Abstract
To study the short- and long-term effects of preventive treatment in a cohort of migraine patients, enlightening possible predictive factors for ineffectiveness and also analyzing the preventive’s dropout rates, clarifying the underlying reasons. This retrospective analysis included 210 patients who received a diagnosis of migraine without aura (MO), migraine with aura (MA), or chronic migraine (CM), according to ICHD-3 diagnostic criteria, with indication for prophylactic treatment. Three groups were defined and studied regarding the efficacy of oral preventives and dropout rates: group A referred to patients treated with a first preventive, group B with a second, and group C a third, respectively. Overall efficacy of our preventive treatment was low with 40% of patients improving with their first preventive. Also, successive prophylactic attempts were associated with progressively lower rates of efficacy. Patients in whom coexisted MOH (medication overuse headache) had lower rates of preventive inefficacy. The preventive’s dropout rates observed were also high (reaching 63.2% in subgroup C patients) with adverse drug reactions such as weight gain and cognitive dysfunction being the main reason for this. The modest effect of the oral preventive drugs as well as the high proportion of patients who dropped out due to drug side events confirms that in a significant proportion of patients, oral preventives can only delay a more focused therapeutic approach such as the new therapies with monoclonal CGRP antibodies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Migraine is a common and disabling neurological condition that affects approximately 12–14% of the adults in occidental countries [1]. Despite advances in the management of headache disorders, some patients with migraine remain without symptomatic pain relief despite acute or preventive treatments [2].
Treatment should be individualized for each patient, taking into account variables such as frequency and severity of migraine episodes, trigger factors, comorbidities, patient’s lifestyle, and patient preferences [3]. To date, pharmacological care of migraine headaches includes acute therapies aimed to relieve the symptoms during the attacks and preventive therapies that aim to reduce migraine frequency, duration, or severity of attacks [4].
A preventive migraine drug is considered effective if it reduces migraine attack frequency or days by at least 50% within 3 months. Additional benefits include reduced attack duration or severity, enhanced response to acute treatments, improved ability to function, and reduced disability [5].
Currently available preventive oral drugs belong to different therapeutic classes, primarily developed for other disorders such as epilepsy, depression, or high blood pressure: topiramate, amitriptyline, propranolol, respectively (among others) [6]. Until recently, the therapeutic choice for prevention was influenced mainly by comorbidities and adverse effects. The approval of onabotulinumtoxinA (for chronic migraine prevention only) and monoclonal antibodies to calcitonin gene–related peptide or its receptor (for migraine prevention of any frequency), such as eptinezumab, fremanezumab, galcanezumab, and erenumab are options for patients with frequent migraine who have not responded to established oral medications [7, 8]. These medications target the peripheral trigeminovascular system and do not significantly penetrate the blood–brain barrier. Therefore, they are typically better tolerated than alternative treatments. However, cost and access may limit its use, and existing guidance from the American Headache Society recommends that monoclonal antibodies to calcitonin gene–related peptide or its receptor should be offered when established treatments are ineffective [9].
The indications for migraine preventive treatment have been well described: should be prescribed for patients having four or more headaches a month or at least eight headache days a month, having debilitating attacks despite appropriate acute management, difficulty tolerating or having a contraindication to acute therapy, patients with medication-overuse headache (MOH), in case of patient preference, or in the presence of certain uncommon migraine disorders where non-headache symptoms are prolonged or severe (such as hemiplegic migraine or frequent, persistent, or uncomfortable aura symptoms) [10]. However, there are still some concerns with limited efficacy, an unfavorable side effect profile and relatively low benefits of preventive treatments [11].
