Abstract
Preterm birth remains the leading cause of neonatal morbidity and mortality, with complex biochemical pathways requiring continued understanding and assessment. The objective of this study is to assess the associations between maternal cortisol and placental corticotropin–releasing hormone (placental CRH) concentrations with birth outcomes when stratified by placental histopathology. We conducted an analysis of 112 singleton pregnancies who received betamethasone between 23 and 34 weeks’ gestation. Maternal blood and saliva were collected prior to betamethasone administration and samples assayed for plasma cortisol (pCort), salivary cortisol (sCort), and placental CRH levels. Placental findings were characterized as inflammatory, maternal vascular underperfusion (MVU), or no pathology, and compared for the outcomes of placental CRH, pCort, and sCort levels, gestational age at birth (GAB), and birthweight percentiles (BWP). Thirty-six subjects were characterized as inflammatory, 38 as MVU, and 38 without placental abnormalities. Histopathology groups differed significantly on placental CRH levels, GAB, and BWP. Post hoc tests suggested that the MVU group had higher placental CRH than the inflammatory or no pathology groups, and despite delivering earlier than the other two groups, the inflammatory group had infants with significantly higher BWP. No differences existed between groups in terms of mean plasma or sCort levels. Higher placental CRH and pCort levels were associated with earlier GAB in the overall sample, but when split by group, these associations remained significant only among the MVU group. Higher placental CRH was also associated with lower BWP in the overall sample but did not remain significant when split by group. Higher sCort was associated with lower BWP only in the MVU group. There is differentiation of placental CRH, cortisol, and birth outcomes when evaluated by placental histopathology. This highlights the importance of evaluating birth outcomes within the context of placental histopathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preterm birth (PTB) is a multifactorial syndrome, with numerous, and often overlapping etiologies complicating approximately one in every ten U.S. pregnancies, and is the leading cause of neonatal morbidity and mortality in this country [1,2,3,4,5]. Preterm infants are at increased risk for both short- and long-term adverse health outcomes, including neurodevelopmental, cardiovascular, respiratory, and endocrine disorders [6, 7]. Given these morbidities, there is compelling need to better understand the mechanism(s) leading to PTB, and develop new methods to identify pregnancies at greatest risk [8].
Historically, PTB was classified as either spontaneous or indicated; however, this methodology is flawed in several ways [3,4,5, 9]. For instance, retrospectively distinguishing spontaneous preterm labor (PTL) from preterm premature rupture of membranes (PPROM) can often be difficult. Similarly, indicated PTB can encompass a broad array of indications, including third-trimester bleeding, hypertension, or intrauterine growth restriction (IUGR), which researchers may not be able to glean from historical review of the medical record.
A complete understanding of PTB requires assessment of maternal, fetal, and placental conditions that contribute to PTB [4, 5, 9]. This has led researchers to evaluate birth outcomes based on placental histopathology, and has resulted in the concept of two distinct schema of placental histopathology relating to PTB — maternal vascular underperfusion (MVU) and infection/inflammation [10,11,12]. These schema are important in the understanding of PTB because of its many complex etiologies [10].
Additionally, much research has focused on identifying maternal biomarkers to screen for obstetric complications. Although the ideal biomarker predictive of PTB remains elusive, several have shown promise. Placental corticotropin–releasing hormone (placental CRH), identical in structure and function to the neuropeptide of hypothalamic origin, is one of the primary neuroendocrine mediators of spontaneous labor and fetal development [8, 13]. As pregnancy progresses, placental CRH is expressed in increasing amounts into the maternal and fetal circulations. Studies have not only demonstrated a link between elevated placental CRH and PTB, [14] but also between elevated placental CRH and pregnancies complicated by hypertension, PPROM, and IUGR, suggesting differential expression of placental CRH depending on varying forms of stress to the maternal-fetal unit [8, 15,16,17,18,19,20].
