Abstract
Endometriosis (EM) is a common gynecologic condition that often leads to infertility in women of reproductive age. Cell adhesion molecule 2 (CADM2) is involved in maintaining cell adhesion and polarity, as well as suppressing tumors. However, the role and mechanism of CADM2 in endometriosis is unclear. Therefore, this study evaluated the expression levels of CADM2 and epithelial-mesenchymal transition (EMT)-related marker proteins (E-cadherin, α-SMA, and N-cadherin). Compared to normal endometrial tissue, CADM2 was expressed at low levels in ectopic endometrial tissue from patients with EM. We performed clone formation assays, wound healing assays, and Transwell cell invasion assays to investigate the effects of CADM2 on the biological behavior of endometriosis epithelial cells (11Z) and ectopic endometrial stromal cells (EESCs). The growth, migration, and invasion abilities of these cells were significantly inhibited by overexpression of CADM2. The results were reversed after the knockdown of CADM2. Finally, western blotting (WB) was utilized to detect the effect of CADM2 on EMT in endometriosis cells. CADM2 inhibited EMT in endometriosis cells. In conclusion, our study suggests that CADM2 is a negative regulator of endometriosis development and may inhibit endometriosis development by suppressing EMT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometriosis (EM) is a long-term inflammatory disorder that is dependent on estrogen [1]. Approximately one-tenth of females of reproductive age experience endometriosis [2]. The disease can affect the ovaries, fallopian tubes, and endometrium in different ways, impairing their normal biological functions and causing dysmenorrhea, pelvic pain, infertility, and other clinical symptoms [3]. There are various theories that have been proposed to explain the pathogenesis of endometriosis [4]. Sampson's suggestion in the 1920s of retrograde menstruation is the most broadly accepted [5]. Nevertheless, this theory cannot explain all endometriosis. In clinical practice, non-invasive and accurate methods for diagnosis are lacking, leading to low diagnostic rates and poor clinical outcomes.
During tissue development, cells are divided into two main categories: epithelial and mesenchymal. Epithelial cells are usually tightly connected, forming an impermeable barrier. Mesenchymal cells, on the other hand, are loosely connected and highly motile. Since most tumors originate in the epithelium, the tight junctions between the epithelial cells limit their motility. Therefore, primary tumors need to undergo mesenchymal transformation in order to metastasize to distant sites. It has been shown that epithelial-mesenchymal transition (EMT) plays a crucial role in the metastasis of tumor cells [6,7,8]. Endometriosis resembles tumors in various biobehavioral characteristics. Matsuzaki and Darcha found that the endometrium in women forms during embryonic development from mesodermal tissue through the transformation of mesenchymal cells to epithelial cells. The transformed endometrial epithelium retains some imprints associated with its mesenchymal origin. Therefore, it is particularly susceptible to reverting to its original state through EMT [9]. In addition, insufficient expression of markers on epithelial cells in endometriotic foci in the pelvic peritoneum and ovaries of patients with endometriosis. On the contrary, the expression of markers in mesenchymal cells is upregulated [10]. Chen et al. used bioinformatics to analyze the key pathways related to the pathogenesis of endometriosis. The EMT ranked first in Hallmark pathway enrichment [11]. Therefore, we focused on investigating the effects of the EMT signaling pathway on endometriosis in this study.