The available data about preventive treatment prescriptions and their efficacy in patients observed at third-level headache centers is scarce. Such data could potentially help understand the utility of available preventive drugs and the real need for new drugs for migraine prevention [12]. Numerous studies have reported real data about preventive treatment prescription for general practitioners (GPs) and neurologists. In the USA, an observational study with 43,660 migraine patients receiving different preventive drugs highlighted the main comorbidities associated with its prescription, but there are no data on specific treatments and their effects [13]. Another study, in Italy, evaluated the use of triptans in migraine patients proving that the use of triptans was significantly lower among subjects treated with oral preventive therapies than among those without these drugs, though mild improvement was present in the group with chronic migraine. This study pointed out the limitations of current preventive therapies, which, in general, has revealed low benefits and reinforces the idea that migraine patients have unmet needs [14]. A Spanish study assessed the determinants of the prescription of migraine acute or preventive therapies by 155 neurologists. It concluded that management of episodic migraine differed from chronic migraine, both in terms of neurologist treatment’s choice and in their perceived efficacy, although there is scarce evidence of the real efficacy of those treatments [15].
Also, although preventive’s failure is considered when there is a lack of efficacy or tolerability to the preventive drug, a well-accepted definition of failure is needed in clinical practice and for research [2]. There are available consensus trying to define failure to acute therapies such as triptans [16]. These definitions will be helpful in standardizing research on migraine preventive care.
The aim of this study was to determine the proportion of patients for whom preventive treatment was effective, trying to enlighten the predictive factors for ineffectiveness and also analyze the preventive dropout rates, clarifying the underlying reasons.
Subjects and Methods
Study Design
This was an observational retrospective cohort study based on data collected in a tertiary headache center—Hospital of Braga, Portugal.
Setting
All patients were asked to keep a headache diary after their first visit and to return for a follow-up visit. An example of a headache diary used by patients is reported in Fig. 2 (supplementary). The local Ethics and Health Committee of Braga’s Hospital approved the use of the electronic database.
Participants
The present data was extracted from an electronic dataset collected from October 2014 to December 2020.
We analyzed a consecutive sample of every patient followed at headache consultation in our hospital who received a diagnosis of migraine without aura (MO), migraine with aura (MA), or chronic migraine (CM), according to ICHD-3 diagnostic criteria [17]; we included those who were prescribed with a preventive treatment according to Portuguese guidelines and who had had a control visit after their first access [10]—those who abandoned the consultation after an initial assessment despite they had started on medication were excluded.
We divided our patients in 3 different subgroups.
-
> Subgroup A refers to all patients being treated with a first preventive drug—we included all the preventive drugs with level of evidence A according to Portuguese guidelines, including antidepressants (amitriptyline), beta-blockers (propranolol and metoprolol), calcium channel blockers (flunarizine), and antiepileptic drugs (topiramate and acid valproic).
-
> Subgroup B refers to patients treated with a second preventive—we did a therapeutic switch from the first preventive to a different one with evidence level A or to a preventive of evidence level B.
-
> Subgroup C refers to patients treated with a third preventive—we did a therapeutic switch from the previous second preventive to another one with evidence level A (different from the previous used drugs) or evidence level B.
Of evidence level B the following drugs were used: gabapentin, fluoxetine, or venlafaxine, mainly because of the presence of comorbid depression in those patients. Other drugs with level B or C of evidence, such as candesartan or verapamil, were not used in our analysis.
Variables
As a primary outcome measure of the effectiveness of preventive treatment, we considered the change in the frequency of headache at follow-up visit. Treatment was considered effective once it could reduce the average monthly number of headache days by 50% when compared to the average of the 3-month period previous to the beginning of medication. For all the preventive drugs, the minimum dose considered effective was reached previously to the therapeutic switch.
We analyzed the effectiveness of preventive treatment with the first, second, and third prophylactic attempts.
All patients were given suggestions to take triptans and/or NSAIDs (400–600 mg of ibuprofen) for migraine attacks. Patients with MOH were requested to replace the abused drug and to seek symptomatic therapy only in cases of severe headache while they were starting on a prophylactic drug.
As possible predictive factors for ineffectiveness of the oral preventive treatment, we considered gender, migraine onset age, frequency of the headache (episodic or chronic), the presence of aura, allodynia, and comorbidities including anxiety, depression, fibromyalgia, and MOH (Table 5).
