Abstract
This study explores the management methods and approaches for patients with vascular Ehlers-Danlos Syndrome (vEDS) in a minimally invasive manner. In this paper, we presented two cases diagnosed with vEDS that presented with multiple aneurysms during their lives which were managed intravascularly, and outcomes were expressed. Two young male cases diagnosed with vEDS complained of numerous femoral, axillar, vertebral, and superior mesenteric artery aneurysms which were managed endovascularly with stent-grafts, coils, and plugs. We aimed to state that managing vascular complications in vEDS patients may be done minimally invasive with no major traditional surgery and should contain a multidisciplinary approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ehlers-Danlos Syndrome (EDS) is a genetic connective tissue disorder caused by a mutation in the COL3A1 gene, which encodes for type III collagen [1]. The vascular subtype of EDS (type IV EDS) is characterized by a high risk of arterial complications, including rupture, dissection, and aneurysm formation [2]. Traditional surgical approaches for the management of vascular complications in EDS can be challenging due to the fragility of the vessels. Endovascular management has emerged as a promising minimally invasive approach to manage these complications.
In this article, we aim to provide an overview of the role of endovascular management, and by highlighting the current evidence and ongoing research, we hope to contribute to the growing body of knowledge surrounding the use of endovascular management in type IV EDS patients.
Cases Description
The following cases have been presented with the explicit written consent from the patients, who have reviewed and approved the content to be shared for educational and illustrative purposes.
Case 1
An 8-year-old boy attended our hospital complaining of vomiting. After appropriate investigations, a 22 mm (N: 9.65–11.63 mm) pseudoaneurysm on his infrarenal abdominal aorta and a hematoma were found in his abdominal CT. The diagnosis of vEDS was confirmed after detecting a pathogenic variant in COL3A1 genetic testing. The covering segment with pseudoaneurysm was treated endovascularly with a 10 × 59 mm balloon expandable graft stent implantation. After a month, he complained of pain and swelling in his right neck after swimming. An enhanced CT revealed an approximate 20 mm saccular pseudoaneurysm in the proximal V2 segment of the right vertebral artery. After placing a guiding catheter in the right subclavian artery, a microcatheter was placed in the pseudoaneurysm lumen with the help of a 0.012-inch guide wire. After filling the pseudoaneurysm with several detachable coils, total embolization of the pseudoaneurysm was observed in control cerebral angiography. In the same session, a traumatic vertebrovertebral arteriovenous fistula (AVF) was observed in the cervical V2 segment of the right vertebral artery. After placing a guiding catheter in the left vertebral artery, the fistulous point was reached with a microcatheter from the contralateral vertebral artery in a trans-circular manner. The fistula level and parent artery were embolized with several detachable coils. Control angiographies showed total occlusion of the AVF. After that, cardiovascular surgery was requested to close the intervention site in the left femoral artery. In his follow-up after 2 years, he is still alive under celiprolol, and there are no aneurysms (Figs. 1, 2, 3, and 4).
