Abstract
Hematopoietic stem cell transplantation (HSCT) is one available curative treatment for sickle cell disease (SCD). The process of deciding in favor or against the procedure encompasses several factors, including the prospect of improving long-term quality of life (QoL). The present study aimed to assess the QoL indexes of adult patients with SCD who underwent allogeneic HSCT. In this descriptive, exploratory, cross-sectional study, patients were assessed before and at 1 and 2 years after transplantation, by the Generic Questionnaire for Quality of Life Assessment (SF-36). For each of the eight components of SF-36, the differences between assessments at each time point (pre-HSCT, 1 year, and 2 years) were compared. The population was composed of 14 patients (nine males) with a mean age of 28.07 years. The results showed significant increase in all eight components of the SF-36 in the three time points compared, evidencing that even long-term after the procedure, the QoL continues to increase. The physical components of SF-36 improved since the first year post-HSCT. Important variables for the preservation of QoL were detected: not having developed GVHD, being gainfully employed, and having more than 8 years of schooling. Importantly, there was also a delayed but significant increase in the mental component of SF-36, here shown as unprecedented data. These results reaffirm that it is worth investing in HSCT for sickle cell patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sickle cell disease (SCD) is one of the most common monogenic hereditary diseases in the world (Rees et al., 2018; Menezes et al., 2013). In Brazil, sickle cell anemia (SCA), the most severe form of SCD, affects one in every 1,000 live births, with an estimated 3,000 children with SCA born every year. The estimates indicate a prevalence of 20 to 30 thousand patients with SCA and more than seven million individuals with sickle cell trait in Brazil (Cançado et al., 2009).
Sickle cell patients are severely affected by the disease and often need to adjust to lifestyles that are different from those of the healthy population. Chronic pain, skin ulcers, neurological disability, and episodes of respiratory distress, among other manifestations, lead to frequent hospital admissions and distressing treatments. The repeated episodes of frustrations, limitations, and losses that characterize this disorder ultimately affect quality of life (QoL) (Menezes et al., 2013).
Allogeneic hematopoietic stem cell transplantation (HSCT) is the only curative treatment currently available for patients with SCD (Bhatia et al., 2015; Ferrari et al., 2017). Allogeneic HSCT is a procedure indicated, primarily, for life-threatening hematological diseases (leukemias, lymphomas, severe aplastic anemia), primary immunodeficiencies, and some inherited genetic disorders. In SCD patients, indications for HSCT comprise involvement of the central nervous system, alloimmunization against red blood cells, and recurrent vaso-occlusive episodes, including acute chest syndrome and priapism (Kanter et al., 2021). The procedure is divided into the following stages (Alves et al., 2012):
-
(1)
Pre-HSCT stage: involves an outpatient follow-up until hospitalization for the procedure. During this period, the patients undergo a series of evaluations and exams. The bone marrow donors also undergo simultaneous evaluations.
-
(2)
HSCT stage: the patients are hospitalized in exclusive and protective isolation rooms, for an expected period of 30 to 40 days. In this phase, they receive a transplant-conditioning regimen consisting of high doses of chemotherapeutic agents, frequently added to total body irradiation, in order to destroy the diseased bone marrow. There are several side effects associated with these agents, such as nausea, vomiting, diarrhea, headaches, hair loss, and others. The donor bone marrow is infused intravenously in the unit itself, at the patient’s bedside, over a maximum period of 6 h. After the infusion, the patients wait for a few days until the engraftment, when the leukocyte counts begin to increase, indicating adequate function of the newly infused bone marrow.
-
(3)
Post-HSCT stage: it begins with discharge from the hospital. The patients stay in the city, close to the transplant unit, for approximately 3 months for daily to weekly outpatient visits. After this period, they are allowed to return to their original home and will be evaluated at more spaced intervals. This follow-up period is divided into immediate post-HSCT (up to 6 months) and late post-HSCT (from the seventh month on).
In the immediate post-HSCT period, patients may develop graft-versus-host disease (GVHD), a potentially severe post-transplantation complication. In GVHD, the newly engrafted donor bone marrow cells react against the recipient’s tissues, causing inflammation and damage. The already outdated classification criteria divided GVHD into acute or chronic, according to the beginning of manifestations, before or after the 100th day after transplantation, respectively (Toubai et al., 2008). To date, a newer classification system takes into account pathophysiological mechanisms and clinical presentation of the manifestations (Filipovich et al., 2005). These criteria are considered more suitable, since GVHD has different clinical causes and mechanisms, which may overlap and occur regardless of time after HSCT.