Cell adhesion molecules (CAMs) are a class of proteins present on cell surfaces. They can mediate cell-to-cell or cell-to-extracellular matrix (ECM) binding and adhesion and then participate in cell migration, adhesion, signaling, and other biological processes. The common CAMs are calreticulin, selectins, members of the immunoglobulin family, and integrins [12, 13]. Normal functioning of these molecules is important for maintaining tissue structure. In the early twenty-first century, Witz et al. demonstrated that particular CAMs participate in the progression of early endometriosis lesions [14]. Furthermore, unique CAMs expressed by ectopic endometrial tissue may contribute to the persistence of endometriotic lesions. This was also demonstrated in a series of subsequent studies. Cell adhesion molecule 2 (CADM2) is a member of the large immunoglobulin superfamily (IgSF). It forms an immunoglobulin superfamily together with the highly homologous CADM1, CADM3 and CADM4. The CADM family has been reported to act as tumor suppressors. Previous studies found CADM1 to promote communication between neurons [15, 16]. Moreover, poor prognosis in neuroblastoma patients may be attributed in CADM1 deletions in chromosomes [17]. In recent years, CADM1 expression has been shown to be absent or significantly decreased in several malignant tumors, such as ovarian cancer [18], cervical cancer [19], malignant melanoma [20], breast cancer [21], and gastric cancer [22]. Qin et al. found that the expression of CADM3-AS1 was downregulated in smoke-induced malignant transformed cells and lung cancer and correlated with poor patient prognosis. In addition, CADM4 was found consistently in a variety of tumor tissues or tumor cells [23,24,25]. CADM2 was the last member of the family to be discovered [26]. A study found that CADM2 expression levels were significantly lower in hepatocellular carcinomas with venous metastases than those without venous metastases [27]. In addition, low expression of CADM2 is an independent risk factor for recurrence after hepatectomy [28]. Meanwhile, Li et al. reported that in hepatocellular carcinoma (HCC), CADM2 acts as a tumor suppressor. Up-regulation of CADM2 expression inhibits EMT in HCC cells, thereby affecting HCC cell metastasis [29]. Although many studies have examined the association between CADM family members and disease, little is known about the association between CADM2 and endometriosis.
Here, we identified CADM2 as a negative regulator of endometriosis, inhibiting endometriosis progression by suppressing the EMT process. Our findings indicate that CADM2 might be a promising candidate for treating endometriosis.
Materials and Methods
Sample collection and preparation
Eutopic and ectopic endometrial tissues were obtained from 35 patients undergoing laparoscopic ovarian cystectomy between January and August 2021 at the Department of Reproductive Medicine of the Affiliated Hospital of Shandong Second Medical University. These patients were subsequently diagnosed with endometriosis. Samples of normal endometrial tissue from non-EM patients undergoing hysterectomy for uterine fibroids or high-grade cervical intraepithelial neoplasia during the same period were taken as controls [30]. The inclusion criteria were normal menstrual cycle, complete case data, no hormonal therapy within the previous three months, and no intrauterine device (IUD). The ethics committee of the Affiliated Hospital of Shandong Second Medical University approved all experiments involving human tissue samples (approval number: Wyfy-2023-ky-280). All patients were informed and provided signed consent prior to specimen collection.
Immunohistochemistry
The collected tissues were promptly fixed in 4% buffered formalin. Immunohistochemistry (IHC) staining was done with primary antibodies against CADM2 (1:200; Genxspan, USA), E-cadherin (1:200; Cell Signaling Technology, USA), α-smooth muscle actin (α-SMA) (1:200, Abcam, USA), and N-cadherin (1:200, Cell Signaling Technology, USA). Two pathologists conducted the scoring in a double-blind manner, taking into account the level of staining and the proportion of positive cells. The ultimate score was obtained by adding the two scores together: 1–2 (negative), 3–4 (weakly positive), 5–7 (moderately positive), and > 7 (strongly positive). The degree of dyeing was categorized in the following manner: 0 (cell uncolored), 1 (light yellow), 2 (pale brown), 3 (yellow–brown), and 4 (tan). The grading of the percentage of positive cells was as follows: 0 (0), 1 (< 25%), 2 (25–50%), 3 (51–75%), and 4 (˃75%). The method was performed as previously outlined [31].