A Area of pseudoaneurysm (white arrow) and retroperitoneal hematoma (red arrow) are observed at the level of the infrarenal abdominal aorta of the case 1. B, C Sagittal oblique CT and 3D volume rendering images of the aneurysm. D Filling the pseudoaneurysm sac on DSA images (black arrow). E Balloon expandable covered stent placement. F Pseudoaneurysm filling is not observed after the placement of stent
A Pseudoaneurysm (black arrow) in the right vertebral artery and hematoma (asterisk) in the right supraclavicular fossa of case 1. B Thinning and pseudoaneurysm due to vasoconstriction in the vertebral artery in coronal Maximum Intensity Projection (MIP) images on contrast-enhanced CT (black arrow). C Vertebral contrast enhancement is observed in the vertebral vein, paravertebral and epidural venous plexus on the right side secondary to the intervertebral fistula. D, E DSA images of the pseudoaneurysm and catheterization of the aneurysm lumen. F Coil caste after coil embolization
A In the DSA image of case 1 after left vertebral artery catheterization, retrograde filling in the right vertebral artery and early contrast enhancement in the vertebral vein and paravertebral venous plexus secondary to intervertebral fistula are observed. B Coil embolization of the fistula level via left retrograde catheterization of the right vertebral artery. C In control DSA images, the complete embolization of the fistula on the right side, and a low-flow fistula in a thin branch of the left vertebral artery to the right vertebral vein (black arrow) are observed. No additional intervention was planned for this lesion, and it was followed up. D Coil caste after coil embolization for pseudoaneurysm and intervertebral fistula at the level of the right vertebral artery
Case 2
A 15-year-old male patient complained of hematochezia with a diagnosis of superior mesenteric artery (SMA) aneurysm. The diagnosis of vEDS was confirmed after genetic testing. Although visceral aneurysms are rare in EDS patients, his DSA showed a saccular fusiform dissecting aneurysm measured 5 × 3 × 2 cm in the distal portion of the SMA. As well as there is also a wide fistulous connection between the aneurysm and superior mesenteric vein (SMV). Due to the risk of complication, no attempt was made and was suggested to intense follow-up. After 6 years, there were axillary and left femoral pseudoaneurysms after an intervention in another medical center. To prevent complications due to the fragility of the vessels, vascular surgeons were called in to address any potential issues. Subclavian artery catheterization cannot be achieved with left brachial artery cannulation. Upon the left upper extremity is fed by collaterals, an Amplatzer vascular plug 10 × 7 mm is placed in the axillary artery through the right femoral artery. Thereafter, the left superficial femoral artery was catheterized, and a Fluency Plus 40 × 7 mm stent graft was placed. In the patient’s SMA aneurysm, there was a regression in its size measured by 4.5 × 2.5 × 3 cm during follow-up and calcification in its wall. During his follow-up after 6 years, numbness and slight loss of strength in the left upper extremity, which was also present in the preoperative period, were observed to be stable (Figs. 5, 6, and 7).
A Upper extremity CTA examination reveals a giant pseudoaneurysm in the left axillary artery and a hematoma in the surrounding area of case 2. B DSA image of the aneurysm shows narrowing of the axillary artery secondary to vasoconstriction and compression. C Pseudoaneurysm filling is not observed after embolization with vascular plug. D Contrast stasis is observed in the aneurysm sac (black arrow: vascular plug)
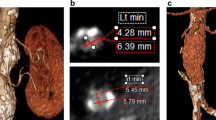
A, B There is a partial thrombosed pseudoaneurysm of 8 × 6 × 5 mm in the distal left main femoral artery and narrowing secondary to vasoconstriction in the femoral artery of case 2. C DSA image of the same patient. D After the placement of a covered stent graft in the patient, no filling is observed in the pseudoaneurysm sac (black arrows: stent markers)
A, B Giant SMA aneurysm originating from jejunal arterial branches, fistulized to the portal venous system of case 2. C, D DSA image of the same patient. E Dimensional reduction and wall calcifications are observed in the CT angiography of the aneurysm sac 6 years later (red arrow: arteriovenous fistula point). F 3D volume rendering image of the lesion in E
Discussion
Vascular Ehlers-Danlos Syndrome (vEDS) is a rare autosomal dominant genetic disorder caused by mutations in the COL3A1 gene [3]. The arterial and organ rupture in vEDS patients are the most seen complications [4]. The early diagnosis of the condition and surveillance imaging such as CTA and MRA are the two most important aspects of detecting and managing vascular complications in vEDS patients [5]. The management of vEDS is challenging due to its unpredictable and life-threatening nature, which requires a multidisciplinary approach [5]. De Backer et al. highlighted the importance of adopting the Paris way as a management approach, which involves close monitoring of patients and using prophylactic measures such as beta-blockers and angiotensin-converting enzyme inhibitors [6]. Assessing arterial damage in vEDS patients is crucial for determining appropriate management strategies. A retrospective multicentric cohort study by Adham et al. evaluated that the patients with vEDS had significantly increased arterial stiffness, which was associated with an increased risk of arterial dissection or rupture. Therefore, non-invasive imaging techniques, such as pulse wave velocity measurement, could be used to monitor arterial stiffness in patients with vEDS [7]. Another study by Adham et al. evaluated that cervical artery dissection is a common complication of vEDS and is associated with a high risk of stroke, for which prophylactic measures, such as antiplatelet therapy, should be considered for these patients [8]. Endovascular management is a minimally invasive approach to managing vascular complications of vEDS patients [9]. Alqahtani et al. [10] reported a study that included five patients with vEDS who underwent endovascular repair for various vascular complications. The study found that endovascular interventions, including stent graft placement and embolization, were effective in managing vascular complications in vEDS, with low rates of perioperative morbidity and mortality. However, the use of endovascular procedures in patients with vEDS is not without its risks. Patients with vEDS are more susceptible to endovascular complications, such as arterial dissection, perforation, and rupture, due to the fragility of their arterial walls [7].