Despite being a curative treatment and an opportunity for new perspectives to patients, according to Fredenburg and Silverman (2014), there are several side effects that can be experienced during transplantation, such as nausea, vomiting, diarrhea, and exhaustion. In addition, sores in the gastrointestinal tract, intestinal cramps, skin rashes, hair loss, liver damage, and even pneumonia can occur after HSCT. Some of the side effects also include weight loss, fever, fatigue, and skin changes, mainly darkening, jaundice, redness, and itching.
In Brazil, the Unified Health System (SUS) included HSCT as a therapeutic option for selected SCD patients, under the ordinance number 1,321, since December 21, 2015 (Brazil, 2015a, 2015b). Allogeneic HSCT is, therefore, a very recent procedure in Brazilian reality, requiring studies to better understand its effectiveness and possible interferences in patient quality of life.
Recent studies have shown that matched sibling allogeneic HSCT has a high survival rate, reaching 94% after 5 years (Bhatia & Sheth, 2015; Gluckman et al., 2017; Simões et al., 2016). Quality of life of SCD patients significantly increases after HSCT, especially within the first year of follow-up (Arnold et al., 2015; Bhatia et al., 2015). Several other studies addressing QoL of patients undergoing HSCT, especially in the setting of hematological malignancies, highlight the need to correlate several variables to understand the complexity of this construct. Multiple factors are pointed out as essential to study post-HSCT QoL, including clinical variables, diagnosis, time after HSCT, and development of GVHD; sociodemographic variables, income, education, gender, and age group; and psychological variables, stress, anxiety, and depression (Mastropietro, 2010; Goetzmann et al., 2006; Sociè et al., 2003).
The vast majority of the above-mentioned studies included participants under 18 years of age and restricted the follow-up to the first year after HSCT, leaving a big gap regarding QoL evaluation in other types of patients and long-term monitoring. Only two studies assessed QoL in adults who underwent HSCT (Gallo et al., 2018; Saraf et al., 2016), both showing improvement of QoL components after the procedure. Here, we aimed to determine the impact of HSCT on QoL of adult SCD patients, evaluating QoL indexes before and after the procedure, up to the 2-year post-transplantation time point.
Patients and Methods
Study Design
This descriptive, exploratory, and cross-sectional study was developed at the Bone Marrow Transplantation Unit from a public hospital in Brazil.
Participants
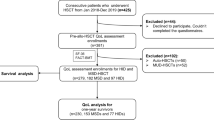
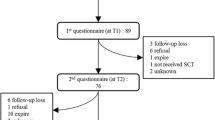
The Bone Marrow Transplantation Unit of the Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto, University of São Paulo, pioneered transplantation for SCD in Brazil, so far totaling 41 procedures, 20 of which in patients older than 18 years of age. Patients with severe forms of SCD and with available HLA-matched sibling donors are recruited from all regions of Brazil, specifically for HSCT. All adult patients transplanted between January 2003 and September 2018 were included: three died; thus their data were not collected, and three others did not complete follow-up, leaving a sample of 14 participants.
Patients were included if 18 years of age or older; having an established diagnosis of SCD; were under post-HSCT care at the outpatient clinic of the Bone Marrow Transplantation Unit at time of assessment, with minimum of 2 years of post-transplantation follow-up; and presenting conditions and willingness to voluntarily collaborate with the survey.
The population was composed of 14 participants, nine men and five women, with a maximum age of 42 years (M = 28.07; SD = 7.43), who fulfilled the inclusion criteria. Table 1 shows the sociodemographic characterization of the sample.
As shown in Table 1, the majority of the population was composed of men (9), aged from 25 to 42 years (8), with more than 8 years of schooling (8), single (11), not engaged in paid remuneration (11), and not having presented GVHD (10) or other clinical complications (8).
