Abstract
Considering the importance of empirical antibiotic treatment before obtaining urine culture results, it is necessary to know the pattern of microbial sensitivity to antibiotics to properly manage urinary tract infection (UTI). The present research aimed at determining type of pathogens causing UTI and the pattern of antibiotic sensitivity in urine cultures of hospitalized patients in Hamadan, Iran. This cross-sectional study was conducted on 120 individuals (including 60 cases as hospital-acquired infection and 60 cases as community-acquired infection group). The urine samples were cultured and processed for subsequent uropathogens isolation. The specimens were cultivated on Muller-Hinton Agar (Merck, Germany) and incubated at 37 °C for 24 h. The antibiotic sensitivity was determined using disc diffusion method by antibiogram discs (English MAST Company, recommended by the Clinical and Laboratory Standards Institute (CLSI) guideline) in two groups of outpatients and inpatients simultaneously. According to the results, most isolates were resistant to commonly used antibiotics in the treatment of UTIs. A significant increase was observed in drug resistance to ciprofloxacin, levofloxacin, cotrimoxazole, and ceftriaxone, especially in community-acquired cases. In community-acquired UTIs from the gram-negative pathogen, E. coli showed the highest drug sensitivity to imipenem (100%) and fosfomycin (95%), and the highest drug resistances were observed for ciprofloxacin (62.5%) and levofloxacin (60%). In the cases of E. coli acquired from the hospital, resistance to fluoroquinolones, ceftriaxone, and cefepime increased, while the sensitivity to meropenem, imipenem, and piperacillin-tazobactam was 80.6%, 87.1%, and 90%, respectively. Urinary tract infection was highly prevalent in the study area and all uropathogens isolated developed resistance against mostly used antibiotic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infection (UTI) is common in many patients referred to emergency units and hospitalizations. UTIs account for up to 40% of all hospital-acquired infections, associated with increased morbidity, mortality, and length of hospitalization. UTIs include asymptomatic bacteriuria, cystitis (infection of the bladder/lower urinary tract), pyelonephritis (infection of the kidney/upper urinary tract), and prostatitis [1]. Various bacteria such as Escherichia coli, Klebsiella spp., Proteous spp., Pseudomonas spp., and Enterococcus spp. are considered major causes of UTIs [2].
The prevalence of hospital-acquired UTIs was estimated to be about 10%, 14%, and 11% in the Pan European Prevalence (PEP), Pan Eurasian Prevalence (PEAP), and a combined analysis studies, respectively [3]. It has been estimated that community-acquired UTIs can be diagnosed in 1% of boys and 3–8% of girls. It has been reported that E. coli is the most common organism causing UTI in adults, accounting for 75–90% of isolated bacteria [4]. Most patients with UTIs are treated empirically with conventional antibiotics. However, in recent years, extended-spectrum beta-lactamase (ESBL)-producing pathogens have been severally reported as a cause of UTI. In this regard, there is a major challenge in treating ESBL-UTIs, due to the resistance of these organisms to cephalosporins and aztreonam as common antibiotics used for UTIs. Moreover, high resistance rates have been reported in these organisms to trimethoprim-sulfamethoxazole (TMP-SMX) and fluoroquinolones [5].
Based on the World Health Organization (WHO) report, ESBL-producing Enterobacteriaceae (ESBL-EB) poses a serious risk to public health [6]. It has also been reported that the rate of resistance to third-generation cephalosporins in E. coli was approximately 15.1% in Europe, whereas the resistance rate of Klebsiella pneumonia was reported to be about 31.7% [7]. In contrast, in a related study, the prevalence of resistant ESBL-EB isolates in USA was reported to be about 12.6% nationwide [8].
Various factors are associated with ESBL-UTI, including older age [9,10,11], male gender [12,13,14], having a history of previous UTI [15, 16], international travel, prior use of antibiotics, diabetes mellitus, and prior use of proton pump inhibitors [9, 16].
Chronic obstructive pulmonary disease, kidney disease, malignancy, consumption of immunosuppressive drugs, and freshwater swimming have been identified as risk factors for UTI [13]. Some other risk factors such as hospitalization in the last 3 months, healthcare-associated UTI, upper UTI, recurrent UTI, and having a urinary catheter are associated with UTI [17].
