Abstract
Helicobacter pylori is the most common cause of gastroduodenal diseases. The concept that cagA-positive H. pylori is a risk factor for gastric cancer appears to be true only for H. pylori strains from Western countries. Other virulent genes may have a synergistic interaction with cagA during pathogenesis. This study aims to investigate H. pylori cagA, vacA, and iceA prevalence, genotypes, and their association to clinical outcomes in Vietnamese patients. The cagA status and vacA and iceA genotypes were determined using the PCR technique on DNA extracted from gastric biopsies of 141 patients with gastroduodenal diseases. After performing molecular analysis for cagA, vacA, and iceA genes, samples with mixed H. pylori strains, positivity, or negativity for both cagA and cagPAI-empty site, or unidentified genotypes were excluded. Finally, 107 samples were examined. The presence of the cagA, vacA, and iceA genes were detected in 77.6%, 100%, and 80.4% of cases, respectively. Notably, cagA( +) with EPIYA-ABD, vacA s1i1m1, vacA s1i1m2, iceA1, and iceA2 accounted for 73.8%, 44.9%, 33.6%, 48.6%, and 31.8% of cases, respectively. Four iceA2 subtypes (24-aa, 59-aa, 94-aa, and 129-aa variants) were found, with the 59-aa variant the most prevalent (70.6%). The cagA( +)/vacAs1i1m1/iceA1 and cagA( +)/vacAs1i1m2/iceA1 combinations were found in 26.2% and 25.1% of cases, respectively. A multivariable logistic regression analysis was performed, after adjusting for age and gender, with the gastritis group was used as a reference control. Statistically significant associations were found between the vacA s1i1m2 genotype, the iceA1 variant, and the cagA( +)/vacAs1i1m2/iceA1 combination and gastric cancer; the adjusted ORs were estimated as 18.02 (95% CI: 3.39–95.81), 4.09 (95% CI: 1.1–15.08), and 16.19 (95% CI: 3.42–76.66), respectively. Interestingly, for the first time, our study found that vacA s1i1m2, but not vacA s1i1m1, was a risk factor for gastric cancer. This study illustrates the genetic diversity of the H. pylori cagA, vacA, and iceA genes across geographical regions and contributes to understanding the importance of these genotypes for clinical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Helicobacter pylori (H. pylori) is a spiral-shaped gram-negative bacterium that colonizes the gastric mucosa of more than half of the population worldwide. This bacterium is a leading cause of gastroduodenal diseases. Notably, H. pylori has been classified as a Group I carcinogen by the International Agency for Research on Cancer (IARC) since 1994 [1]. The pathogenesis of H. pylori infection is associated with their toxins, the most well-studied of which are the virulence factors cytotoxin-associated gene A (CagA) and vacuolating cytotoxin A (VacA) [2, 3].
The cagA gene, located at the 3’-end of the cag pathogenicity island (cagPAI), encodes the CagA protein, which is prevalent in 60–70% of H. pylori worldwide [4, 5]. It is thought that cagA-positive H. pylori strains are a risk factor for gastric cancer (GC). However, this appears to be true only for H. pylori strains in Western countries, where the cagA-positivity rate for H. pylori is only about 40% [6]. At the same time, regardless of gastroduodenal disease, H. pylori strains in East Asian countries exhibit extremely high rates of possessing the cagA gene, up to 90–95% [4, 7, 8]. Therefore, the cagA gene is not the only biological indicator for assessing the clinical outcome caused by H. pylori [9].
The vacA gene, which encodes the VacA protein, is found in all H. pylori strains. This vacuolating cytotoxin plays an important role in apoptosis and the proinflammatory response [7]. The diversity of vacA genotypes causes differences in cytotoxic activity between specific H. pylori strains [10, 11]. The signal region, which has two alleles (s1 and s2), the middle region, which has two alleles (m1 and m2), and the intermediate region, which has two alleles (i1 and i2), are the three main parts of the vacA gene [12, 13]. The H. pylori strains with the vacA s1m1 genotype exhibit the highest vacuolating activity, higher than the vacA s2m2 strains [10]. The toxicity of the vacA s1m2 strains is determined by the combination of alleles i1 or i2, with vacA s1i1m2 strains being vacuolating and vacA s1i2m2 strains being non-vacuolating [12].
Although H. pylori strains with both the cagA gene and vacuolating toxin-producing vacA genotypes are commonly found in patients with gastroduodenal diseases, a significant number of individuals infected with such H. pylori strains remain asymptomatic [14, 15]. Several other H. pylori virulence genes have been studied. Peek, in particular, discovered the iceA gene (induced by contact with epithelium gene A), whose transcription was induced by H. pylori’s adherence to the gastric epithelium. This gene has two major allelic variants, iceA1 and iceA2 [14]. A number of studies have considered the role of the iceA gene in conjunction with the cagA gene and the vacA gene in the pathogenesis of H. pylori [2, 16, 17]. The current study aimed to investigate the prevalence of H. pylori cagA, vacA, and iceA, the genotypes and their association to clinical outcomes in Vietnamese patients.
Materials and methods
Patients
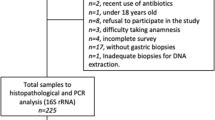
This cross-sectional study was conducted at the University of Medicine and Pharmacy Hospital, Hue University, Vietnam, between June 2019 and February 2022. Patients with dyspepsia symptoms, who underwent esophagogastroduodenoscopies at the Centre of Gastroenterology and Endoscopy and were diagnosed with gastroduodenal diseases, were recruited for the study. At least two gastric mucosa biopsy specimens were obtained from the corpus and antrum to determine H. pylori infection by rapid urease test (RUT). Subsequently, DNA was extracted from these biopsy specimens to confirm the H. pylori positivity and genotyping the H. pylori cagA, vacA, and iceA genes by polymerase chain reaction (PCR) assays. H. pylori infection was diagnosed if both the RUT and PCR (with primers specific for the ureC gene) assays were positive [18]. With respect to patients who had neoplastic suspicious lesions, additional gastric mucosa biopsy specimens were obtained for histopathological examination to confirm gastric cancer. As a result, 141 patients with H. pylori-positive gastroduodenal diseases were recruited for initial study samples. After performing molecular analysis for H. pylori cagA, vacA, and iceA genes, samples with mixed H. pylori strains, positivity or negativity for both cagA and cagPAI empty sites, or unidentified genotypes (for example vacA s? or vacA m?), were excluded. 107 samples were ultimately evaluated regarding their association with clinical outcomes (Fig. 1).