Instruments
The generic six-dimensional short form quality of life questionnaire, SF-36, was used to assess patient QoL. The questionnaire is a generic health assessment tool, multidimensional, originally created in English, easy to administer and understand, and translated and validated for Brazil (Ciconelli et al., 1999). The instrument consists of 36 questions, which measure eight domains of health status, divided into two major groups: (1) physical component, which encompasses functional capacity (FC), physical aspects (PA), pain (PAIN), and general health status (GHS), and (2) mental component, which covers vitality (VIT), social aspects (SA), emotional aspects (EA), and mental health (MH). From the answers obtained, each aspect is quantified on a scale ranging from 0 to 100, with 0 being a worse and 100 a better QoL score.
In addition to SF-36, a sociodemographic and clinical data form was also prepared by the authors to guide additional data collection from individual medical records and from face-to-face interviews. Additional data included age, marital status, educational level, city of origin, occupation, and complications associated with HSCT.
Procedure
The project was approved by the Research Ethics Committee of the Faculty of Philosophy, Sciences and Letters of Ribeirão Preto (FFCLRP-USP).
Data were individually collected on the days of medical appointments at the outpatient clinic, during a face-to-face interview in a psychology room, safeguarding the principles of comfort and privacy. Following each session of data collection, brief conversations were held with the participants, in order to verify their current needs. If necessary, psychological support was offered by the psychology team. Only one, among all participants of the study, accepted psychological care. This specific patient had been under psychological treatment for 2 years and was experiencing a marital crisis at the time data were collected. In addition, the consequences of her GVHD were impairing her ability to work, so she was not able to resume her job. Patients have routine psychological support during the hospitalization phase of transplant and also while at early months after the procedure. Once they are allowed to return to their original homes, psychological evaluations are spaced out and coincide with the scheduled outpatient medical appointments. Any specific demand for more frequent visits is handled by the patient’s primary health service, which includes psychological follow-up. This patient was referred for free psychological care in her city.
All participants agreed to participate voluntarily in the survey and signed written consent forms with the knowledge that they could withdraw their consent and leave the study at any time without any prejudice to their treatment.
Data Analysis
The SF-36 data were analyzed by two independent judges experienced in psychological assessment, one of them being the surveyor, who assessed the results and classified the protocols of the technique. Divergences between corrections were not found, as the instrument has a method of quantitative statistical correction.
Data from the analytical techniques underwent statistical analysis. Since the normal distribution was not assessed by the Shapiro–Wilk test, non-parametric analyses were applied. Subsequently, values obtained in the three assessments over time (Pre, Post 1 and Post 2) were compared by Friedman test, and when significant differences were found, the Wilcoxon test was used with Bonferroni correction to detect where the differences occurred. Significance was set at p ≤ 0.05.
The sociodemographic and clinical variables evaluated were gender (male, female), age (continuous), education (8 years of school or less, more than 8 years of school), occupation (yes, no), presence of GVHD (yes, no), and presence of other clinical complications (yes, no). To assess whether there was a significant difference between the SF36 components and the aforementioned variables, the Mann–Whitney (Z) test was applied. Patients were clustered according to each of the binomial variables (e.g., yes/ no), and compared through the non-parametric, unpaired test, resulting in a p and a Z value. For age, which is a continuous variable, the Pearson’s correlation test (ρ) was applied. Significance was set at p ≤ 0.05.
Results
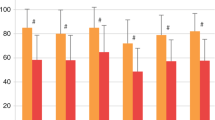
Table 2 presents the median scores from each of the eight components of the QoL, assessed by the SF-36 at the three different time points. From Table 2, it is possible to verify a progressive increase in the scores, all of which reached their highest mean at 2 years after the procedure.
At the pre-HSCT (Pre) time point, the two components with the highest median were MH (68) and FC (67.5), while the lowest were PA (0) and AE (07). At the Post 1 time point, the highest medians were pain (100), EA (91.5), and FC (90); the lowest was PA (59). At the Post 2 time point, the highest medians were PA, pain, SA, and EA components (100), while the lowest was VIT (80). The minimum values increase over time in six of the eight QoL components, and from Post 1 onwards, all domains reach maximum scores of 100.
Table 3 shows that the differences between Pre and Post 2 time points are statistically significant in all eight components, indicating that HSCT directly influences the increase in QoL presented by SCD patients.
At the Post 1 moment, a significant improvement was found in five of the eight QoL components: HR, BP, pain, GHS and MH. The absolute values continue to show an increase at Post 2 but with no significant difference. When comparing Pre and Post 2, all components show an increase, including VIT and AS, which had a more delayed, but progressive improvement.
