Abstract
Purpose
Assess the effectiveness of three cooling strategies during a 10-min break vs. no break or no cooling on internal body temperature responses during an intermittent treadmill exercise simulating the intensity of a tennis match.
Methods
Twelve physically active females (mean ± SD; age, 26 ± 3 years; height, 167.0 ± 4.8 cm; body mass, 58.2 ± 4.2 kg; VO2peak 46.2 ± 2.5 mL/kg/min) completed five 90-min intermittent exercise trials in the heat (WBGT 30.9 ± 0.2 °C) with a 10-min break in different cooling groups: cold water immersion (CWI), ice towel with dampened towels (Towel), cooling vest (Vest), passive rest (Passive), and no break (None). Rectal temperature (Trec), skin temperature (Tsk), and heart rate (HR) were monitored throughout the trials.
Results
There was a significant difference in ΔTrec between None and CWI (P < 0.001, d = 1.71). The effect size for ΔTrec indicated a moderate impact with a 10-min break using Towel, Vest and Passive, without a significant difference from None (P > 0.05, d = 0.52–0.67). CWI had a significantly greater ΔTrec during the first 15-min of subsequent exercise period compared to Vest and Passive while there was no significant difference during a 10-min break between the cooling groups. The effects of cooling on Tsk and HR were not maintained at the end of exercise period.
Conclusion
A 10-min break with CWI effectively attenuated the rise in internal body temperature following intermittent treadmill exercise. A 10-min CWI break may be a potential strategy to mitigate the risk of exertional heat illnesses during tennis tournaments in hot conditions, however the impact on physical performance and the logistical challenges associated with implementation remain unexplored.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last decade, one in three outdoor tennis tournaments has been held in hot environments (25–35℃ wet-bulb globe temperature (WBGT)) [16]. Despite some well-trained athletes being able to compete in extreme heat conditions at high levels of hyperthermia (> 40 °C) without incident of exertional heat illness (EHI) [2, 21], intense exercise couple with environmental heat increases one’s EHI risk profile. For example, during the Australian Open between 2014 and 2016, the incidence rate of EHI ranged from 27.8 to 44.4 cases per 1000 matches [26, 27]; the highest incidence rates recorded within the sport. However, it must be acknowledged that the true incidence of EHI, including potentially fatal exertional heat stroke (EHS), is largely unknown as a large proportion of competitors are participating during unsanctioned tournaments who presumably have no structure in place to accurately track injuries and illnesses occurring at these events.
The feasibility, adoption and effectiveness of within match cooling interventions that could potentially curb the number of tennis match EHIs is still emerging. Due to the nature of most tennis tournaments, matches occur throughout the day with the possibility of athletes competing in multiple matches per day. Given the logistical and scheduling challenges associated with hosting a large tournament, there is often low regard to the potential health and safety concerns for events occurring in hot and humid environments. While the Women’s Tennis Association (WTA) has implemented an extreme weather policy that includes a 10-min break between the second and third sets when wet bulb globe temperature (WBGT) exceeds 30.1 °C [30], there are no such policies in place within other organizations such as the Association of Tennis Professionals (ATP). Emerging evidence suggests that the implementation of the 10-min cooling break during WTA sanctioned tournaments may serve as an effective measure to reduce EHI risk. Tippet et al. found that during a tennis match, the 10-min break allowed for a 0.25 °C reduction in internal body temperature [28], however, the lack of control over the methods of cooling used across players limit the understanding of the most effective methods by which an athlete can cool themselves during this strict time limit. Previous literature has examined the use of various in-play cooling interventions during a tennis match (e.g., ice towels, cooling vests, fans, and water mist) [9, 11, 17, 23, 25], however, the effectiveness of a 10-min cooling break using a systematic and controlled approach remains largely unknown. Therefore, the purpose of this study was to determine the effectiveness of five strategies (four of which incorporated cooling) during a 10-min cooling break on internal body temperature responses during an intermittent treadmill exercise simulating the intensity of a tennis match. Given the variability across tennis governing bodies for the allowance of a cooling break, if this break demonstrates effective mitigation of thermal strain, this would call for strong consideration by other tennis organizations to allow such a break during warm weather matches.