DNA extraction
Gastric mucosa biopsy specimens were kept at -20 °C in tubes containing TE buffer solution at a pH of 7.5 (Promega Corp., Madison, WI, USA) until performing the DNA extraction. Biopsy specimens were ground in 600 μL of Nuclei lysis solution (Promega Corp., Madison, WI, USA) added 17.5 μL of proteinase K, 20 mg/mL (Thermo Scientific, Wilmington, USA), before being extracted using the Wizard® Genomic DNA Purification Kit (Promega Corp., Madison, WI, USA). The DNA concentration was determined using a NanoDrop 2000 UV–Vis spectrophotometer (Thermo Scientific, Wilmington, USA).
Genotyping H. pylori cagA, vacA, and iceA genes
The cagA gene is polymorphic, so the cagA status was identified by two PCR assays, the first using forward primer cag2 and reverse primer CAGTR previously described by Rudi and Yamaoka [19, 20] and the second using primers cag5c-F and cag3c-R developed by Chattopadhyay [21]. Primers cag2 and CAGTR are specific for the region flanking the cagA-EPIYA motif, so the PCR reaction yielded products with different sizes (450–550 bp) depending on the different H. pylori strains. The PCR reaction using primers cag5c-F and cag3c-R yielded products of 350 bp in size. All DNA samples were subjected to PCR assay using primers Luni1 and R5280 specific for the “cagPAI empty site” and yielded a 550-bp product [22]. The samples that were positive with one of two PCR assays (using primers cag2 and CAGTR and/or primers cag5c-F and cag3c-R) and negative with the cagPAI empty site were confirmed as true cagA-positive H. pylori samples, and vice versa. The cagA-EPIYA motif was identified by four single PCR reactions using cag2 forward primer and reverse primers as cagA-P1C, cagA-P2TA, cagAWest, and cagAEast specific for EPIYA-A, -B, -C, and -D, respectively [23, 24]. The EPIYA-A, -B, -C, and -D motifs were identified based on the sizes of specific amplicons, as 172 bp, 216 bp, 402 bp, and 416 bp, respectively.
A multiplex PCR assay was performed for genotyping the vacA sm of the H. pylori strains using the vacA s1/s2 allele-specific primers (VA1-F, VA1-R) and the vacA m1/m2 allele-specific primers (VAG-F, VAG-R) [10, 21, 25]. Samples without amplification with VA1-F and VA1-R primers or VAG-F and VAG-R primers in the multiplex PCR reaction were followed by a simplex PCR assay using the same specific primers. H. pylori vacA sm genotypes were determined based on the sizes of specific amplicons, in particular 259-bp and 286-bp for vacA s1 and s2, respectively, and 567-bp and 642-bp for vacA m1 and m2, respectively.
The genotype of vacA i was determined by two separate PCR assays. The forward primer VacF1 was used in both assays, whereas reverse primers C1-R and C2-R were used for assays identifying vacA i1 and i2, respectively [12]. The amplicon sizes for the i1 and i2 alleles were 426 bp and 432 bp, respectively.
Two separate PCR assays with primers iceA1-F5 and iceA1-R4 and primers iceA2-F6 and iceA2-R5 specific for iceA1 and iceA2 alleles, respectively, were used for genotyping the iceA gene [16]. The iceA1 allele yielded a 247-bp product, whereas the iceA2 allele yielded a 124-bp product corresponding to the absence of the 105-bp sequence encoding 35 amino acids, or yielded 229-bp, 334-bp or 439-bp products depending on whether the presence of the 105-bp sequence was present or repeated twice or three times, respectively. Depending on the number of amino acids (aa) in the encoded sequence, these iceA2 variants are referred to as 24-aa, 59-aa, 94-aa, and 129-aa variants [26].
Each PCR reaction was performed in a total volume of 25 μL, including 12.5 μL GoTaq Green MasterMix 2X (Promega Corp., Madison, WI, USA), 10 pmol each forward and reverse primer, 200 ng of DNA, and nuclease-free water. The positive controls were DNA samples extracted from previous H. pylori isolates which were identified genotypes in our laboratory and the negative control was nuclease-free sterile water. The thermal cycle was as follows: initial denaturation at 95 °C for 5 min; 30 cycles including denaturation at 94 °C for 1 min, annealing at 53 °C for cagA, the cagPAI empty site, and iceA genotyping, at 50 °C for EPIYA motifs, at 52 °C for vacA sm genotyping, at 55 °C for vacA i genotyping, extension at 72 °C for 1 min; and final extension at 72 °C for 10 min. The primer sequences are presented in Table 1. The PCR reactions were performed in the Agilent SureCycler 8800 (Agilent Technologies, Malaysia). The amplification products of cagA, the cagPAI empty site, the EPIYA motifs, vacA i, iceA1, and iceA2 were electrophoresed on 1% agarose gel, whereas the products of vacA sm were electrophoresed on 2% agarose gel (Fig. 2). SafeView (Applied Biological Materials Inc. (abm), Canada) served as DNA staining.