Cell culture
The endometriosis epithelial cell line (11Z) was created by Prof. Anna Strazinski-Powitz [32] and provided by Prof. Sunwei Guo, Fudan University. Ectopic endometrial tissue from patients with ovarian EM was collected and cut into pieces of approximately 1 mm3. Digested tissue fragments with 4% type IV collagenase (Sigma, USA) for 90 min at 37 °C. At the end of digestion, ectopic endometrial stromal cells (EESCs) were isolated by a 400-mesh wire sieve. The above cells were cultured in Dulbecco’s modified Eagle medium/Ham’s F-12 50/50 mix (DMEM/F-12), supplemented with 10% fetal bovine serum (FBS, Gibco), 100 U/mL penicillin, and 100 μg/mL streptomycin. The cells were maintained at 37 °C in a 5% CO2 incubator with a humidifying environment.
Transfection
Inoculate the cells in a 6-well plates and incubate for 24 h. Lipo 2000 (Beyotime, Shanghai, China) was used according to the manufacturer’s guidelines to transfect the plasmids and siRNA into the cells. The siRNA against CADM2 was 5'-UUCAACAACGGUUACAUUCUG-3'. The siRNA sequence used as the negative control was 5'-UUCUCCGAACGUGUCACGUTT-3'.
Colony formation assay
The cells that had been transfected were reintroduced into 6-well plates (400 cells per plate). After 9–12 days of cultivation, the cells were immobilized using 4% paraformaldehyde for a duration of 10 min, followed by a 15 min staining with crystal violet, and photographed.
Wound healing assay
After the cells had been seeded again in 6-well plates, once the cell growth fusion reached 100%, a line was drawn in the center of the cells at the bottom of the petri dish using a pipette tip. The cells were then washed with PBS and photographed. After 24 h, the cells were again photographed.
Transwell invasion assay
Matrigel (BD Biosciences, USA) diluent (40 μL) was added to the Transwell upper chamber, where it underwent incubation at 37 °C for 1 h for gel solidification. Resuspended cells were inoculated into the Transwell upper chamber, and the lower chamber was supplemented with DMEM (600 μL). The cells were incubated in a cell incubator for 48 h. Paraformaldehyde was added to the Transwell upper chamber to fix the submembrane cells, which were then dyed with crystal violet. Cells were counted using a microscope.
Western blot analysis
Total protein was extracted from cells using P0013 lysis buffer (Beyotime, Shanghai, China). The protein was then separated by molecular size with SDS-PAGE, and transferred to a polyvinylidene fluoride (PVDF) membrane. After blocking the PVDF membrane with 5% skim milk at room temperature for 1 h, it was incubated with the primary antibody overnight at 4 °C. The membrane was washed three times with TBST and then incubated with the secondary antibody at room temperature for at least 1 h. Detection and imaging of signals on membranes was done using the Odyssey infrared imaging system, as previously outlined [31].
Statistical analysis
This study’s results were derived from three separate experiments. The analysis was conducted utilizing one-way ANOVA and Student’s t-test through GraphPad Prism version 9.0. P < 0.05 was considered statistically significant.
Results
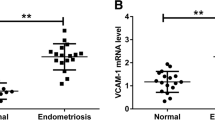
The distribution of CADM2 and EMT-related proteins in endometriosis
IHC techniques were employed to explore the distribution of CADM2 and proteins associated with EMT in patients with EM. Normal endometrial tissue from non-EM patients was used as a control for comparison. The IHC staining indicated that CADM2 was abundantly present in the glandular and mesenchymal tissues of normal endometrium and was localized predominantly to the cellular membrane and cytoplasmic regions. Ectopic endometrium exhibited a significant decrease in CADM2 and E-cadherin levels compared to normal and eutopic endometrium. In contrast, α-SMA and N-cadherin expression levels were notably elevated in ectopic endometrium (Fig. 1a and b). Moreover, we examined the association between CADM2 and proteins implicated in EMT. As shown in Fig. 1c, there was a positive association between CADM2 and E-cadherin expression and a negative correlation with α-SMA and N-cadherin expression.