Objectives
Considering that the antibiotic sensitivity report of urine samples is generally accessible within 48–72 h after the request [4] and the empirical treatment must be started earlier, it is essential to obtain accurate information regarding common antibiotic resistance in each region and even in each hospital to provide appropriate treatment measures, reduce treatment failure, and reduce bacterial resistance. The objective of the present study was to investigate the type of pathogens and the pattern of antibiotic sensitivity in the urine cultures of patients hospitalized in Shahid Beheshti Hospital in Hamadan province, Iran. The samples were classified into two community and hospital-acquired UTIs and the results were compared between the two groups during 2017–2019 to obtain the exact pattern of antibiotic sensitivity. In this study, for the first time, the E-test method was applied to evaluate the bacterial sensitivity to various antibiotics such as vancomycin and colistin.
Patients and Methods
Study Population
This cross-sectional study was performed in Shahid Beheshti Hospital, a tertiary care and referral center located in Hamadan City, the center of Hamadan province in the west of Iran. Patients referred to the hospital who met the inclusion criteria from March 21, 2018, to March 20, 2020, were included in the present study.
The patients were eligible for the study if their urine cultures were positive (both for the community and for the hospital cases). Cases with false-positive urine cultures and the growth of more than two organisms in the urine sample (sample contamination) were excluded from the study. In this study, hospital-acquired UTI means the occurrence of a urinary infection in a patient within 48 h after hospitalization (the patient was not infected at the time of hospitalization or was not in the incubation period) or the occurrence of a urinary infection in a patient who has undergone surgery or recent urological interventions. Moreover, community-acquired UTI refers to the positive culture of a urine sample in a symptomatic outpatient without urological interventions in the previous 2 weeks (regardless of whether the patient is treated on an outpatient basis or needs to be admitted to the hospital and receives injectable medicine). Finally, 100 CFU/mL in symptomatic cases was enough to diagnose positive urine culture (whether acquired from the community or the hospital).
Variables and Data Collection Tool
The data collection tool was a self-administered questionnaire consisting of demographic variables (e.g., age, sex, and marital status), underlying disease (urinary stones, diabetes mellitus, kidney transplantation, history of kidney surgery, dialysis, spinal cord injury, malignancy, heart diseases, and high blood pressure), a history of UTI, type of uropathogens, pattern of antibiotic sensitivity, duration of hospitalization, duration of catheterization, receiving antibiotics in the last 2 weeks, and type of antibiotic regimen.
Sample Processing and Antimicrobial Susceptibility Testing
In the current descriptive cross-sectional study, 120 urine samples were collected from patients were referred to Shahid Beheshti Hospital located in Hamadan province, Iran, for 2 years (2017–2019). The specimens were cultivated on Muller-Hinton Agar (Merck, Germany) and incubated at 37 °C for 24 h. First, the colonies were counted, and then the cultures of specimens with bacterial counts of > 102 cfu/mL, were considered positive, and gram-staining technique was performed. The antibiotic sensitivity was determined using disc diffusion method by antibiogram discs (English MAST Company, recommended by the Clinical and Laboratory Standards Institute (CLSI) guideline) in two groups of outpatients and inpatients simultaneously. In the specimens that the obtained gram-negative organism was resistant to cephalosporins and carbapenems (multi-drug resistant), the sensitivity to colistin was evaluated and determined using E-TEST strips (Biofiltem). Then, bacterial genus and species were determined using the standard biochemical tests.
Sample Size
A 1-sided type I error probability of 0.05 with a power of 0.8 was considered a statistical study assumption. In order to demonstrate our expected effect, by considering a 1-sided significance level of 5% and a power of 80%, 60 patients were estimated as the sample size. This assumption was based on Khoshbakht Rahem et al. study with a UTI proportion of 83%.
Statistical Analysis
Mean (standard deviation) and frequency (percentage) were used for describing quantitative and qualitative variables. Fisher's exact test was applied for comparing the antibiogram results of qualitative variables, and one-way analysis of variance (ANOVA) was used for quantitative variables. P < 0.05 was considered statistically significant.
Results
This study was conducted to compare the frequency of bacterial agents and their antibiotic sensitivity patterns in patients referred to Shahid Beheshti Hospital in Hamadan, Iran. A total of 120 patients were examined. Of them, 60 patients had hospital-acquired UTIs, and 60 patients had community-acquired UTIs. In the community-acquired UTI, 30% of the cases were male, and 70% were female. In hospital-acquired UTIs, 56.7% of the cases were men, and 43.3% were women. There was a significant difference in gender distribution between the community and hospital-acquired infections (P = 0.003). In other words, in hospital-acquired infections, the dominant gender was men, and in community-acquired infections, the dominant gender was women.
The mean (standard deviation) of the age in patients with community and hospital-acquired UTIs were 53.34 ± 18.09 and 63.58 ± 19.51 years, respectively. The mean age of the patients with hospital-acquired UTIs was significantly higher than the patients with community-acquired UTIs (P = 0.003). The most common age groups involved in the hospital- and community-acquired UTIs were 60–69 and 30–39 years old, respectively. Individuals aged 70–79 years and 60–69 years had the highest relative frequency of hospital-acquired UTIs, respectively. There were no significant differences between the two groups in terms of marital status, smoking, place of residence, length of hospitalization, and history of antibiotic consumption. Although, the presence of underlying diseases in the hospital-acquired UTIs group was significantly higher than the community-acquired UTIs group (P < 0.001). There was a statistically significant relationship between the history of urological interventions and the occurrence of hospital-acquired infection (P = 0.004). E. coli and Pseudomonas (each with a frequency of 25%) were the most common microorganisms causing nosocomial UTI caused by intervention. Table 1 presents the demographic and clinical manifestations of the two groups of patients (community and hospital-acquired infection).
Based on the results presented in Tables 2 and 3, there was a decreasing trend in the sensitivity of E. coli in both community and hospital-acquired groups to ceftriaxone, gentamicin, levofloxacin, ciprofloxacin, cotrimoxazole, and even cefepime. While the sensitivity to piperacillin-tazobactam and carbapenems were still high, and the sensitivity to fosfomycin was 95% and high in both groups. Also, the sensitivity of Enterobacteriaceae in both community or the hospital-acquired groups to nitrofurantoin, ceftriaxone, ciprofloxacin, gentamicin, cefepime, and cotrimoxazole was low, while the sensitivity to fosfomycin, carbapenems, and piperacillin-tazobactam in the patients of the community-acquired group was high and even showed a sensitivity of 100%. In the hospital-acquired group, antibiotic resistance was still high. However, all carbapenems-resistant cases showed a 100% sensitivity to colistin. Tables 2 and 3 present more detail about the antibiotic sensitivity pattern of gram-negative/positive microorganisms in patients with community/hospital-acquired UTIs.
Of 60 hospital-acquired UTIs, 13 cases (21.7%) occurred in the ICU and 57 cases (78.3%) in other units. The incidence of hospital-acquired UTIs in the internal department was significantly higher than in other hospital units (P < 0.001).
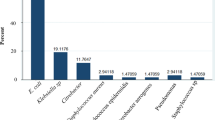
The sensitivity of hospital-acquired Enterococci to ceftriaxone, gentamicin, ciprofloxacin, ampisulbactam, and fosfomycin was decreasing, so that sensitivity to vancomycin, imipenem/cilastatin, and ampicillin/sulbactam was observed in 70%, 50%, and 60% of the cases, respectively (Fig. 1).
Our analysis indicated that ceftriaxone and ciprofloxacin were the most experimentally prescribed antibiotics in all hospitalized patients, whether acquired from the community or the hospital. Nevertheless, the compliance rate of the prescribed empirical regimen with the antibiogram pattern in community-acquired and hospital-acquired UTIs was 33.33% and 37.68%, respectively. Resistance to ceftriaxone in community and hospital-acquired UTIs was 3.56% and 51.6%, respectively. Resistance to ciprofloxacin in community-acquired and hospital-acquired UTIs was 90% and 60.8%, respectively. No resistance to vancomycin, meropenem, gentamycin, levofloxacin, and cefepime was observed in the community-acquired UTI samples. In general, 33.33% of the community-acquired UTIs were sensitive to antibiotics, and the rest of the samples were resistant (66.66%). In terms of hospital-acquired UTIs, 37.68% of the cases were sensitive, 5.79% were semi-sensitive, and the rest of them were resistant to antibiotics (56.52%).
Discussion
This cross-sectional study was conducted to compare the resistance pattern of uropathogens and their compatibility with empirical treatments in the community and hospital-acquired UTIs. Our results indicated that community-acquired UTI was more common among women, while hospital-acquired UTI was more common among men. The mean age of patients with hospital-acquired UTI was higher than that of the patients with community-acquired UTI. However, the average age of patients in both groups was over 50 years. The history of comorbidity and underlying diseases in the hospital-acquired UTI was significantly higher than the community-acquired UTI. Drug resistance in microorganisms causing hospital-acquired UTI was higher than that in the community-acquired group. There was a very low frequency of drug sensitivity in empirical regimen for the treatment of UTI. In addition, our result indicated that among the gram-negative bacteria, E. coli and Enterobacter were the only causes of community-acquired UTI, while in hospital-acquired UTI, E. coli, Enterobacter, Pseudomonas, and Proteus spp. were the most common microorganisms, respectively. It should be noted that infection with E. coli in the hospital-acquired UTI was significantly higher than that in the community hospital-acquired UTI. On the other hand, among gram-positive bacteria, Enterococcus was obviously increased in hospital cases and urological interventions. This finding was consistent with the results of Tandogdu et al. [18], Hoban et al. [19], Akoachere et al. [20], and Magaliano et al. [21] studies.
The sensitivity of community-acquired E. coli was 37.5% to ciprofloxacin, 37.5% to levofloxacin, and 40% to ceftriaxone. While the sensitivity to cotrimoxazole and gentamicin was 75%, it seems that regarding the outpatient empirical regimen, the prescription of these two drugs is preferable to the drug regimens based on fluoroquinolones. Due to 100% sensitivity to imipenem compared to 92.5% to meropenem and 90% to piperacillin-tazobactam, the empirical imipenem regimen seems more suitable for critical cases.
In the cases of E. coli acquired from the hospital, sensitivity to fluoroquinolones (30%), ceftriaxone (29%), and cefepime (41.2%) decreased, while the sensitivity to meropenem, imipenem, and piperacillin-tazobactam was 80.6%, 87.1%, and 90%, respectively. Therefore, it seems that these antibiotics can be used as a preferred option in the hospital-acquired type.
Regarding Enterobacter, the sensitivity to nitrofurantoin, ceftriaxone, ciprofloxacin, levofloxacin, cefepime, and cotrimoxazole was low in both groups. For example, in the case of cefepime, 57.1% sensitivity was observed in the community-acquired cases, while it decreased to 14.3% in the hospital-acquired cases. Moreover, in cases of broad-spectrum antibiotic regimens, 28.6% of Enterobacter samples obtained from hospitals were resistant to imipenem and 49.2% to meropenem.
Regarding Pseudomonas, which was obtained only in cases acquired from the hospital, the sensitivity to ceftriaxone was 25%, to cefepime, levofloxacin, and gentamicin was 50%, and sensitivity to fosfomycin was 75%. Also, 75% of the Pseudomonas were sensitive to piperacillin-tazobactam and carbapenems, and all of them were sensitive to colistin.
All gram-negative bacteria were sensitive to fosfomycin at a high rate, and no cases of resistance to colistin (by the E-test method) were found.
In terms of gram-positive urinary organisms, the most important factor was Enterococci, which in the hospital-acquired UTIs was significantly higher than the community-acquired UTIs. The sensitivity of this microorganism was 20% to ceftriaxone, 60% to ampicillin-sulbactam, 70% to cefoxitin and vancomycin, and 50% to imipenem. In hospital-acquired cases, 30% of Enterococci were not sensitive to vancomycin, while in community-acquired cases, 100% were sensitive to vancomycin. Therefore, the increase in cases of vancomycin-resistant Enterococci in the hospital setting or after urological interventions is worthy of consideration.
In the majority of cases, especially in the community-acquired, the initial empirical regimen was based on fluoroquinolones, ceftriaxone, or cefepime, but only ciprofloxacin was 10% and 34.8% sensitive and effective in community and hospital-acquired cases, respectively. In other words, in most cases, the antibiotic sensitivity was inconsistent with the patient's initial prescription regimen.
Our results showed that the most common gram-negative microorganism causing UTIs was E. coli. Based on previous research, E. coli accounts for as many as 90% of all UTIs among ambulatory populations. Among healthy women aged 18–39, 80% of UTIs are caused by E. coli. It has been well known that among different species causing UTIs, gram-negative, facultative anaerobic, and uropathogenic E. coli (uPeC) are the most common causes of these infections in the population [22].
In terms of gender, in hospital-acquired infections, the dominant gender was men, and in community-acquired infections, the dominant gender was women. Women are at risk of UTIs compared to men due to differences in anatomy. In women, moist areas around the urethra and vagina promote the growth of uropathogens. The short distance between the urethra and the opening of the anus and bladder increases the possibility of infection caused by ascending uropathogens [15]. In general, about half of women experience a UTI in their late 20 s [23]. Moreover, approximately 20–30% of women with a first UTI will experience two or more infections. Among them, in 5% of the cases, chronic recurrent infection affects their quality of life [13]. In the present study, most of the hospital-acquired UTIs were observed in men (56.7%), which could be due to the existence of a specialized urology department at Shahid Beheshti Hospital in Hamadan.
Our results indicated that people with comorbidities and underlying diseases are at a higher risk of developing UTIs (in both the community and acquired UTI groups). Several antibiotic treatments are used in patients with comorbidity, which could change the normal bacterial flora and increase the risk of infection caused by multi-drug-resistant pathogens; in fact, UTIs patients are at increased risk for colonization with resistant organisms, and colonization may persist for long periods (i.e., months to years) [24]. In all these cases, there is a possibility of increasing the risk of various infections, including UTIs, especially in patients with comorbidities. For example, diabetes mellitus is an underlying disease investigated in this research. Based on previous research, diabetes mellitus increases the risk of several infections such as UTI. Multiple epidemiological studies showed a 1.21–2.2 increase in the relative risk of UTI in individuals with diabetes compared to those without diabetes. Multiple potential mechanisms of diabetes may contribute to this increased susceptibility to UTI. Higher glucose concentrations in urine may promote the growth of pathogenic bacteria and act as a culture medium. Decreased immune function, such as impaired migration, intracellular killing, phagocytosis, or chemotaxis in polymorphonuclear leukocytes in patients with diabetes, may weaken host defenses against UTI. Finally, genitourinary nerve damage caused by diabetes may lead to inefficient bladder emptying and partial urinary retention, leading to favorable conditions for UTI [25].
Another interesting finding in the present study was that the prevalence of hospital-acquired UTIs was higher in the elderly over 60 years of age, and in community-acquired urinary infections, people over 50 had the highest frequency. This result is consistent with the findings of the previous studies. For instance, it has been reported that the elderly are at a higher risk of contracting UTIs due to various reasons, such as reduced immune system function, bladder problems, kidney failure, urinary incontinence, straining while urinating, insufficient nutritional status, loss of resistance to infections, and the use of medical methods such as urinary catheters [11, 26].
Conclusion
According to these results, community-acquired urinary infection is more common in women and hospital-acquired urinary infection is more common in men. The average age of hospital-acquired urinary infection patients is significantly higher than community-acquired urinary infection. Drug resistance in hospital-acquired UTI microorganisms was higher than in the community. The drug sensitivity rate of empirical regimen for urinary infection was very low. Also, among gram-negative bacteria causing UTIs, non-E. coli cases, especially Enterobacter and Pseudomonas, showed a high frequency. Moreover, a high frequency was observed for Enterococci among the urinary gram-positive bacteria, especially in hospital-acquired cases. Also, most of these uropathogens were resistant to commonly used antibiotics in the treatment of UTIs; a significant increase was observed in drug resistance to ciprofloxacin, levofloxacin, cotrimoxazole, and ceftriaxone, especially in community-acquired cases. Therefore, it is necessary to determine the frequency and regional antibiotic sensitivity patterns of bacteria causing UTIs, and even separately for each hospital treatment center, to provide an effective and proper protocol for the management and treatment of serious and critical patients with UTIs. It can be concluded that based on the antibiotic sensitivity pattern of the urine culture test, the appropriate regimen should be selected for each patient. Also, considering the result of high sensitivity to fosfomycin, this drug can be a suitable choice for the empirical regimen of hospitalized patients with cystitis. Finally, according to the increasing trend of drug resistance, physicians and medical staff should seriously prevent the arbitrary and unnecessary prescription of antibiotics, especially in the treatment of asymptomatic bacteriuria.
Limitations of the Study
A lack of access to the previous history of antibiotic use of some patients due to the lack of medical records. It is recommended that researchers use a larger sample size in future studies.
Data Availability
The data regarding this work is available in the SPSS format and can be provided by the corresponding author upon request.
Code Availability
Not applicable.
References
Azap OK, Arslan H, Serefhanoğlu K, et al. Risk factors for extended-spectrum beta-lactamase positivity in uropathogenic Escherichia coli isolated from community-acquired urinary tract infections. Clin Microbiol Infect. 2010;16(2):147–51. https://doi.org/10.1111/j.1469-0691.2009.02941.
Ronald A. The etiology of urinary tract infection: traditional and emerging pathogens. Am J Med. 2002;113(Suppl. 1A):14S-19S. https://doi.org/10.1016/s0002-9343(02)01055-0.
Johansen TE, Cek M, Naber K, Stratchounski L, Svendsen MV, Tenke P, PEP and PEAP study investigators, Board of the European Society of Infections in Urology. Prevalence of hospital-acquired urinary tract infections in urology departments. Eur Urol. 2007;51(4):1100–12.
Bader MS, Loeb M, Brooks AA. An update on the management of urinary tract infections in the era of antimicrobial resistance. Postgrad Med. 2017;129(2):242–58. https://doi.org/10.1080/00325481.2017.1246055.
Chandrasekhar D, Dollychan A, Roy BM, Cholamughath S, Parambil JC. Prevalence and antibiotic utilization pattern of uropathogens causing community-acquired urinary tract infection in Kerala. India J Basic Clin Physiol Pharmacol. 2018;29(6):671–7. https://doi.org/10.1515/jbcpp-2018-0015.
Mancuso G, Midiri A, Gerace E, Biondo C. Bacterial antibiotic resistance: the most critical pathogens. Pathogens. 2021;10(10):1310. https://doi.org/10.3390/pathogens10101310.
Friedrich AW. Control of hospital acquired infections and antimicrobial resistance in Europe: the way to go. Wien Med Wochenschr. 2019;169(Suppl. 1):25–30. https://doi.org/10.1007/s10354-018-0676-5.
Gupta V, Ye G, Olesky M, Lawrence K, Murray J, Yu K. Trends in resistant Enterobacteriaceae and Acinetobacter species in hospitalized patients in the United States: 2013–2017. BMC Infect Dis. 2019;19(1):742. https://doi.org/10.1186/s12879-019-4387-3.
KettaniHalabi M, Lahlou FA, Diawara I, et al. Antibiotic resistance pattern of extended spectrum beta lactamase producing Escherichia coli isolated from patients with urinary tract infection in Morocco. Front Cell Infect Microbiol. 2021;11:720701. https://doi.org/10.3389/fcimb.2021.720701.
Puspandari N, Sunarno S, Febrianti T, et al. Extended spectrum beta-lactamase-producing Escherichia coli surveillance in the human, food chain, and environment sectors: tricycle project (pilot) in Indonesia. One Health. 2021;13:100331. https://doi.org/10.1016/j.onehlt.2021.100331.
Tüzün T, Sayın Kutlu S, Kutlu M, Kaleli İ. Risk factors for community-onset urinary tract infections caused by extended-spectrum β-lactamase-producing Escherichia coli. Turk J Med Sci. 2019;49(4):1206–11. https://doi.org/10.3906/sag-1902-24.
Ben-Ami R, Rodríguez-Baño J, Arslan H, et al. A multinational survey of risk factors for infection with extended-spectrum beta-lactamase-producing enterobacteriaceae in nonhospitalized patients. Clin Infect Dis. 2009;49(5):682–90. https://doi.org/10.1086/604713.
Søgaard M, Heide-Jørgensen U, Vandenbroucke JP, Schønheyder HC, Vandenbroucke-Grauls CMJE. Risk factors for extended-spectrum β-lactamase-producing Escherichia coli urinary tract infection in the community in Denmark: a case-control study. Clin Microbiol Infect. 2017;23(12):952–60. https://doi.org/10.1016/j.cmi.2017.03.026.
Ghelichkhani S, Jenabi E, Jalili E, Alishirzad A, Shahbazi F. Pregnancy outcomes among SARS-CoV-2-infected pregnant women with and without underlying diseases: a case-control study. J Med Life. 2021;14(4):518.
Inns T, Millership S, Teare L, Rice W, Reacher M. Service evaluation of selected risk factors for extended-spectrum beta-lactamase Escherichia coli urinary tract infections: a case-control study. J Hosp Infect. 2014;88(2):116–9. https://doi.org/10.1016/j.jhin.2014.07.009.
Rogers BA, Ingram PR, Runnegar N, et al. Community-onset Escherichia coli infection resistant to expanded-spectrum cephalosporins in low-prevalence countries. Antimicrob Agents Chemother. 2014;58(4):2126–34. https://doi.org/10.1128/AAC.02052-13.
Søraas A, Sundsfjord A, Sandven I, Brunborg C, Jenum PA. Risk factors for community-acquired urinary tract infections caused by ESBL-producing enterobacteriaceae–a case-control study in a low prevalence country. PLoS One. 2013;8(7):e69581. https://doi.org/10.1371/journal.pone.0069581.
Tandogdu Z, Wagenlehner FM. Global epidemiology of urinary tract infections. Curr Opin Infect Dis. 2016;29(1):73–9. https://doi.org/10.1097/QCO.0000000000000228.
Hoban DJ, Lascols C, Nicolle LE, et al. Antimicrobial susceptibility of Enterobacteriaceae, including molecular characterization of extended-spectrum beta-lactamase-producing species, in urinary tract isolates from hospitalized patients in North America and Europe: results from the SMART study 2009–2010. Diagn Microbiol Infect Dis. 2012;74(1):62–7. https://doi.org/10.1016/j.diagmicrobio.2012.05.024.
Akoachere JF, Yvonne S, Akum NH, Seraphine EN. Etiologic profile and antimicrobial susceptibility of community-acquired urinary tract infection in two Cameroonian towns. BMC Res Notes. 2012;5:219. https://doi.org/10.1186/1756-0500-5-219.
Magliano E, Grazioli V, Deflorio L, et al. Gender and age-dependent etiology of community-acquired urinary tract infections. Sci World J. 2012;2012:349597. https://doi.org/10.1100/2012/349597.
Mohamed MA, Abdifetah O, Hussein FA, Karie SA. Antibiotic resistance pattern of Escherichia coli isolates from outpatients with urinary tract infections in Somalia. J Infect Dev Ctries. 2020;14(3):284–9. https://doi.org/10.3855/jidc.12189.
Prasada Rao CMM, Vennila T, Kosanam S, et al. Assessment of bacterial isolates from the urine specimens of urinary tract infected patient. Biomed Res Int. 2022;2022:4088187. https://doi.org/10.1155/2022/4088187.
Laudisio A, Marinosci F, Fontana D, et al. The burden of comorbidity is associated with symptomatic polymicrobial urinary tract infection among institutionalized elderly. Aging Clin Exp Res. 2015;27(6):805–12. https://doi.org/10.1007/s40520-015-0364-x.
Woldemariam HK, Geleta DA, Tulu KD, et al. Common uropathogens and their antibiotic susceptibility pattern among diabetic patients. BMC Infect Dis. 2019;19(1):43. https://doi.org/10.1186/s12879-018-3669-5.
Chu CM, Lowder JL. Diagnosis and treatment of urinary tract infections across age groups. Am J Obstet Gynecol. 2018;219(1):40–51. https://doi.org/10.1016/j.ajog.2017.12.231.
Acknowledgements
All authors would like to thank the Deputy of Research and Technology, Hamadan University of Medical Sciences, for their financial support in this research.
Funding
This project was financially supported by the Vice-Chancellor for Research and Technology, Hamadan University of Medical Sciences (project code: 891114026).
Author information
Authors and Affiliations
Contributions
FTA. Methodology: FTA, MA, AM. Validation: FTA, AM. Formal Analysis: AM. Investigation: FTA, MA, NR. Resources: FTA, MA. Data Curation: AM, NR. Writing—Original Draft Preparation: FTA, NR. Writing—Review and Editing: MA. Visualization: NR. Supervision: FTA, MA. Project Administration: FTA. Funding Acquisition: NR.
Corresponding author
Ethics declarations
Ethics Approval
The research followed the tents of the Declaration of Helsinki. The Ethics Committee of the Hamadan University of Medical Sciences approved this study. The institutional ethical committee at the Hamadan University of Medical Sciences approved all study protocols (IR.UMSHA.REC.1398.734).
Consent to Participate
Accordingly, written informed consent was taken from all participants before any intervention.
Consent for Publication
All authors have reviewed the final version and gave their approval for publication.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Torkamanasadi, F., Alemi, M., Rahim, N. et al. Are Empirical Treatments Compatible with the Pattern of Antibiotic Sensitivity in Urinary Tract Infections?. SN Compr. Clin. Med. 5, 155 (2023). https://doi.org/10.1007/s42399-023-01488-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01488-y