Agarose gel electrophoresis image of the PCR products. Lane M: 100 bp DNA ladder (Promega Corp., Madison, WI, USA). 2A, 2B, and 2C: Amplication products of cagA gene using primers cag5c-F and cag3c-R, primers cag2 and CAGTR, and amplication products using primers Luni1 and R5280 specific for the “cagPAI empty site”, respectively; lanes 1, 2, 4, 6: cagA ( +) and cagPAI empty site (-); lanes 3, 5, 8: cagA (-) and cagPAI empty site ( +); lane 7: cagA ( +) and cagPAI empty site ( +); lane 9: cagA (-) and cagPAI empty site (-). 2D, 2E, 2F, and 2G: Amplication products of EPIYA-A, EPIYA-B, EPIYA-C and EPIYA-D, respectively; lanes 1, 3, 4, 5: EPIYA-ABD subtype; lane 2: EPIYA-ABC subtype. 2H: Amplication products of vacA sm, lanes 1, 7: s1; lanes 2, 5, 6, 13: s1m1; lanes 3, 4, 8–11, 14–16: s1m2; lane 12: s2m2. 2I and 2 J: Amplication products of vacA i1 and i2, respectively; lanes 1–3, 7, 8, 11: i2; lanes 4–6, 12, 13: i1; lanes 14: i1/i2. 2 K and 2L: Amplication products of iceA1 and iceA2, respectively; lane 1: iceA1 ( +) / iceA2 ( +) with 59-aa variant; lane 2: iceA1 (-) / iceA2 ( +) with 94-aa variant; lane 3: iceA1 ( +) / iceA2 ( +) with 24-aa variant; lane 4: iceA1 (-) / iceA2 ( +) with 129-aa variant; lanes 5, 7: iceA1 ( +) / iceA2 (-); lane 6: iceA1 (-) / iceA2 ( +) with 59-aa variant; lane 8: iceA1 ( +) / iceA2 ( +) with 59-aa and 94-aa variants; lane 9: iceA1 (-) / iceA2 (-)
Statistical analysis
The IBM SPSS Statistics Version 20 software was used to analyze the data. The chi-square test or Fisher’s exact test (if more than 20% of expected frequencies were smaller than 5) was used to assess the linkage of genotypes, as well as the differences in distribution of genotypes between clinical outcomes. After adjusting for age (less than 40 years old; equal to or more than 40 years old) and gender (male; female), a multivariable logistic regression analysis was performed in order to assess the associations between genotypes and clinical outcomes. The adjusted odds ratio (aOR) and 95% confidence interval (CI) were estimated to identify the strength of the associations. P-values less than 0.05 were considered statistically significant.
Results
General characteristics of the study population
This study included 107 patients with H. pylori-positive gastroduodenal diseases. Gastritis comprised 57% (n = 61) of these cases, gastric ulcer (GU) 15% (n = 16), duodenal ulcer (DU) 14% (n = 15), and GC 14% (n = 15) of the total cases. In terms of gender, 47.7% were males and 52.5% were females. The mean age was 47.0 ± 17.2 years, with 36 patients being younger than 40 years old (see Table 2).
The present investigation comprised a sample of 107 patients who were diagnosed with gastroduodenal diseases positive for H. pylori. Gastritis comprised 57% (n = 61) of these cases, gastric ulcer (GU) 15% (n = 16), duodenal ulcer (DU) 14% (n = 15), and GC 14% (n = 15) of the total cases.
H. pylori cagA, vacA, and iceA genotypes
The overall distribution of the cagA, vacA, and iceA genotypes among the H. pylori strains is presented in Table 3. The presence of the cagA, vacA, and iceA genes were detected in 77.6%, 100% and 80.4% of the cases, respectively. The majority of cagA-positive H. pylori strains carried the EPIYA-ABD motif, while only four strains exhibited the EPIYA-ABC motif.
Regarding the vacA genotypes, the s1i1m1 and s1i1m2 were most frequent, accounting for 44.9% and 33.6%, respectively. The s1i2m2 genotype was found as 19.6%, while the s2i2m2 genotype was very rare (1.9%). The vacA s1 was found to be predominant compared to the vacA s2, in 105 cases (98.1%) compared to two cases (1.9%). Similarly, the vacA i1 was more prevalent than the vacA i2, in 84 cases (78.5%) compared to 23 cases (21.5%). Moreover, the vacA m1 and m2 accounted for 44.9% and 55.1%, respectively (p = 0.332).
With respect to the iceA gene, the iceA1 and iceA2 accounted for 48.6% and 31.8%, respectively, while 19.6% of samples were negative for the iceA gene. Among the iceA2-positive H. pylori strains, the 59-aa variant was the most prevalent (70.6%), whereas the 129-aa variant was very rare (2.9%). The 24-aa and 94-aa variants were found in 14.7% and 11.8% of cases, respectively.
Our findings revealed that most cagA-positive H. pylori strains have vacA s1i1m1 and s1i1m2 genotypes, as well as iceA1 or iceA2 alleles, whereas most cagA-negative H. pylori strains have vacA s1i2m2 and s2i2m2 genotypes, with iceA negativity. H. pylori strains with vacA s1i1m1 genotypes are also more likely to have iceA1 or iceA2 alleles, whereas vacA s1i2m2 genotypes are more likely to have iceA negativity (Fig. 3). The combinations of more virulent variants, such as cagA( +)/vacAs1i1m1/iceA1 and cagA( +)/vacAs1i1m2/iceA1, were found to be prevalent, at 26.2% and 25.1%, respectively. In addition, cagA( +)/vacAs1i1m1/iceA2 accounted for 17.8%. The combinations of less virulent variants, such as cagA(-)/vacAs1i2m2/iceA(-), was also found to have remarkable prevalence, namely 15.9% (Table 3).