The distribution of cell adhesion molecule 2 (CADM2) and epithelial-mesenchymal transition (EMT)-related proteins in endometriosis. a Immunohistochemical analysis was performed for CADM2, E-cadherin, α-smooth muscle actin (α-SMA), and N-cadherin across normal, eutopic, and ectopic endometrium. (Scale bars, 50 μm). b The normal, eutopic, and ectopic endometrium were subjected to semi-quantitative immunohistochemical analysis for CADM2, E-cadherin, α-SMA, and N-cadherin. All experiments were repeated at least three times. Data are shown as the mean ± standard deviation. *P < 0.05, ** P < 0.01, *** P < 0.001, and **** P < 0.0001. c A Pearson correlation assessment was performed to determine the relationship between the expression of CADM2 and those of E-cadherin, α-SMA, and N-cadherin in ectopic tissues
Overexpression of CADM2 inhibits cell growth, migration, and invasion in endometriosis cells
To understand the role of CADM2 in endometriosis, we overexpressed CADM2 in 11Z and EESCs by plasmid transfection and examined its expression level by western blot assay. CADM2 was successfully overexpressed in the above two cells (Fig. 4a). The growth of 11Z and EESCs was hindered by the overexpression of CADM2, as determined through a colony formation assay (Fig. 2a). In addition, wound healing and Transwell invasion assays revealed a decrease in cellular migration and invasion when CADM2 was overexpressed (Fig. 2b and c). In conclusion, the overexpression of CADM2 had a detrimental effect on the growth, migration, and invasion behavior of the endometriotic cells.
Overexpression of CADM2 inhibits cell growth, migration, and invasion in endometriosis cells. 11Z and EESCs were transfected with CADM2 overexpression plasmid (ex-CADM2) or empty vector (Vector), re-inoculated into 6-well plates the next day, and then lysed for western blotting after 48 h. a The influence of CADM2 on the growth of 11Z and EESCs was evaluated using a colony formation assay. b The influence of CADM2 on the migration abilities of 11Z and EESCs was evaluated using a wound healing assay. c The influence of CADM2 on the invasive abilities of 11Z and EESCs was evaluated using a Transwell invasion assay. All experiments were repeated at least three times. Data are presented as the mean ± standard deviation. The Student’s t-test was used for data analysis. ** P < 0.01, and.*** P < 0.001
Knockdown CADM2 promotes cell growth, migration, and invasion in endometriosis cells
To explore the effect of CADM2 knockdown on the biological behavior of endometriosis cells, CADM2 was knocked down in 11Z and EESCs. Western blot results showed that CADM2 was successfully knocked down in the two cell lines (Fig. 4b). Inhibiting CADM2 expression in the 11Z and EESCs promoted cell growth, as determined by the colony formation assay (Fig. 3a). Furthermore, as shown in Fig. 3b and c, the downregulation of CADM2 led to enhanced cell migration and invasion, as demonstrated by the results of the wound healing and Transwell invasion assays. In conclusion, the decreased expression of CADM2 facilitated the growth, migration, and invasion of the endometrial cells.
The knockdown of CADM2 promotes cell growth, migration, and invasion of endometriosis cells. 11Z and EESCs were transfected with CADM2 small interfering RNA (si-CADM2) or control siRNA (si-NC), re-inoculated into 6-well plates the next day, and then lysed for western blotting after 48 h. a The influence of CADM2 on the growth of 11Z and EESCs was evaluated using a colony formation assay. b The influence of CADM2 on the migration abilities of 11Z and EESCs was evaluated using a wound healing assay. c The influence of CADM2 on the invasive abilities of 11Z and EESCs was evaluated using a Transwell invasion assay. All experiments were repeated at least three times. Data are presented as the mean ± standard deviation. The Student’s t-test was used for data analysis. *** P < 0.001, **** P < 0.0001
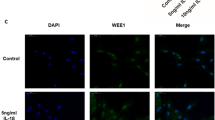
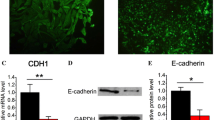
CADM2 inhibits EMT in endometriosis cells
Cells acquire migratory and invasive capabilities through EMT. In addition, EMT has been shown to be involved in the pathogenesis of endometriosis [11]. Therefore, we used western blotting to investigate whether CADM2 affects the EMT process in endometriosis. As shown in Fig. 4a and b, the upregulation of CADM2 expression in 11Z and EESCs was followed by increased levels of E-cadherin and decreased levels of α-SMA and N-cadherin. However, the knockdown of CADM2 in 11Z and EESCs resulted in decreased E-cadherin levels and increased α-SMA and N-cadherin levels. In conclusion, CADM2 inhibited EMT in the endometriosis cells.