Cortisol, the hormonal end-point of stress-related physiologic activation of the hypothalamic-pituitary-adrenal axis, has also been the focus of several studies regarding its association with reduced fetal weight. Although the association between cortisol and IUGR has, at times been contradictory [21,22,23,24,25], a recent, large meta-analysis demonstrated an association between elevated maternal salivary cortisol levels, and reduced fetal birthweight [26]. The authors concluded that much of the variation reported in the literature may be due to methodologic differences in the timing, and the type of cortisol—protein bound or unbound—being measured.
The evaluation of outcomes within the context of placental pathology, and separately, the identification of biomarkers such as placental CRH and cortisol, has provided valuable insight into predicting birth outcomes. Recent research of birth outcomes within the context of abnormal placental pathology and elevated placental CRH levels demonstrated significant correlation between adverse outcomes, elevated placental CRH, and placental abnormalities [27]. It is possible that further evaluation of placental CRH and cortisol within placental histopathology schema may disclose new insights into our understanding of the causes of PTB and/or fetal growth abnormalities. The purpose of the current study was to assess the association(s) between maternal cortisol and placental CRH levels with birth outcomes, when stratified by placental histopathology characteristic of either inflammation or maternal vascular underperfusion.
Study Design
Subject Selection
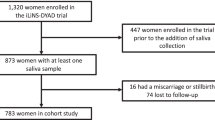
This was a prospective study performed at an academic medical center between 2011 and 2014 evaluating the ability of placental CRH to predict PTB [14]. Study protocols were reviewed and received approval from the Institutional Review Board. Written and informed consent was obtained from each woman prior to study enrollment. In conformity with standardized hospital protocol, an attending obstetrician evaluated each subject, and determined whether temporizing measures and/or betamethasone (BMZ) were indicated. If deemed necessary, BMZ was administered in two doses (12 mg intramuscular, 24 h apart). Subjects with a history of illicit drug use or corticosteroid use were excluded from participation. A total of 153 women receiving BMZ gave consent for study involvement. Fourteen subjects were excluded for twin gestations and another 19 for other various reasons, including patient refusal of blood collection, positive toxicology screens, or receipt of blood transfusions during the time of blood sampling. Of the remaining 120 subjects, birth outcomes and placental histological data was available for 112. All 112 singleton pregnancies received BMZ between 23.9 and 32.7 weeks’ gestation (mean 28.7 weeks) for various indications, including PTL, short cervix, PPROM, placental abruption, preeclampsia with or without severe features, gestational hypertension, worsening chronic hypertension, or IUGR with or without abnormal uterine artery Doppler velocimetry.
Hormone Collection
Maternal blood samples were collected via venipuncture into K2EDTA BD Vacutainers, and maternal saliva samples were collected into Salivette® Cortisol (Sarstedt) tubes, both prior to treatment with corticosteroids. Because it remains unclear whether the free or the protein-bound form of cortisol is associated with fetal growth impairment, and to comprehensively assess all possible associations, both salivary and plasma cortisol were analyzed [22,23,24,25,26, 28]. Free/unbound cortisol is best assessed in saliva, while total/protein-bound cortisol is best assessed in plasma. Conversely, placental CRH is known to be highly protein bound within plasma until the end of the third trimester [29]. Immediately after blood collection, 50 μL of protease inhibitor, aprotinin (Thermo Fisher Scientific) was added, and samples were kept frozen at − 70C until processed. Blood and saliva samples were spun at 2500 rpm in a refrigerated centrifuge for 15 min. Plasma was then aliquoted into separate cryovials for measurement of placental CRH and plasma cortisol. All samples were assayed in duplicate. Plasma placental CRH assays were completed by Dr. Roger Smith’s lab at the University of Newcastle, Australia. Placental CRH concentrations (pg/ml) were batch-analyzed by radioimmunoassay (RIA). Extraction recovery was 82.5%. No correction of the data for extraction recoveries was made. Inter- and intraassay coefficients of variance (CVs) were 10.2% and 8.2%, respectively. A computer-assisted four-parameter logistics program was utilized for RIA assay data reduction [30]. Plasma and salivary cortisol assays were completed by Dr. Nicolas Rohleder’s lab at Brandeis University, Waltham, Massachusetts. Plasma cortisol was measured using enzyme-linked immunosorbent assays (ELISAs, IBL-International, Toronto, ON, Canada, www.ibl-international.com). Inter- and intraassay CVs for plasma cortisol were 8.03% and 5.70%, respectively. Salivary cortisol was measured using a chemiluminescence immunoassay (CLIA, IBL-International, Toronto, ON, Canada), and luminescence was read on a Berthold MLP1 luminescence plate reader. Inter- and intraassay CVs for salivary cortisol were 10.23% and 5.3%, respectively.