The relationship of cagA, vacA, and iceA genotypes among 107 Helicobacter pylori strains without mixed or non-identified genotypes. The numbers on the graph are absolute values for H. pylori strain amounts. Statistical analysis revealed a significant association between cagA, vacA, and iceA genotypes, with p-values lower than 0.0001
Associations of cagA, vacA, and iceA genotypes with clinical outcomes
Overall, there was no statistically significant difference in the rate of cagA-positive H. pylori between the groups of gastroduodenal diseases (gastritis, GU, DU, and GC). In terms of the iceA genotype, neither the prevalence of iceA1 nor of iceA2 differed among the groups of gastroduodenal diseases. A statistically significant difference in vacA genotypes was found; specifically, vacA s1i1m1 (62.5%) was predominant in GU (p = 0.037) and vacA s1i1m2 (86.7%) was frequent in GC (p < 0.001). Regarding the combination of cagA, vacA, and iceA genotypes, we found a statistically significant difference in the rate of cagA( +)/vacAs1i1m2/iceA1 among the groups of gastritis, GU, DU, and GC; in particular, this combination was the most prevalent in GC patients, at 66.7%, p < 0.001 (Table 4).
However, a multivariable logistic regression analysis, after adjusting for age and gender, with the gastritis group used as a control group, found statistically significant associations between the vacA s1i1m2 genotype, the iceA1 variant, and the cagA( +)/vacAs1i1m2/iceA1 combination and GC. The adjusted ORs were estimated as 18.02 (95% CI: 3.39–95.81), 4.09 (95% CI: 1.11–15.08), and 16.19 (95% CI: 3.42–76.66), respectively (Table 5).
Discussion
The cagA, vacA, and iceA genotypes are essential for H. pylori toxicity. However, the role of these genes in the pathogenesis of gastroduodenal disease is controversial. The main causes are the geographical differences in the prevalence of H. pylori virulence genes and genotypes, as well as the synergic interaction between these genes.
In this study, we performed DNA extraction from gastric mucosa biopsy specimens in order to investigate H. pylori virulence genes. This approach avoided the bacteria culture process, which requires time and labor. We cleared our samples prior to analysis by discharging samples with mixed H. pylori strains, cases of positivity or negativity for both the cagA and cagPAI empty sites, or unidentified genotypes (in this study, only six samples had unidentified genotypes for vacA m). This mixture of multiple H. pylori strains had been observed in previous studies analyzing gastric mucosa biopsy specimens [21, 27], and even in culture isolates [22].
Prevalence of cagA-positive H. pylori strains
East Asian H. pylori strains were found to have a higher cagA gene prevalence (90–95%) than strains from other regions [7]. However, in the current study, this prevalence was only 77.6%. Our results were consistent with those of previous research studies conducted in Vietnam, such as Phan’s study, which was conducted in Hue city between 2012 and 2014, and found a cagA-positive H. pylori prevalence of 84% (n = 88) [28]; and Nguyen’s study, which was conducted in Ho Chi Minh city between 2016 and 2017, and found a cagA-positive H. pylori prevalence of 79.5% (n = 83) [29]. By contrast, the cagA prevalence was much higher in other regions of Vietnam, such as 99% (n = 96) in Daklak, 100% (n = 75) in Lao Cai [30], and 96.2% (n = 53) in Hanoi [31]. Regarding the EPIYA motif of cagA-positive H. pylori, our findings revealed that only four strains carried the EPIYA-ABC motif, with no EPIYA-C repetitions. This showed that patients in our region, a city in central Vietnam, were infrequently infected by Western-type H. pylori strains.
Although we discharged the samples that were positive with both PCR assays specific for the cagA gene and the cagPAI empty site, as well as ones that were negative with both these PCR assays, this issue should be discussed, because it reveals specific genetic diversity with regard to the cagA gene and the cagPAI in Vietnamese H. pylori strains. The cagA gene is thought to be an indicator of the presence of cagPAI and the ability to produce the CagA protein; some studies have revealed a partial deletion of this island with a low prevalence of 5–10% [32]. In studies by Censini et al. and Maeda et al., the cagA gene was found in all H. pylori strains from Western countries and Japan that had a partial deletion of cagPAI [32, 33]. On the other hand, Nguyen demonstrated that 6 of the 12 Vietnamese H. pylori strains with partial deletion of cagPAI had a deleted part that included the cagA gene [34]. As a result, these strains are negative for both cagA and cagPAI empty site PCR assays. In the current study, 4 of 141 initial samples were negative for both the cagA gene and the cagPAI empty site. It is possible that H. pylori strains with partial deletion of cagPAI were present in our samples. Furthermore, the cagA point mutation could be a contributing factor to this situation [28]. The percentage of samples that were found to be negative for both cagA and cagPAI empty site PCR assays was very low at only 2.8% (4/141), so it did not significantly affect the prevalence of cagA-positive H. pylori in this study.
H. pylori vacA genotypes
The vacA gene, which encodes the VacA protein, a vacuolating cytotoxin, was detected in all H. pylori strains. This is a highly polymorphic gene that exhibits alternating activity depending on the genotype. Three specific regions of VacA that were extensively studied were the s- and i-regions on the p33 domain, as well as the m region on the p55 domain [35]. A 12-amino-acid segment found in VacA s2 but not in VacA s1 prevents vacuolating activity of the VacA s2 subtype, whereas the VacA s1 subtype exhibits this activity [35, 36]. It is known that the m region has cell-type specificity and plays a role in binding to epithelial cells [37,38,39]. Rhead et al. reported the i region for the first time in 2007, with two variants, i1 and i2, with the i1 form being more toxic than the i2 [12].
To identify the vacA s, m, and i genotypes, we performed multiplex and simplex PCR assays. All samples in the current study possessed the vacA gene. Our observations reveal that the vacA s1 subtype predominated. Previous research has found an extremely high prevalence of the vacA s1 genotype, at approximately 98–100%, in H. pylori strains infected Vietnamese patients with gastroduodenal diseases [2, 28,29,30]. By comparison, Hispanics, people of African origin, and others have a prevalence of only 65%, 80%, and 93%, respectively [2].
