Abstract
Introduction
Hepatitis B vaccination of newborns (HBV) and surveillance of pregnant women during antenatal care are complementary to prevent mother to child transmission (MTCT) of HBV infection.
Aim
The aim was to identify the prevalence and pattern of HBV infection in pregnant women born before and after implementing HBV vaccination of newborn in Egypt.
Methods
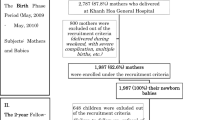
The study included 600 women attended antenatal clinic of the Suez Canal University Hospital, Ismailia, Egypt. All were inquired about risk factors of HBV infection, vaccination, and screened for hepatitis markers. HBsAg carriers were tested for HBeAg, HBeAb, ALT, and HBV DNA. Participants were divided into group 1 of 285 (47.5%) vaccinated women ≤ 25 years, and 315 (52.5%) non-vaccinated > 25 years.
Results
The prevalence of HBcAg, HBsAg, and HBsAb were 18.3%, 5.0%, and 30.7%. Of the 110 women exposed to infection, 40 (36.4%) cleared infection, 30 (27.2%) were HBsAg carriers, and 40 (36.4%) showed isolated HBcAb. HBsAg carriers were HBeAg negative, HBeAb positive, and HBV-DNA positive and had high ALT. Group 1 had significantly higher frequency of vaccination-related immunity, lower frequency of isolated HBcAb, and susceptibles than group 2 (44.9%, 3.5%, and 38.6% vs. 4.1%, 9.5%, and 75.9% ). The prevalence of HBV exposure and chronic HBsAb carriers in both groups were close (4.9% and 16.5% for group 1 vs. 5.1% and 20% for group 2, p > 0.05).
Conclusion
Although the outcomes of HBV infection were favorable in vaccinated group, chronic HBV represents a potential risk for MTCT that necessitates screening during pregnancy in all public health care settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV) infection is a common and potentially life-threatening infection. Following acute hepatitis, resolution of infection occurs in the majority of patients. However, in 5% of adults and up to 90% of infections occurring during the first year of life, HBV can cause chronic hepatitis and put people at high risk of death from cirrhosis and liver cancer. Worldwide, an estimated 257 million people are living with HBV infection. Nearly one quarter of infected people suffer serious complications resulting in about one million deaths every year [1, 2].
Endemicity of HBV infection differs from country to another according to the prevalence of HBsAg; from low (< 2%), to intermediate (2– < 8%), and high (> 8%). Overall, Egypt was considered as a country of intermediate endemicity, the prevalence ranged between 3 and 11%, being more in Upper Egypt and among men [3]. In endemic areas, infantile infection with HBV occurs mainly vertically through mother to child transmission (MTCT) at time of parturition [4, 5].
Immunization of newborns with hepatitis B vaccine aims to prevent future infection leading to chronic liver disease and cancer liver. The World Health Organization (WHO) recommends a birth dose given within 12–24 h as an important post-exposure prophylaxis for infants born of HBV-infected mothers. However, many low- and middle-income countries adopted different timing and included hepatitis B vaccine with other immunizations starting at 6 to 8 weeks after birth for more compliance [6]. Therefore, in such countries, children who are given the full doses of vaccination may experience no or incomplete protection during the first few months after birth [7].
In Egypt, the universal program of infant vaccination against hepatitis B has been implemented late in 1992. Till recently, the three doses were given at 2, 4, and 6 months after birth with other obligatory vaccines [8, 9]. The impact of hepatitis B vaccination on lowering the overall prevalence of HBsAg has been studied and appreciated worldwide. In Egypt, the overall prevalence of HBsAg among blood donors in Egypt was 1.58 [10, 11]. In a national-wide study, the prevalence was 1.4%, among 26047 tested individuals aged 1–59 years. The prevalence was significantly higher in males (1.9%) compared to females (1.1%) [12].
