Abstract
The aim of this study was to evaluate the frequency of oral mucositis in patients with hematologic malignancies and relating to the cancer treatment and chemotherapy regimen. This was a cross-sectional study with 112 patients with hematologic malignancies treated by chemotherapy. The association between oral mucositis and the variables was performed by Pearson’s chi-square test, considering a 5% error probability. The frequency of oral mucositis was low (25%). Its occurrence was associated with hematopoietic stem cell transplantation (PR = 3.33, 95% CI = 1.60–6.91) and the use of melphalan or methotrexate (PR = 5.26, 95% CI = 2.31–11.95). Some chemotherapy drugs, such as melphalan and methotrexate, are more toxic to the oral mucosa, as well as the chemotherapy regimen prior to hematopoietic stem cell transplantation. Furthermore, the low frequency of oral mucositis may be related to preventive non-pharmacological protocols, like cryotherapy during drug infusion and laser therapy. This result suggests the importance of the oral care to patients with hematologic malignancies undergoing chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mucositis is an acute inflammatory reaction of the gastrointestinal tract resulting from chemotherapy and/or radiotherapy. The lesions are commonly characterized as large, irregular, deep, and painful ulcers, often covered by a pseudomembrane and may be infected secondarily [1, 2]. The most common sites for oral mucositis are the lip mucosa, the jugal mucosa, the mouth floor, the belly, the borders of the tongue, and the oropharynx [1].
This complication has a direct impact on patients undergoing cancer treatment, as it may result in increased pain symptoms, eating difficulties, need for parenteral nutrition, and decreased quality of life [3]. Additionally, there are financial problems due to high hospital charges and treatment costs [4].
Recent studies on the pathophysiology of mucositis have helped to understand its occurrence and the development of prophylactic techniques. However, oral mucositis is very difficult to manage and so far, there is no fully effective protocol for its treatment [2]. So, this study was aimed at evaluating the frequency of oral mucositis and its relationship to the cancer treatment and chemotherapy drugs in patients with hematologic malignancies.
Methods
Study Design and Ethical Considerations
This was an observational study, conducted at a university hospital, from November 2013 to February 2016, with patients submitted to hematologic malignancy treatment. The study was approved by the Research Ethics Committee of university hospital (number 1.158.496).
Patients and Data Collection
Patients submitted to hematologic malignancy treatment, prior to or during the period of the survey and receiving professional oral care, were included. The exclusion criterion was poor general health status to perform the oral exam.
Patients who met the eligibility criteria and who agreed to participate in the study signed an informed consent form. Information about the sample (age, sex, and education level) and disease (diagnosis and treatment) was collected in the record of the hospital. The patients were submitted to oral examination to identify oral mucositis. Patients who had already been discharged from the hospital and were receiving follow-up care had the data collected by secondary sources.
Protocol of the Hospital’s Oral Care Department for Oral Mucositis Control
Cryotherapy (ice cubes applied on the oral mucosa during chemotherapy infusion) and laser therapy on the oral mucosa were performed during cancer treatment. We employed an AIGaInP laser with the following parameters: wavelength of 660 nm, power 60 mW, and energy density 5 J/cm2. We applied red laser light on all the oral mucosa, daily or on 48-h interval. The standard protocol comprises seven applications in 15 days.
Oral Health Care Assessment
Prior to cancer treatment or between cycles of chemotherapy, the patients received dietary and oral hygiene guidance and had infectious foci and dental biofilm removed. Moreover, preventive strategies were used during chemotherapy cycles for maintenance of oral health, such as daily tooth brushing and use of dental floss.
Data Analysis
The Statistical Package for the Social Sciences (SPSS) software (IBM SPSS Statistics for Windows, version 22.0, Armonk, NY: IBM Corp.) was used for statistical analysis of the data. Descriptive statistics was carried out to characterize the distribution of sociodemographic factors, the hematologic disease, and the cancer treatment modality as well as the frequency of oral mucositis and chemotherapy drugs used in these patients. The chi-square test was used for analysis of categorical data. Univariate analysis was performed to describe the likelihood of patients undergoing melphalan or methotrexate treatment to present oral mucositis compared with patients undergoing other chemotherapy regimen. Also, this analysis was performed to compare the oral mucositis frequency between patients undergoing hematopoietic stem cell transplantation (HSCT) or other therapies. For all analyses, the level of significance was set at < 0.05.