With respect to the vacA i genotype, the prevalence of vacA i1 in the current study was also high (78.5%); it was however lower than the prevalence of 91% found by the study of Phan et al. in Vietnam [28]. In contrast to the vacA s and i genotypes, the vacA m genotype was fairly evenly distributed in the m1 and m2 subtypes, p = 0.332. This distribution is consistent with previous findings in the Vietnamese population [28, 29]. However, a study on minor ethnic groups in Vietnam found a discrepancy, with m1 prevalence (65.5%) higher than that of m2 (33.3%) [30]. Regarding the combination of the vacA s, m, and i variants, our results reveal a predominance of the s1i1m1 and s1i1m2 genotypes, which could be due to selected advantage of higher toxicity. To date, there has been relatively little research on this intermediate region of H. pylori strains in Vietnam. Even recent studies published in 2018 and 2021 [29, 30] only investigated the vacA s and m genotypes in H. pylori strains in infected patients in Vietnam. Therefore, our findings on the vacA s, i, and m genotypes may contribute to elucidating the genetic diversity of H. pylori among the Vietnamese population.
H. pylori iceA1 and iceA2 alleles
The iceA gene, which has two alleles known as iceA1 and iceA2, was first identified by Peek et al. in 1998. The iceA transcription is induced by adherence to gastric epithelial cells, so IceA may contribute to the development of gastrointestinal pathogenesis within infected patients [14, 40]. Numerous studies on the prevalence of and association between iceA1 and iceA2 variants and clinical outcomes have been conducted. The iceA1 allelic variant is more prevalent in Asian countries, while the iceA2 allelic variant is more prevalent in Western countries [41].
The current study found that the prevalence of iceA-positive H. pylori is 80.4%, with iceA1 predominating over iceA2 in clinical H. pylori strains. Another study among the Vietnamese population has revealed similar results, with iceA1 and iceA2 indicating prevalence of 50% and 44%, respectively [31]. In Vietnam, the iceA gene of H. pylori has rarely been studied. The present study is the first to investigate the iceA2 subtypes. We found four iceA2 subtypes, namely the 24-aa, 59-aa, 94-aa, and 129-aa variants, with the 59-aa variant the most prevalent (70.6%). Most studies on the iceA gene have revealed two iceA2 variants, 59-aa and 94-aa, with the 59-aa variant being predominant [2, 41]. The 24-aa variant has rarely been reported worldwide. It was found in only two out of 424 samples in a study by Yamaoka et al. [2], and in 5.8% of a study by Figueiredo et al. [26]. The current study highlights the higher prevalence (14.7%) of the 24-aa variant. The existence of the four variants demonstrates the genotypic diversity of iceA2 among the Vietnamese population.
Combination of cagA, vacA, and iceA genotypes
Several studies have demonstrated the interaction of CagA and VacA. This property enables H. pylori to survive and cause damage to gastric epithelial cells without killing them [42, 43]. The combination of more virulent genetic variants of H. pylori, such as the cagA( +)/vacAs1/iceA1 genotype, was demonstrated by van Doorn in H. pylori strains in the Netherlands [16], by Yamaoka in H. pylori strains in Japan and Korea [2], and by Fan in H. pylori strains in China [44]. The current study highlights that highly toxic genotypes tend to mix together in H. pylori genomes, with the cagA( +)/vacAs1i1m1/iceA1 and cagA( +)/vacAs1i1m2/iceA1 combinations being the predominant genotype. These combinations explain the ability of H. pylori strains to cause damage to gastric mucosa.
Associations of cagA, vacA, and iceA genotypes with clinical outcomes
In this study, we found no association between cagA status and gastroduodenal diseases. This is consistent with previous research on East Asian H. pylori strains, where cagA prevalence was high regardless of clinical outcomes [2, 9]. As previously stated, the vacA gene is present in all H. pylori strains and the vacA s-, i-, and m-region variants play different roles in the pathogenesis. Our study is one of only a few that looked at all three vacA regions of Vietnamese H. pylori strains. We discovered that the vacA s1i1m2 genotype, but not the vacA s1i1m1 genotype, is identified as a risk factor for GC when compared to a gastritis group as a control group. This is in contrast to several other studies that found the s1i1m1 to be a risk factor for GC [45, 46]. To the best of our knowledge, only one other study found s1cm2 to predominate in GC [47]. The s- and i-regions of VacA are required for vacuolating activity, whereas the m-region is cell-type specific [12]. According to Pagliaccia’s research, the m2 variant is not toxic to HeLa cells, but it did exhibit vacuolating activity in cultured gastric cells [38]. This is consistent with the observation of a higher prevalence of the m2 variant in cohorts with a high prevalence of GC, such as in our country and reported in the study by Wei et al. in China [47]. Furthermore, a study by González-Rivera et al. demonstrated that the i-region variants altered the ability of the vacA s1m2 subtype to vacuolate: the s1i1m2 subtype but not the s1i2m2 induced vacuolating activity [48]. Several studies have demonstrated a significant correlation between s1i1 and GC [49, 50]. Taken together, the above studies support our findings that the vacA s1i1m2 can be a risk factor for GC.