Methods
Design
Our study utilized a counter-balanced, crossover design in which the participants were randomly assigned to each cooling intervention trial. The participants completed one baseline visit and five laboratory-based experimental trials: (1) no break (None), (2) passive rest (Passive), (3) cooling vest (Vest), (4) ice water-soaked towels (Towels), and (5) cold water immersion (CWI). The baseline visit was conducted at least 24 h before the first experimental trial. The five experimental trials were scheduled at the end of their baseline visit to ensure that all five trials occurred at approximately the same time of day within a ± 2-h time frame. Each experimental trial was scheduled at least three days apart to allow for recovery and all five visits completed within 3–5 weeks. All trials were conducted in an environmentally controlled chamber with WBGT at 30.1 °C [ambient temperature, 40 °C; relative humidity (RH), 31%]. These environmental conditions were chosen based on the current threshold for extreme weather policy activation during the WTA tournaments. The study was approved by the University of Connecticut's Institutional Review Board. Data are available from the authors upon reasonable request.
Participants
Twelve physically active females (mean ± SD; age, 26 ± 3 years; height, 167.0 ± 4.8 cm; body mass, 58.2 ± 4.2 kg; peak oxygen consumption (VO2peak) 46.2 ± 2.5 mL/kg/min) were recruited for this study. All participants self-reported participating in moderate to vigorous physical activity three to five days per week during the screening process and had to have a VO2peak > 40 mL/kg/min. Moderate to vigorous physical activities are defined using a heart rate (HR) between 65%–95% of their maximum HR or perceiving the activity as ranging from somewhat hard to very hard on the rating of perceived exertion scale (RPE; [1]) (MacIntosh et al. [12]). The phase of menstrual cycle was not controlled as the previous study has reported that menstrual cycle does not significantly affect metabolic heat production and heat dissipation during exercise in the heat, regardless of the heat load [18]. Exclusion criteria included any current musculoskeletal injury that would limit physical activity and individuals with a history of cardiovascular, metabolic, respiratory disease or heat-related illnesses. Participants taking medications known to influence body temperature (e.g., acetaminophen, diuretics, NSAIDs aspirin and antidepressants) were excluded. All participants were medically cleared by a designated physician of this study and provided written informed consent for participation.
Exercise Protocol
Baseline Visit
The baseline visit included anthropometric measures (i.e., height and body mass) and a VO2peak treadmill exercise test. Upon arrival to the lab, urine specific gravity (USG) and urine color were assessed to ensure euhydration status (USG < 1.020). If the participants arrived with a USG between 1.020 and 1.025, they were asked to drink 500 mL of water to improve hydration status. Nude body mass was obtained while the participant was in the private bathroom. Prior to the VO2peak test, the participant was familiarized with RPE scale [1] and completed 5 min of a self-selected pace warm-up on a treadmill. During the test, the treadmill speed was increased either 0.8 or 1.6 km/h after each 2-min stage and continued until reaching volitional fatigue while monitoring their HR and RPE.
Experimental Trials
Prior to each trial, the participants were asked to collect all expelled urine into clean urine jugs from 24 h before the scheduled visit. In addition to the 24-h urine sample collection, urine specific gravity (USG) and urine color were assessed to ensure euhydration status (USG < 1.020) when the participant arrived the lab. Similar to the baseline visit, if the participants arrived with a USG between 1.020 and 1.025, indicating significant dehydration, she was asked to drink 500 mL of water to improve hydration status. Prior to the beginning of exercise, participants were asked to insert a rectal thermistor (YSI 400, YSI Inc., Yellow Spring, OH) 10–15 cm beyond the anal sphincter to provide readings of rectal temperature (Tre) and then fitted with a heart rate monitor (Polar H10, POLAR, Lake Success, NY). Skin temperature (Tsk) sensors (DS1922L, iButtonLink Technology, Whitewater, WI) were placed on the right chest, shoulder, thigh, and calf using the methods of Ramanathan [22].