Similarly, among pregnant women, the prevalence shows progressive decline over the last two decades. In Assiut, the prevalence decreased from 14.7% in 1993 to 6.4% in 2010 [13, 14]. In Nile Delta, more recently, lower prevalences were reported, being 2.3% during 2014 in Menofia and 1.56% during 2017 in Benha [15, 16]. In Cairo University Hospitals, the prevalence fluctuated from 1.6% in 2013 to 1.2% in 2014 [17, 18].
Despite this progress, the risk of MTCT is high and could be significantly reduced if routine screening for hepatitis viruses is implemented before marriage and during antenatal care and provision of post-exposure prophylaxis immediately after birth [19]. Recent studies, from Egypt, focused on epidemiology and risk factors of HBV infection among cohorts of pregnant women born before implementation of the infantile vaccination. Worldwide, the majority of people living with HBV infection are unaware of their status. Therefore, infected mothers are a risk of transmitting the virus to their offspring if no post-exposure prophylactic immunization measures are taken within 12 to 24 h after birth [20]. Meanwhile, in women who are HBsAg-positive and HBeAg-positive, infection transmission occurs in an average of 10% of infants taking the post-exposure prophylaxis at the proper time [21].
In Egypt, vaccination failure among vaccinated children of infected mothers has been reported; all missed the birth dose of hepatitis B vaccine [5]. In Egypt, according to the latest census declared in Sep 2017, about 46% of the population aged less than 25 years and born after implementation of hepatitis B vaccination in 1992. This demographic change would enable studying the effectiveness of hepatitis B vaccination and its impact on exposure to infection [22]. Accordingly, this study aimed to identify Hepatitis B virus infection status and immunogenicity of the vaccine among pregnant women born after implementation of the vaccine.
Subjects and methods
This cross-sectional study was carried out at the in Suez Canal University Teaching Hospital Ismailia, Egypt. The study included 600 pregnant women, aging 18 to 45 years and attending the outpatient clinic for antenatal care from January 2018 to January 2019. All were selected by convenience sampling after approval and signing an informed consent. Participants responded to a short questionnaire including sociodemographic data as well risk factors for HBV infection. Only women born before 1992 were inquired about history of hepatitis B vaccination.
Participants were further divided into two groups, group 1 (≤ 25 years, who were presumed to receive HBV vaccination early during infancy) and group 2 (> 25 years, born before the universal vaccination program). Women in group 1 received doses of the vaccine at 2, 4, and 6 months after birth.
Screening of HBV infection
All pregnant women were screened for HBV infection by testing for HBsAg using ELISA (Murex HBsAg Version 3, Diasorin, Italy). Anti-HBc and quantitative detection of anti-HBs were tested by enzyme immunoassay (ELISA) (Murex anti-HBc (total) and ETI-AB-AUK-3 (anti-HBs), Diasorin, Italy). All serologic assays were carried out according to the manufacturer’s instructions. Anti-HBs titer was considered protective if its concentration is ≥ 10 mIU/ml. [23].
HBV DNA quantification
Positive samples for HBsAg were further tested for HBeAg (ETI-EBK PLUS, Diasorin, Italy), HBeAb (ETI-AB-EBK PLUS, Diasorin, Italy), ALT (Cobas, Roche), and HBV-DNA viral load by real-time polymerase chain reaction (PCR). The viral DNA was extracted from 200 μl of serum samples positive for HBsAg using the QIAamp DNA MiniKit (QIAGEN, Hilden, Germany), and re-suspended in 100 μl of a storage buffer provided by the kit manufacturer. HBV-DNA was quantified by real-time detection polymerase chain reaction primers according to the previously described protocol. The method was applied with slight modification as described previously [24, 25] The detection limit was 100 copies/ml. The extracted samples were tested for the presence of HBV DNA by 7500 Real-Time PCR machine to determine the viral load, or HBV real-time assays were performed using Artus HBV RG PCR Kit (Artus™ GmbH, Hamburg Germany) and the Real-Time PCR instrument, Rotor-Gene Q (QIAGEN, Germany). Detection limit of this assay is 3.8 IU/mL.