Results
Considering the eligibility criteria, the sample was composed of 112 patients with hematologic malignancies. Twenty-four data were collected by means of secondary sources.
Table 1 shows characteristics related to sociodemographic factors, hematologic disease, cancer treatment modality, and chemotherapy regimen, as well as the frequency of oral mucositis. The ages varied between 15 and 85 years old, mean of 41.08 (± 17.26) years old, with a discrete predominance of the 43- to 54-year-old group. Of the 72 patients who provided information about educational level, there was a prevalence of patients with up to 8 years of schooling, followed by patients between 9 and 11 years (Table 1).
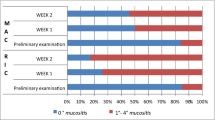
Concerning the oncologic disease, acute leukemia and multiple myeloma were the most frequent. Regarding the cancer treatment, most patients were submitted to treatments other than HSCT. Only 28 subjects (25%) had oral mucositis and 46 (41.1%) used melphalan or methotrexate (Table 1).
Table 2 shows the association between the cancer treatment and the chemotherapy drugs used and the frequency of oral mucositis. There was a statistically significant association between these variables (p ≤ 0.05). Hematologic malignancy patients who underwent HSCT had more oral mucositis than those did not submitted (PR = 3.33, 95% CI = 1.60–6.91). Similarly, hematologic malignancy patients who used melphalan or methotrexate had more oral mucositis than those who used other chemotherapy drugs (PR = 5.26, 95% CI = 2.31–11.95).
Discussion
The results showed that the frequency of oral mucositis in the studied population was low (25% of the sample), compared with other studies. Scully et al. [5] sustain that at least 40 to 70% of the patients treated with chemotherapy are likely to have oral mucositis. In the study carried out by Rodrigues et al. [6], 93.6% of the patients with multiple myeloma, who underwent chemotherapy with melphalan, showed some degree of oral mucositis. The results of Ramírez-Amador et al. [7] found 41.37% of oral mucositis in patients with leukemia.
A possible explication for our results is the oral care provided to patients of this study. Laser therapy and cryotherapy were the protocols adopted for the prevention of oral mucositis at the institution. These protocols are based on scientific evidence showing a reduction in the frequency and severity of oral mucositis when these associated therapies are used, prior to the onset of chemotherapy [8,9,10,11,12,13].
Prevention of oral mucositis can be explained by laser therapy mechanism of action, based on the absorption of visible and near-infrared monochromatic radiation by components of the electron respiratory chain, increasing cell metabolism and its resistance to damage caused by chemotherapy drugs [14,15,16,17,18]. Oral cryotherapy promotes vasoconstriction by reducing blood flow in the oral cavity and, consequently, the amount of chemotherapy delivered to oral tissues [19, 20].
The oral mucositis is the major cause of painful symptomatology during the chemotherapy, which may lead to oral feeding difficulties, requiring the use of parenteral nutrition or even the interruption of the antineoplastic treatment [7]. Therefore, preventing oral mucositis diminishes suffering and improves better quality of life for these patients. Consequently, health costs are reduced due to fewer comorbidities, fewer opioids, shorter length of hospital stay, and less need for parenteral nutrition [3, 8].
We also observed that the occurrence of oral mucositis was associated with HSCT and the use of melphalan or methotrexate. Regarding the association between HSCT and the occurrence of oral mucositis, our study showed that patients who were submitted to HSCT were more likely to develop oral mucositis in comparison to those who were not submitted to this therapy, although the preventive protocol was used. This can be explained because the conditioning regimen prior to HSCT is intense and the patient’s immune recovery is slow, leading to the development of adverse effects, such as vomiting, diarrhea, and oral complications [21]. However, studies using laser therapy and oral cryotherapy have shown a reduction in the severity and painful symptoms of oral mucositis in patients submitted to HSCT [22, 23]. Therefore, even if mucositis develops clinically, these therapies are fundamental to improve quality of life during HSCT.