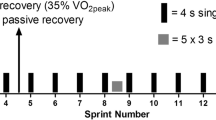
Following equipping participants with the measurement devices, they entered the environmental chamber to begin a 10-min equilibration period. Following equilibration, participants began the exercise protocol on a motorized treadmill (TRM 800–18, Precor®, Woodinville, WA). The exercise protocol, displayed in Fig. 1, was designed to simulate the intensity of a tennis match play [11, 25] and consisted of cycles of short periods of sprinting, running (10 s), jogging (15 s), walking (15 s), and standing (20 s) on a treadmill. The treadmill speed was individualized based on the participant’s velocity achieved at VO2peak (vVO2) during baseline testing and ranged between 0% of vVO2 (standing), 35% of vVO2 (walking), 70% of vVO2 (jogging/running), and 85% of vVO2 (sprinting). For exercise duration, participants completed three 30-min exercise bouts to simulate a typical 3 set tennis match. During Vest, Towels, Passive and CWI experimental trials, a 10-min break was added between the second and third exercise bout to mimic the 10-min cooling break during a tennis match. For Vest, Towels, Passive and CWI experimental trials, participants exited the environmental chamber during the 10-min cooling break. For the None trial, participants remained in the environmental chamber and there was no break between the second and third exercise bout. Trec, Tsk and HR were monitored continuously and recorded at the beginning of every 90- or 120-s break during the trials. During all exercise trials, the participants were allowed to drink water ad libitum from bottles that were all filled at one of two water bottle filling stations by the lab. The amount of fluid intake was recorded at the end of exercise trial to calculate sweat rate. The body mass loss was calculated as percentage using pre- and post-body mass. After each exercise trial, the participant was discharged when Trec reached 38.5 °C.
Cooling Intervention
The 10-min break began when the participant exited the laboratory, at minute 60 of the protocol (T60), and ended upon re-entry to the laboratory. The cooling period was tightly managed by the researchers to complete each cooling intervention within 10 min (ending at minute 70 of the protocol; T70). The environmental conditions of the locker room where the cooling interventions took place were recorded. For the CWI trial, a cold-water immersion tub (Rubbermaid, Atlanta, GA) was filled with ice water and the target water temperature was to be maintained below 15 °C. The participant was asked to submerge at least to their chest with minimal clothing worn (e.g., sports bra, compression shorts, and socks). After 5 min, they exited the tub and dried their body before going back to the laboratory. Due to the time restriction of the break, the participant did not change their clothes after CWI. If the participants submerged with socks, they are allowed to quickly change into extra pairs of socks. For the Towel trial, a towel was filled with ice and secured into 4 sections with tape. The ice towel was applied on the neck for 7 min. Additionally, two towels were soaked with ice water maintained between 0 and 3 °C and placed on the head and thighs. Towels were replaced once by soaking into the ice water again at the halfway through the 7 min. For the Vest trial, the participant was asked to wear a cooling vest (Ultimo CoolVest, Oro Sports + Safety, Buffalo, NY) for 7 min. Ice packs were stored in a freezer and taken out by a researcher 3–5 min before a 10-min break. Those ice packs were inserted into the pockets of the vest immediately before the cooling period began. For the Passive trial, the participant seated for 10 min in the locker room without receiving any cooling. For the None trial, participants did not have a 10-min break and proceeded directly to the third exercise bout after recording all physiological measures.
Statistical Analysis
All statistical analyses were completed using SPSS Statistics, Version 29 (IBM Corp). The normality of the data was determined in SPSS using Normal Q-Q plots and the assessment of skewness and kurtosis. These analyses indicated normal distribution, supporting the use of parametric tests. One-way repeated-measures analyses of variance (ANOVAs) with Bonferroni post hoc tests were performed to examine differences between the cooling intervention groups in USG, urine color, 24-h urine sample collection, sweat rate, the amount of fluid intake, and % body mass loss. One-way repeated measures ANOVAs with Bonferroni post hoc tests were performed to assess differences in pre-post measure changes of Trec, Tsk, and HR (ΔTrec, ΔTsk, and ΔHR) between five cooling strategies. Two-way repeated-measures ANOVAs with Bonferroni post hoc tests were performed to examine differences in Trec, Tsk, and HR between the four cooling intervention groups (omitting the None trial) and time points at 60-, 70-, 85- and 100-min (T60, T70, T85, and T100). Tsk was calculated by using the following formula: mean weighted Tsk = 0.3 (the sum of chest and arm Tsk) + 0.2 (the sum of thigh and calf Tsk). Additionally, two-way repeated measures ANOVAs with Bonferroni post hoc tests were performed to assess differences in ΔTrec between the four cooling intervention groups and time periods during a 10-min break (T60–T70) and after a 10-min break (T60–T85, T60–T100). All data were reported as mean (M) ± standard deviation (SD). Significance was set a priori at P < 0.05. Effect size (ES) was calculated using Cohen’s d with the resulting magnitude-based interpretation of the effect; small (0.20–0.49), medium (0.50–0.79), or large (> 0.8) [5]. All data are reported as mean ± SD.