Interpretation of hepatitis markers
Interpretation of hepatitis markers was done according to the CDC criteria [23]. An individual was considered to have active infection if she is positive for HBsAg and HBcAb, resolving infection if HBcAb was only positive, while positive HBsAb was considered a marker of immunity due to vaccination if HBcAb was negative or as a sequence of previous infection if HBcAb was positive.
Ethical aspect
The study was approved by the Faculty of Medicine Ethical Committee (approval number 3860). The title, aim, and benefits of the study were explained individually to each pregnant women and after approval, an informed consent was obtained from each participant.
Statistical analysis
Statistical analysis was performed using SPSS-17 software (SPSS Inc., Chicago, Illinois, USA). Quantitative data were described in terms of range and mean (±SD), while non-numeric data were described as frequencies and percentages. Comparison of groups was performed by chi-square test and Student’s t test. HBsAb titer was represented as range, median, and geometric mean concentration. Comparison of HBsAb titer between groups was performed by a non-parametric, Kruskal-Wallis test. A value of p < 0.05 was considered statistically significant.
Results
Descriptive results
This study included 600 pregnant women divided into two groups. Group 1 included 285 (47.5%) aged 25 years or less; all received hepatitis B vaccination during their infancy while group 2 included the remaining 315 (52.5%); all were born before the vaccination program. The mean age of the studied women was 27.76 ± 6.77 years. Two thirds (67.8%) were from rural areas, 17.5% gave history of previous surgery and only 3.5% received blood transfusion. Of all participants, previous diagnosis of chronic illness was reported by 7.8%, and 12.5% gave family history of viral liver disease, due to HBV infection in 20 (3.3%) and HCV infection in 55 (9.2%).
The prevalence of HBV exposure (positive HBcAb) was 18.3% (110 women) and current infection (positive for HBsAg) was detected in 5% (30 women). Anti HBs antibodies were found in 30.7% (184 women). Coexistence of HBsAb with HBsAg and HBcAb was found in 3 (0.5%) women belonging to group 1.
According to the CDC criteria, participants were classified into 5 serological categories; immunity following infection in 40 women (6.7%), immunity related to vaccination in 141 (23.5%), current infection in 30 (5%), lone HBcAb sero-reactivity in 40 (6.7%), and 349 (58.2%) women were susceptible to HBV infection.
Comparative results
In this study, exposure to HBV (HBcAb positive) was higher among group 2 compared to group 1 (20.0% vs 16.5%, p = 0.29) and higher in women from rural areas compared to urban areas (20.1% vs. 14.5%, p = 0.11). Exposure to HBV was also more frequent in women with history of surgery and previous blood transfusion compared those without (19.0% and 23.8% vs. 18.2% and 18.1% respectively) with no statistically significance difference. However, the frequency of exposure to HBV infection was significantly higher among women with chronic illness compared to others without (31.9% and 17.2% respectively, P = 0.018). By logistic regression analysis, of all previous risk factors, only chronic illness proved to be an independent predictor of exposure to HBV infection (p = 0.025) (Table 1).
In this study, there was no significant differences between group 1 and group 2 regarding residence (p = 0.73), previous blood transfusion (p = 0.5), and chronic illness (p = 0.22). However, group 2 showed significantly higher frequency of previous surgery (p = 0.018) and family history of viral liver disease (p = 0.036) compared to group 1. Past exposure and current infection of HBV was more frequent in group 2 (20% and 5.1%) compared to group 1 (16.5% and 4.9%). However, the difference was not statistically significant. The frequency of sero-reactivity to HBsAb was significantly more in group 1 compared to group 2 (54.0% vs. 9.4%, p < 0.001) (Table 2).
Interpretation of hepatitis markers in groups 1 and 2
These serological profiles summarize the outcomes of HBV infection in group 1 and 2.
Table 3 demonstrates interpretation of hepatitis B markers in the studied groups. Group 1 showed a significantly higher frequency of women with immunity related to vaccination compared to group 2 (44.9 vs. 4.1%), a significantly lower frequency of women with lone HBcAb and lower frequency of women susceptible to HBV infection (3.5% and 38.6%) compared to group 2 (9.5% and 75.9%). Meanwhile, there was no statistically significant difference between both groups regarding the frequency of women with immunity following infection and chronic hepatitis B being 8.1 and 4.9% in group 1 and 5.4 and 5.1% for group 2. It is worth noting that 13 of 315 (4.1%) pregnant women in group 2 had evidence of post-vaccination immunity without evidence of exposure (HBsAb positive, HBcAb negative).
In this study, the titer of HBsAb of all studied women has a range of 0 and 371.6 mIU/ml. The median titer of HBsAb was significantly higher in group 1 than in group 2 (11 and 6 respectively IU/L, (p < 0.05). The frequency of HBsAb titers of < 10, 10–100, and > 100 mIU/ml were 46.0%, 40.3%, and 13.7% respectively in group 1 compared to 90.5%, 7.6%, and 1.9% in group 2 and these differences were statistically significant (p < 0.05). Meanwhile, the overall geometric mean of HBsAb values in women with protective titers was 45.2 and 43.29 IU/L respectively in groups 1 and 2 with no significantly difference (P > 0.5). In either group, the geometric mean of HBsAb values associated with infection was higher compared to that of post-vaccination effect; being 91.21and 40.1 mIU/ml (p < 0.05) in group 1 and 47.4 and 38.45 mIU/ml, (p > 0.05) in group 2. Meanwhile, the geometric mean of HBsAb concentration was significantly higher in infected individuals who cleared infection in group 1 than group 2 (91.21 vs. 47.4 IU/L, p < 0.05) (Fig. 1).
The geometric mean concentration (in mIU/ml) of HBsAb in immune women for the overall studied populationtotal (181), due to infection (40) or vaccination effect (141). After exclusion of 3 women with coexistent HBsAb and HBsAg, the geometric mean of 181 women with protective titers (151 in group 1 and 30 in group 2) was analyzed. Immune women following infection and due to vaccination were 23 and 128 in group 1 and 17 and 13 in group 2 respectively
Characteristics of women with chronic hepatitis B infection
In this study, all women positive to HBsAg (30 women) were HBeAg-negative, positive for HBeAb, and had high ALT. Meanwhile, all HBsAg-positive women were viremic, and the viral load ranges from 340 and 6590 copies/ml with a median of 836. The median level of viremia was higher in group 2 compared to group 1 patients (929 and 656, p = 0.0118). We noticed also the mean ALT level was higher in group 2 than group 1 women (43.25 ± 14.5 and 35.7 ± 9.0 IU/L respectively, p = 0.095).
Discussion
This study aimed to explore and interpret HBV markers among a large cohort of pregnant women born before and after the universal hepatitis B vaccination program for the newborn in Egypt. A secondary objective was to study the risk of MTCT of hepatitis B in view of the status of HBeAg and viral load in sera of HBsAg carriers. Although several studies have demonstrated the protective effects of hepatitis B vaccination in different age groups that received it during infancy, only few studies have examined the effect of vaccination in adults exceeding 18 years including an important risk group that is females at the age of child bearing.
In our study, interpretation of hepatitis markers revealed three important observations: (a) the high prevalence of exposure to HBV (18.3%), (b) the need for vaccination of more than one-half of the studied women (58.2%) that were negative for all markers of HBV, and (c) the high prevalence (5%) of HBsAg carriers with replicating virus. The latter represents a real risk of transmission to their offspring if not diagnosed and managed to provide post-exposure prophylaxis immediately after birth.
Efficacy of hepatitis B vaccination
The study also proved the efficacy of the universal vaccination given during infancy. Compared to non-vaccinated (group 2), vaccinated women (group 1) showed a significantly higher rate of immunity evidenced by having HBsAb titer ≥ 10 IU/L [(9.5% vs. 53%), lower prevalence of lone HBcAb (3.5% vs. 9.5%), and less frequency of susceptibility to HBV infection (38.6 vs. 75.9%). The latter group should be vaccinated if a further decline in the prevalence of HBV in the community is targeted. Unfortunately, the prevalence of HBsAg seropositivity was similarly high in both groups of the study.
The cause of vaccination failure in 14 women who received the vaccination is difficult to discuss particularly in the absence of documented evidence of receiving the three doses after their birth. However, till recently, the first dose of the vaccine was given with the conventional vaccines at the age of 2 months followed by two other doses at 4 and 6 months [19]. Vaccination failure probably occurred during parturition or due to vertical or horizontal modes within the family during the first months due to missing the birth dose [7]. Vaccinated women in this study had not received the birth dose of the vaccine which is an important post-exposure prophylactic measure in addition to HB immune globulin (HBIG). The possibility of transmission of HBV late in pregnancy or even during labor has been reported in 5% to 15% of infants born to mothers with high-level viremia despite prophylaxis with HBIG and the vaccine given at birth [26, 27]. It is worth noting that in 3 of 30 HBsAg carriers, there was co-existence of HBsAb, all were vaccinated. Infection with surface escape mutant could be another possible explanation which needs further study [28, 29].
In view of the high prevalence of active HBV infection found in this study and the lack of policy for ante-natal screening for HBV in hospitals of the Ministry of Health in Egypt, newborn of infected mothers could get infection without adequate post-exposure prophylaxis. Although recently, newborns receive the birth dose of the vaccine, lack of a simultaneous dose of HBIG could lead to transmission of infection particularly if the mother is not aware of infection. In 1989, MTCT was studied in a cohort of 35 HBsAg positive mothers by Ghaffar and colleagues. The authors reported that HBsAg was positive in 24% of newborn at birth, and increased to 37% at the age of 1 year [30]. However, in that study, no post-exposure prophylaxis was given.
In the current study, HBsAg carriers represent a real risk of transmission infection to their offspring in view of the results of testing HBeAg and HBV DNA viral load in their sera. Studies showed that in HBsAg-positive mothers, 90% of their offspring become infected if HBeAg is positive compared to 5–20% transmission if HBeAg is negative. Also, high viral load carries a higher risk of mother to child transmission. Reports of MTCT have been described despite of timely post-exposure prophylaxis with maternal HBV DNA levels of 106 to 108 copies/mL [30, 31]. It is worth noting that all the 30 HBsAg carriers, diagnosed in this study, were not aware of their infection status, and in 27 of them (90%), the ALT levels were high. Meanwhile, all carriers were HBeAg negative/HBeAb positive, and their HBV DNA levels were low (less than 2000 IU/ml). Accordingly, the risk of mother to child transmission in this study could be relatively low but this needs further study.
Pattern of HBsAb titer
In this study, women positive for HBsAb were classified into three categories [32]. The first was associated with resolved infection (positive for HBcAb), another one with HBsAg coexistence, and the third was immunity due to vaccination effect (negative for HBcAb. Although the GMC of HBsAb in groups 1 and 2 were very close (45.4 and 43.3 IU/L respectively), the GMC associated with infection was higher than that due to vaccination effect. This difference was statistically significant in group 1 [91.21 vs. 47.4 IU/L, p < 0.05] compared to group 2 [47.4 vs. 38.45 IU/L in group 2, p = 0.69]. This finding might suggest that in previously vaccinated individuals, HBV infection could occur when their HBsAb weans to below the protective levels. This infection, in previously immunized individuals, boosts the immune response as an anamnestic reaction while infection in an unvaccinated individual is a type of primary immune response.
The impact of repeated natural boosting on the titer of HBsAb among vaccinated individuals was tested in many studies. It has been reported that exposure to natural infection in individuals vaccinated during infancy is associated with an increase in the titer of HBsAb many years later. Offspring of infected mothers who received the vaccination showed better protection later in their lives (aged 5–20 years), compared to offspring of non-infective mothers [33,34,35].
In this study, weaning of HBsAb to levels below the protective level was evident in 46%. The progressive decline in the antibody titer in vaccinated children was reported in many studies. The level of HBsAb following exposure to hepatitis B proteins is also determined by the time of exposure. This is evidenced by a higher antibody response in vaccinated adults who received their doses during adolescence compared to their peers who received pediatric doses [36, 37].
In this study, the relatively high prevalence rate of HBsAg in vaccinated pregnant women could reflect a specific population in Ismailia; most of them were living in rural areas. Meanwhile, the prevalence of HBsAg in pregnant women is much higher than 1.4% reported in volunteer blood donors during the recent years. As in many countries all over the world, there is a trend toward a lower prevalence of HBsAg in Egypt during the last few decades. This could be attributed to the HBV vaccination of all newborns, pre-donation testing at blood banks, and careful preoperative and infection control measures [38].
Limitations of the study
In our study, there is no documented data regarding the completeness of the three doses of the vaccine and there is no documented data regarding HBV infection status among their family members. Furthermore, in 13 women, who were born before the vaccination program, there was evidence of post-vaccination immunity. Although they did not give history of vaccination, such individuals could receive the vaccine during one time of their life after their infancy. Furthermore, recall bias was evident regarding HBV infection among family members.
In conclusion, pregnant women born after the implementation of the universal infant vaccination program showed a higher degree of protection against HBV infection. However, the presence of high prevalence of HBsAg carriers in this group raised the possibility of active maternal infection and transmission during their birth.
Recommendation
As mother to child transmission is responsible for one-third of chronic HBV infections worldwide, efforts should be integrated to eliminate this route of transmission in Egypt. Screening of pregnant women during their ante-natal care and provision of HBIG to newborns of infected mothers are integral to achieve this goal.
Funding
This study is self-funded.
References
Hepatitis B http://www.who.int/mediacentre/factsheets/fs204/en/ Accessed on 27.3.2019
Lingala S, Ghany MG (2015) Natural history of hepatitis C. Gastroenterol Clin North Am 44(4):717–734
Ragheb MM (2010) Prevalence of hepatitis B virus in Egypt: Current status in an Afro-Asian country. Hepatology Research 40:732. https://doi.org/10.1111/j.1872-034X.2010.00677.x
Elinav E, Ben-Dov IZ, Shapira Y, Daudi N, Adler R, Shouval D, Ackerman Z (2006) Acute hepatitis A infection in pregnancy is associated with high rates of gestational complications and preterm labor. Gastroenterology 130(4):1129–1134
Ragheb M, Elkady A, Tanaka Y, Murakami S, Attia FM, Hassan AA, Hassan MF, Shedid MM, Abdel Reheem HB, Khan A, Mizokami M (2012) Multiple intra-familial transmission patterns of hepatitis B virus genotype D in north-eastern Egypt. J Med Virol. 84(4):587–595. https://doi.org/10.1002/jmv.23234
Schweitzer A, Akmatov MK, Krause G (2017) Background characteristics and sampling for the 47 low- and middle-income countries surveyed, by national hepatitis B vaccination schedule. Bull World Health Organ. 95(3):199–209G. https://doi.org/10.2471/BLT.16.178822