Placental Examination and Group Designation
Following delivery, all 112 placentae were reviewed by two pathologists, including one with expertise in placental pathology, and any discrepancies were resolved by dual review at a multiheaded microscope. Neither pathologist had knowledge of outcomes, lab results, or any other clinical information, other than gestational age at delivery. Subjects with histopathologic findings of chorionitis, chorioamnionitis, chorioamnionitis involving the basal plate, microabscesses, funisitis, and/or vasculitis were categorized as “inflammatory”. Subjects with accelerated villous maturation, perivillous fibrin deposition, placental infarction, chorangiosis, nucleated red blood cells, and/or increased syncytial knots were characterized as “MVU”. All placental abnormalities were defined according to standardized guidelines [31]. Subjects with histopathology characteristic of both groups were assigned to a scoring system in which each of their placental findings was assigned a score of one point. An additional 1, 2, or 3 points were assigned to placentae with infarcts involving < 5%, 5–10%, or > 10% of the placenta, respectively. Subjects were then reassigned into either the inflammatory or MVU group based on the higher cumulative score of their placental findings. In cases where the cumulative histopathology score between groups was equal, subjects were assigned to either the inflammatory or MVU group based on additional review of placental histopathology and relative severity of their placental findings. Placentae without abnormal findings were classified as “no pathology (NP)”. It is important to note that the NP group does not represent a true control group as these pregnancies were also afflicted with preterm complications serious enough to merit treatment with BMZ.
Statistical Analysis
Statistical analysis was performed using SPSS Statistics™, Version 24.0.0.1 (Armonk, N.Y., USA). ANOVA and χ2 tests were used to assess demographic group differences and identify potential covariates. Placental CRH levels were log-transformed to reduce skew prior to analysis. ANCOVA was utilized to assess differences in hormone levels, GAB, and BWP among histopathology groups. Post hoc comparisons were then performed using Bonferroni correction to identify individual group differences. Chi-squared tests were used to test for differences in the proportion of infants born preterm (< 37 weeks’ gestation) and small for gestational age (SGA, < 10th percentile) by histopathology group. Partial correlations were used to evaluate the association(s) between hormone levels and birth outcomes in the overall sample and within each histopathology group. Birthweight percentile was assessed by GAB and infant sex based on US natality data [32].
Results
Placental Histopathology
Initial review of placental histology identified 38 subjects without placental histopathology, 26 subjects with inflammatory placental histopathology, and 32 with histopathology characterized solely by maternal vascular underperfusion. Sixteen subjects exhibited pathology characteristic of both inflammation and vascular underperfusion, of which 14 were reassigned based on the cumulative score of their histopathology, and two based on additional review of placental histopathology. This totaled 36 subjects categorized into the inflammatory group, 38 into the MVU group, and 38 into the NP group. Indications for BMZ administration by group are displayed in Table 1.
Covariate Selection
Group demographics are presented in Table 2. Gestational age at sample collection was used as a covariate in all hormone analyses. Additional variables were included as covariates if they were associated (p < 0.10) both with histopathology group and birth outcome. Potential covariates included maternal age, race/ethnicity, gravidity, parity, BMI, household income, and fetal sex. Only maternal BMI was associated both with histopathology group and BWP and was therefore included as a covariate in all BWP analyses. None of the potential covariates were associated both with histopathology group and GAB.
Differences Between Histopathology Groups
Group differences in hormone levels and birth outcome are presented in Table 3. Of the three hormones assessed, only placental CRH differed significantly by histopathology group {F(2,108) = 3.52, p = 0.03}. Post hoc results suggest that the MVU group had higher placental CRH levels than both the inflammatory (p = 0.06) and NP (p = 0.09) groups (see Fig. 1 for placental CRH profiles by group). GAB and BWP also differed significantly by histopathology group {F(2,109) = 3.53, p = 0.03 and F(2,104) = 7.07, p = 0.001, respectively}. Despite delivering an average of 2.5 weeks earlier than the MVU and NP groups (ps < 0.10), the inflammatory group had infants with significantly higher BWP (ps < 0.05), even after covarying for maternal BMI. When stratifying deliveries by term and SGA status, a non-significant difference was observed in the proportion of subjects delivering preterm (69.4% in the inflammatory group, 44.7% in the MVU group, and 60.5% in the NP group; χ2{2, N = 112) = 4.78, p = 0.09}.
Placental CRH profiles by histopathology group with mean and standard error bars. a Raw, unadjusted placental CRH values and b placental CRH values adjusted for GA at collection (standardized residuals from a linear regression with GA at collection predicting placental CRH values). Note: Raw placental CRH values were log transformed to reduce skew prior to analysis, and all placental CRH analyses included GA at collection as a covariate
Associations Between Hormones and Birth Outcomes
Associations between biomarkers and birth outcomes are displayed in Table 4. Higher placental CRH and pCort levels were associated with earlier GAB in the overall sample (r = − 0.34, p < 0.01) but, when split by group, these associations remained significant only among the MVU group (r = − 0.56, p = < 0.01; see Fig. 2). Higher placental CRH was also associated with lower BWP in the overall sample (r = − 0.19, p < 0.05), but did not remain significant when split by group (ps > 0.10). Higher sCort was associated with lower BWP only in the MVU group (r = − 0.35, p < 0.05).
Placental CRH level and GAB for inflammatory (blue), MVU (orange), and no pathology (green) groups. Note: For graphing purposes, placental CRH values have been log transformed and adjusted for GA at collection (standardized residuals from a linear regression with GA at collection predicting placental CRH values). All placental CRH analyses were conducted using log transformed placental CRH data and covarying for GA at collection
Discussion
In this analysis of 112 subjects who received BMZ for various indications portending potential PTB, we examined the relation between birth outcomes and maternal hormone profiles within the context of three distinct placental histopathology schema—maternal vascular underperfusion, inflammation, and those without abnormal placental histopathology. Our findings suggest clear distinctions between histopathology groups regarding both hormone profiles and birth outcome. Subjects with histopathology characteristic of vascular underperfusion demonstrated higher levels of placental CRH than either of the other groups, while no differences were found in salivary or plasma cortisol levels. Subjects in the inflammatory group delivered earlier than either the MVU or NP groups; however, they delivered infants with significantly higher BWP. When evaluating the relationship between hormones and birth outcomes, higher levels of placental CRH were found to be correlated with earlier GAB in the overall sample, but when split by group, this association remained significant only among the MVU group. Placental CRH was also found to be negatively correlated with BWP in the overall sample, but this association became nonsignificant when stratified by histopathology group. Conversely, salivary cortisol was not correlated with BWP in the overall sample, but a significant negative correlation was identified within the MVU group. Our findings suggest a differential expression of maternal biomarkers depending on the type of physiological stress to the maternal-fetal unit, and highlight the importance of evaluating the association between biomarkers and adverse birth outcomes within the context of placental histopathology.
Differences Between Histopathology Groups
In 2017, Catov et al. reviewed 20,091 births (15,710 term, 4381 preterm) and their placentae, and classified them according to the presence/absence of placental malperfusion or intrauterine inflammation/infection. Similar to our findings, they found that among preterm births, placental malperfusion was associated with impaired fetal growth, while lesions of inflammation/infection were associated with earlier delivery, but not smaller infants. They concluded that the addition of placental histopathology to the evaluation of PTB may aid in the search for biomarkers contributing to these phenomena [3]. Our findings support this conclusion. Furthermore, the fact that a study with only 112 subjects exhibited findings similar to one involving more than 20,000, highlights the importance of including placental histopathology in the evaluation of PTB. It should be noted that the mean GAB of the group without placental pathology was nearly identical to that of the MVU group. This, in addition to the finding that the group without placental pathology exhibited a significantly lesser BWP than the inflammatory group, serves as a reminder that this group does not serve as a normal control group. Rather, they represent a group whose preterm complications’ etiology is not discernable via pathological evaluation of the placenta.