Results
Participants were exercising in an environmentally controlled chamber with WBGT of 30.9 ± 0.2 °C (ambient temperature 40.3 ± 0.4 °C, 31.2% ± 5.8% RH). The environmental conditions of the locker room where the cooling interventions took place were an ambient temperature of 22.3 ± 0.6 °C with 29.4% ± 4.4% RH. During CWI trial, the water temperature was maintained at 14.6 ± 0.5 °C. For Towel trial, the temperature of ice water was 2.4 ± 0.9 °C. There were no significant differences in pre- and post-USG, urine color, the amount of 24-h urine sample, fluid intake, sweat rate, and % body mass loss between cooling intervention groups (P > 0.10) (Table 1).
Comparison Between with and Without a 10-min Break
The pre-post exercise ΔTrec for each trial is displayed in Fig. 2. There was a significant difference in ΔTrec between None and CWI (P < 0.001, d = 1.71). There were no significant differences between None and Towel, Vest, and Passive while the effect size indicated a moderate change with a 10-min break using those cooling strategies (P > 0.05, d = 0.52–0.67). There were no significant differences in ΔTsk (P = 0.132, d < 0.20) and ΔHR (P = 0.430, d < 0.23) between None and other four cooling intervention groups.
Comparison of rise in rectal temperature (ΔTrec) pre-post 90-min of intermittent exercise in the heat with and without various 10-min cooling interventions. *Significant difference from None, #Significant difference from CWI, P < 0.05. None received no 10-min break. CWI cold water immersion, Towel ice towel with dampened towels, Vest cooling vest, Passive passive rest
Effectiveness of Different Cooling Interventions on Physiological Measures
During the first 60 min of exercise (just prior to the 10-min break), there were no significant differences in Trec, Tsk and HR between the groups indicating that all trials and exercise sessions were similar. Mean Trec is displayed in Fig. 3. There was no significant difference in Trec between the groups at the end of the 10-min break, at T70 (P > 0.05, d = 0.57–1.12). However, Trec was significantly lower for the CWI compared to all other cooling intervention groups at T85 (P < 0.003, d = 1.68–1.81) and T100 (P < 0.006, d = 1.49–1.73). Additionally, there was no significant difference in ΔTrec during T60–T70 between the cooling groups (P > 0.05, d = 0.53–0.76). However, ΔTrec during T60–T85 and T60–T100 was significantly different between the groups. Pairwise comparisons revealed that CWI had a greater decrease in ΔTrec compared to Vest (P < 0.002, d = 1.39–1.51) and Passive (P < 0.001, d = 1.35–1.48) during T60–T85 and T60–T100. There was no significant difference in ΔTrec between CWI and Towel during T60–T85 and T60–T100, but CWI had a large ES compared to Towel (P > 0.088, d = 0.88–0.98). Overall, pre-post exercise ΔTrec indicated that CWI had significantly smaller ΔTrec compared to other cooling groups at the end of exercise trial (P < 0.003; Fig. 2). Mean weighted Tsk is shown in Fig. 4. CWI was significantly lower than in the cooling intervention groups at T70 (P < 0.002, d = 3.81–6.99) and T85 (P < 0.005, d = 1.72–2.70). Additionally, Towel was significantly lower compared to Vest and Passive at T70 (P = 0.002, d = 2.54, P < 0.001, d = 2.46 respectively). There was no significant difference between groups at T100 (P > 0.05, d = 0.62–0.92). Mean HR is displayed in Fig. 5. CWI was significantly lower compared to Towel and Passive at T70 (P = 0.047, d = 0.72, P = 0.008, d = 0.95, respectively) and other cooling intervention groups at T85 (P < 0.028, d = 0.64–0.71). However, there was no significant difference between groups at T100 (P < 0.05, d = 0.35–0.47).