CADM2 inhibits EMT in endometriosis cells. a After overexpression of CADM2 in 11Z and EESCs, the expressions of E-cadherin, α-SMA, and N-cadherin were detected by western blotting. b After knockdown of CADM2 in 11Z and EESCs, the expressions of E-cadherin, α-SMA, and N-cadherin were detected by western blotting. All experiments were repeated at least three times
Discussion
Previous research has demonstrated that CADM2 is expressed at low levels in a variety of tumor tissues. It is a tumor suppressor protein and acts as an important negative regulator in tumorigenesis and progression. In prostate cancer, the expression level of CADM2 is significantly reduced, possibly partly attributable to hypermethylation of the DNA promoter region [33]. CADM2 has low expression in esophageal squamous cell carcinoma (ESCC) tissues and cell lines. The overexpression of CADM2 inhibits proliferation and induces apoptosis in ESCC cells [34]. In addition, some studies found that ESCC patients with high CADM2 expression have a higher survival rate than those with low CADM2 expression. Meanwhile, CADM2 expression in ESCC tissues is closely associated with TNM stage and lymph node metastasis [35]. CADM2 is predominantly enriched in the central nervous system. However, studies have found that in glioma tissues, CADM2 expression levels are significantly lower than in normal brain tissues. Tissue microarray results showed that the intensity of CADM2 expression significantly correlates with the pathologic grading of the patients. In higher-grade glioma tissues, the expression level of CADM2 is significantly lower. In addition, glioma patients with high CADM2 expression exhibit longer survival compared to those with low expression [36]. Upregulation of CADM2 in retinoblastoma inhibits tumor cell viability, invasion, and angiogenesis [37]. Studies on cervical cancer have found that CADM2 expression levels in cervical cancer tissues are remarkably lower than that in normal cervical tissues, with consistent findings in cervical cancer cell lines [19]. Overexpression of CADM2 results in cell cycle arrest at the G0/G1 phase and reduced levels of metallo-matrix protease 2 (MMP2), cyclin D1, and CDK4 proteins, and thus inhibits the malignant progression of cervical cancer. However, another study found that CADM2 expression is upregulated in non-small cell lung cancer (NSCLC) patients with brain metastases compared to those without brain metastases. In addition, CADM2 knockdown inhibits the migration, invasion, and EMT process of NSCLC cells. Therefore, in patients with NSCLC with brain metastases, CADM2 may contribute to their poor prognosis [38]. In summary, various studies have found that the biological function of CADM2 is complex, and it may have a bidirectional function as an oncogene or an anti-oncogene. In the present study, we demonstrated that CADM2, which has low expression levels in ectopic endometrial tissues of endometriosis patients, inhibits the growth, migration, and invasion of endometriosis cells and is a negative regulator of endometriosis. This enriches our understanding of the pathogenesis of endometriosis.
