by one grade only (ten between Grades 0 and 1, and one between grade 1 and 2).
There was no significant difference in breach count (Yes or No) between the three groups when evaluating the 28 assessments included in all three techniques (p = 0.453). When comparing only CT and CBT dual (72 assessments each) there was no statistical difference (p = 0.1). Of these 72 assessments, 62 (86.1%) had agreement. For CBT single compared to the gold standard of CT, sensitivity was 80.0% (95% CI 44.4% to 97.5%) and specificity was 83.3% (95% CI 58.6% to 96.4%). For CBT dual compared to the gold standard of CT (72 assessments), sensitivity was 75.0% (95% CI 56.6% to 88.5%) and specificity was 95.0% (95% CI 83.1% to 99.4%).
Artifact assessment
All 72 of the CT assessments were graded either Grade 2 (moderate) or Grade 3 (large) (Table 2). Furthermore, in CT images, the three spines that had implants including Ti rods received Grade 2 and the three spines with CoCr rods received Grade 3. All 72 CBT dual image assessments received a Grade 1 (mild artifact seen). All CBT single image assessments received artifact grade of 3 bilaterally for the three most distal levels which were nearer the edge of the images. CBT single images received artifact grade 1 bilaterally for the three spinal levels in the middle of the image with the exception of one level, both sides, which received a “transitional” grade of 2.
Discussion
Over the past decade, more centers are using intra-operative axial imaging to assess pedicle screw position during scoliosis deformity correction. 2D/3D fluoroscopy and intra-operative CT are currently available and provide confirmation of screw position as well as allow navigation to aid in implant placement. Similar to the use of neuromonitoring in scoliosis surgery, axial imaging has the potential to become “standard of care” to decrease the incidence of implant malposition, neurologic compromise or revision surgery. Current intra-operative imaging technologies however have some limitations including radiation exposure, modified surgical work flow including delays due to imaging acquisition and processing, and challenges due to bulky imaging equipment and limited operating room space.
3D CBT was recently developed to improve our ability to acquire intra-operative axial imaging of the spine. Another potential benefit of this modality is the ability to use it simultaneously as a standard fluoroscan machine for localization or identification of anatomic landmarks for freehand pedicle screw placement. However, as this technology is still in development, we aimed to perform a pre-clinical in-vitro trial in a porcine model to evaluate image quality, image acquisition and reconstruction time and exposure to ionizing radiation. In summary, we found that the single and dual CBT modalities were able to provide adequate axial imaging in significantly shorter time and with significantly less ionizing radiation.
The subjective quality of the images was definitely inferior compared to CT, especially with single modality CBT. However, if the goal of this technology is to assess pedicle screw position and ensure that the screws are contained within the medial and lateral walls and short of the anterior cortex, our analysis demonstrates that this could be achieved. Additionally, assessment of the bony landmarks was possible even with pedicle screws instrumented in the porcine spines.
Subjectively we found substantial differences between the single and dual CBT modes, especially at the periphery of image data acquisition. The single CBT images are obtained with a single anterior to posterior exposure and the axial images are reconstructed from the acquired data (Fig. 3). On the other hand, the dual images are obtained by performing two oblique images that are 30° from the coronal position in both directions (Fig. 4). With this additional information, the axial representation of the spine was subjectively more accurate. This technique is unique from other fluoroscopy based technologies that acquire several hundred images circumferentially around the patient. While the exposure to ionizing radiation has been published previously using these devices, a direct comparison to CBT technology has not been performed.
This study has some limitations that should be considered. The use of dosimeters placed on a spine specimen may not provide an accurate approximation of exposure to a patient’s body, but does allow a direct comparison of the radiation exposure between imaging techniques. Additionally, only six levels of the spine were instrumented, longer spinal procedures, multiple acquisitions would be required to image the entire instrumented spine, requiring additional time and radiation exposure. Thirdly, all measurements were made by a single unbiased observer as such inter-rater reliability of these measurements is not available. Finally, this study does not assess the clinical adoption and integration of this technology in a functioning operating room. Future studies will be required to determine true clinical applicability of this technology in surgical management of pediatric spinal deformities, as well as present inter- and intra-rater reliability.
In conclusion, this study demonstrated that although CBT axial image quality appeared subjectively inferior to CT, it enabled consistent assessment of pedicle width and screw breach, at half the time and 10× lower radiation exposure. Pedicle width measurements were not different between the three techniques, both with and without the presence of pedicle screws. CT imaging artifact is sensitive to implant metal (Ti had moderate artifact and CoCr had a large amount of artifact) whereas this metal difference was not seen in any CBT images. With continued refinements, CBT technology may allow for adequate intra-operative axial imaging using low radiation exposure.
IRB statement
This project does not involve live humans or animals so IRB and IACUC approval are not necessary.
Key points
-
As long as the pedicle was adequately visualized, CBT single and dual modes offered accurate magnitude of pedicle width measurement and pedicle breach assessment.
-
CBT single mode radiation exposure was 20× lower than CT and CBT dual mode was 10× lower than CT.
-
Adding pedicle screws did not change pedicle width measurements when using CT, CBT single mode and CBT dual mode.
-
Pedicle width measurements were not different between CT and the two CBT modes, both with and without the presence of pedicle screws.
References
Goodman TR, Mustafa A, Rowe E (2019) Pediatric CT radiation exposure: where we were, and where we are now. Pediatr Radiol 49:469–478
Brenner DJ, Hall EJ (2007) Computed tomography—an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Brenner DJ (2010) Should we be concerned about the rapid increase in CT usage? Rev Environ Health 25:63–68
Hadelsberg UP, Harel R (2016) Hazards of ionizing radiation and its impact on spine surgery. World Neurosurg 92:353–359
Urakov TM (2018) Practical assessment of radiation exposure in spine surgery. World Neurosurg 120:e752–e754
Laudato PA, Pierzchala K, Schizas C (2018) Pedicle screw insertion accuracy using o-arm, robotic guidance, or freehand technique: a comparative study. Spine 43:E373–E378
Conger A, Shah L, Shah V, McCormick Z (2020) Cone beam tomosynthesis: an emerging technology for procedural image guidance. Pain Med. https://doi.org/10.1093/pm/pnz340(Online ahead of print)
Atria C, Noo F, Keiriz J, Packard N, Last L (2017) Assessment of a novel real-time cone beam tomosynthesis (cbt) X-ray scanner. Med Phys 44:3013
Atria C, Last L, Packard N, Noo F (2018) Cone beam tomosynthesis fluoroscopy: a new approach to 3D image guidance. In: Medical imaging: image-guided procedures, robotic interventions, and modeling 105762018:105762V. International Society for Optics and Photonics
Balaguru D, Rodriguez M, Leon S, Wagner LK, Beasley CW, Sultzer A (2018) Numan MT comparison of skin dose measurement using nanoDot. Ann Pediatr Cardiol 11:12–16
Ben Abdennebi A, Aubry S, Ounalli L, Fayache MS, Delabrousse E, Petegnief Y (2017) Comparative dose levels between CT-scanner and slot-scanning device (EOS system) in pregnant women pelvimetry. Phys Med 33:77–86
Ding GX, Malcolm AW (2013) An optically stimulated luminescence dosimeter for measuring patient exposure from imaging guidance procedures. Phys Med Biol 58:5885–5897
Rampersaud YR, Pik JH, Salonen D, Farooq S (2005) Clinical accuracy of fluoroscopic computer-assisted pedicle screw fixation: a CT analysis. Spine 30:E183–190
Acknowledgements
Tracey P. Bastrom, MS for statistical analysis.
Funding
nView medical (Salt Lake City, UT) funded the study in part and provided use of imaging equipment, software and radiolucent table. Additional support was from the Orthopedic Division, Children’s Specialists of San Diego. Grant of use of spinal implants and instrumentation from OrthoPediatrics, Warsaw, IN.
Author information
Authors and Affiliations
Contributions
VU, CF—Design; Data acquisition, analysis and/or interpretation of work; Manuscript drafting and/or critically revising. Final approval of submitted manuscript. HB—Data acquisition, analysis and/or interpretation of work; Manuscript drafting and/or critically revising. Final approval of submitted manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Upasani, V.V., Bandaralage, H. & Farnsworth, C.L. 3D cone-beam tomosynthesis provides axial imaging of the spine with lower radiation compared to computed tomography. Spine Deform 9, 41–49 (2021). https://doi.org/10.1007/s43390-020-00199-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00199-x