Edmunds WJ, Medley GF, Nokes DJ, Hall AJ, Whittle HC (1993) The influence of age on the development of the hepatitis B carrier state. Proc Biol Sci 253(1337):197–201
Elmaghloub R, Elbahrawy A, Didamony GE, Elwassief A, Saied Mohammad AG, Alashker A, Zedan H, Abdallah AM, Hemidah MH, Elmestikawy A, Fayoumei ME, Shahba H, Gawish A, Morsy MH, Hashim A, Abdelbaseer MA, Ueda Y, Chiba T, Abdelhafeez H (2017) Hepatitis B virus genotype E infection among Egyptian health care workers. J Transl Int Med. 5(2):100–105. https://doi.org/10.1515/jtim-2017-0012. eCollection 2017 Jun
Unicef (2015) Children in Egypt, 2015, A statistical Digtest, https://www.unicef.org/egypt/eg_Ch4.Immunization_and_Health_2015.pdf. Accessed 20 July 2019
Babanejad M, Izadi N, Najafi F, Alavian SM (2016) The HBsAg prevalence among blood donors from Eastern Mediterranean and Middle Eastern countries: a systematic review and meta-analysis. Hepat Mon 16(3):e35664. https://doi.org/10.5812/hepatmon.35664 eCollection 2016 Mar
Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ (2015) Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet. 386:1546–1555
El-Zanaty and Associates. EGYPT HEALTH ISSUES SURVEY (2015) Ministry of Health and Population, Cairo, Egypt. The DHS Program, ICF International, Rockville
Youssef MA, Abd-Elaleem HA, Elkabsh MY (1993) Prevalence of hepatitis C and hepatitis B among pregnant women in Assiut. Proceedings of Egyptian medical syndicate (EMS) annual scientific congress, February 2-4, Cairo, Egypt
Zahran KM, Badary MS, Agban MN, Abdel Aziz NH (2010) Pattern of hepatitis virus infection among pregnant women and their newborns at the Women’s Health Center of Assiut University, Upper Egypt. Int J Gynaecol Obstet 111(2):171–174
Abo-Salem ME, Mahrous OA, El-Shaarawy AA, Mohamed HM, Yehia SA (2014) Seroprevalence of hepatitis B among pregnant women attending maternal and child health centres in Shebin El-Kom district (Menoufia governorate). Menoufia Med J 27:847–852
Gad MA, Metwally MA, Eissa HA, Gehad MA, Rayan MM (2017) Antenatal screening for hepatitis B virus infection. Benha Med J 34:113–118
EL-Shabraw M, Mohamed MF, Hamdi MS, Ehab M et al (2013) Prevalence of hepatitis B virus infection among Egyptian pregnant women - a single center study. International Journal of Tropical Disease & Health 3(2):157–168
El-Karaksy HM, Mohsen LM, Saleh DA, Hamdy MS, Yassin NA, Farouk M, Salit ME, El-Shabrawi MH (2014) Applicability and efficacy of a model for prevention of perinatal transmission of hepatitis B virus infection: single center study in Egypt. World J Gastroenterol 20(45):17075–17083. https://doi.org/10.3748/wjg.v20.i45.17075
Mansour E, Abdul-Rahim S, Batouty G, Zaghloul I, Abdel-Hadi S (1993) Integration of hepatitis B immunization in the expanded program on immunization of the child survival project. J Egypt Public Health Assoc. 68(5-6):487–494
Preventing mother to child transmission of hepatitis B: operational field guidelines for delivery of birth dose of hepatitis B vaccine. http://www.wpro.who.int/hepatitis/hepb_operationalfieldguidelines.pdf. Accessed 20 July 2019
Lee C, Gong Y, Brok J, Boxall EH, Gluud C. Effect of hepatitis B immunisation in newborn infants of mothers positive for hepatitis B surface antigen: systematic review and meta-analysis. BMJ. Feb 11 2006;332(7537):328-336.