Additionally, the incidence and severity of oral mucositis depend on the type of HSCT. The study conducted by Vagliano et al. [1] showed that adults undergoing allogeneic HSCT had 2.88-fold higher risk of developing severe mucositis than those submitted to autologous HSCT. Also, subjects who underwent allogeneic transplantation and who used methotrexate for prophylaxis of graft-versus-host disease (GVHD) had a higher incidence and severity of mucositis when compared to those who did not use methotrexate as prophylaxis for GVHD [21].
In our study, it was not possible to determine the HSCT modality performed (autologous or allogeneic). However, it is believed that most patients were submitted to autologous HSCT, since this is more commonly performed at this hospital. This also would explain the low frequency (25%) of oral mucositis in the evaluated sample.
Regarding the association between oral mucositis and the use of melphalan or methotrexate during the antineoplastic treatment, we observed that patients who used these chemotherapy drugs were more likely to develop mucositis compared to those who used other chemotherapy regimen. Methotrexate is a specific drug of the S phase of the cell cycle and inhibits the synthesis of DNA. Acting in this phase, this drug has more toxic effects on oral mucosa, and therefore, it has been associated with the development of oral mucositis, especially in high doses (> 1 g/m2) [24,25,26,27]. Also, some studies suggest that this drug is secreted in the saliva, which may increase its toxicity in the oral mucosa [26, 27]. Melphalan is cycle-non-specific alkylating drug that causes changes in the DNA chain and prevents its replication. It is also associated with the development of mucositis, especially at high doses (> 140 mg/m2) [24, 27]. This high dose is used in the conditioning regimen for autologous HSCT as a single agent or in combination with other chemotherapy drugs [28].
In our study, leukemia and multiple myeloma were the most frequent hematologic malignancies, which are treated with chemotherapy protocols including methotrexate [24] and melphalan [28], respectively. Therefore, it is important to emphasize that the dentist should perform interventions that prevent oral mucositis in patients who will undergo chemotherapy protocols that include high doses of methotrexate (CODOX-M, FLAMSA, or HyperCVAD cycles) and melphalan (BEAM chemotherapy) and when a chemotherapy drug is used as a sole agent in the conditioning regimen for autologous HSCT.
Regarding research limiting factors, this was a cross-sectional study; therefore, we were careful not to infer causal relations due to the difficulties in establishing the temporal association between outcome and exposure. Furthermore, data collected from secondary sources did not yield complete information about the HSCT modality performed.
Conclusions
In conclusion, this study showed that melphalan and methotrexate, as well as HSCT with a conditioning regimen, are associated with the development of oral mucositis. The low frequency of oral mucositis may be related to the non-pharmacological preventive protocols performed in these patients, reinforcing the importance of the dentist in the health team.
Data Availability
Not applicable.
References
Vagliano L, Feraut C, Gobetto G, Trunfio A, Errico A, Campani V. Incidence and severity of oral mucositis in patients undergoing haematopoietic SCT—results of a multicentre study. Bone Marrow Transplant. 2011;46:727–32.
Sonis ST. Oral mucositis. Anti-Cancer Drugs. 2011;22:607–12.
Antunes HS, Schluckebier LF, Herchenhorn D, Pequena IA, Araújo CM, Viégas CM. Cost-effectiveness of low-level laser therapy (LLLT) in head and neck cancer patients receiving concurrent chemoradiation. Oral Oncol. 2016;52:85–90.
Mccullough RW. US oncology-wide incidence, duration, costs and deaths from chemoradiation mucositis and antimucositis therapy benefits. Future Oncol. 2017;13:2823–52.
Scully C, Epstein J, Sonis S. Oral mucositis: a challenging complication of radiotherapy, chemotherapy, and radiochemotherapy: part 1, pathogenesis and prophylaxis of mucositis. Head Neck. 2003;25:1057–70.