Since its discovery in 1998, the iceA1 variant has been found to have a statistically significant high prevalence among patients with peptic ulcer disease (PUD) [14, 16]. Huang’s meta-analysis of 22 studies indicated that infection with iceA1-positive H. pylori strains is a risk factor for PUD [51]. However, our study does not confirm this association. By contrast, we found iceA1 allele increases the risk of GC but not of GU or DU. Various other studies have indicated an association between iceA1 and GC in both Asian and Western populations [47, 49, 52, 53]. The current study found no association between iceA2 and gastroduodenal diseases. Although both iceA1 and iceA2 alleles are expressed in gastric cells, iceA1 expression induced inflammation via an increase in interleukin 8 [14, 16]. This clarifies the role of the iceA1 allele in the pathogenesis of H. pylori. Although cagA ( +) was not found to be a risk factor for GC in this study, the cagA( +)/vacA s1i1m2/iceA1 combination was. This is consistent with the pathogenesis of H. pylori-induced gastroduodenal diseases, in which the interaction of several virulent genes plays an important role.
In conclusion, this study demonstrates the genetic diversity of the H. pylori cagA, vacA and iceA genes and contributes to elucidating the important roles of these genotypes for clinical outcomes. The vacA s1i1m2 and iceA1 genotypes and the cagA( +)/vacAs1i1m2/iceA1 combination are risk factors for GC. Our findings also reveal that Vietnamese H. pylori strains exhibit geographical differences.
Data Availability
The data that support the findings of this study are available from the corresponding author, TMTH, upon reasonable request.
References
IARC Helicobacter pylori Working Group (2014) Helicobacter pylori eradication as a strategy for preventing gastric cancer. Lyon, France: International Agency for Research on Cancer (IARC Working Group Reports, No 8).
Yamaoka Y, Kodama T, Gutierrez O, Kim JG, Kashima K, Graham DY (1999) Relationship between Helicobacter priori iceA, cagA, and vacA status and clinical outcome: Studies in four different countries. J Clin Microbiol 37(7):2274–2279
Imoto I, Oka S, Katsurahara M, Nakamura M, Yasuma T, Akada J, D’Alessandro-Gabazza CN, Toda M, Horiki N, Gabazza EC, Yamaoka Y (2022) Helicobacter pylori infection: is there circulating vacuolating cytotoxin A or cytotoxin-associated gene A protein? Gut Pathog 14:43
Jones KR, Whitmire JM, Merrell DS (2010) A tale of two toxins: Helicobacter pylori CagA and VacA modulate host pathways that impact disease. Front Microbiol 1:115
Hatakeyama M (2014) Helicobacter pylori CagA and gastric cancer: A paradigm for hit-and-run carcinogenesis. Cell Host Microbe 15(3):306–316
Hatakeyama M (2006) Helicobacter pylori CagA-a bacterial intruder conspiring gastric carcinogenesis. Int J Cancer 119:1217–1223
Yamaoka Y (2010) Mechanisms of disease: Helicobacter pylori virulence factors. Nat Rev Gastroenterol Hepatol 7(11):629–641. https://doi.org/10.1038/nrgastro.2010.154
Zhu X, Zhao Y, Zhu C, Wang Y, Liu Y, Su J (2022) Rapid detection of cagA-positive Helicobacter pylori based on duplex recombinase aided amplification combined with lateral flow dipstick assay. Diagn Microbiol Infect Dis 103(1):115661
Maeda S, Yoshida H, Kanai F, Ikenoue T, Kato N, Shiratori Y, Omata M (1998) Major virulence factors, VacA and CagA, are commonly positive in Helicobacter pylori isolates in Japan. Gut 42:338–343
Atherton JC, Cao P, Peek RM, Tummuru MKR, Blaser MJ, Cover TL (1995) Mosaicism in vacuolating cytotoxin alleles of Helicobacter pylori. J Biol Chem 270(30):17771–17777
Xue Z, Yang H, Su D, Song X, Deng X, Yu C, Sun C, He L, You Y, Gong Y, Fan D, Sun L, Han X, Fan R, Zhang M, Yan X, Qian J, Zhang J (2021) Geographic distribution of the cagA, vacA, iceA, oipA and dupA genes of Helicobacter pylori strains isolated in China. Gut Pathog 13:39
Rhead JL, Letley DP, Mohammadi M, Hussein N, Mohagheghi MA, Eshagh Hosseini M, Atherton JC (2007) A New Helicobacter pylori vacuolating cytotoxin determinant, the intermediate region, is associated with gastric cancer. Gastroenterology 133(3):926–936
Ferreira RM, Machado JC, Letley D, Atherton JC, Pardo ML, Gonzalez CA, Carneiro F, Figueiredo C (2012) A novel method for genotyping the Helicobacter pylori vacA intermediate region directly in gastric biopsy specimens. J Clin Microbiol 50(12):3983–3989
Peek J, Thompson SA, Donahue JP, Tham KT, Atherton JC, Blaser MJ, Miller GG (1998) Adherence to gastric epithelial cells induces expression of a Helicobacter pylori gene, iceA, that is associated with clinical outcome. Proc Assoc Am Physicians 110(6):531–544
Malfertheiner P, Camargo MC, El-Omar E, Liou JM, Peek R, Schulz C, Smith SI, Suerbaum S (2023) Helicobacter pylori infection. Nat Rev Dis Primers 9:19
van Doorn LJV, Figueiredo C, Sanna R, Plaisier A, Schneeberger P, De Boer W, Quint W (1998) Clinical relevance of the cagA, vacA, and iceA status of Helicobacter pylori. Gastroenterology 115(1):58–66