Education
Considering the education variable, participants were divided into two groups (more or less than 8 years of schooling). A significant difference was observed only in GHS at Post 2, with the group of participants with more than 8 years of schooling showing significantly higher scores (p = 0.03). Trends (p < 0.10) were found in MH (Post 1), FC (Post 2), and VIT (Post 2) (Table 4).
Engagement in Remunerated Activity
At the pre-transplantation time point, higher values of PA (p = 0.008), GHS (p = 0.019), and EA (p = 0.054) were detected in patients engaged versus those non-engaged in remunerated activities. Trends (p < 0.10) were also found at the Post 1 moment concerning MH, EA, and VIT, favoring participants who were engaged in paid activities (Table 5).
Graft-Versus-Host Disease (GVHD)
At the Post 1 time point, participants who did not have GVHD presented higher scores in VIT (p = 0.03) and in MH (p = 0.01). Favorable trends (p < 0.10) were also found, for the same group, in MH scores at time Post 2 (Table 6).
Discussion
Here, we present an innovative work, since few studies have been dedicated to analyze the QoL of adult patients transplanted for SCD (Gallo et al., 2018; Saraf et al., 2016), and to our knowledge, it is the only study to evaluate QoL at late periods post-HSCT.
Participants were assessed at three time points: before the procedure and at 1 and 2 years after transplantation. Before HSCT, the QoL assessment indicates an impairment of several aspects of this construct in SCD patients, especially concerning the physical aspects. This physical impairment may result from partial or total loss of autonomy due to physical weaknesses, which are characteristic of this chronic condition, and, according to Menezes et al. (2013), from the deleterious impact of conventional treatment itself. These two aspects of the disease contribute to the patient’s decision to undergo HSCT (Khemani et al., 2018). A positive result, at the pre-transplantation time point, was the preservation of mental health, reflecting that even with limitations, patients found emotionally healthy ways to deal with the disease.
At 1 year after HSCT, the results became more homogeneous, decreasing the discrepancy between the participants’ HRQoL indicators among themselves, besides a general increase in the QoL numbers, although the physical aspects remained the most compromised. Improvements in the HRQoL indicators of patients with SCD at 1 year after HSCT were also observed by Saraf et al. (2016) and by Bathia et al. (2015), the latter also showing little improvement in physical aspects. In addition, patient QoL before transplantation may interfere in the post-HSCT results, as a possible reason for physical aspects having still remained at low levels at the Post 1 time point. In addition, we must take into account that HSCT is a highly complex treatment and that patients may still be distressed by side effects and complications of this procedure at the end of the first year of follow-up (Crovador et al., 2013).
At the 2 years after HSCT time point, the gains in QoL were even more evident, with a smaller discrepancy between individual scores and increases in component absolute values. According to research conducted with patients transplanted for other diseases, this recovery of the components in the late post-HSCT is expected (Alves et al., 2012; Crovador et al., 2013; Guimarães et al., 2010; Mastropietro et al., 2010a, 2010b, 2011; Oliveira et al., 2009).
On longitudinal analysis, the results here presented demonstrate the improvement in QoL of the participants throughout the evaluations. All components assessed by the SF-36 increased their mean scores, both between Pre and Post 1 and between Post 1 and Post 2, demonstrating that the improvement of QoL is sustained until 2 years after HSCT. It is no coincidence that all components of the SF-36 showed a significant difference between Post 2 and Pre, probably influenced by the new possibilities acquired in this period, such as going back to public places with many people, the possibility of interacting with pets, and restart sexual intercourse, among other common practices for most people, but that were restricted to this population because of their prolonged immunosuppression.
For physical components, the effectiveness of HSCT has been previously proven by other studies that evaluated patients with emphasis on the physical aspects of SCD, such as improvement of pain, resumption, or beginning of work activities, and functional capacity of the individual, among other aspects (Arnold et al., 2015; Cela et al., 2016). Fewer studies address components related to the mental health of these patients, and even when such evaluations are included, they tend to be partial (Cela et al., 2016; Kelly et al., 2012; Khemani et al., 2018). From our results, we observe that the mental components tend to improve after basic needs related to the physical components are met, such as pain reduction and functional capacity improvement, for example.
The rise in SF36 scores reflect the efficacy of HSCT regarding the more subjective aspects of QoL, generally not perceived by clinical evaluations, but which are extremely important for the well-being of those who undergo HSCT (Graves et al., 2016). These aspects were shown to be quite impaired in the Pre assessment, possibly influenced by the limitations imposed by the SCD, such as pain, physical fatigue, restrictions of social activities possible to participate in, and recurrent hospitalizations (Martins et al, 2010; Simões et al., 2016).
In this scenario, a question arises: which variables would be important for understanding this gain in QoL? From our analysis, we were able to identify three variables that were significant in this scenario: GVHD, having a paid activity, and education. Participants without GVHD had significantly higher scores in vitality and mental health at Post 1. Such data are important to understand that the impact of a physical illness is not restricted to this scope, also reflecting in more subjective aspects of QoL. GVHD is known to affect both the physical health and the QoL of patients undergoing HSCT (Mastropietro, 2010; Toubai et al., 2008), but we may now add a new item to this picture: the negative impact of GVHD on the mental components of QoL.
Enrolment in paid activity was another important variable. In the present study, 79% of the participants were unpaid, a rate even higher than that found by Silva et al., (1993), whose rate of unemployment was 57%. In that study, the most worrisome implication of the disease for adult patients was the difficulty of getting paid work. The challenges in keeping a formal job for non-transplanted patients with SCD are associated with the physical restrictions and unpredictable course of a chronic disease (Thomas & Lipps, 2011). Pain episodes, hospitalizations, and the treatment itself hinder attendance to work and school and may be associated with impairments of daily life activities. Indeed, one of the possible benefits of HSCT is to enable the patient to resume/develop a productive occupational life (Dias et al., 2012; Van Speybroeck, Adeniyi, & Hsu, 2016). According to Mastropietro et al. (2010b), higher income is also directly associated with better QoL. Income is strongly linked to paid activity and productivity and mirrors feelings of personal competence and psychological adjustment.
The influence of schooling on the preservation of QoL is another topic that warrants further understanding. In our study, we found that the group of participants with more than 8 years of schooling presented significantly higher scores in the general state of health at the 2 years after the HSCT time point. These data are not corroborated by the findings of Mastropietro et al. (2010b), which showed no relationship between formal level of education and QoL but are in line with the results of Marques et al. (2017), which described low education as a risk factor for QoL, suggesting that more educated patients would have a better understanding of the illness and treatment, contributing to better QoL. Another point to consider is the relationship between the severity of the disease and schooling. It is known that the most severe forms of SCD lead to school absences and consequent impairment of studies and school dropout. Therefore, the three variables, severity of the disease, schooling, and quality of life, influence each other.
The data presented here may endorse the efficacy of HSCT, regarding its influence on more subjective components of long-term QoL. Thus, the important improvements in aspects of QoL that impact patient daily lives, sustained over the 2-year follow-up, substantiate their decision to undergo HSCT (Khemani et al., 2018; O'Brien & Hankins, 2009; Roth et al., 2012).
Conclusions
The results herein described show improvements in the components that influence QoL at different time points in the 2 years that follow HSCT, revealing that they can increase over time after a medical procedure. In addition to time, we were able to detect other important variables that were associated with the preservation of QoL, such as absence of GVHD, engagement in a paid activity, and having more than eight years of schooling.
A limitation of the study is that the transplanted patients are those with the most severe disease and therefore do not represent the general population of sickle cell patients. This is an important aspect that needs to be emphasized in these studies.
This is an original longitudinal study with an unprecedented long-term follow-up of SCD patients after HSCT. Future studies should continue the assessment over the years, aiming to verify how health-related QoL evolves over even longer follow-up.
Data Availability
The data sets generated during and/or analyzed during the ongoing study are not publicly available due to ethical issues but are available from the corresponding author upon reasonable request.
Code Availability
Not applicable.
References
Alves, R. C. P., Oliveira-Cardoso, E. A., Mastropietro, A. P., Voltarelli, J. C., & Santos, M. A. (2012). Transplante de células-tronco hematopoéticas e qualidade de vida após a alta hospitalar. Psicologia, Saúde & Doenças, 13(1), 87–99.