Conclusions
Vascular Ehlers-Danlos Syndrome is a potentially life-threatening genetic disorder. Through analysis of patient data in our study, we reveal significant reductions in complications such as arterial dissections and aneurysms following endovascular intervention. The successful outcomes underscore the importance of early detection and intervention utilizing endovascular techniques. Continuous research and refinement of endovascular techniques hold promise for further enhancing the efficacy and safety of vascular interventions in managing the complex manifestations of vEDS. Ultimately, our study reinforces the notion that targeted endovascular interventions address acute complications and hold promise in fostering long-term vascular health and enhancing the quality of life for vEDS patients.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Byers PH, Murray ML. Ehlers-Danlos syndrome: a showcase of conditions that lead to understanding matrix biology. Matrix Biol. 2014;33:10–5.
Pepin MG, Schwarze U, Rice KM, Liu M, Leistritz D, Byers PH. Survival is affected by mutation type and molecular mechanism in vascular Ehlers-Danlos syndrome (EDS type IV). Genet Med. 2014;16(12):881–8.
Byers PH. Vascular Ehlers-Danlos syndrome. GeneReviews® [Internet]; 2019.
Byers, P. H., Belmont, J., Black, J., De Backer, J., Frank, M., Jeunemaitre, X., ... & Wheeldon, N. (2017, March). Diagnosis, natural history, and management in vascular Ehlers–Danlos syndrome. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics 175, 1, 40–47
Abayazeed A, Hayman E, Moghadamfalahi M, Cain D. Vascular type Ehlers-Danlos Syndrome with fatal spontaneous rupture of a right common iliac artery dissection: case report and review of literature. J Radiol Case Rep. 2014;8(2):63.
De Backer J, De Backer T. Vascular Ehlers-Danlos syndrome management: the Paris way, a step forward on a long road. J Am Coll Cardiol. 2019;73(15):1958–60.
Adham S, Legrand A, Bruno RM, Billon C, Dalens V, Boutouyrie P, ..., Jeunemaitre X (2022). Assessment of arterial damage in vascular Ehlers-Danlos syndrome: a retrospective multicentric cohort. European Heart Journal, 43(Supplement_2), ehac544–1981
Adham S, Billon C, Legrand A, Domigo V, Denarié N, Charpentier E, ..., Frank M (2021) Spontaneous cervical artery dissection in vascular Ehlers-Danlos syndrome: a cohort study. Stroke, 52(5), 1628–1635
Benrashid E, Ohman JW. Current management of the vascular subtype of Ehlers-Danlos syndrome. Curr Opin Cardiol. 2020;35(6):603–9.
Alqahtani M, Claudinot A, Gaudry M, Bartoli A, Barral PA, Vidal V ..., Bal L (2022) Endovascular management of vascular complications in Ehlers–Danlos syndrome type IV. J Clinical Med, 11(21), 6344
Author information
Authors and Affiliations
Contributions
C.C. and I.O. conceptualized the research study and designed the methodology. M.A. and C.P. conducted the experiments and collected the data. M.A. and I.O. analyzed the data and interpreted the results. M.A. drafted the initial manuscript. C.P. and C.C. critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Written consent for publication has been obtained from the patient parents.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Avarand, M., Pinarci, C., Cinar, C. et al. Endovascular Procedure in Managing Vascular Complications of Type IV Ehlers-Danlos Syndrome: Case Report. SN Compr. Clin. Med. 6, 97 (2024). https://doi.org/10.1007/s42399-024-01714-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-024-01714-1