Mean rectal temperature and standard deviation (Trec) during a 10-min cooling break (60–70 min) and subsequent intermittent exercise in the heat. *Significant group by time difference in Trec between CWI and other cooling intervention groups. Letters indicate significant Trec decrease (ΔTrec) in CWI vs. Towel (a), Vest (b), Passive (c), at indicated points of comparison P < 0.05
Discussion
Our primary purpose was to assess the impact of five strategies during a 10-min break on internal body temperature response and report the effectiveness of the various cooling strategies during intermittent exercise in the heat. To our knowledge, this is one of the select few studies to evaluate the effect of in-play cooling interventions, specifically during a 10-min break in a simulated tennis match.
Comparison Between with and Without a 10-min Break
The trial where participants received no break provided valuable results for the real-life situations in addition to the other four cooling interventions. Our findings showed ΔTrec was significantly different between None vs. CWI while there were no differences between None vs. Towel, Vest, and Passive. Most tennis players are recreationally engaging in tennis and participating in non-sanctioned tennis tournaments without any heat-related rules and guidelines [9]. Although the risk of uncompensable heat stress and developing EHIs would vary depending on intrinsic (e.g., heat acclimation status, anthropometric characteristics, hydration status) and extrinsic (e.g., environmental condition, clothing) factors [3], a significant number of the tennis population is at risk of developing EHIs when participating in the unsanctioned tennis tournaments under hot conditions throughout the year. Compared to None, 5-min of CWI effectively reduced Trec within a 10-min break and helped mitigate thermal strain during the subsequent exercise period in the heat. Other cooling interventions did not show a significant difference in ΔTrec compared to None. However, the ES for ΔTrec indicated a medium effect with a 10-min break using other cooling strategies. Therefore, the implementation of a 10-min break alone would be moderately beneficial to mitigate thermal strain and prevent EHIs during tennis tournaments in hot conditions and highly effective if CWI is utilized. To date, the lack of heat-related rules and guidelines is a matter of great concern. It is crucial for tennis governing bodies, tournament officials, and the medical team to take steps towards improving athlete safety in the near future.
Effectiveness of Different Cooling Interventions on Physiological Measures
Our study demonstrated significantly different responses in Trec, ΔTrec, Tsk and HR after a 10-min break between the four cooling intervention groups. CWI trial had a significantly greater decrease in ΔTrec during the first 15-min of subsequent exercise period and maintained Trec below 38.5 °C until the end of exercise trial. Tippet et al. reported that Trec decreased by 0.25 ± 0.20 °C after a 10-min break [28]. Since their study was conducted during an outdoor tournament, the type of cooling interventions was not controlled to optimize the cooling intervention period (e.g., towel dry, change of clothes). In our study, Trec decreased during a 10-min break by 0.76 ± 0.5 °C with a 5-min of CWI while 7-min of repeated ice-soaked towels and cooling vest decreased Trec by 0.51 ± 0.4 °C and 0.47 ± 0.3 °C respectively. Furthermore, there was a significant after drop or lasting effect with 5-min of CWI [20]. Previous studies described that after drop is caused by a rapid redistribution of blood from the cooled peripheral tissues to the core. Our study observed decrease in Trec by 0.28 ± 0.2 °C during the first 15 min of subsequent exercise periods in the CWI trial. Our finding aligns with previous studies that reported after drop occurring within the first 20 min of the subsequent exercise period following 2.5- to 5-min of CWI intervention, which was associated with a decrease in Trec by 0.4° [7, 19]. Overall, there was a reduction of 1.04 ± 0.5 °C in Trec during and after a 5-min of CWI. After the first 15 min of exercise, Trec began to increase gradually due to a combined effect of an increase in metabolism and restoration of normal muscle temperature which results in the distribution of heat from the active musculature to the core. Previous studies suggested that the increased heat storage capacity induced by the after drop in Trec likely contributes to the overall beneficial effects in subsequent intermittent exercise period [7, 14, 15, 31]. Although the effects of cooling on Tsk, and HR were not maintained at the end of exercise period, the reduction in HR during the CWI trial at T70 and T85 would be explained by the effect of the after drop. Our study also observed that there was no significant difference in ΔTrec between CWI and Towel during and after a 10-min break, suggesting that the use of ice towel with dampened towels during a cooling break may provide a sufficient source of body cooling and minimize the logistical issues associated with CWI (e.g., drying off one’s body and changing clothes, etc.).