Arnold, S. D., Jin, Z., Sands, S., Bhatia, M., Kung, A. L., & Satwani, P. (2015). Allogenic hematopoietic cell transplantation for children with sickle cell disease is beneficial and cost-effective: A single-center analysis. Biology of Blood and Marrow Transplantation, 21(7), 1258–1265. https://doi.org/10.1016/j.bbmt.2015.01.010
Bhatia, M., Kolva, E., Cimini, L., Jin, Z., Satwani, P., Savone, M., George, D., Garvin, J., Paz, M. L., Briamonte, C., Cruz-Arrieta, E., & Sands, S. (2015). Health- related quality of life after allogenic hematopoietic stem cell transplantation for sickle cell disease. Biology of Blood and Marrow Transplantation, 21(4), 666–672. https://doi.org/10.1016/j.bbmt.2014.12.007
Cançado, R. D., Lobo, C., Angulo, I., Araújo, P. I. C., & Jesus, J. A. (2009). Protocolo clínico e diretrizes terapêuticas para uso de hidroxiureia na anemia falciforme. Revista Brasileira De Hematologia e Hemoterapia, 31(5), 361–366. https://doi.org/10.1590/S1516-84842009005000076
Cela, E., Vélez, A. G., Aguado, A., Medín, G., Bellón, J. M., & Beléndez, C. (2016). Chronic brain damage in sickle cell disease and its relation with quality of life. Medicina Clinica, 147(12), 531–536. https://doi.org/10.1016/j.medcle.2016.12.041
Ciconelli, M. R., Ferraz, B. M., Santos, W., Meinão, I., & Quaresma, R. M. (1999). Tradução para a língua portuguesa e validação do questionário genérico de avaliação de qualidade de vida SF 36 (Brasil SF 36). Revista Brasileira De Reumatologia, 39(3), 209–214.
Crovador, L. F., Oliveira-Cardoso, E. A., Mastropietro, A. P., & Santos, M. A. (2013). Qualidade de vida relacionada à saúde de pacientes com esclerose múltipla antes do transplante de células-tronco hematopoéticas. Psicologia: Reflexão e Crítica, 26(1), 58–66. https://doi.org/10.1590/S0102-79722013000100007
Dias, V. N., Mastropietro, A. P., Oliveira-Cardoso, E. A., & De Carlo, M. M. R. P. (2012). Transplante de células-tronco hematopoéticas – Um estudo controlado sobre papéis ocupacionais. Caderno De Terapia Ocupacional UFSCAR, 20(2), 165–171. https://doi.org/10.4322/cto.2012.016
Ferrari, G., Cavazzana, M., & Mavilio, F. (2017). Gene therapy approaches to hemoglobinopathies. Hematology/oncology Clinics of North America, 31(5), 835–852. https://doi.org/10.1016/j.hoc.2017.06.010
Filipovich, A. H., Weisdorf, D., Pavletic, S., Socie, G., Wingard, J. R., Lee, S. J., Martin, P., Chien, J., Przepiorka, D., Couriel, D., Cowen, E. W., Dinndorf, P., Farrell, A., Hartzman, R., Henslee-Downey, J., Jacobsohn, D., McDonald, G., Mittleman, B., Rizzo, J. D., … Flowers, M. E. (2005). National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biology Blood Marrow Transplantation, 11(12), 945–56. https://doi.org/10.1016/j.bbmt.2005.09.004
Fredenburg, H. A., & Silverman, M. J. (2014). Effects of music therapy on positive and negative affect and pain with hospitalized patients recovering from a blood and marrow transplant: A randomized effectiveness study. The Arts in Psychotherapy, 41, 174–180. https://doi.org/10.1016/j.aip.2014.01.007
Gallo, A. M., Patil, C., Adeniyi, T., Hsu, L. L., Rondelli, D., & Saraf, S. (2018). Health-related quality of life and personal life goals of adults with sickle cell disease after hematopoietic stem cell transplantation. West Journal Research, 41(4), 555–575. https://doi.org/10.1177/0193945918768277
Gluckman, E., Cappelli, B., Bernaudin, F., Labopin, M., Volt, F., Carreras, J., Simões, B. P., Ferster, A., Dupont, S., de la Fuente, J., Dalle, J. H., Zecca, M., Walters, M. C., Krishnamurti, L., Bhatia, M., Leung, K., Yanik, G., Kurtzberg, J., Dhedin, N., … Eapen, M. (2017). Sickle cell disease: An international survey of results of HLA-identical sibling hematopoietic stem cell transplantation. Blood, 129(11), 1548–1556. https://doi.org/10.1182/blood-2016-10-745711
Goetzmann, L., Klaghofer, R., Wagner-Huber, R., Halter, J., Boehler, A., Muellhaupt, B., Schanz, U., & Buddeberg, C. (2006). Quality of life and psychosocial situation before and after a lung, liver or an allogeneic bone marrow transplantation. Swiss Medical Weekly, 136, 281–290.
Guimarães, F. A. B., Oliveira-Cardoso, E. A., Mastropietro, A. P., Voltarelli, J. C., & Santos, M. A. (2010). Impact of autologous hematopoetic stem cell transplantation on the quality of life of patients with multiple sclerosis. Arquivos De Neuro-Psiquiatria, 68(4), 522–527. https://doi.org/10.1590/S0004-282X2010000400009
Graves, J. K., Hodge, C., & Jacob, E. (2016). Depression, anxiety, and quality of life in children and adolescents with sickle cell disease. Pediatric Nursing, 42(3), 113–119.
Kanter, J., Liem, R. I., Bernaudin, F., Bolaños-Meade, J., Fitzhugh, C. D., Hankins, J. S., Murad, M. H., Panepinto, J. A., Rondelli, D., Shenoy, S., Wagner, J., Walters, M. C., Woolford, T., Meerpohl, J. J., & Tisdale, J. (2021). American Society of Hematology 2021 guidelines for sickle cell disease: Stem cell transplantation. Blood Advance, 5(18), 3668–3689.
Kelly, M. J., Pennarola, B. W., Rodday, A. M., & Pearsons, S. K. (2012). Health-related quality of life (HRQL) in children with sickle cell disease and thalassemia following hematopoietic stem cell transplant (HSCT). Pediatric Blood & Cancer, 59(4), 725–731. https://doi.org/10.1016/j.bbmt.2014.12.007
Khemani, K., Ross, D., Sinha, C., Haight, A., Bakshi, N., & Krishnamurti, L. (2018). Experiences and decision making in hematopoietic stem cell transplant in sickle cell disease: Patients’ and caregivers’ perspectives. Biology of Blood and Marrow Transplantation, 24(5), 1041–1048. https://doi.org/10.1016/j.bbmt.2017.11.018
Marques, A. C. B., Proença, S. F. F. S., Machado, C. A. M., Guimarães, P. R. B., Bettencourt, P. R., Maftum, M. A., & Kalinke, L. P. (2017). Qualidade de vida nos primeiros seis meses pós-transplante de células-tronco Hematopoéticas. Texto & Contexto-Enfermagem, 26(3), 5040016. https://doi.org/10.1590/0104-07072017005040016
Martins, P. R. J., Moraes-Souza, H., & Silveira, T. B. (2010). Morbimortalidade em doença falciforme. Revista Brasileira De Hematologia e Hemoterapia, 32(5), 378–383. https://doi.org/10.1590/S1516-84842010000500010
Mastropietro, A. P., Oliveira-Cardoso, E. A., Simões, B. P., Voltarelli, J. C., & Santos, M. A. (2010a). Impacto da DECH crônica na qualidade de vida pós-TCTH alogênico. Revista Brasileira De Hematologia e Hemoterapia, 32(5), 358–364. https://doi.org/10.1590/S1516-84842010000500007
Mastropietro, A. P., Oliveira-Cardoso, E. A., Simões, B. P., Voltarelli, J. C., & Santos, M. A. (2010b). Relação entre renda, trabalho e qualidade de vida de pacientes submetidos ao transplante de medula óssea. Revista Brasileira De Hematolologia e Hemoterapia, 32(2), 102–107. https://doi.org/10.1590/S1516-84842010005000035
Mastropietro, A. P., Oliveira-Cardoso, E. A., & Santos, M. A. (2011). Vida ocupacional de pacientes sobreviventes ao transplante de medula óssea: Estudo exploratório. Revista Brasileira De Orientação Profissional, 12(2), 241–252.