In the current study, we found evidence that subjects in the MVU group exhibited higher placental CRH levels as compared with the rest of the cohort. In 2002, McGrath et al. found that subjects who underwent indicated PTB demonstrated significantly increased placental CRH levels compared with those who experienced spontaneous PTB. The authors concluded that excessive fetomaternal stress may be responsible for the increased sensitivity to placental CRH among subjects requiring indicated PTB [18]. More recently, Perng et al. (2018) demonstrated significant correlation between obstructive placental vascular pathology and small for gestational age fetuses [27]. Although intergroup differences in placental CRH concentration reached only trend-level significance—likely as a result of a modest sample size—our findings suggest a unique biochemical milieu between subjects whose placentae demonstrate histopathologic evidence characteristic of either vascular underperfusion or infection/inflammation.
Associations Between Hormones and Birth Outcomes
Although it remains to be proven whether placental CRH is involved in the etiology of PTB, or is simply a biochemical result of it, many researchers agree that placental CRH is involved in the regulation of gestational length [8, 13, 19, 33, 34]. Complications of pregnancy linked to elevated placental CRH levels, and thus an increased risk for PTB, include hypertensive disorders, IUGR, PTL, and PPROM [16,17,18,19,20]. Our finding of an association between placental CRH and shorter gestation supports the model of placental CRH as a regulator of gestational length. This finding is supported by prior research; in the aforementioned study by Perng et al., elevated CRH levels were associated with PTB and SGA fetuses among placentae with obstructive vascular pathologies [27]. The apparent differential expression of placental CRH varying with placental pathology suggests that the expression of placental CRH, and its associated downstream effects, is influenced by the type of underlying stress—in this case, inflammatory or vascular underperfusion—applied to the maternal-fetal unit.
Previous research has demonstrated associations between altered cortisol levels and the outcomes of PTB and decreased birthweight [21,22,23,24,25, 28, 35]. The current study showed a trend toward significantly lower pCort levels within the MVU group as compared with those with inflammatory placental pathology or no pathology. It has been well described that MVU pathology is associated with chronic maternal-fetal stress, which clinically, manifests as preeclampsia, fetal growth restriction, and preterm birth [11, 12, 27, 36]. In their case-control study of 142 maternal-fetal dyads, Su et al. (2015) demonstrated that infants of mothers with higher amounts of stress during pregnancy exhibited significantly lower plasma cortisol levels, birthweight, and head circumferences. They reasoned that lower levels of cortisol were the result of chronic stimulation of the HPA axis, adrenal hyporesponsivity, and downregulation of adrenal cortisol receptors [22]. Although there existed only a trend-level significant difference in sCort levels between histopathology groups, sCort correlated significantly with decreased BWP among neonates within the MVU group. This is consistent with results from a large metaanalysis performed by Cherak et al. (2018), which demonstrated that for every unit increase in sCort, fetal birthweight decreased by 2.3 g [26]. The fact that this correlation existed within the MVU group and not the inflammatory group supports the concept of MVU histopathology as a result of chronic fetomaternal stress, and underscores the importance of placental pathology in the search for causes of preterm birth and fetal growth restriction.
Strengths and Weaknesses
Any patient experiencing preterm complications warranting treatment with BMZ is likely to have some degree of underlying abnormal placental pathology. Furthermore, the effect of BMZ on placental pathology in and of itself is unknown. As evident from our GAB and BWP findings, the group without placental pathology does not represent a control group. A true control group would consist of normal pregnancies without significant preterm complications and without placental pathology. We acknowledge the lack of a true control group in this study as a limitation. Conversely, having each placenta reviewed by two pathologists, including one with subspecialty training in placental pathology increases confidence in the validity of our findings, which we believe to be a major strength of this study. Lastly, although it is unclear if placental histopathology illustrates the cause or the effect in the evolution of PTB and IUGR, our findings indicate that when evaluating the association between biomarkers and birth outcomes, additional insights become apparent within the context of placental histopathology.