CensusInfo Egypt http://www.capmas.gov.eg/Pages/ShowPDF.aspx?page_id=http://www.censusinfo.capmas.gov.eg/. Accessed on 27.3.2019
Center of Disease and Control: Interpretation of Hepatitis B Serologic Test Results https://www.cdc.gov/hepatitis/hbv/pdfs/serologicchartv8.pdf?fbclid=IwAR1qt6lj4RU1WksaIhRT8O-aPy3NsqsQINIJNBJRhUg0XhUNnpikWy9Gmv4. Accessed 21 July 2019
Tanaka Y, Hasegawa I, Kato T, Orito E, Hirashima N, Acharya SK et al (2004) A case–control study for differences among hepatitis B virus infections of genotypes A (subtypes Aa and Ae) and D. Hepatology 40:747–755. https://doi.org/10.1002/hep.20365
Shin IT, Tanaka Y, Tateno Y, Mizokami M (2008) Development and public release of a comprehensive hepatitis virus database. Hepatol Res 38:234–243. https://doi.org/10.1111/j.1872-034X.2007.00262.x
Han G-R, Cao M-K, Zhao W, Jiang H-X, Wang C-M, Bai S-F, Yue X, Wang GJ, Tang X, Fang ZX (2011) A prospective and open-label study for the efficacy and safety of telbivudine in pregnancy for the prevention of perinatal transmission of hepatitis B virus infection. J Hepatol. 55:1215–1221. https://doi.org/10.1016/j.jhep.2011.02.032
Wen W-H, Chang M-H, Zhao L-L, Ni Y-H, Hsu H-Y, Wu J-F, Chen PJ, Chen DS, Chen HL (2013) Mother-to-infant transmission of hepatitis B virus infection: significance of maternal viral load and strategies for intervention. J Hepatol. 59:24–30. https://doi.org/10.1016/j.jhep.2013.02.015
Oon CJ, Chen WN (1998) Current aspects of hepatitis B surface antigen mutants in Singapore. J Viral Hepat 5 Suppl 2:17–23
Carman WF, Zanetti AR, Karayiannis P, Waters J, Manzillo G, Tanzi E, Zuckerman AJ, Thomas HC (1990) Vaccine-induced escape mutant of hepatitis B virus. Lancet. 336(8711):325–329
Ghaffar YA, elSobky MK, Raouf AA, Dorgham LS (1989) Mother-to-child transmission of hepatitis B virus in a semirural population in Egypt. J Trop Med Hyg 92(1):20–26
Nelson NP, Easterbrook PJ, McMahon BJ (2016) Epidemiology of hepatitis B virus infection and impact of vaccination on disease. Clin Liver Dis. 20(4):607–628
Ponde RA, Cardoso DD, Ferro MO (2010) The underlying mechanisms for the ‘anti-HBc alone’ serological profile. Archives of Virology 155:149–158
Poovorawan Y, Chongsrisawat V, Theamboonlers A, Bock HL, Leyssen M, Jacquet JM (2010) Persistence of antibodies and immune memory to hepatitis B vaccine 20 years after infant vaccination in Thailand. Vaccine 28(3):730–736
Huang LM, Chiang BL, Lee CY, Lee PI, Chi WK, Chang MH (1999) Long-term response to hepatitis B vaccination and response to booster in children born to mothers with hepatitis B e antigen. Hepatology 29(3):954–959
Resti M, Azzari C, Rossi ME, Adami Lami C, Tucci F, Vierucci A (1991) Five-year follow-up of vaccination against hepatitis B virus in newborns vaccinated with a reduced number of doses. Vaccine 9(1):15–18
Pileggi C, Papadopoli R, Bianco A, Pavia M (2017) Hepatitis B vaccine and the need for a booster dose after primary vaccination. Vaccine. 35(46):6302–6307. https://doi.org/10.1016/j.vaccine.2017.09.076
Bini C, Grazzini M, Chellini M, Mucci N, Arcangeli G, Tiscione E, Bonanni P (2018) Is hepatitis B vaccination performed at infant and adolescent age able to provide long-term immunological memory? An observational study on healthcare students and workers in Florence. Italy. Hum Vaccin Immunother. 14(2):450–455. https://doi.org/10.1080/21645515.2017.1398297
Nelson NP, Jamieson DJ, Murphy TV (2014) Prevention of perinatal hepatitis B virus transmission. J Pediatric Infect Dis Soc. 3(Suppl 1):S7–S12
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Responsible Editor: Giliane Souza Trindade.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kishk, R., Mandour, M., Elprince, M. et al. Pattern and interpretation of hepatitis B virus markers among pregnant women in North East Egypt. Braz J Microbiol 51, 593–600 (2020). https://doi.org/10.1007/s42770-019-00174-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-019-00174-3