Menezes, A. S. O. P., Len, C. A., Hilário, M. O. E., Terreri, M. T. R. A., & Braga, J. A. P. (2013). Qualidade de vida em portadores de doença falciforme. Revista Paulista De Pediatria, 31(1), 24–29. https://doi.org/10.1590/S0103-05822013000100005
O’Brien, S. H. O., & Hankins, J. S. (2009). Decision analysis of treatment strategies in children with severe sickle cell disease. Journal of Pediatric Hematology/oncology, 31(11), 873–878. https://doi.org/10.1097/MPH.0b013e3181b83cab
Roth, M., Krystal, J., Manwani, D., Driscoll, C., & Ricafort, R. (2012). Stem cell transplant for children with sickle cell anemia: Parent and patient interest. Biology of Blood and Marrow Transplantation, 18(11), 1709–1715. https://doi.org/10.1016/j.bbmt.2012.05.013
Saraf, S. L., Oh, A. L., Patel, P. R., Jalundhwala, Y., Sweiss, K., Koshy, M., Campbell-Lee, S., Gowhari, M., Hassan, J., Peace, D., Quigley, J. G., Khan, I., Molokie, R. E., Hsu, L. L., Mahmud, N., Levinson, D. J., Pickard, A. S., Garcia, J. G., Gordeuk, V. R., & Rondelli, D. (2016). Nonmyeloablative stem cell transplantation with alemtuzumab/low-dose irradiation to cure and improve the quality of life of adults with sickle cell disease. Biology of Blood and Marrow Transplantation, 22(3), 441–448. https://doi.org/10.1016/j.bbmt.2015.08.036
Silva, R. B. P., Ramalho, A. S., & Cassorla, R. M. S. (1993). A anemia falciforme como problema de Saúde Pública no Brasil. Revista De Saúde Pública, 27(1), 54–58.
Simões, B. P., Pieroni, F., Costa, T., Barros, G. N., Darrigo, G Jr., Grecco, C. S., Bernardes, J. E., Moraes, D., Stracieri, A. B. L., Cunha, R., & Rodrigues, M. C. (2016). Allogenic bone narrow transplantation in sickle-cell diseases. Revista da Associação Médica Brasileira, 62(1), 16–22. https://doi.org/10.1590/1806-9282.62.Suppl1.16
Sociè, G., Salloja, N., Cohen, A., Rovelli, A., Carreras, E., Locasciulli, A., Korthof, E., Weis, J., Levy, V., & Tichelli, A. (2003). Nonmalignant late effects after allogeneic stem cell transplantation. Blood, 101(9), 3373–3385. https://doi.org/10.1182/blood-2002-07-2231
Thomas, J. A., & Lipps, G. E. (2011). Subjective well-being of adults with homozygous sickle cell disease in Jamaica. Western Indian Medical Journal, 60(1), 181–187.
Toubai, T., Sun, Y., & Reddy, P. (2008). GVHD pathophysiology: Is acute different from chronic? Best Practice & Research Clinical Haematology, 21(2), 101–117. https://doi.org/10.1016/j.beha.2008.02.005
Funding
This research was funded by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Author information
Authors and Affiliations
Contributions
Lucas dos Santos Loterio was the principal researcher, responsible for collecting data and preparing the manuscript, during his master’s degree. Érika Arantes de Oliveira-Cardoso was the researcher–advisor, contributing to the conduction of the research and preparing the manuscript. Belinda Pinto Simões and Maria Carolina de Oliveira were the heads of the departments where the research was conducted and allowed it to happen, as well as participating in the writing and revision of the manuscript. Juliana Tomé Garcia and Ana Luisa Guimarães assisted in data collection. Karla, Thalita, Renato, and Manoel participated in the revision of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The project was approved by the Research Ethics Committee of the Faculty of Philosophy, Sciences and Letters of Ribeirão Preto (FFCLRP-USP), on an Ordinary Meeting, on August 24th, 2017, CAAE nº 72589517.7.0000.5407.
Consent to Participate
All participants agreed to participate voluntarily in the survey and signed written consent forms with the knowledge that they could leave the study at any time without any harm in their treatment.
Consent for Publication
The consent forms the participants signed also informed them that the data collected could be published for educational purposes.
Conflict of Interest
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
dos Santos Lotério, L., de Oliveira-Cardoso, É.A., Simões, B.P. et al. Quality of Life of Sickle Cell Disease Patients After Hematopoietic Stem Cell Transplantation: a Longitudinal Study. Trends in Psychol. 30, 513–527 (2022). https://doi.org/10.1007/s43076-021-00132-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43076-021-00132-9