Abstract
To assess the utility of Patient-Based Disease Activity Score 2 (PDAS-2) in assessing the disease activity in rheumatoid arthritis (RA). A prospective cohort study was conducted on 80 patients of RA. The demographic and clinical characteristics of the patients were recorded. They were assessed for disease activity using “Disease Activity Score 28” (DAS-28), “Clinical Disease Activity Index” (CDAI), and PDAS-2 score at baseline (M0), at 2 months (M2), and at 4 months (M4) while they were on treatment. Data were analyzed for correlation of PDAS-2 with other scores and internal reliability. p<0.05 was considered for statistical significance. The mean age was 40.13 \(\pm\) 11.74 years with 70 females and 10 males. There was significant reduction in DAS-28, CDAI, and PDAS-2 score over 4-month follow-up (all scores’ p values <0.001). Internal reliability (as assessed by Cronbach’s alpha) of PDAS-2 was 0.578. PDAS-2 showed significant correlation with DAS-28 at M0, M2, and M4 (r=0.792, 0.757, and 0.669 respectively, p value <0.001) and CDAI (r=0.861, 0.832, and 0.695 respectively, p value <0.001). Overall there was a significant agreement between DAS-28 and PDAS-2 (K=0.788, p <0.001) and between CDAI and PDAS-2 (K=0.766, p <0.001). PDAS-2 score can be routinely used in clinical practice owing to its correlation with DAS-28/CDAI and because of the advantage that it assessed the patients’ daily living activities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The disease activity in rheumatoid arthritis (RA) needs regular assessment due to regular fluctuations and guidance of treatment [1]. Clinically, the physicians have the prime focus of controlling the ongoing inflammation [2], to achieve a low disease activity [3, 4].
For disease activity, the applied tools in the current scenario include DAS-28 and CDAI, which are physician dependent and outpatient department (OPD) based [5,6,7,8,9,10]. But since Indian rheumatology is too busy with time constraints, the physician gets little time to assess the disease holistically. So there is an increasing focus on patient-centered care. This has shifted the focus on the tools which are patient dependent rather than physician dependent.
Patient-reported outcome measures (PROMs) have been found to be patient-friendly, non-specific to location, and time-efficient. The domains generally considered for assessment by the patient himself are pain, physical functions, functional disability, patient’s global assessment, emotional and physical well-being, and sleep disturbances [11,12,13,14].
Previous studies on the psychometric properties of composite indices based purely on PROMs, such as Patient Activity Scale (PAS), the RADAI [11, 12], or RAPID-3 [13, 14] index, have demonstrated adequate reliability, validity, and responsiveness of these indices among patients with RA and proven them to be feasible, informative quantitative measures in busy clinical settings [12, 14]. In RA, self-monitoring of disease at home can make the patient self-aware in availing medical advice during increasing disease activity. These considerations were inculcated in the development of an index, termed Patient-Based Disease Activity Score (PDAS)15.
Earnest H. Choy et al developed and validated PDAS-1 (with ESR) and PDAS-2 (without ESR) in 2008 [15, 16]. The application of PDAS-2 without any laboratory parameter increases the feasibility of its use by the patients themselves at home [15]. However, there is a paucity of data on the correlation of DAS-28 and CDAI and PDAS-2 in RA in the Indian population. Thus, the current study was undertaken to assess the correlation of PDAS-2 with the routinely applied DAS-28 and CDAI.
Methods
The study was a prospective observational cohort study over a period of 1 year where a total of eighty patients of RA as per ACR criteria (1987) [17] and on regular treatment reporting to the Outpatient Department of Rheumatology Clinic of a tertiary care hospital, Rohtak, were enrolled. Patients with severe anemia, hypothyroidism, renal, hepatic, cardiac, or pulmonary disease were excluded. Written informed consent was obtained from all eligible patients.
Sample Size Calculation
The study of Leung et al [16] observed that correlation between DAS-28 and PDAS-2 was 0.650. Taking this value as reference, the minimum required sample size with 99% power of study and 1% level of significance is 44 patients. To reduce margin of error, total sample size taken was 80.