Rodrigues GH, Jaguar GC, Alves FA, Guollo A, Camandoni VO, Damascena AS, et al. Variability of high-dose melphalan exposure on oral mucositis in patients undergoing prophylactic low-level laser therapy. Lasers Med Sci. 2017;32:1089–95.
Ramírez-Amador V, Anaya-Saavedra G, Crespo-Solís E, Camacho EI, González-Ramirez I, Ponce de Leon S. Prospective evaluation of oral mucositis in acute leukemia patients receiving chemotherapy. Support Care Cancer. 2010;18:639–46.
Ethier MC, Regier DA, Tomlinson D, Judd P, Doyle J, Gassas UM, et al. Perspectives toward oral mucositis prevention from parents and health care professionals in pediatric cancer. Support Care Cancer. 2012;20:1771–7.
Bezinelli LM, Eduardo FDP, Marques R, Biazevic MG, De Paula EC, Correa G, et al. Cost-effectiveness of the introduction of specialized oral care with laser therapy in hematopoietic stem cell transplantation. Hematol Oncol. 2013;32:31–9.
Zecha JA, Raber-Durlacher JE, Nair RG, Epstein JB, Elad S, Hamblin MR. Low-level laser therapy / photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer : part 2 : proposed applications and treatment protocols. Support Care Cancer. 2016;24:2793–805.
Lalla RV, Bowen J, Barasch A, Elting L, Epstein J, Keefe DM, et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer. 2014;120:1453–61.
Eduardo FDP, Bezinelli LM, Marques R, Nascimento-Sobrinho JJ, Hamerschlak N, Correa L. Efficacy of cryotherapy associated with laser therapy for decreasing severity of melphalan-induced oral mucositis during hematological stem-cell transplantation : a prospective clinical study. Hematol Oncol. 2015;33:152–8.
Rozza-de-Menezes R, Souza PHC, Westphalen FH, Ignácio SA, Moysés ST, Sarmento VA. Behaviour and prevention of 5’fluorouracil and doxorubicin-induced oral mucositis in immunocompetent patients with solid tumors: a randomised trial. Oral Heal Prev Dent. 2018;16:549–55.
Zecha JA, Raber-Durlacher JE, Nair RG, Epstein JB, Elad S, Hamblin MR. Low level laser therapy / photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer : part 1 : mechanisms of action, dosimetric, and safety considerations. Support Care Cancer. 2016;24:2781–92.
Freire MRS, Almeida D, Santos JN, Sarmento VA. Evaluation of bone repair after radiotherapy by photobiomodulation-an animal experimental study. Laser Phys. 2011;21:958–64.
Freire M, do RS FR, Colombo F, Valença A, Marques AM, Sarmento VA. LED and laser photobiomodulation in the prevention and treatment of oral mucositis: experimental study in hamsters. Clin Oral Investig. 2014;18:1005–13.
Da Cunha SS, Sarmento V, Ramalho LMP, De Almeida D, Veeck EB, Da Costa NP. Effect of laser therapy on bone tissue submitted to radiotherapy: experimental study in rats. Photomed Laser Surg. 2007;25:197–204.
Almeida SV, Aparecida M, Cordeiro M. The low-intensity laser photobiomodulation in the management of oral mucositis : report of cases. Arch Oral Sci Res. 2012;1:205–9.
Wang L, Gu Z, Zhai R, Zhao S, Luo L, Li D, et al. Efficacy of oral cryotherapy on oral mucositis prevention in patients with hematological malignancies undergoing hematopoietic stem cell transplantation: a meta-analysis of randomized controlled trials. PLoS One. 2015;10:1–12.
Riley P, Glenny AM, Worthington HV, Littlewood A, Clarkson JE, Mccabe MG. Interventions for preventing oral mucositis in patients with cancer receiving treatment : oral cryotherapy ( Review ). Cochrane Database Syst Rev. 2015:1–98.
Weissheimer C, