Abstract
Study design
Retrospective.
Objective
Can a standardized, hospital-wide care bundle decrease surgical site infection (SSI) rate in pediatric spinal deformity surgery?
Summary of background data
SSI is a major concern in pediatric spinal deformity surgery.
Methods
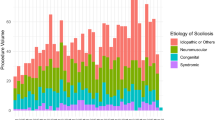
We performed a retrospective review of our primary scoliosis surgeries between 1999 and 2017. In 2008, we implemented a standardized infection reduction bundle. Interventions included preoperative nares screening for methicillin-resistant staphylococcus aureus or methicillin-sensitive Staphylococcus aureus 2 weeks preoperatively, and treatment with intranasal mupirocin when positive, a bath or shower the night before surgery, a preoperative chlorohexidine scrub, timing of standardized antibiotic administration, standardized intraoperative re-dosing of antibiotics, limiting operating room traffic, and standardized postoperative wound care. In 2011, we added intrawound vancomycin powder at wound closure. Our inclusion criteria were patients 21 years of age or less with idiopathic, neuromuscular, syndromic, or congenital scoliosis who had a primary spinal fusion or a same day anterior and posterior spine fusion with segmental spinal instrumentation of six levels or more. We compared the incidence of early (within 90 days of surgery) and late (> 91 days) SSI during the first postoperative year.
Results
There were 804 patients who met inclusion criteria: 404 in the non-bundle group (NBG) for cases prior to protocol change and 400 in the bundle group (BG) for cases after the protocol change. Postoperatively, there were 29 infections (7.2% of total cases) in the NBG: 9 early (2.2%) and 20 late (5.0%) while in the BG there were only 10 infection (2.5%): 6 early (1.5%) and 4 late (1.0%). The reduction in overall SSIs was statistically significant (p = 0.01). There was a trend toward decreased early infections in the BG, without reaching statistical significance (p = 0.14).
Conclusion
Standardized care bundles appear effective in reducing the incidence of postoperative pediatric spine SSIs.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical site infections (SSI) continue to be a significant concern in pediatric spinal deformity surgery. The associated costs of an infection can be overwhelming. A single SSI after pediatric spine deformity surgery can generate mean hospital charges of $154,537 [1]. This is in addition to the psychosocial cost on a family caring for their child, plus the real cost to them of lost work during their child’s hospitalization. From a public policy perspective, the Department of Health and Human Services has identified healthcare-associated infections as the most common type of complication for hospitalized patients and, in 2008, began not paying hospitals for the costs of treating such infections, deeming them preventable events. Furthermore, the Affordable Care Act’s Hospital Acquired Condition Reduction Program, implemented in 2015, reduces all payments to facilities in the lowest quartile for hospital-acquired conditions [2]. Due to significant patient morbidity and the myriad of negative repercussions resulting from SSIs, surgeons have made it a priority to identify modifiable risk factors and preventative strategies that can decrease the rate of SSIs in spinal deformity patients.
Nevertheless, SSIs continue to be a vexing problem for modern medicine and surgery. There are often no discernible inciting events for SSI. Even the effects of wound healing and intraoperative bacterial contamination on SSI rates, from a basic science perspective, are not fully understood [3, 4].
However, it is understood that different populations of patients with spinal deformity, including idiopathic, neuromuscular, syndromic, and congenital all carry unique underlying factors contributing to their spinal deformity. As a result, patient-specific risk factors for these subgroups also differ, as do the corresponding rates of SSIs. Published infection rates vary, but can range from as low as 0.5% in adolescent idiopathic scoliosis to upwards of 25% for patients with neuromuscular scoliosis [5, 6].
As most patient-specific risk factors cannot be modified, some surgeons have focused their efforts on standardizing care by employing preventative strategies to lower infection rate and by addressing modifiable risk factors, thereby minimizing the risk of SSI [7]. To that end, our institution developed a comprehensive, standardized infection reduction bundle in 2008. While surgeries prior to 2008 did have a standardized care path, this care path had minimal focus on SSI reduction and only included 24 h of prophylactic antibiotics. There were no changes to the preoperative antibiotics to cover MRSA or Gram-negative bacteria, and no focus on the time frame in which preoperative antibiotics were administered. The new infection reduction bundle focused specifically on minimizing risk factors for SSIs. Our interventions include preoperative nares screening for methicillin-resistant Staphylococcus aureus (MRSA) or methicillin-sensitive Staphylococcus aureus (MSSA) approximately 2 weeks preoperatively, and treatment with intranasal mupirocin when positive; a bath or shower the night before surgery; a preoperative chlorohexidine scrub immediately before surgery; timing of standardized antibiotic administration; standardized intraoperative re-dosing of antibiotics; limiting operating room (OR) traffic; and standardized postoperative wound care (Appendix). Minor modifications to the bundle occurred over time including adding vancomycin powder to the wound in 2011. We incorporated these changes into our existing care path for preoperative, intraoperative, and postoperative care of our pediatric spinal deformity patients.
Through a retrospective cohort design, we sought to understand if our new infection prevention bundle affected rates of SSI in primary posterior spinal fusion surgeries and segmental spinal instrumentation for pediatric spinal deformity.
Materials and methods
Using our Institutional Review Board (IRB)-approved Pediatric Orthopaedic Spine Database, we performed a retrospective review of our primary scoliosis surgeries between 1999 and 2017. This study was also IRB approved.
Our inclusion criteria were patients 21 years of age or less with a diagnosis of idiopathic, neuromuscular, syndromic, and congenital scoliosis who had a posterior spinal fusion or a same day anterior and posterior spine fusion with segmental spinal instrumentation of six levels or more, and a minimum of 1 year of postoperative follow-up.
We excluded patients with kyphosis, staged anterior and posterior procedures, anterior only procedures, growing rod procedures, and instrumentation of five levels or less.
Patients were assigned to the non-bundle group (NBG) for cases prior to the protocol change in 2008, or to the bundle group (BG) for cases after 2008. Patients in the NBG were treated only with cefazolin for 24 h, with no other infection reduction methods as part of their care. Our senior nurse practitioner was present in the OR for all spine surgeries in the NBG. Antibiotics were consistently discussed with anesthesia and administered, though timing of dosing related to incision was not mandated by a protocol and compliance was not specifically monitored. Patients in the BG were all treated in line with the standardized infection reduction bundle and were all followed by our senior pediatric orthopaedic nurse practitioner to ensure protocol adherence. To add further verification and eliminate bias, a pediatric infectious disease nurse independently monitored all spine surgeries for compliance. Lack of full compliance with all components of the bundle did not result in cancelling cases. Two specific components had compliance rates less than 100%: staph screens (99% compliance) and chlorhexidine wipes in the PACU (97%). We studied patient demographics, operative details, and the incidence of early (within 90 days of surgery) and late (> 91 days) infections between the two groups as described by the Centers for Disease Control [8].
Results
There were 804 consecutive patients who met inclusion criteria. There were 404 patients in the NBG and 400 patients in the BG. Due to the large number of patients, the demographics of both groups were very similar (Table 1). There were 251 patients with idiopathic scoliosis (IS) in the NBG and 237 patients in the BG; 116 patients with neuromuscular scoliosis (NMS) in the NBG and 118 patients in the BG; 26 patients with syndromic scoliosis in the NBG and 29 patients in the BG; and 11 congenital scoliosis patients in the NBG and 16 patients in the BG.
The mean age of the patients at surgery in both groups was also similar. The mean age of NBG patients with IS was 14 ± 2 years, NMS patients were 13.6 ± 2.6 years, syndromic patients were 14 ± 1.4 years, and congenital were 11.5 ± 1.6 years. The mean age of BG patients with IS was 14 ± 2 years, NMS patients was 13.9 ± 2.7 years, syndromic patients was 13.4 ± 2.5 years, and congenital was 12.7 ± 1.6 years. The mean preoperative major curve magnitude of NBG patients with IS was 57° ± 11°, NMS was 71° ± 20°, syndromic was 65° ± 20°, and congenital was 61° ± 14°. The mean preoperative curve magnitude of BG patients with IS was 56° ± 10°, NMS was 71° ± 20°, syndromic was 67° ± 15°, and congenital was 70° ± 16°. The mean follow-up of the NBG was 5.7 years ± 3.4 years and the BG was 3.3 years ± 2.1 years.
Surgery-specific variables were also examined to ensure similarity between groups, examining operative time (incision to closure), levels fused, and transfusion requirements. These findings are also outlined in Table 1.
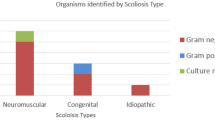
Postoperatively, there were 29 infections (7.2% of total cases) in the NBG: 9 early (2.2%) and 20 late (5.0%). This included 1 early and 14 late infections in the IS group, 5 early and 5 late in the NMS group, 3 early and 0 late in the syndromic group and 0 early and 1 late in the congenital group. The BG had ten infections (2.5% of total cases): six early (1.5%) and four late (1.0%). There were no early or late infections in the IS group, five early and four late in the NMS group, one early and zero late in the syndromic group and no early or late infections in the congenital group (Table 2).
The mean time to early infections was 18.9 days in NBG and 18.2 days in BG. The mean time to late infection in NBG was 4.1 years and 2 years in the BG. There was only one late infection in both groups within the first year.
Associated respiratory and urinary tract infections were also noted. There were six patients in the NBG who developed a postoperative UTI, one of which ultimately had an early SSI with Enterococcus faecalis. Three patients in the BG had a postoperative UTI, though none developed a postoperative SSI. Overall, there were 23 patients in the NBG who developed a postoperative respiratory complication (pneumothorax (6), pleural effusion (6), hemothorax (3), atelectasis (3), respiratory arrests (3), and aspiration pneumonia (2)), none of which had a subsequent SSI. In the BG, seven patients developed a postoperative respiratory complication [plural effusion (2), pneumothorax (2), aspiration pneumonia (1), hemothorax (1), pneumonia (1)], none of which developed a postoperative SSI.
The type of metal in the instrumentation was also noted between both groups (Table 3).
As all perioperative data were prospectively recorded in our Pediatric Orthopaedic Spine Database, we were able to document compliance with each component of the bundle throughout the study period, with 99% compliance for staph screens, 100% compliance for mupirocin treatment if positive staph screen, 97% compliance with chlorhexidine wipes in PACU, 100% compliance with vancomycin powder, and 100% compliance with antibiotic timing and redosing.
Overall, the reduction for all SSIs was statistically significant for (p = 0.01). There was a trend toward decreased infection rate for early infections, but this did not reach statistical significance (p = 0.14). Overall, we have had no early infections between November 2015 and now (May 2019).
Discussion
Implementing the infection bundle led to a statistically significant reduction in all SSIs. Twenty-nine of 404 patients (7.2%) in the NBG before the bundle were implemented developed postoperative infections, compared with only 10 of 400 patients (2.5%) in the BG after bundle implementation. While there was a trend toward decreased early infection rates in patients treated after the bundle was implemented, this did not reach statistical significance. We feel this was due to our low number of infection cases overall. Our incidence is currently even lower owing to no acute infections since November 2015.
We acknowledge that this study has limitations, including the single-center patient pool, the bundled enacting several changes at one time, and the retrospective methodology. Although our sample included a large number of patients, when splitting the analysis by diagnosis, the subgroups declined in size. It is difficult to provide an adequately large patient pool in each subgroup of spinal fusions by diagnosis in one center. Additionally, as an academic medical center, findings specific to our institution may not be applicable to the general population. However, the effect of intergroup variability on the results was minimized as the demographics between groups were very similar. Also, as any practice would over nearly 2 decades, our cohort of surgeons evolved, with some staying and gaining more experience, new surgeons joining, and some leaving. While each of these factors may have some effect, we would suggest it would not be substantially different than any other academic practice over such a length of time. Additionally, all surgeons followed the same infection reduction bundle, which decreases variability between individual surgeons. Temperature management of the patients during and immediately after surgery was not different between both groups. There was, however, a difference in blood loss between the groups, though aminocaproic acid was used in both groups. In 2009, a bipolar sealer was added to our tool box, which may explain the decrease in blood loss in the BG [9]. However, blood loss has not been demonstrated to affect the rate of SSIs in a systematic review of the literature [10]. Despite these limitations, this study provides evidence that a systematic, preoperative bundled approach can decrease SSIs in pediatric patients undergoing spinal surgery.
SSIs continue to be a significant problem after pediatric spine surgeries, but literature varies widely in reporting how commonly SSIs occur. SSI rates are reported between 0.5% and 25% for pediatric patients after scoliosis surgeries, depending on the underlying etiology [7, 11]. Additionally, infection rates vary widely among different institutions [12]. In 2016, Garg et al. retrospectively analyzed an 8-site multicenter database for patients implanted with VEPTR, and found the rate of SSIs ranged from 2.9 to 42.9% [12]. By standardizing protocols across centers, we can aim to optimize a bundle to decrease SSIs based on best evidence and practices.
