Abstract
Objective
Thoracoscopic repair of esophageal atresia (EA) in the presence of right aortic arch (RAA) in neonates is still not widely reported due to its rare prevalence. This systematic review was performed for thoracoscopic repair of EA and RAA in the past two decades.
Methods
PubMed, Google Scholar, and Science Direct databases were searched for articles on children with the thoracoscopic repair of EA and RAA published between 2002 and 2023. Data were extracted with regards to number of patients, preoperative diagnosis and approach, intraoperative diagnosis and approach, conversion, morbidity, and mortality.
Results
The review identified 8 articles and offered a total of 22 neonates with EA and RAA with attempted thoracoscopic repair. Data extrapolated showed (a) preoperative diagnosis confirmation (n = 10), (b) approach with confirmed preoperative diagnosis: right thoracoscopy (n = 5), left thoracoscopy (n = 5), (c) intraoperative diagnosis (n = 12), (d) approach after intraoperative diagnosis: shift right thoracoscopy to left thoracoscopy (n = 6), right thoracoscopy (n = 6), open conversion (n = 2), (e) total conversions: total (n = 4): thoracotomy (n = 2), right thoracoscopy to left thoracoscopy and then right thoracotomy (n = 1), to left thoracotomy (n = 1), (f) repair outcomes: primary repairs (n = 17) and staged repair (n = 5),(g) morbidity: leaks( n = 2), stricture (n = 1), no data (n = 11) and (h) mortality (n = 3).
Conclusion
There is an equal distribution in the side of approach in EA with preoperative diagnosis of RAA. This is also evident when the findings are confirmed intraoperatively. In 50% of the cases with intraoperative RAA findings, a switch to the left side was preferred. Conversions are reported in approximately 14% cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The past two decades have witnessed advances in the minimally access surgical approach to esophageal atresia (EA) repairs. The thoracoscopic repair is now considered a standard approach in EA in many tertiary pediatric surgery centers.
The right aortic arch (RAA) is regarded as the anomalous curvature of the aorta that descends on the right side of the spine. Despite only being reported in 1.8%–3.6% of newborns with EA [1, 2], RAA poses a predicament regarding the optimal surgical approach, mainly with regards to the side for repair. The presence of RAA has been reported to increase the technical difficulty of the operation, due to the aortic arch being in front of the esophagus and obscuring its upper pouch. Although the presence of RAA is not a contraindication for the right-sided thoracic approach, an unrecognized RAA found intraoperatively may complicate the repair of EA and TEF (tracheoesophageal fistula) [3, 4].
Echocardiography still remains the gold standard in the diagnosis of cardiac and vascular anomalies. Unfortunately, RAA can be correctly identified in only 1 in 4–5 neonates on echocardiography routinely performed prior to EA/TEF repair [5]. Prior to the past two decades, suspicion of RAA was reported to be an indication for a left sided approach (thoracotomy) [2]. There are ongoing discussions in the literature with regards to the optimal approach for the repair of EA/TEF in neonates with RAA, albeit focusing mainly on thoracotomies [6]. The present systematic review was performed to analyze thoracoscopic repair of EA in cases with RAA.
Methods
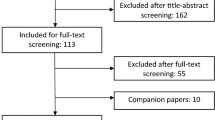
The systematic review was performed using the PRISMA guidelines [7]. PubMed, Science Direct, and Google Scholar databases were searched for articles on thoracoscopic repair of EA and RAA published from January 2002 to September 2023. The search terms were “esophageal atresia”, “right-sided aortic arch”, “thoracoscopic repair” and “neonates”. Inclusion criteria were English-language articles reporting original data on the diagnosis and treatment of newborns with EA and RAA (Fig. 1).
Two independent reviewers extracted information related to eligible articles. Full manuscripts were reviewed, and data were extracted for number of patients, preoperative diagnosis of RAA and approach, intraoperative diagnosis and approach, type of surgical repair, conversions, morbidity, and mortality rate (Table 1).
Results
The initial search of the 3 databases yielded 89 articles. After the exclusion of duplicates and articles not relevant to this analysis, 8 articles met the inclusion criteria. The articles were retrospective studies, case reports or case series and a single multi-institutional study. The 8 articles reported on 22 cases of EA with RAA [8,9,10,11,12,13,14,15]. All 22 cases had a preoperative chest X-ray and an echocardiography.
RAA was confirmed prior to EA surgery in 10 cases [8, 12,13,14,15]. Seliem et al. [9] reported 4 cases of preoperatively identified RAA, and the planned approach for the cases stayed unchanged as the right thoracoscopic approach. Two of those cases required conversion to right thoracotomy. Rothenberg et al. [12] and Holcomb et al. [15] identified 4 cases preoperatively, 2 cases each. However, the approach of choice was the left thoracoscopy in all these cases. The 4 cases were completed successfully thoracoscopically with fistula ligation and primary anastomosis was achieved. Saka et al. also reported a single case that was preoperatively diagnosed with a left-sided primary repair [14]. There is also another primary repair achieved through right thoracoscopy [13].
In 12 cases, the preoperative diagnosis did not confirm a RAA that was subsequently found at the time of repairs using right thoracoscopy. Of these, 5/12 cases were successfully completed through right thoracoscopy [8, 10, 13,14,15]. Switching to left thoracoscopy was opted in 6/12 cases [8, 9, 11, 15]; one of these the converted to right thoracotomy in the case of unforeseen RAA with aberrant left subclavian artery (ALSA) [8]. One case (1/12) had conversion to left thoracotomy [14].
Primary repair was achieved and reported for 17 cases (right n = 8/left n = 9) [8, 10, 12,13,14,15] and four cases of staged repair due to long gap atresia were reported [8, 9, 11]. There was one case with a mirror-image right arch, that underwent ligation of the fistula, an esophagostomy, and a gastrostomy [8].
Four conversions were reported [8, 14, 15]. Two conversions were to right thoracotomy [8, 14], both being in cases with preoperative confirmed diagnosis of RAA. There was one conversion directly from right thoracoscopy to left thoracotomy after intraoperative diagnosis of RAA and unsuccessful operative progression [15], and one to left thoracoscopy then to right thoracotomy, also in a case of intraoperative diagnosis of RAA.[8].
Data on morbidity was only reported in 2/3 of the cases. There were 2 reports of anastomotic leakage [8], and one case of postoperative stricture in the long-term follow-up [10] without further information on dilatation or interventions. There was no available data on morbidity for 9 cases.
There were 3 lethal outcomes reported [8]. All three patients were diagnosed with RAA along with ALSA. The cause of death was septicemia (n = 1) and associated congenital anomalies (n = 2); the anomalies being ventricular septal defect (VSD) and portal hypertension in one, and atrial septal defect (ASD), ventricular hypertrophy, and bilateral renal back pressure in the other [8].
Discussion
The first thoracoscopic repair of esophageal atresia was at the International Pediatric Surgical Endoscopy (IPEG) meeting in Berlin in 1999 [16]. The operation was on a 2-month-old infant with isolated esophageal atresia. In 2000, Rothenberg reported the first “Thoracoscopic repair of a tracheoesophageal fistula in an infant.” [17]. Since 2000, there has been a focus by pediatric surgeons on the thoracoscopic approach to EA/TEF. Despite the similarity in the postoperative outcome and morbidity between the thoracoscopic repair and thoracotomy, the advantages of minimal access surgery include earlier extubation, less pain, and shorter hospital stay [18, 19].
Echocardiography has been used as a non-invasive technique to screen for vascular anomalies, including the laterality of the aortic arch. However, the sensitivity of echocardiography is low. In this review, it was found that over half of the cases were missed preoperatively and were identified intraoperatively.
RAA poses a dilemma about the optimal surgical approach, mainly the side of the thoracoscopy for repair. In the reviewed cases, there has been an equal number of right and left thoracoscopic approaches, both associated with successful repairs. Nevertheless, Rothenberg et al., Saka et al., and Holcomb et al. opted directly for a left thoracoscopy in the case of a preoperative diagnosis of RAA [12, 14, 15]. Oshima et al. and Tainaka et al. reported the switch to the left thoracoscopy on intraoperative diagnosis of RAA with completed primary repair [9, 11].
In the series of 104 patients described by Holcomb et al., 6 patients who were found to have RAA, either pre- or intraoperatively, all received their operative repair through the left chest, 5 with thoracoscopy, and 1 with thoracotomy [15]. This review also identified that the presence of RAA did not interfere with the primary thoracoscopic repair, which was achieved in 70% of the cases.
The morbidities reported were not specific to the RAA, and generally not different from the cases with left aortic arch. They varied between leaks, which was managed conservatively, and strictures for which more data was not found [8].
Regarding the mortalities, the three cases reported had RAA combined with ALSA. While isolated RAA is usually asymptomatic, RAA combined with ALSA can worsen respiratory distress in a newborn with EA [4]. The reported mortalities were not associated with surgical complications.
EA with RAA diagnosed preoperatively is approached equally from the right and the left side. If the diagnosis is intraoperative, 50% had a preference to switch to the left side to continue with the repair.
Conclusion
In the present systematic review, EA with RAA can be completed with access from both sides. Also, when unable to proceed with right thoracoscopy, the switch to left thoracoscopy offers an option to complete the repair. Future studies with larger sample sizes are still required to compare between the two approaches.
Data availability
Data analyzed in this study has been included in the references.