Feliciano O, Gutierrez O, Valdés L, Fragoso T, Calderin AM, Valdes AE, Llanes R (2015) Prevalence of Helicobacter pylori vacA, cagA, and iceA genotypes in Cuban patients with upper gastrointestinal diseases. Biomed Res Int Vol 2015. https://doi.org/10.1155/2015/753710
Bickley J, Owen RJ, Fraser AG, Pounder RE (1993) Evaluation of the polymerase chain reaction for detecting the urease C gene of Helicobacter pylori in gastric biopsy samples and dental plaque. J Med Microbiol 39(5):338–344
Rudi J, Kolb C, Maiwald M, Kuck D, Sieg A, Galle PR, Stremmel W (1998) Diversity of Helicobacter pylori vacA and cagA genes and relationship to VacA and CagA protein expression, cytotoxin production, and associated diseases. J Clin Microbiol 36(4):944–948
Yamaoka Y, Malaty HM, Michael SO, Graham DY (2000) Conservation of Helicobacter pylori genotypes in different ethnic groups in Houston, Texas. J Infect Dis 181:2083–2086
Chattopadhyay S, Patra R, Ramamurthy T, Chowdhury A, Santra A, Dhali GK, Bhattacharya SK, Berg DE, Nair GB, Mukhopadhyay AK (2004) Multiplex PCR assay for rapid detection and genotyping of Helicobacter pylori directly from biopsy specimens. J Clin Microbiol 42(6):2821–2824
Mukhopadhyay AK, Kersulyte D, Jeong JY, Datta S, Ito Y, Chowdhury A, Chowdhury S, Santra A, Bhattacharya SK, Azuma T, Nair GB, Berg DE (2000) Distinctiveness of genotypes of Helicobacter pylori in Calcutta, India. J Bacteriol 182(11):3219–3227
Argent RH, Zhang Y, Atherton JC (2005) Simple method for determination of the number of Helicobacter pylori CagA variable-region EPIYA tyrosine phosphorylation motifs by PCR. J Clin Microbiol 43(2):791–795
Schmidt HMA, Goh KL, Ming Fock K, Hilmi I, Dhamodaran S, Forman D, Mitchell H (2009) Distinct cagA EPIYA Motifs are associated with ethnic diversity in malaysia and singapore. Helicobacter 14:256–263
Atherton JC, Cover TL, Twells RJ, Morales MR, Hawkey CJ, Blaser MJ (1999) Simple and accurate PCR-based system for typing vacuolating cytotoxin alleles of Helicobacter pylori. J Clin Microbiol 37(9):2979–2982
Figueiredo C, Quint WGV, Sanna R, Sablon E, Donahue JP, Xu Q, Miller GG, Peek RM, Blaser MJ, van Doorn LJ (2000) Genetic organization and heterogeneity of the iceA locus of Helicobacter pylori. Gene 246(1–2):59–68
Akeel M, Shehata A, Elhafey A, Elmakki E, Aboshouk T, Ageely H, Mahfouz M (2019) Helicobacter pylori vacA, cagA and iceA genotypes in dyspeptic patients from Southwestern region, Saudi Arabia: Distribution and association with clinical outcomes and histopathological changes. BMC Gastroenterol 19(1):16
Phan TN, Santona A, Tran VH, Tran TNH, Le VA, Cappuccinelli P, Rubino S, Paglietti B (2017) Genotyping of Helicobacter pylori shows high diversity of strains circulating in central Vietnam. Infect Genet Evol 52:19–25
Nguyen TH, Ho TTM, Nguyen-Hoang TP, Qumar S, Pham TTD, Bui QN, Bulach D, Nguyen TV, Rahman M (2021) The endemic Helicobacter pylori population in Southern Vietnam has both South East Asian and European origins. Gut Pathog 13:57. https://doi.org/10.1186/s13099-021-00452-2
Binh TT, Tuan VP, Dung HDQ, Tung PH, Tri TD, Thuan NPM, Tam LQ, Nam BC, Giang DA, Hoan PQ, Uchida T, Trang TTH, Van Khien V, Yamaoka Y (2018) Molecular epidemiology of Helicobacter pylori infection in a minor ethnic group of Vietnam: A multiethnic, population-based study. Int J Mol Sci 19(3):708
Nguyen TL, Uchida T, Tsukamoto Y, Trinh DT, Ta L, Mai BH, Le SH, Thai KD, Ho DD, Hoang HH, Matsuhisa T, Okimoto T, Kodama M, Murakami K, Fujioka T, Yamaoka Y, Moriyama M (2010) Helicobacter pylori infection and gastroduodenal diseases in Vietnam: a cross-sectional, hospital-based study. BMC Gastroenterol 10:114
Maeda S, Yoshida H, Ikenoue T, Ogura K, Kato N, Shiratori Y, Omata M (1999) Structure of cag pathogenicity island in Japanese Helicobacter pylori isolates. Gut 44:336–341
Censini S, Lange C, Xiang Z, Crabtree JE, Ghiara P, Borodovsky M, Rappuoli R, Covacci A (1996) cag, a pathogenicity island of Helicobacter pylori, encodes type I-specific and disease-associated virulence factors. Proc Natl Acad Sci USA 93:14648–14653
Nguyen LT, Uchida T, Tsukamoto Y, Trinh TD, Ta L, Mai HB, Le HS, Ho DQD, Hoang HH, Matsuhisa T, Okimoto T, Kodama M, Murakami K, Fujioka T, Yamaoka Y, Moriyama M (2010) Clinical relevance of cagPAI intactness in Helicobacter pylori isolates from Vietnam. Eur J Clin Microbiol Infect Dis 29(6):651–660
McClain MS, Beckett AC, Cover TL (2017) Helicobacter pylori vacuolating toxin and gastric cancer. Toxins 9(10):316
Letley DP, Atherton JC (2000) Natural diversity in the N terminus of the mature vacuolating cytotoxin of Helicobacter pylori determines cytotoxin activity. J Bacteriol 182(11):3278–3280
Caston RR, Sierra JC, Foegeding NJ, Truelock MD, Campbell AM, Frick-Cheng AE, Bimczok D, Wilson KT, McClain MS, Cover TL (2020) Functional properties of Helicobacter pylori vacA toxin m1 and m2 variants. Infect Immun 88(6):e00032-e120