Conclusion
Preterm birth remains a common perinatal outcome characterized by complex molecular pathways that continue to elude prevention and treatment. By analyzing the associations between birth outcomes and maternal biomarkers in terms of placental histopathology, our findings suggest that the evaluation of different biomarkers may be unique to the underlying cause of PTB. Future research should continue to explore the subjectivity of placental CRH and cortisol expression, both temporally throughout gestation and in relation to varying clinical conditions and histopathologic findings, as a means of seeking additional biochemical markers of PTB, in order to reduce its incidence.
References
Goldenberg R, Jobe A. Prospects for research in reproductive health and birth outcomes. JAMA. 2001;285(5):633–9.
Hamilton B, et al. Births: preliminary data for 2014. Natl Vital Stat Rep. 2015;64(6).
Catov JM, et al. Neonatal outcomes following preterm birth classified according to placental features. Am J Obstet Gynecol. 2017;216(4):411 e1–411 e14.
Goldenberg RL, Gravett MG, Iams J, Papageorghiou AT, Waller SA, Kramer M, et al. The preterm birth syndrome: issues to consider in creating a classification system. Am J Obstet Gynecol. 2012;206(2):113–8.
Kramer MS, Papageorghiou A, Culhane J, Bhutta Z, Goldenberg RL, Gravett M, et al. Challenges in defining and classifying the preterm birth syndrome. Am J Obstet Gynecol. 2012;206(2):108–12.
Chaiworapongsa T, et al. Pravastatin for the prevention of adverse pregnancy outcome: preeclampsia and more? J Matern Fetal Neonatal Med. 2016;1.
Saigal S, Doyle L. An overview of mortality and sequelae of preterm birth from infancy to adulthoood. Lancet. 2008;371:261–9.
Wadhwa PD, Garite TJ, Porto M, Glynn L, Chicz-DeMet A, Dunkel-Schetter C, et al. Placental corticotropin-releasing hormone (CRH), spontaneous preterm birth, and fetal growth restriction: a prospective investigation. Am J Obstet Gynecol. 2004;191(4):1063–9.
Villar J, et al. The preterm birth syndrome: a prototype phenotypic classification. Am J Obstet Gynecol. 2012;206(2):119–23.
Korzeniewski SJ, et al. Maternal plasma angiogenic index-1 (placental growth factor/soluble vascular endothelial growth factor receptor-1) is a biomarker for the burden of placental lesions consistent with uteroplacental underperfusion: a longitudinal case-cohort study. Am J Obstet Gynecol. 2016;214(5):629 e1–629 e17.
Odibo AO, Patel KR, Spitalnik A, Odibo L, Huettner P. Placental pathology, first-trimester biomarkers and adverse pregnancy outcomes. J Perinatol. 2014;34(3):186–91.
Triunfo S, et al. Angiogenic factors at diagnosis of late-onset small-for-gestational age and histological placental underperfusion. Placenta. 2014;35(6):398–403.
Behrman R,Butler A. Preterm birth: causes, consequences, and prevention. Institute of Medicine, National Academy of Sciences; 2007.
Swales DA, et al. Can placental Corticotropin-releasing hormone inform timing of antenatal corticosteroid administration? J Clin Endocrinol Metab. 2018.
Giles W, et al. Abnormal umbilical artery Doppler waveforms and cord blood corticotropin-releasing hormone. Obstet Gynecol. 1996;87(1):107–11.
Hobel C, Arora C, Korst L. Corticotrophin-releasing hormone and CRH-binding protein. Differences between patients at risk for preterm birth and hypertension. Ann N Y Acad Sci. 1999;897:54–65.
Warren W, Gurewitseh E, Goland R. Corticotropin-releasing hormone and pituitary-adrenal hormones in pregnancies complicated by chronic hypertension. Am J Obstet Gynecol. 1994;172(2):661–6.
McGrath S, McLean M, Smith D, Bisits A, Giles W, Smith R. Maternal plasma corticotropin-releasing hormone trajectories vary depending on the cause of preterm delivery. Am J Obstet Gynecol. 2002;186(2):257–60.
McLean M, Smith R. Corticotrophin-releasing hormone and human parturition. Reproduction. 2001;121:493–501.
Torricelli M, Novembri R, Bloise E, de Bonis M, Challis JR, Petraglia F. Changes in placental CRH, urocortins, and CRH-receptor mRNA expression associated with preterm delivery and chorioamnionitis. J Clin Endocrinol Metab. 2011;96(2):534–40.
Ecnomides D, et al. Plasma cortisol and adrenocorticotropin in appropriate and small for gestational age fetuses. Fetal Ther. 1988;3(3):158–64.
Su Q, Zhang H, Zhang Y, Zhang H, Ding D, Zeng J, et al. Maternal stress in gestation: birth outcomes and stress-related hormone response of the neonates. Pediatr Neonatol. 2015;56(6):376–81.
Economides D, Nicolaides K, Campbell S. Metabolic and endocrine findings in appropriate and small for gestational age fetuses. J Perinat Med. 1991;19(1–2):97–105.
Bolten MI, et al. Cortisol levels in pregnancy as a psychobiological predictor for birth weight. Arch Womens Ment Health. 2011;14(1):33–41.
Sandman CA, Glynn L, Schetter CD, Wadhwa P, Garite T, Chicz-DeMet A, et al. Elevated maternal cortisol early in pregnancy predicts third trimester levels of placental corticotropin releasing hormone (CRH): priming the placental clock. Peptides. 2006;27(6):1457–63.
Cherak SJ, Giesbrecht GF, Metcalfe A, Ronksley PE, Malebranche ME. The effect of gestational period on the association between maternal prenatal salivary cortisol and birth weight: a systematic review and meta-analysis. Psychoneuroendocrinology. 2018;94:49–62.
Perng W, et al. Placental pathology, corticotropin-releasing hormone, timing of parturition, and fetal growth in the Pregnancy Outcomes and Community Health Study. J Matern Fetal Neonatal Med. 2018;1–231.
Hoffman MC, Mazzoni SE, Wagner BD, Laudenslager ML, Ross RG. Measures of maternal stress and mood in relation to preterm birth. Obstet Gynecol. 2016;127(3):545–52.
Wadhwa P, Porto M, Garite TJ, Chicz-DeMet A, Sandman CA. Maternal corticotropin-releasing hormone levels in the early third trimester predict length of gestation in human pregnancy. Am J Obstet Gynecol. 1998;179(4):1079–85.
Smith R, Mesiano S, McGrath S. Hormone trajectories leading to human birth. Regul Pept. 2002;108:159–64.
Khong T, Mooney EE, Ariel I, Balmus NC, Boyd TK, Brundler MA, et al. Sampling and definitions of placental lesions. Arch Pathol Lab Med. 2016;140:698–713.
Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3(6).
Korebrits C, Ramirez MM, Watson L, Brinkman E, Bocking AD, Challis JR. Maternal Corticotropin-releasing hormone is increased with impending preterm birth. J Clin Endocrinol Metab. 1998;83(5):1585–91.
Smith R, Nicholson R. Corticotrophin releasing hormone and the timing of birth. Front Biosci. 2007;12:912–8.
Garcia-Blanco A, et al. Can stress biomarkers predict preterm birth in women with threatened preterm labor? Psychoneuroendocrinology. 2017;83:19–24.
Parra-Saavedra M, Crovetto F, Triunfo S, Savchev S, Peguero A, Nadal A, et al. Placental findings in late-onset SGA births without Doppler signs of placental insufficiency. Placenta. 2013;34(12):1136–41.
Acknowledgments
The assistance of the research team who assisted with data collection is gratefully appreciated, as are the families who participated in this project.
Funding
This research was supported by the National Institutes of Health [RO1 HD065823].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Johnston, R.C., Faulkner, M., Carpenter, P.M. et al. Associations Between Placental Corticotropin–Releasing Hormone, Maternal Cortisol, and Birth Outcomes, Based on Placental Histopathology. Reprod. Sci. 27, 1803–1811 (2020). https://doi.org/10.1007/s43032-020-00182-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-020-00182-x