We also measured dropout rates of the preventive treatments and analyzed the underlying reasons (Table 4). “Dropout” refers to the patients who stopped the preventive on their own decision before the subsequent visit or observation in which all outcome data are missing after a certain point.
The lack of distinction between headache and migraine days could be potentially confusing for the evaluation of the outcome; a source of potential bias is the low reliability of headache diaries (with potential lack of data about the number of migraine days in the medical diaries) and, as this was a retrospective study, the data was not collected at a fixed interval. Also we consider there is a potential bias in the choice of treatments other than those recommended as evidence level A drugs (included in the subgroups B and C), which may happen in clinical practice.
Patients with missing data for the variables considered primary and secondary outcome measures were not considered in the present analysis.
Patients under treatment with botulinum toxin or monoclonal antibodies directed against CGRP were excluded.
Statistical Analysis
X2 test was used to test 2-group differences for categorical data. Pre-defined significance levels were set to P < 0.05. Unless otherwise stated, 95% confidence intervals are given.
Statistical analyses were performed using SPSS 24.0.
Results
Patient Population
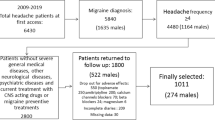
A total of 783 patients were referred to our headache consultation, 548 (70%) with a diagnosis of migraine.
Of those, 281 (51%) met the criteria to start on preventive oral treatment. After excluding those who missed the subsequent appointment, those who did not properly fulfill their diaries did not adhere to treatment and those who started on botulinum toxin or mAbs; our final sample totaled 210 patients. From those 165 patients had a diagnosis of migraine without aura (MO), 45 migraine with aura (MA), and 33 chronic migraine (CM).
The flowchart depicting patient selection is shown in Fig. 1.
Our population consisted mostly of female patients (90%) aged between 9 and 70 years, although 75% of patients were aged between 18 and 50. The average time from the onset of symptoms to the first headache appointment was 16 years (95% CI ± 14 years).
Among the 33 patients with chronic migraine (CM), 25 (76%) reported the use of more than 10 monthly doses of NSAIDs, so they received a diagnosis of medication-overuse headache (MOH) [10]. CM patients presented with older age and higher anxiety and depression scores than the other participants.
Full data of pre-treatment demographic and clinical evaluation is summarized in Table 1.
Table 2 specifies the preventives used and their relative frequency in the first, second, and third attempts at our consultation. As a first preventive treatment, patients of subgroup A only received evidence level A drugs. In the other subgroups B and C, second and third attempts, respectively, different evidence levels A or B drugs were used. The doses used varied within the range described in the table below.
Efficacy
As showed in Table 3, the first attempt of an oral preventive drug was effective in approximately 40% of our patients (n = 84) as those where the ones who noticed a reduction in the frequency of monthly headache days equal to or greater than 50% comparing to the monthly number prior to the beginning of the preventive. Of the remaining patients who did not improve after introducing the first prophylactic, almost 40% (n = 50) improved with the therapeutic switch to a second prophylactic. From the remaining 76 patients, 21% improved with the third preventive.
Therapeutic switch was performed in all patients in whom the neurologist considered that the preventive was not effective or in patients who dropout preventive therapy on their own (mainly due to their adverse effects, but also including patient perception of ineffectiveness—Table 4). In those patients who dropout their preventive treatment due to financial reasons, a switch to a lower cost prophylactic was done.
We also analyzed possible predictors of preventive inefficacy, including multiple variables shown in Table 5. We found that patients with MOH were the ones who had greater efficacy with preventive treatment.
Dropouts
Of all the patients undergoing a first preventive (subgroup A), 76 (36%) dropout. The vast majority of patients who dropped out of treatment was due to reported adverse effects (52.6%). Patient notion of ineffectiveness and also preventive’s cost were the other reasons related with dropping out of preventive treatment.
The main adverse effects reported for evidence level A preventive drugs (subgroup A) are detailed in Table 6. For the remaining drugs, anti-cholinergic effects were reported in 4 out of 8 (50%) patients treated with fluoxetine. No patients requested hospitalization.