The detailed history and clinical examination along with relevant hematological and biochemical evaluation were done. The patients were primarily on treatment with steroids and conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) such as sulfasalazine, methotrexate, gold salts, leflunomide, and hydroxychloroquine (HCQ). No intra-articular injections or biologicals were given to the study patients. Among all patients, DAS-28, CDAI, and PDAS-2 scores were calculated (Annexure I) using the formulas:[8, 9]
where TJC is the tender joint count (range, 0–28), SJC is the swollen joint count (range, 0–28), ESR is the erythrocyte sedimentation rate in mm first hour by Wintrobe method, and GH is the general health as assessed by physician (0–100 mm) [10].
where SJC is the swollen joint count (range, 0–28), TJC is the tender joint count (range, 0–28), PGA is the patient global assessment of disease activity (on VAS, 0 to 10 cm), and EGA is the evaluator global assessment of disease activity (on VAS, 0 to 10 cm) [15].
where PGA is the patient global assessment of disease activity (0–100 mm), HAQ is the Health Assessment Questionnaire [18, 19], Patient 28 Self-SJC is the Swollen Joint Count of 28 joints as assessed by the patient him/herself (Supplementary Figure 1), and EMS is the early morning stiffness (in minute).
All subjects were on their medication and all the three mentioned scores were reassessed at baseline (M0) and at follow-up of 2 months (M2) and 4 months (M4). During the follow-up, ongoing therapy was changed according to the disease activity (CDAI scores).
Statistical Analysis
Data was collected, plotted on Microsoft excel sheet, and analyzed statistically by using SPSS software. The PDAS-2 score was compared with DAS-28, CDAI score, and with disease activity variables of DAS-28 and CDAI. Pearson correlation test was used to assess the correlation between two quantitative variables. Cronbach’s alpha test was used to check the internal consistency of the indicators used in PDAS-2. Interclass correlation coefficient was measured to assess the agreement between PDAS-2 and DAS-28/CDAI. For all tests, confidence interval was kept at 95%. Statistical significance was measured by p-value <0.05.
Results
The mean age of the study group was 40.13±11.74 years, and there were 70 females and ten males (Table 1). The mean duration of the disease was 67.5 ±57.8 months.
Assessment of Disease Activity
Disease activity was assessed using DAS-28, CDAI, and PDAS-2 score at baseline (M0), at 2-month (M2), and at 4-month (M4) follow-up (Table 2). There was a statistically significant reduction (all p values <0.001) in DAS-28, CDAI, and PDAS-2 score over 4-month duration of therapy (Table 3). This may be because of the introduction of steroids in the early phase of the treatment.
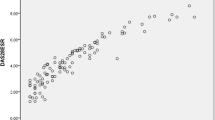
PDAS-2 score showed significant (all p-value <0.001) correlation with DAS-28 and CDAI score at M0, M2, and M4 as assessed by Pearson’s coefficient (Table 4). Cronbach’s alpha was used to calculate the internal reliability of scores. It was 0.799 for DAS-28, 0.794 for CDAI, and 0.578 for PDAS-2 score (Table 5). It was noticed that if early morning stiffness was excluded from PDAS-2, its Cronbach’s alpha value turned to be highly significant 0.757 (Table 6). To measure the agreement between disease activity categories of PDAS-2, DAS-28, and CDAI, the interclass coefficient (ICC) was used. The agreement between DAS-28 and PDSA-2 was 0.788 (p <0.001) and between CDAI and PDAS-2 was 0.766 (p<0.001) (Table 7), which is comparable to agreement between DAS-28 and CDAI, that is, 0.757 (p<0.001).
Discussion
The ongoing advancements in therapeutics require continuous upgrades in disease activity measurement tools. The present study holds strength in showing the positive correlation of PDAS-2 with the currently applied physician-centered clinical tools (DAS-28 and CDAI).
In the normal outpatient departments, it is very difficult and time consuming to assess the RA disease activity using well-known scores (e.g., DAS28, CDAI). All indices to assess disease activity in RA have some shortcomings. DAS-28 includes four variables, and it requires complex calculations like square root and logarithm. Furthermore, DAS-28, SDAI, and CDAI do not include patient functional status (Health Assessment Questionnaire (HAQ)), which is the best predictor of most severe long-term outcomes of RA.
These shortcomings are overcome with the use of PDAS-2 where the clinical symptoms of the disease are self-assessed by the patients at home. It includes all the clinical symptoms of RA like fatigue, early morning stiffness, tender joint count, and swollen joint count. In comparison to PDAS-1, PDAS-2 has the advantage of not including ESR measurement, which is a laboratory-based test [20].
In our study, PDAS-2 was significantly correlated with DAS-28 with Pearson’s coefficient 0.792, 0.757, and 0.669 and with CDAI with Pearson’s coefficient 0.861, 0.832, and 0.695 respectively at M0, M2, and M4 intervals, which is comparable to the correlation shown in study done by Earnest H choy et al (2008) [15] (between DAS-28 and PDAS-2 score was 0.76 and between CDAI and PDAS-2 score was 0.73). In our study, the agreement between DAS-28 and PDSA 2 was 0.788 (p <0.001) and between CDAI and PDAS-2 was 0.766 (p<0.001) which is comparable to agreement between DAS-28 and CDAI 0.757 (p<0.001). The study by Alexander M.H. Leung et al [16] depicted similar results (correlation between DAS-28 and PDAS-2 was 0.650, between CDAI and PDAS-2 score was 0.680, and between CDAI and DAS-28 was 0.810). In our study, the Cronbach’s alpha for PDAS-2 was 0.578. It was noticed that if early morning stiffness was excluded from PDAS-2, its Cronbach’s alpha value turned to be highly significant 0.757 suggesting a good internal consistency. In the study of Earnest H Choy et al, Cronbach’s alpha of PDAS-2 was 0.400. They also opined that early morning stiffness score can be omitted without significantly affecting the validity and sensitivity of the instrument15.
The PDAS-2 holds strength since the subjects found it very easy to fill. Subjects, by self-assessing their disease activity using PDAS-2 questionnaire, improved their overall understanding of the disease. Many of them agreed that their understanding and involvement helped optimizing medication; as using PDAS-2 they could assess disease activity on that very day; an early and prompt medical attention could be sought which is important in line of management. However, the score suffers from the limitation that it requires the patient to be well educated and with a good common sense. The ignorant behavior or the lack of understanding of the clinical assessment tool may cause an underestimation of the disease activity as well, leading to worse consequences.
Conclusion
The use of PDAS-2 may be a novel approach for RA as the other disease activity scores (DAS-28 and CDAI) assess the inflammatory part of disease objectively but do not assess the impact on the activity of daily living. Single-handed practitioners and clinicians working in an environment in which resources are limited could adopt patient-derived measures of disease activity such as the PDAS-2. It could also be used in Web-based recording of disease activity in future years. Nonetheless, it is suggested that larger and longer duration studies are needed to establish the firmness of the above correlation between PDAS-2 (PRO) and DAS-28 and CDAI (conventional method) to assess disease activity.
Availability of Data and Material
The detailed data is available on request.
Code Availability
Not applicable.
References
Marjonne CW, Creemers, Leo BA, Isenberg DA, Maddison PJ, Woo P ,et al Rheumatoid arthritis. Oxford text book of rheumatology. 3rded. New York: Oxford University Press; 2008. p. 697-710.
Wolfe F, Cush JJ, O’Dell JR, Kavanaugh A, Kremer JM, Lane NE, et al. Consensus recommendations for the assessment and treatment of rheumatoid arthritis. J Rheumatol. 2001;28:1423–30.
Fransen J, Stucki G, van Riel P. The merits of monitoring: should we follow all our rheumatoid arthritis patients in daily practice? Rheumatology (Oxford). 2002;41:601–4.
Kiely PD, Brown AK, Edwards CJ, O'Reilly DT, Ostör AJ, Quinn M, et al. Contemporary treatment principles for early rheumatoid arthritis: a consensus statement.Rheumatology (Oxford). 2009;48:765-72.
Hendrikx J, Jonge MJ de, Fransen J, Kievit W, Riel PL van. Systematic review of patient-reported outcome measures (PROMs) for assessing disease activity in rheumatoid arthritis. RMD Open 2016;2(2):e000202. Available from: https://rmdopen.bmj.com/content/2/2/e000202
Aletaha D, Landewe R, Karonitsch T, et al. Reporting disease activity in clinical trials of patients with rheumatoid arthritis: EULAR/ACR collaborative recommendations. Arthritis Rheum. 2008;59:1371–7.
Stoffer MA, Schoels MM, Smolen JS, et al. Evidence for treating rheumatoid arthritis to target: results of a systematic literature search update. Ann Rheum Dis. 2016;75:16–22.
Maska L, Anderson J, Michaud K. Measures of functional status and quality of life in rheumatoid arthritis: Health Assessment Questionnaire Disability Index (HAQ), Modified Health Assessment Questionnaire (MHAQ), Multidimensional Health Assessment Questionnaire (MDHAQ), Health Assessment Questionnaire II (HAQ-II), Improved Health Assessment Questionnaire (Improved HAQ), and Rheumatoid Arthritis Quality of Life (RAQoL). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S4-13.
Janta I, Naredo E, Martinez-Estupinan L, et al. Patient self-assessment and physician’s assessment of rheumatoid arthritis activity: which is more realistic in remission status? A comparison with ultrasonography Rheumatology (Oxford). 2013;52:2243–50. https://doi.org/10.1093/rheumatology/ket297.
Jaclyn K. Anderson, Jimmerman L, Caplan L, and Michaudk K. Measures of Rheumatoid Arthritis Disease Activity Patient (PtGA) and Provider (PrGA) Global Assessment of Disease Activity, DiseaseActivity Score (DAS) and Disease Activity Score With 28-Joint Counts (DAS28),Simplified Disease Activity Index (SDAI), Clinical Disease Activity Index (CDAI), PatientActivity Score (PAS) and Patient Activity Score-II (PASII), Routine Assessment of PatientIndex Data (RAPID), Rheumatoid Arthritis Disease Activity Index (RADAI) andRheumatoid Arthritis Disease Activity Index-5 (RADAI-5), Chronic Arthritis SystemicIndex (CASI), Patient-Based Disease Activity Score With ESR (PDAS1) and Patient-BasedDisease Activity Score Without ESR (PDAS2), and Mean Overall Index for RheumatoidArthritis (MOI-RA). Arthritis Care & Research. 2011;63:14-36.
Stucki G, Liang MH, Stucki S, Bruhlmann P, Michel BA : A self-administered rheumatoid arthritis disease activity index (RADAI) for epidemiologic research. Psychometric properties and correlation with parameters of disease activity. Arthritis Rheum. 1995;38:795-8.
Veehof MM, Ten Klooster PM, Taal E, van Riel PLCM, van de Laar MAFJ. Psychometric properties of the rheumatoid arthritis disease activity index (RADAI) in a cohort of consecutive Dutch patients with RA starting antitumor necrosis factor treatment. Ann Rheum Dis. 2008;67:789–93.
Pincus Y. Yazicy, Bergman M, Maclean R, Harrington T: A proposed continuous quality improvement approach to the assessment and management of patients with rheumatoid arthritis without formal joint counts based on quantitative routine assessment of patient index data (RAPID) scores on a multidimensional health assessment questionnaires (MDHAQ). Best Pract Res Clin Rheumatol. 2007;21:789–04.
Wolfe F, Michaud K, Pincus T. A composite disease activity scale for clinical practice, observational studies and clinical trails: the patient activity scale (PAS/PAS-2). J Rheumatol. 2005;32:2410–5.
Choy EH, Khoshaba B, Cooper D, MacGregor A, Scott DL. Development and validation of a patient-based disease activity score in rheumatoid arthritis that can be used in clinical trials and routine practice. Arthritis Rheum. 2008;59:192–9.
Alexander MH, Farewell LD, Lau CS, Ernest HS. Defining criteria for rheumatoid arthritis patient-derived disease activity score that correspond to Disease Activity Score 28 and Clinical Disease Activity Index based disease states and response criteria. Rheumatology. 2016;55:1954–8.
Aletaha D, Neogi T, Silman AJ, Funovitis J, Felson DT, Birnbaum NS, et al. Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–81.
Riazzoli J, Nilsson JÅ, Teleman A, et al. Patient-reported 28 swollen and tender joint counts accurately represent RA disease activity and can be used to assess therapy responses at the group level. Rheumatology (Oxford). 2010;49:2098–103.
Nikiphorou E, Radner H, Chatzidionysiou K, Desthieux C, Zabalan C, van Eijk-Hustings Y, et al. Patient global assessment in measuring disease activity in rheumatoid arthritis: a review of the literature. Arthritis Research & Therapy 2016;18(1):251. Available from: https://doi.org/10.1186/s13075-016-1151-6.
Pollard LC, Kingsley GH, Choy EH, Scott DL. Fibromyalgia rheumatoid arthritis and disease assessment. Rheumatology. 2010;49:924–8.
Author information
Authors and Affiliations
Contributions
Conception of work: HS, SG, HK, PY, and MK; design: HS, SG; acquisition, analysis, and interpretation of data: HK, PY, and MK; drafting of work and critical revision: HK, PY, and MK; final version for publication was approved by all authors.
Corresponding author
Ethics declarations
Ethics Approval
The ethical clearance was waived off since the study did not affect the patient outcomes.
Consent to Participate
A written informed consent was obtained from the patients before enrolling them into the study.
Written Consent for Publication
A written informed consent was obtained from the patients for publications and the authors give full consent for publication and data.
Conflict of Interest
The authors declare no competing interests.
Prior Publication
Nil
Any Previous Presentation
Nil
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Singh, H., Giri, S., Kumar, H. et al. An Observational Study on Assessment of Disease Activity in Rheumatoid Arthritis Patients Using Patient-Based Disease Activity Score 2 (PDAS-2). SN Compr. Clin. Med. 4, 1 (2022). https://doi.org/10.1007/s42399-021-01096-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-021-01096-8