CADM2 is probably engaged in biological processes like cell adhesion, cell–cell interactions, and apoptosis. However, the first step in primary tumor metastasis requires disruption of cell adhesion. CADM2 inhibits biological behaviors of glioma cells, such as proliferation and migration, possibly by suppressing the glioma cell cycle and EMT process [36]. In hepatocellular carcinoma, CADM2 affects HCC cells migration and invasion by inhibiting their EMT [39]. Upregulation of CADM2 expression counteracts the promotion of miR-146a on cell proliferation, migration, invasion, and the EMT process in clear renal cell carcinoma (ccRCC) cells [40]. The present study showed consistent findings. Our results showed a positive correlation between CADM2 and the expression of the EMT-associated epithelial marker E-cadherin but a negative correlation with the expression of the mesenchymal cell markers α-SMA and N-cadherin in the ectopic endothelial group. We manipulated the expression of CADM2 in 11Z and EESCs to explore the effect of its overexpression and knockdown on EMT in endometriosis cells. The results showed that the expression level of E-cadherin in endometriosis cells increased with overexpression of CADM2 and decreased with knockdown of CADM2, while the opposite was true for α-SMA and N-cadherin. These experimental results show that CADM2 may inhibit the occurrence and development of EM by suppressing the EMT signaling pathway.
However, our study has some shortcomings. It has been reported that CADM2 promoter hypermethylation is one of the causes of low CADM 2 expression in tumor tissues. In our study, CADM2 had low expression in ectopic endometrial tissues of patients with endometriosis. However, we did not explore the reasons for its low expression. In addition, our study explored the effect of only CADM2 on the EMT signaling pathway in endometriosis. Given the complex pathogenesis of endometriosis, whether it participates in the pathogenesis of endometriosis by influencing other signaling pathways needs to be explored further. Finally, the effects of CADM2 on other biological functions in endometriosis cells need to be added, such as the effects of CADM2 on the apoptotic process of endometriotic cells. In the future, we will research these aspects to find new ideas for better treatment of the disease.
To summarize, our research indicates that CADM2 is expressed at a low level in ectopic endometrial tissues, potentially contributing to the occurrence of endometriosis. Furthermore, we showed that CADM2 has a restraining effect on endometriosis by blocking EMT. CADM2 could be a promising new tool for diagnosing and treating endometriosis.
Data availability
All data analyzed during this study will be made available on reasonable request.
Code availability
Not applicable.
Change history
31 May 2024
A Correction to this paper has been published: https://doi.org/10.1007/s43032-024-01609-5
References
Krina T, Zondervan DPCM, Stacey A, Missmer SD. Endometriosis. New Engl J Med. 2020;382(13):1244–56.
Agostinis C, Balduit A, Mangogna A, et al. Immunological basis of the endometriosis: the complement system as a potential therapeutic target. Front Immunol. 2021;11:599117.
Bjedov S, Lvodylnxã LX, RãnrHãlq DD, et al. Endometriosis, pain and mental health. Psychiatria Danubina. 2021;33(Suppl 4):632–6.
Lagana AS, Garzon S, Gotte M, et al. The Pathogenesis of Endometriosis: Molecular and Cell Biology Insights. Int J Mol Sci. 2019;20(22):5615.
Sampson JA. Metastatic or embolic endometriosis, due to the menstrual dissemination of endometrial tissue into the venous circulation. Am J Pathol. 1927;3(2):93–110.
Dongre A, Weinberg RA. New insights into the mechanisms of epithelial-mesenchymal transition and implications for cancer. Nat Rev Mol Cell Biol. 2019;20(2):69–84.
Das V, Bhattacharya S, Chikkaputtaiah C, et al. The basics of epithelial-mesenchymal transition (EMT): A study from a structure, dynamics, and functional perspective. J Cell Physiol. 2019;234(9):14535–55.
Jolly MK, Ware KE, Gilja S, et al. EMT and MET: necessary or permissive for metastasis?. Mol Oncol. 2017;11(7):755–69.
Matsuzaki S, Darcha C. Epithelial to mesenchymal transition-like and mesenchymal to epithelial transition-like processes might be involved in the pathogenesis of pelvic endometriosis. Hum Reprod. 2012;27(3):712–21.
Xiong W, Zhang L, Liu H, et al. E(2) -mediated EMT by activation of beta-catenin/Snail signalling during the development of ovarian endometriosis. J Cell Mol Med. 2019;23(12):8035–45.