Discussion
This observational retrospective cohort study tested the effects of preventive treatments in a population of migraine patients visiting a tertiary headache center.
The main results consisted of a mild effect of treatments on headache frequency, with less than half of the patients improved with a first preventive drug, in accord with the findings of previous studies based on indirect evidence [18].
Our impression is that most of the patients were referred to our center for medium–high frequency migraine that was previously underestimated, though in about half of the cases, patients had a clear indication to start prophylaxis.
Hospital appointments are a good opportunity for patient and family education concerning headaches but we also should invest in the expertise of general practitioners in managing these patients in an earlier phase at primary care [19]. Evaluating the response to preventive treatment should be a collaborative effort between clinicians and patients that involves the regular use of validated instruments that are reliable, convenient for use in clinical practice, and able to provide information about efficacy and helps to identify the need for adjustments, such as the headache diary (Supplementary Fig. 2).
Since comorbid medical and psychological illnesses are prevalent in patients with migraine, one must consider comorbidity when choosing preventive drugs. Topiramate followed by amitriptyline were the most prescribed drugs. The choice of topiramate as a first-line therapy was preferred for patients with chronic migraine, which is also concordant with previous studies [20].
The amitriptyline choice was also prevalent in our population, perhaps reflecting the high level of psychiatric comorbidities on our sample. Furthermore, optimal treatment of migraine and a comorbid disorder may require the use of two or more different medications [21, 22].
According to current national guidelines, venlafaxine, fluoxetine, and gabapentin have a recommendation level B, but clinicians used it in only a small number of patients, generally as a second or third choice or in case of adverse reactions to the level A prescribed drugs.
We also showed that successive attempts of preventive oral drugs were associated with progressively lower rates of efficacy (subgroups B and C), confirming that oral preventives may not be effective even in tertiary headache centers.
Patients in whom medication overuse headache (MOH) coexisted (n = 40) were those who obtain lower rates of inefficacy with preventive treatment. We believe that, as they have their own perception of relief with acute symptomatic treatment (which leads them to the abuse), they also have a perception of improvement with the preventive drug. This also may be related to the fact they frequently require regular monitoring with a closer surveillance in the subsequent appointments, perhaps facilitating adherence to treatment [23].
We would expect that fibromyalgia and allodynia as well as psychiatric comorbidities such as depression would be associated with a higher rate of inefficacy, though we did not find any association. It may be due to the fact that most of these patients were already taking an antidepressant and needed additional different therapeutic classes.
Poor adherence is recognized as a major factor impairing preventive successful therapeutic results. The main reason observed in our study related with dropping out of preventive treatment was the intolerance to drug side effects reported by patients. Low compliance was also attributed to patient perception of ineffectiveness of the prescribed drugs. Meanwhile, national hospital response time limitations may delay medical response to early drug dropouts.
Chronic migraine is defined by its high attack frequency and preventive therapy is indicated for all such patients. Patients with CM had more severe disability and higher anxiety and depression scores. A large proportion (43%) had a history of drug abuse, which is in line with the current literature [24, 25]. After the introduction of the preventive treatment, half of these CM patients remain chronic with the medication overuse due to the weak effect of preventive treatments. The results concerning chronic migraine patients should be interpreted with caution due to the small proportion of these patients.
This review has some limitations. First, relevant studies may have been missed during the literature review. Second, other comorbidities, such as hypertension or obesity, lifestyle, physical inactivity, habits, smoking, or even professions, could affect the outcome of treatments, but we decided to focus on the main clinical and demographic aspects in selected patients during their first, second, and third preventive approaches, reserving a global evaluation of these factors for further analyses. Third, the study is observational and lacks a control population, which would be useful for dissecting the effect of drugs from spontaneous evolution. Fourth we analyzed the “pain” relying on patient’s perception of pain by his calendar fulfillment (an intensity qualitative scale such as the MIDAS score was not used). Also our population consisted mostly of female patients with a disparity that may not reflect our reality worldwide.