References
Chittmittrapap S, Spitz L, Kiely EM, Brereton RJ (1989) Oesophageal atresia and associated anomalies. Arch Dis Child 64:364–368. https://doi.org/10.1136/adc.64.3.364
Babu R, Pierro A, Spitz L, Drake DP, Kiely EM (2000) The management of oesophageal atresia in neonates with right-sided aortic arch. J Pediatr Surg 35:56–58. https://doi.org/10.1016/s0022-3468(00)80013-5
Harrison MR, Hanson BA, Mahour GH, Takahashi M, Weitzman JJ (1977) The significance of right aortic arch in repair of esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 12:861–869. https://doi.org/10.1016/0022-3468(77)90595-4
Allen SR, Ignacio R, Falcone RA, Alonso MH, Brown RL, Garcia VF et al (2006) The effect of a right-sided aortic arch on outcome in children with esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 41:479–483. https://doi.org/10.1016/j.jpedsurg.2005.10.051
Wood JA, Carachi R (2012) The right-sided aortic arch in children with oesophageal atresia and tracheo-oesophageal fistula. Eur J Pediatr Surg 22:3–7. https://doi.org/10.1055/s-0031-1285906
Parolini F, Armellini A, Boroni G, Bagolan P, Alberti D (2016) The management of newborns with esophageal atresia and right aortic arch: a systematic review or still unsolved problem. J Pediatr Surg 51:304–309. https://doi.org/10.1016/j.jpedsurg.2015.10.043
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Seleim HM, Wishahy AMK, Magdy B, Elseoudi M, Zakaria RH, Kaddah SN et al (2022) The dilemma after an unforeseen aortic arch anomalies at thoracoscopic repair of esophageal atresia: is curtailing surgery still a necessity? Scand J Surg 111:14574969221090488. https://doi.org/10.1177/14574969221090487
Oshima K, Uchida H, Tainaka T, Tanano A, Shirota C, Yokota K et al (2017) Left thoracoscopic two-stage repair of tracheoesophageal fistula with a right aortic arch and a vascular ring. J Minim Access Surg 13:73–75. https://doi.org/10.4103/0972-9941.181771
Fonte J, Barroso C, Lamas-Pinheiro R, Silva AR, Correia-Pinto J (2016) Anatomic thoracoscopic repair of esophageal atresia. Front Pediatr 4:142. https://doi.org/10.3389/fped.2016.00142
Tainaka T, Uchida H, Tanano A, Shirota C, Hinoki A, Murase N et al (2017) Two-Stage thoracoscopic repair of long-gap esophageal atresia using internal traction is safe and feasible. J Laparoendosc Adv Surg Tech A 27:71–75. https://doi.org/10.1089/lap.2016.0207
Rothenberg SS (2012) Thoracoscopic repair of esophageal atresia and tracheo-esophageal fistula in neonates: evolution of a technique. J Laparoendosc Adv Surg Tech A 22:195–199. https://doi.org/10.1089/lap.2011.0063
Wong KK, Tam PK (2010) Thoracoscopic repair of esophageal atresia through the right chest in neonates with right-sided aortic arch. J Laparoendosc Adv Surg Tech A 20:403–404. https://doi.org/10.1089/lap.2009.0265
Saka R, Tazuke Y, Ueno T, Nomura M, Deguchi K, Okuyama H (2020) Esophageal atresia with right aortic arch: an experience of thoracoscopic repair through left thorax. Asian J Endosc Surg 14:301–304. https://doi.org/10.1111/ases.12862
Holcomb GW 3rd, Rothenberg SS, Bax KM, Martinez-Ferro M, Albanese CT, Ostlie DJ et al (2005) Thoracoscopic repair of esophageal atresia and tracheoesophageal fistula: a multi-institutional analysis. Ann Surg 242:422–428. https://doi.org/10.1097/01.sla.0000179649.15576.db
Lobe TE, Rothenberg SS, Waldschmitt J et al (1999) Thoracoscopic repair of esophageal atresia in an infant: a surgical first. Pediatr Endosurg Innov Tech 3:144–148. https://doi.org/10.1089/pei.1999.3.141
Rothenberg SS (2000) Thoracoscopic repair of tracheoesophageal fistula in a newborn infant. J Pediatr Endosurg Innov Tech 37:869–872. https://doi.org/10.1089/pei.2000.4.289
Okuyama H, Saka R, Takama Y, Nomura M, Ueno T, Tazuke Y (2019) Thoracoscopic repair of esophageal atresia. Surg Today 50:966–973. https://doi.org/10.1007/s00595-019-01884-9
Yang Y, Dong R, Zheng C et al (2016) Outcomes of thoracoscopy versus thoracotomy for esophageal atresia with tracheoesophageal fistula repair. Medicine (Baltimore) 95:1–6. https://doi.org/10.1097/MD.0000000000004428
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
None.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Elsherbiny, S., Saxena, A.K. Thoracoscopic repair of esophageal atresia with right-sided aortic arch: systematic review. J Ped Endosc Surg 5, 165–169 (2023). https://doi.org/10.1007/s42804-023-00206-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42804-023-00206-8