Chen M, Zhou Y, Xu H, et al. Bioinformatic analysis reveals the importance of epithelial-mesenchymal transition in the development of endometriosis. Sci Rep. 2020;10(1):8442.
Lessey BA, Young SL. Integrins and other cell adhesion molecules in endometrium and endometriosis. Semin Reprod Endocrinol. 1997;15(3):291–9.
Elangbam CS, Qualls CJ, Dahlgren RR. Cell adhesion molecules–update. Vet Pathol. 1997;34(1):61–73.
Witz CA. Cell adhesion molecules and endometriosis. Semin Reprod Med. 2003;21(2):173–82.
Fogel AI, Akins MR, Krupp AJ, et al. SynCAMs organize synapses through heterophilic adhesion. J Neurosci. 2007;27(46):12516–30.
Robbins EM, Krupp AJ, Perez DAK, et al. SynCAM 1 adhesion dynamically regulates synapse number and impacts plasticity and learning. Neuron. 2010;68(5):894–906.
Li H, Gao J, Zhang S. Functional and Clinical Characteristics of Cell Adhesion Molecule CADM1 in Cancer. Front Cell Dev Biol. 2021;9:714298.
Wu D, Lei Y, Liu Q, et al. Characterization and clinical significance of the CADM1/HER2/STAT3 axis in serous ovarian tumors. Medicine (Baltimore). 2021;100(8):e23777.
Del Pino M, Sierra A, Marimon L, et al. CADM1, MAL, and miR124 promoter methylation as biomarkers of transforming cervical intrapithelial lesions. Int J Mol Sci. 2019;20(9):2262–2262.
Fortune JE, Wissler RN, Vincent SE. Prolactin modulates steroidogenesis by rat granulosa cells: II. effects on estradiol. Biol Reprod. 1986;35(1):92–9.
Zhang G, Zhong L, Luo H, et al. MicroRNA-155-3p promotes breast cancer progression through down-regulating CADM1. Onco Targets Ther. 2019;12:7993–8002.
Shi XY, Sun YZ, Li M, et al. LncRNA CADM1-AS1 serves as a new prognostic biomarker for gastric cancer. Eur Rev Med Pharmacol Sci. 2019;23(3 Suppl):232–8.
Kim KJ, Kim JY, Hong SM, et al. Loss of CADM4 expression is associated with poor prognosis in small intestinal adenocarcinomas. APMIS. 2017;125(5):437–43.
Saito M, Goto A, Abe N, et al. Decreased expression of CADM1 and CADM4 are associated with advanced stage breast cancer. Oncol Lett. 2018;15(2):2401–6.
Bang S, Jee S, Son H, et al. Decreased expression of cell adhesion molecule 4 in gastric adenocarcinoma and its prognostic implications. Diagnostics. 2022;12(4):941.
Biederer T. Bioinformatic characterization of the SynCAM family of immunoglobulin-like domain-containing adhesion molecules. Genomics. 2006;87(1):139–50.
Budhu A, Forgues M, Ye QH, et al. Prediction of venous metastases, recurrence, and prognosis in hepatocellular carcinoma based on a unique immune response signature of the liver microenvironment. Cancer Cell. 2006;10(2):99–111.
Yang S, Yan HL, Tao QF, et al. Low CADM2 expression predicts high recurrence risk of hepatocellular carcinoma patients after hepatectomy. J Cancer Res Clin Oncol. 2014;140(1):109–16.
Li D, Zhang Y, Zhang H, et al. CADM2, as a new target of miR-10b, promotes tumor metastasis through FAK/AKT pathway in hepatocellular carcinoma. J Exp Clin Cancer Res. 2018;37(1):46.
Lu C, Qiao P, Fu R, et al. Phosphorylation of PFKFB4 by PIM2 promotes anaerobic glycolysis and cell proliferation in endometriosis. Cell Death Dis. 2022;13(9):790.