Conclusion
The modest effect of the oral preventive drugs such as topiramate or propanolol on migraine features as well as the high proportion of patients who dropped out due to drug side events confirms that in a significant proportion of patients, oral preventives can only delay a more focused therapeutic approach such as the new therapies with monoclonal CGRP antibodies. Also, successive attempts of preventive oral drugs were associated with progressively lower rates of efficacy. Patients in whom coexisted MOH had lower rates of preventive inefficacy. Whether the migraine was episodic or chronic, the presence of psychiatric comorbidities and the drugs used to treat the migraine were not related with inefficacy of preventive treatment.
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Code Availability
Not applicable.
References
World Health Organization (WHO) Disease burden and mortality estimates. 2018
Sacco S, Braschinsky M, Ducros A, Lampl C, Little P, van den Brink AM, Pozo-Rosich P, Reuter U, de la Torre ER, Sanchez Del Rio M, Sinclair AJ, Katsarava Z, Martelletti P. European headache federation consensus on the definition of resistant and refractory migraine : developed with the endorsement of the European Migraine & Headache Alliance (EMHA). J Headache Pain. 2020;21(1):76. https://doi.org/10.1186/s10194-020-01130-5.
Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–9. https://doi.org/10.1212/01.wnl.0000252808.97649.21.
Silberstein SD, Winner PK, Chmiel JJ. Migraine preventive medication reduces resource utilization. Headache. 2003;43(3):171–8. https://doi.org/10.1046/j.1526-4610.2003.03040.x.
Silberstein SD. Preventive migraine treatment. Continuum (Minneap Minn). 2015;21(4 Headache):973–89. https://doi.org/10.1212/CON.0000000000000199.
Sprenger T, Viana M, Tassorelli C. Current prophylactic medications for migraine and their potential mechanisms of action. Neurotherapeutics. 2018;15(2):313–23. https://doi.org/10.1007/s13311-018-0621-8.
Aurora SK, Dodick DW, Turkel CC, et al. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia. 2010;30:793–803. https://doi.org/10.1177/0333102410364676.
Edvinsson L. The journey to establish CGRP as a migraine target: a retrospective view. Headache. 2015;55:1249–55. https://doi.org/10.1111/head.12656.
Ailani J, Burch RC, Robbins MS. The American Headache Society Consensus statement: update on integrating new migraine treatments into clinical practice. Headache J Head Face Pain. 2021;61(7):1021–39. https://doi.org/10.1111/head.14153.
Parreira E. Recomendações Terapêuticas Para Cefaleias da Sociedade Portuguesa de Cefaleias – 2021. Sinapse. 2021;21(supplement 1):3–100.
D’Antona L, Matharu M. Identifying and managing refractory migraine: barriers and opportunities? J Headache Pain. 2019;23:20.
Edvinsson L, Haanes KA, Warfvinge K, Krause DN. CGRP as the target of new migraine therapies - successful translation from bench to clinic. Nat Rev Neurol. 2018;14(6):338–50. https://doi.org/10.1038/s41582-018-0003-1.
Ford JH, Schroeder K, Buse DC, et al. Predicting initiation of preventive migraine medications: exploratory study in a large US medical claims database. Curr Med Res Opin. 2020;36(1):51–614. https://doi.org/10.1080/03007995.2019.1657716.
Piccinni C, Cevoli S, Ronconi G, et al. A real-world study on unmet medical needs in triptan-treated migraine: prevalence, preventive therapies and triptan use modification from a large Italian population along two years. J Headache Pain. 2019;20(1):74. https://doi.org/10.1186/s10194-019-1027-7.
García-Azorin D, Santos-Lasaosa S, Gago-Veiga AB, Viguera Romero J, Guerrero-Peral AL. Real world preventative drug management of migraine among Spanish neurologists. J Headache Pain. 2019;20(1):19. https://doi.org/10.1186/s10194-019-0971-6.