Interestingly, no significant differences were observed in Trec, ΔTrec and HR between Towel trial and Vest/Passive trials. Although Tsk was significantly lower in Towel trial at T70 compared to Vest and Passive trials, the cooling effect was not seen at T85 and T100. Towel trial also decreased Trec by 0.56 ± 0.5 °C during T60–T85. However, the observed after drop in Vest and Passive did not show a significant difference from that of Towel trial (0.49 ± 0.3 °C and 0.47 ± 0.3 °C respectively). Since the magnitude of the after drop was smaller in Towel compared to CWI trial, the cooling effects of Towel trial did not result in significant reductions in Trec, and HR compared to Vest and Passive during the subsequent exercise period.
Feasibility of CWI Implementation During Tennis Events in Hot Conditions
Our study also assessed the feasibility of CWI intervention by tightly managing the cooling period within 10 min. To adhere to the limited period of a break in a tennis match, our participants were unable to change their clothes following CWI. Some participants experienced discomfort during the subsequent exercise period due to the wetness of their clothing, while others found the CWI refreshing and preferred it over the other cooling interventions. In a real-world setting, it is unlikely that athletes would want to compete in wet clothes, thus reducing the likelihood of success from an implementation perspective seeing as the other cooling strategies used still effectively attenuated the rise in internal body temperature at the completion of exercise. Also, and while effectively lowering Trec, CWI reduces muscle temperature directly and could negatively affect exercise performance by altering the contractile function of working muscles [10, 29]. The cooling effects of CWI with extremely cold water (< 8 °C) include decreased muscle power, force, velocity, and a loss of dexterity [6, 13, 24]. A previous study reported that the effect of cooling resulted a reduction in lower extremity power output persisting for 10 min, while the decline in speed and acceleration lasted up to 20 min following a 15-min of lower extremity CWI with a water temperature of 5 °C [6]. Therefore, when providing guidelines for cooling interventions in athletes, it is imperative to evaluate the potential impact on exercise performance and incorporate strategies to prevent EHIs while optimizing the performance. Successful implementation of CWI would also require collaboration and logistical coordination between tournament officials and medical providers during tennis events.
Limitations
Our participants were allowed to drink water ad libitum throughout the trials, even though tennis players typically have limited opportunities for hydration, mainly during changeover breaks or between sets. Given that Trec increased by ~ 0.2 °C for every 1% of body mass loss [4], the availability of additional hydration opportunities could have an impact on the changes in physiological measures, including Trec and HR in this study. Future studies should control the hydration opportunity to replicate the real-life situation for tennis players in hot environments. Additionally, our study recorded Trec only at the beginning and the end of a 10-min break (e.g., T60 and T70) and was not able to report the exact cooling rate for each strategy during a 10-min break. Although there was no significant difference in Trec during T60 and T70 between the groups, the cooling rate would provide crucial information, particularly when selecting a cooling strategy within a short, constrained break period. Future study should investigate the exact cooling rate for each strategy during a 10-min break. Lastly, our study used a traditional treadmill to simulate the intensity of a tennis match in the laboratory. The treadmill speed was changed manually between 10–30 s by a researcher. A tennis match is characterized by shorter periods (4–10 s) of high intensity activities and short recovery periods (10–20 s), interspersed with rest periods lasting 60–90 s [8]. Moreover, the duration of a match could be more than 3 h. While our study still observed the changes in physiological measure throughout the exercise trials, there were challenges when simulating the complex intermittent exercise in the laboratory.
Conclusion
The implementation of a 10-min break with CWI effectively reduced thermal strain as measured by ΔTrec compared to None and Towel, Vest, and Passive strategies. CWI may be a potential strategy to mitigate the risk of EHIs during tennis tournaments in hot conditions. However, the implementation of CWI as a risk mitigation strategy during a tennis match must be considered when determining the most optimal cooling strategy to utilize given the implications that CWI has on performance outcomes. While this study demonstrated that CWI effectively attenuated the rise in internal body temperature during the subsequent intermittent treadmill exercise, simulating the intensity of a tennis match, future studies should aim to address the logistical challenge of CWI implementation for athletes, with consideration of prevention of EHIs and optimization of exercise performance.
Data availability
Data are available upon reasonable request.
References
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81.
Byrne C, Lee JKW, Chew SAN, Lim CL, Tan EYM. Continuous thermoregulatory responses to mass-participation distance running in heat. Med Sci Sports Exerc. 2006;38(5):803–10. https://doi.org/10.1249/01.mss.0000218134.74238.6a.