Lu C, Ren C, Yang T, Sun Y, Qiao P, Wang D, Lv S, Yu Z. A noncanonical role of fructose-1, 6-bisphosphatase 1 Is essential for inhibition of notch1 in breast cancer. Mol Cancer Res. 2020;18(5):787–96.
Gaetje R, Kotzian S, Herrmann G, et al. Nonmalignant epithelial cells, potentially invasive in human endometriosis, lack the tumor suppressor molecule E-cadherin. Am J Pathol. 1997;150(2):461–7.
Chang G, Xu S, Dhir R, et al. Hypoexpression and epigenetic regulation of candidate tumor suppressor gene CADM-2 in human prostate cancer. Clin Cancer Res. 2010;16(22):5390–401.
Li X, Chen D, Li M, et al. The CADM2/Akt pathway is involved in the inhibitory effect of miR-21-5p downregulation on proliferation and apoptosis in esophageal squamous cell carcinoma cells. Chem Biol Interact. 2018;288:76–82.
Zhu ZQ, Hu HF, Zheng XY, et al. Effects of microRNA-182-5p on cell proliferation and invasion of esophageal squamous cell carcinoma and related molecular mechanisms. Zhonghua Zhong Liu Za Zhi. 2020;42(8):635–43.
Liu N, Yang C, Bai W, et al. CADM2 inhibits human glioma proliferation, migration and invasion. Oncol Rep. 2019;41(4):2273–80.
Huang YX, Nie XG, Li GD, et al. Downregulation of microRNA-182 inhibits cell viability, invasion and angiogenesis in retinoblastoma through inhibition of the PI3K/AKT pathway and CADM2 upregulation. Int J Oncol. 2018;53(6):2615–26.
Dai L, Zhao J, Yin J, et al. Cell adhesion molecule 2 (CADM2) promotes brain metastasis by inducing epithelial-mesenchymal transition (EMT) in human non-small cell lung cancer. Ann Transl Med. 2020;8(7):465.
Li D, Zhang Y, Zhang H, Zhan C, Li X, Ba T, Qiu Z, Fang E, Guixiang LV, Zou C, Wang C, Si L, Zou C, Li Q, Gao X. CADM2, as a new target of miR-10b, promotes tumor metastasis through FAK/AKT pathway in hepatocellular carcinoma. J Exp Clin Cancer Res. 2018;37(1):46.
Yang L, Zhao G, Wang F, Li C, Wang X. Hypoxia-regulated miR-146a targets cell adhesion molecule 2 to promote proliferation, migration, and invasion of clear cell renal cell carcinoma. Cell Physiol Biochem. 2018;49(3):920–31.
Acknowledgements
We thank International Science Editing ( http://www.internationalscienceediting.com ) for editing this manuscript.
Funding
This work was supported by the Shandong Traditional Chinese Medicine Technology Project (Q-2022128) and the Weifang Health Commission Scientific Research Project (WFWSJK-2022–006).
Author information
Authors and Affiliations
Contributions
We express our gratitude to all authors for their valuable contributions. AJ, TY, ZW, QZ, and CZ were responsible for the design of the experiments. ZW, QZ, CZ, and JY were responsible for conducting the experiments. TY and AJ offered both experimental and analytical assistance. Reagents, materials, and analysis tools were contributed by TY. The responsibility of interpreting the data and writing the manuscript lies with ZW, QZ, and CZ. AJ conducted a thorough evaluation of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The ethics committee of the Affiliated Hospital of Shandong Second Medical University granted approval for all experiments involving human tissue samples (Approval number: Wyfy-2023-ky-280).
Consent to participate
Informed consent was obtained from each patient.
Consent for publication
All authors have agreed to publish the article.
Conflict of interest
There is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Z., Zhang, Q., Zhang, C. et al. CADM2 participates in endometriosis development by influencing the epithelial-mesenchymal transition. Reprod. Sci. (2024). https://doi.org/10.1007/s43032-024-01592-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43032-024-01592-x