Pagliaccia C, De Bernard M, Lupetti P, Ji X, Burroni D, Cover TL, Papini E, Rappuoli R, Telford JL, Reyrat JM (1998) The m2 form of the Helicobacter pylori cytotoxin has cell type-specific vacuolating activity (mosaic structure). Proc Natl Acad Sci USA 95:10212–10217
Ji X, Fernandez T, Burroni D, Pagliaccia C, Atherton JC, Reyrat JM, Rappuoli R, Telford JL (2000) Cell Specificity of Helicobacter pylori cytotoxin is determined by a short region in the polymorphic midregion. Infect Immun 68(6):3754–3757
Baj J, Forma A, Sitarz M, Portincasa P, Garruti G, Krasowska D, Maciejewski R (2021) Helicobacter pylori virulence factors—mechanisms of bacterial pathogenicity in the gastric microenvironment. Cells 10:27
Shiota S, Watada M, Matsunari O, Iwatani S, Suzuki R, Yamaoka Y (2012) Helicobacter pylori iceA, clinical outcomes, and correlation with cagA: a meta-analysis. PLoS One 7(1):e30354
Argent RH, Thomas RJ, Letley DP, Rittig MG, Hardie KR, Atherton JC (2008) Functional association between the Helicobacter pylori virulence factors VacA and CagA. J Med Microbiol 57(2):145–150
Abdullah M, Greenfield LK, Bronte-Tinkew D, Capurro MI, Rizzuti D, Jones NL (2019) VacA promotes CagA accumulation in gastric epithelial cells during Helicobacter pylori infection. Sci Rep 9(1):1–9
Fan L, Lia R, Li H, Zhang J, Wang L (2018) Detection of CagA, VacA, IceA1 and IceA2 virulent genes in Helicobacter pylori isolated from gastric ulcer patients. J Lab Med 42(4):155–162
Kim JY, Kim N, Nam RH, Suh JH, Chang H, Lee JW, Kim YS, Kim JM, Choi JW, Park JG, Lee YS, Lee DH, Jung HC (2014) Association of polymorphisms in virulence factor of Helicobacter pylori and gastroduodenal diseases in South Korea. J Gastroenterol Hepatol 29(5):984–991
El-Khadir M, Alaoui Boukhris S, Benajah DA, El Rhazi K, Adil Ibrahimi S, El Abkari M, Harmouch T, Nejjari C, Mahmoud M, Benlemlih M, Bennani B (2017) VacA and CagA status as biomarker of two opposite end outcomes of Helicobacter pylori infection (gastric cancer and duodenal ulcer) in a Moroccan population. PLoS One 12(1):1–14
Wei GC, Chen J, Liu AY, Zhang M, Liu XJ, Liu D, Xu J, Liu BR, Ling H, Wu HX, Du YJ (2012) Prevalence of Helicobacter pylori vacA, cagA and iceA genotypes and correlation with clinical outcome. Exp Ther Med 4(6):1039–1044
González-Rivera C, Algood HMS, Radin JN, McClain MS, Cover TL (2012) The intermediate region of Helicobacter pylori VacA is a determinant of toxin potency in a Jurkat T cell assay. Infect Immun 80(8):2578–2588
Kaneko K, Zaitoun AM, Letley DP, Rhead JL, Torres J, Spendlove I, Atherton JC, Robinson K (2022) The active form of Helicobacter pylori vacuolating cytotoxin induces decay-accelerating factor CD55 in association with intestinal metaplasia in the human gastric mucosa. J Pathol 258(2):199–209
Djekic A, Müller A (2016) Review the immunomodulator vaca promotes immune tolerance and persistent Helicobacter pylori infection through its activities on T-cells and antigen-presenting cells. Toxins 8:187
Huang X, Deng Z, Zhang Q, Li W, Wang B, Li M (2016) Relationship between the iceA gene of Helicobacter pylori and clinical outcomes. Ther Clin Risk Manag 12:1085–1092
Aghdam SM, Sardari Z, Safaralizadeh R, Bonyadi M, Abdolmohammadi R, Moghadam MS, Khalilnezhad A (2014) Investigation of association between oipA and iceA1/iceA2 genotypes of Helicobacter pylori and gastric cancer in Iran. Asian Pac J Cancer Prev 15(19):8295–8299
Koehler CI, Mues MB, Dienes HP, Kriegsmann J, Schirmacher P, Odenthal M (2003) Helicobacter pylori genotyping in gastric adenocarcinoma and MALT lymphoma by multiplex PCR analyses of paraffin wax embedded tissues. Mol Pathol 56(1):36–42
Acknowledgements
We gratefully acknowledge the Centre of Gastroenterology and Endoscopy, University of Medicine and Pharmacy Hospital, Hue University for their assistance in collecting samples. We are grateful to the Department of Medical Genetics at University of Medicine and Pharmacy, Hue University, Vietnam for their assistance with molecular biology analysis.
Funding
This work was supported by scientific grants from the University of Medicine and Pharmacy, Hue University (37BV/20).
Author information
Authors and Affiliations
Contributions
Conceptualization: Thi Minh Thi Ha, Van Huy Tran; Methodology: Thi Minh Thi Ha, Van Huy Tran; Formal analysis and investigation: Thi Minh Thi Ha, Thi Mai Ngan Nguyen, Van Huy Tran; Writing—original draft preparation: Thi Minh Thi Ha, Thi Mai Ngan Nguyen; Writing—review and editing: Thi Minh Thi Ha, Van Huy Tran.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethics Committee of the University of Medicine and Pharmacy, Hue University Vietnam (H2020-108). Each patient provided written informed consent.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Responsible Editor: Roxane M Piazza
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nguyen, T.M.N., Tran, V.H. & Ha, T.M.T. Helicobacter pylori cagA, vacA, and iceA genotypes and clinical outcomes: a cross-sectional study in central Vietnam. Braz J Microbiol 55, 1393–1404 (2024). https://doi.org/10.1007/s42770-024-01328-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-024-01328-8