Sacco S, Lampl C, Amin FM, Braschinsky M, Deligianni C, Uludüz D, Versijpt J, Ducros A, Gil-Gouveia R, Katsarava Z, Martelletti P, Ornello R, Raffaelli B, Boucherie DM, Pozo-Rosich P, Sanchez-Del-Rio M, Sinclair A, Maassen van den Brink A, Reuter U. European Headache Federation (EHF) consensus on the definition of effective treatment of a migraine attack and of triptan failure. J Headache Pain. 2022;23(1):133. https://doi.org/10.1186/s10194-022-01502-z.
Headache Classification Subcommittee of International headache Society. The international classification of headache disorders, 2nd edition. Cephalalgia. 2004;24(Suppl. 1):24–36
De Tommaso M, Delussi M. Failure of preventive treatments in migraine: an observational retrospective study in a tertiary headache center. SSRN Electron J. 2020. https://doi.org/10.2139/ssrn.3566240.
Steiner TJ, Jensen R, Katsarava Z, et al. Aids to management of headache disorders in primary care (2nd edition): on behalf of the European Headache Federation and Lifting The Burden: the Global Campaign against Headache. J Headache Pain. 2019;20(1):57. https://doi.org/10.1186/s10194-018-0899-2.
Diener HC, Agosti R, Allais G, Bergmans P, Bussone G, Davies B, Ertas M, Lanteri-Minet M, Reuter U, Sánchez Del Río M, Schoenen J, Schwalen S, van Oene J; TOPMAT-MIG-303 Investigators Group. Cessation versus continuation of 6-month migraine preventive therapy with topiramate (PROMPT): a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2007 Dec;6(12):1054–62. https://doi.org/10.1016/S1474-4422(07)70272-7. Erratum in: Lancet Neurol. 2008 Jan;7(1):25.
Sacco S, Cerone D, Carolei A. Comorbid neuropathologies in migraine: an update on cerebrovascular and cardiovascular aspects. J Headache Pain. 2008;9:237–48. https://doi.org/10.1007/s10194-008-0048-4.
Schulman EA, Lake AE 3rd, Goadsby PJ, Peterlin BL, Siegel SE, Markley HG, Lipton RB. Defining refractory migraine and refractory chronic migraine: proposed criteria from the refractory headache special interest section of the American headache society. Headache. 2008;48:778–82. https://doi.org/10.1111/j.1526-4610.2008.01132.x.
Vandenbussche N, Laterza D, Lisicki M, Lloyd J, Lupi C, Tischler H, Toom K, Vandervorst F, Quintana S, Paemeleire K, Katsarava Z. Medication-overuse headache: a widely recognized entity amidst ongoing debate. J Headache Pain. 2018;19(1):50. https://doi.org/10.1186/s10194-018-0875-x.
Weatherall MW. The diagnosis and treatment of chronic migraine. Ther Adv Chronic Dis. 2015;6(3):115–23. https://doi.org/10.1177/2040622315579627.
Boes CJ, Capobianco DJ. Chronic migraine and medication-overuse headache through the ages. Cephalalgia. 2005;25(5):378–90. https://doi.org/10.1111/j.1468-2982.2005.00868.x.
Author information
Authors and Affiliations
Contributions
All the authors were involved in the conception of the work and the acquisition, analysis an interpretation of data. A.F and S.M. were responsible for drafting of the work, revising it critically for important intellectual content and agreement in all aspects related to the accuracy or integrity.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the local Ethics Committee—Ethics and health commission of Hospital of Braga, Portugal.
Consent to Participate
Oral informed consent for inclusion in the study were obtained from all subjects.
Consent for Publication
All authors gave written and verbal informed consent for publication.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ferreira, A., Marques, S.R., Lopes, S. et al. Preventive Oral Treatment in Migraine: Efficacy and Dropout Rates Observed at a Tertiary Headache Center. SN Compr. Clin. Med. 5, 38 (2023). https://doi.org/10.1007/s42399-022-01369-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01369-w