The merits of standardized protocols to decrease SSIs has been demonstrated across disciplines in the surgical literature [13,14,15,16]. Stambough et al. found a decreased SSI rate in arthroplasty patients after implementation of an infection reduction care bundle, noting a 0.8% rate of SSIs before the bundle, and a 0.2% rate of SSIs after the bundle [13]. Additionally, Gorgun et al. found similar benefits of a standardized care bundle in colorectal cancer, reporting a decrease in SSI rates from 11.8 to 6.6% after the Colorectal Surgery SSI Prevention Bundle Protocol was implemented [16].
Specific to spinal surgery, multiple studies have shown that adhering to protocols decreases rates of SSIs [17,18,19]. In 2018, Lopez et al. investigated the impact of a Vancomycin and Cefazolin as a standard preoperative prophylactic antibiotic regiment on SSIs in adult spinal fusions [18]. The study involved comparing rates of SSIs before and after a standard antibiotic protocol. The authors found a significant reduction in SSI from 4 to 2%. Glotzbecker et al. compared infection rates in high-risk posterior spinal fusion pediatric patients before and after a multidisciplinary clinical pathway was implemented at their institution. The pathway was created in 2012, and the study examined rate of infection before and after implementation, finding that adherence to a multi-factorial protocol led to lower SSI rates, decreased cost associated with care, and ultimately improved patient outcomes [17]. In 2018, Vandenberg et al. studied a group of patients treated after a multidisciplinary task force updated protocols to address modifiable risk factors for SSI. The study compared rates of SSI in patients who were compliant with the protocol versus patients who were non-compliant and found that compliance with an antibiotic bundle was associated with decreased risk of developing an SSI in pediatric patients undergoing index or revision posterior spine fusion surgery [19].
Although evidence remains limited and sometimes contradictory, several recent studies have measured single-variable changes in care, which can add to the evidence supporting an optimal bundle for pediatric spinal fusion patients [20,21,22]. Yet not all components to a bundle have good supporting evidence as a single variable. For example, we addressed the timing of intravenous antibiotics. However, the literature reported conflicting findings on the importance of this aspect of care [7]. We also included preoperative nares screening for MRSA and MSSA. Previous studies suggest prophylactic screening and treatment of MRSA can improve SSI rates [23, 24]. We employed a pre-operative chlorohexidine scrub, which has suggested reduced rates of SSI in various surgical specialties; however, the effectiveness of this practice has not been demonstrated in pediatric patients with spinal deformities [25]. Additional aspects of the care bundle we implemented included minimizing OR traffic, although OR traffic has not been associated with increased risk of SSIs [26]. Finally, standardizing postoperative wound care was a component of our bundle, although there is insufficient evidence that specific wound care affects SSI rates in pediatric spine deformity surgeries [7].
Several recent studies have examined the effect of intra-wound vancomycin powder. There is variable reporting on the effect of vancomycin and risk of postoperative SSIs [27, 28, 21]. Garg et al. studied the effectiveness of topical vancomycin in a mixed population of pediatric patients undergoing primary or revision posterior spinal fusion. This study found that the use of intra-wound vancomycin was not effective in reducing SSIs in pediatric spine surgeries [27]. Contrary to the Garg et al. study, Thompson et al. studied early-onset scoliosis patients at our institution and found that that vancomycin was effective at reducing the rate of SSIs though their study was in an early-onset scoliosis population [28].
We acknowledge that the bundle did not test individual measures, but rather evaluated changes as a whole when quantifying reduction in infection rates. Further studies are needed to identify the benefits of individual preventative strategies added to infection reduction bundles, as well as any potential additive or synergistic benefit by combining several interventions. Although we were unable to provide evidence for each individual component, cumulatively we observed a decrease in infection rate after our bundle was enacted.
Surgical site infections remain a significant concern in pediatric spinal deformity surgery. Our bundled approach to infection reduction demonstrated a statistically significant decrease in SSIs. Further work is needed to optimize the interventions contained within a bundle utilizing larger standardized data sets, as well as investigations regarding individual interventions in specific patient subpopulations.
References
Hedequist D, Haugen A, Hresko T, Emans J (2009) Failure of attempted implant retention in spinal deformity delayed surgical site infections. Spine (Phila Pa 1976) 34(1):60–64. https://doi.org/10.1097/BRS.0b013e31818ed75e
Patrick Conway MD (2013) Testimony on U.S. Efforts To Reduce Healthcare-Associated Infections. Committee on Health, Education, Labor & Pensions. U.S. Department of Health & Human Services, https://www.hhs.gov/asl/testify/2013/09/t20130924.html
Bowler PG (2002) Wound pathophysiology, infection and therapeutic options. Ann Med 34(6):419–427
Gottrup F, Agren MS, Karlsmark T (2000) Models for use in wound healing research: a survey focusing on in vitro and in vivo adult soft tissue. Wound Repair Regen 8(2):83–96
Cahill PJ, Warnick DE, Lee MJ, Gaughan J, Vogel LE, Hammerberg KW, Sturm PF (2010) Infection after spinal fusion for pediatric spinal deformity: thirty years of experience at a single institution. Spine (Phila Pa 1976) 35(12):1211–1217. https://doi.org/10.1097/BRS.0b013e3181c212d1
Stella G, Ascani E, Cervellati S, Bettini N, Scarsi M, Vicini M, Magillo P, Carbone M (1998) Surgical treatment of scoliosis associated with myelomeningocele. Eur J Pediatr Surg 8(Suppl 1):22–25. https://doi.org/10.1055/s-2008-1071247
Mistovich RJ, Jacobs LJ, Campbell RM, Spiegel DA, Flynn JM, Baldwin KD (2017) Infection control in pediatric spinal deformity surgery: a systematic and critical analysis review. JBJS Rev 5(5):e3. https://doi.org/10.2106/JBJS.RVW.16.00071
CDC (2017) Surgical Site Infection (SSI) Event. https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf
Gordon ZL, Son-Hing JP, Poe-Kochert C, Thompson GH (2013) Bipolar sealer device reduces blood loss and transfusion requirements in posterior spinal fusion for adolescent idiopathic scoliosis. J Pediatr Orthop 33(7):700–706. https://doi.org/10.1097/BPO.0b013e31829d5721
Du JY, Poe-Kochert C, Thompson GH, Son-Hing JP, Hardesty CK, Mistovich RJ (2019) Risk factors for early infection in pediatric spinal deformity surgery: a multivariate analysis. Spine Deform 7(3):410–416. https://doi.org/10.1016/j.jspd.2018.09.011
Glotzbecker MP, Riedel MD, Vitale MG, Matsumoto H, Roye DP, Erickson M, Flynn JM, Saiman L (2013) What's the evidence? Systematic literature review of risk factors and preventive strategies for surgical site infection following pediatric spine surgery. J Pediatr Orthop 33(5):479–487. https://doi.org/10.1097/BPO.0b013e318285c507
Garg S, Cyr M, St Hilaire T, Flynn T, Carry P, Glotzbecker M, Smith JT, Sawyer J, Pahys J, Luhmann S, Flynn JM, El-Hawary R, Vitale M (2016) Variability of surgical site infection with VEPTR at eight centers: a retrospective cohort analysis. Spine Deform 4(1):59–64. https://doi.org/10.1016/j.jspd.2015.07.009
Stambough JB, Nam D, Warren DK, Keeney JA, Clohisy JC, Barrack RL, Nunley RM (2017) Decreased hospital costs and surgical site infection incidence with a universal decolonization protocol in primary total joint arthroplasty. J Arthroplasty 32(3):728–734e721. https://doi.org/10.1016/j.arth.2016.09.041
Crolla RM, van der Laan L, Veen EJ, Hendriks Y, van Schendel C, Kluytmans J (2012) Reduction of surgical site infections after implementation of a bundle of care. PLoS ONE 7(9):e44599. https://doi.org/10.1371/journal.pone.0044599
Harold RE, Butler BA, Lamplot J, Luu HH, Lawton CD, Manning D (2018) Multifaceted aseptic protocol decreases surgical site infections following hip arthroplasty. Hip Int 28(2):182–188. https://doi.org/10.5301/hipint.5000551
Gorgun E, Rencuzogullari A, Ozben V, Stocchi L, Fraser T, Benlice C, Hull T (2018) An effective bundled approach reduces surgical site infections in a high-outlier colorectal unit. Dis Colon Rectum 61(1):89–98. https://doi.org/10.1097/DCR.0000000000000929
Glotzbecker M, Troy M, Miller P, Berry J, Cohen L, Gryzwna A, McCann ME, Hresko MT, Goobie S, Emans J, Brustowitz R, Snyder B, Hedequist D (2019) Implementing a multidisciplinary clinical pathway can reduce the deep surgical site infection rate after posterior spinal fusion in high-risk patients. Spine Deform 7(1):33–39. https://doi.org/10.1016/j.jspd.2018.06.010