Casa DJ, DeMartini JK, Bergeron MF, Csillan D, Eichner ER, Lopez RM, Ferrara MS, Miller KC, O’Connor F, Sawka MN, Yeargin SW. National Athletic Trainers’ Association Position Statement: exertional heat illnesses. J Athl Train. 2015;50(9):986–1000. https://doi.org/10.4085/1062-6050-50.9.07.
Casa DJ, Stearns RL, Lopez RM, Ganio MS, McDermott BP, Walker Yeargin S, Yamamoto LM, Mazerolle SM, Roti MW, Armstrong LE, Maresh CM. Influence of hydration on physiological function and performance during trail running in the heat. J Athl Train. 2010;45(2):147–56. https://doi.org/10.4085/1062-6050-45.2.147.
Cohen J. Statistical power analysis for the behavioral sciences. New York: Routledge; 1988.
Didehdar D, Sobhani S. The effect of cold-water immersion on physical performance. J Bodyw Mov Ther. 2019;23(2):258–61. https://doi.org/10.1016/j.jbmt.2018.05.001.
Egaña M, Jordan L, Moriarty T. A 2.5 min cold water immersion improves prolonged intermittent sprint performance. J Sci Med Sport. 2019;22(12):1349–54. https://doi.org/10.1016/j.jsams.2019.07.002.
Fernandez J, Mendez-Villanueva A, Pluim BM. Intensity of tennis match play. Br J Sports Med. 2006;40(5):387–91. https://doi.org/10.1136/bjsm.2005.023168.
Internatinal Tennis Federetion. ITF Global Tennis Report 2021. 2021. http://itf.uberflip.com/i/1401406-itf-global-tennis-report-2021/7? Accessed 16 Aug 2021.
Jiang D, Yu Q, Liu M, Dai J. Effects of different external cooling placements prior to and during exercise on athletic performance in the heat: a systematic review and meta-analysis. Front Physiol. 2023;13:1091228. https://doi.org/10.3389/fphys.2022.1091228.
Lynch GP, Périard JD, Pluim BM, Brotherhood JR, Jay O. Optimal cooling strategies for players in Australian Tennis Open conditions. J Sci Med Sport. 2018;21(3):232–7. https://doi.org/10.1016/j.jsams.2017.05.017.
MacIntosh BR, Murias JM, Keir DA, Weir JM. What is moderate to vigorous exercise intensity? Front Physiol. 2021;12:682233. https://doi.org/10.3389/fphys.2021.682233. PMID: 34630133; PMCID: PMC8493117
Maley MJ, Minett GM, Bach AJE, Zietek SA, Stewart KL, Stewart IB. Internal and external cooling methods and their effect on body temperature, thermal perception and dexterity. PLoS ONE. 2018;13(1):e0191416. https://doi.org/10.1371/journal.pone.0191416.
Marino FE. Methods, advantages, and limitations of body cooling for exercise performance. Br J Sports Med. 2002;36(2):89–94. https://doi.org/10.1136/bjsm.36.2.89.
McCarthy A, Mulligan J, Egaña M. Postexercise cold-water immersion improves intermittent high-intensity exercise performance in normothermia. Appl Physiol Nutr Metab. 2016;41(11):1163–70. https://doi.org/10.1139/apnm-2016-0275.
Misailidi M, Mantzios K, Papakonstantinou C, Ioannou LG, Flouris AD. Environmental and psychophysical heat stress in adolescent tennis athletes. Int J Sports Physiol Perform. 2021;16(12):1895–900. https://doi.org/10.1123/ijspp.2020-0820.
Naito T, Nakamura M, Muraishi K, Eda N, Ando K, Takemura A, Akazawa N, Hasegawa H, Takahashi H. In-play optimal cooling for outdoor match-play tennis in the heat. Eur J Sport Sci. 2022;22(3):326–35. https://doi.org/10.1080/17461391.2020.1870160.
Notley SR, Dervis S, Poirier MP, Kenny GP. Menstrual cycle phase does not modulate whole body heat loss during exercise in hot, dry conditions. J Appl Physiol. 2019;126(2):286–93. https://doi.org/10.1152/japplphysiol.00735.2018.
Périard JD, Eijsvogels TMH, Daanen HAM. Exercise under heat stress: thermoregulation, hydration, performance implications, and mitigation strategies. Physiol Rev. 2021;101(4):1873–979. https://doi.org/10.1152/physrev.00038.2020.