Lopez W, Rider SM, Nwosu K, Kazarian E, Blucher J, Schoenfeld E, Simpson A, Kang J, Schoenfeld AJ (2018) The impact of vancomycin and cefazolin as standard pre-operative antibiotic prophylaxis on surgical site infections following instrumented spinal fusion. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0000000000002839
Vandenberg C, Niswander C, Carry P, Bloch N, Pan Z, Erickson M, Garg S (2018) Compliance with a comprehensive antibiotic protocol improves infection incidence in pediatric spine surgery. J Pediatr Orthop 38(5):287–292. https://doi.org/10.1097/BPO.0000000000000812
Imahiyerobo T, Minkara AA, Matsumoto H, Vitale MG (2018) Plastic multilayered closure in pediatric nonidiopathic scoliosis is associated with a lower than expected incidence of wound complications and surgical site infections. Spine Deform 6(4):454–459. https://doi.org/10.1016/j.jspd.2017.12.009
Sweet FA, Roh M, Sliva C (2011) Intrawound application of vancomycin for prophylaxis in instrumented thoracolumbar fusions: efficacy, drug levels, and patient outcomes. Spine (Phila Pa 1976) 36(24):2084–2088. https://doi.org/10.1097/BRS.0b013e3181ff2cb1
Narayan P, Brown M, Gould J (2014) Use of silver-impregnated dressings to reduce neurosurgical infections. Childs Nerv Syst 30(11):1953
Chen AF, Wessel CB, Rao N (2013) Staphylococcus aureus screening and decolonization in orthopaedic surgery and reduction of surgical site infections. Clin Orthop Relat Res 471(7):2383–2399. https://doi.org/10.1007/s11999-013-2875-0
Schweizer ML, Chiang HY, Septimus E, Moody J, Braun B, Hafner J, Ward MA, Hickok J, Perencevich EN, Diekema DJ, Richards CL, Cavanaugh JE, Perlin JB, Herwaldt LA (2015) Association of a bundled intervention with surgical site infections among patients undergoing cardiac, hip, or knee surgery. JAMA 313(21):2162–2171. https://doi.org/10.1001/jama.2015.5387
Mackenzie WG, Matsumoto H, Williams BA, Corona J, Lee C, Cody SR, Covington L, Saiman L, Flynn JM, Skaggs DL, Roye DP Jr, Vitale MG (2013) Surgical site infection following spinal instrumentation for scoliosis: a multicenter analysis of rates, risk factors, and pathogens. J Bone Jt Surg Am 95(9):800–806. https://doi.org/10.2106/JBJS.L.00010(S801–S802)
Wanta BT, Glasgow AE, Habermann EB, Kor DJ, Cima RR, Berbari EF, Curry TB, Brown MJ, Hyder JA (2016) Operating room traffic as a modifiable risk factor for surgical site infection. Surg Infect (Larchmt) 17(6):755–760. https://doi.org/10.1089/sur.2016.123
Garg S, Bloch N, Potter M, Quick H, Palmer C, Michael N, O'Donnell C, Erickson M (2018) Topical vancomycin in pediatric spine surgery does not reduce surgical site infection: a retrospective cohort study. Spine Deform 6(5):523–528. https://doi.org/10.1016/j.jspd.2018.01.010
Thompson GH, Poe-Kochert C, Hardesty CK, Son-Hing J, Mistovich RJ (2018) Does vancomycin powder decrease surgical site infections in growing spine surgery?: a preliminary study. J Bone Jt Surg Am 100(6):466–471. https://doi.org/10.2106/JBJS.17.00459
Funding
No separate copyrights are held on the included material and all relevant IRB approval forms may be published. This study used our IRB-approved Pediatric Orthopaedic Spine Database and was IRB approved. No funding was required for this project.
Author information
Authors and Affiliations
Contributions
Study idea/design: CP-K, RJM. Data collection: CP-K, GHT, JPS-H, CKH, RJM. Statistical analysis: CP-K, JLS, RJM. Manuscript draft: CP-K, JLS, GHT, JPS-H, CKH, RJM. Manuscript review and revision: CP-K, JLS, GHT, JPS-H, CKH, RJM. Final approval: CP-K, JLS, GHT, JPS-H, CKH, RJM.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Poe-Kochert, C., Shimberg, J.L., Thompson, G.H. et al. Surgical site infection prevention protocol for pediatric spinal deformity surgery: does it make a difference?. Spine Deform 8, 931–938 (2020). https://doi.org/10.1007/s43390-020-00120-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00120-6