Proulx CI, Ducharme MB, Kenny GP. Effect of water temperature on cooling efficiency during hyperthermia in humans. J Appl Physiol. 2003;94(4):1317–23. https://doi.org/10.1152/japplphysiol.00541.2002.
Racinais S, Moussay S, Nichols D, Travers G, Belfekih T, Schumacher YO, Periard JD. Core temperature up to 41.5°C during the UCI Road Cycling World Championships in the heat. Br J Sports Med. 2019;53(7):426–9. https://doi.org/10.1136/bjsports-2018-099881.
Ramanathan NL. A new weighting system for mean surface temperature of the human body. J Appl Physiol. 1964;19:531–3. https://doi.org/10.1152/jappl.1964.19.3.531.
Robin N, Dominique L, Coudevylle GR. Playing tennis in hot environment: applied strategies and new directions. ITF Coach Sport Sci Rev. 2021;29(83):10–2. https://doi.org/10.52383/itfcoaching.v29i83.47.
Schniepp J, Campbell TS, Powell KL, Pincivero DM. The effects of cold-water immersion on power output and heart rate in elite cyclists. J Strength Cond Res. 2002;16(4):561–6.
Schranner D, Scherer L, Lynch GP, Korder S, Brotherhood JR, Pluim BM, Périard JD, Jay O. In-play cooling interventions for simulated match-play tennis in hot/humid conditions. Med Sci Sports Exerc. 2017;49(5):991–8. https://doi.org/10.1249/MSS.0000000000001183.
Smith MT, Reid M, Kovalchik S, Wood T, Duffield R. Heat stress incidence and matchplay characteristics in Women’s Grand Slam Tennis. J Sci Med Sport. 2018;21(7):666–70. https://doi.org/10.1016/j.jsams.2017.11.006.
Smith MT, Reid M, Kovalchik S, Woods TO, Duffield R. Heat stress incident prevalence and tennis matchplay performance at the Australian Open. J Sci Med Sport. 2018;21(5):467–72. https://doi.org/10.1016/j.jsams.2017.08.019.
Tippet ML, Stofan JR, Lacambra M, Horswill CA. Core temperature and sweat responses in Professional Women’s Tennis players during tournament play in the heat. J Athl Train. 2011;46(1):55–60. https://doi.org/10.4085/1062-6050-46.1.55.
Treigyte V, Eimantas N, Venckunas T, Brazaitis M, Chaillou T. Moderate muscle cooling induced by single and intermittent/prolonged cold-water immersions differently affects muscle contractile function in young males. Front Physiol. 2023;14:1172817. https://doi.org/10.3389/fphys.2023.1172817.
Women’s Tennis Association. WTA Rules. 2023. https://www.wtatennis.com/wta-rules. Accessed 16 Dec 2023.
Yeargin SW, Casa DJ, McClung JM, Knight JC, Healey JC, Goss PJ, Harvard WR, Hipp GR. Body cooling between two bouts of exercise in the heat enhances subsequent performance. J Strength Cond Res. 2006;20(2):383–9. https://doi.org/10.1519/R-18075.1.
Acknowledgements
Funding for this work was supported by Korey Stringer Institute.
Funding
This work was funded by the Korey Stringer Institute.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception. Material preparation, and data collection were performed by AY, JRO, AMD, FAC, and EBF. Data analyses were performed by AY, RLS and WMA. The first draft of the manuscript was written by AY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
This work is the author’s (WMA) own and not that of the United States Olympic & Paralympic Committee, or any of its members or affiliates. WMA receives royalties from Springer Nature. WMA also receives compensation from Emerja Corporation, My Normative, Wu Tsai Human Performance Alliance as a member of the respective advisory boards. WMA is the owner of Adams Sports Medicine Consulting LLC.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the University (11/21/2022 /NO: H22-0138).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoshihara, A., O’Neil, J.R., Defino, A.M. et al. Impact of Various 10-min Cooling Breaks on Internal Body Temperature Responses During Subsequent Intermittent Exercise in the Heat: Application to Tennis. J. of SCI. IN SPORT AND EXERCISE 6, 244–252 (2024). https://doi.org/10.1007/s42978-024-00281-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42978-024-00281-0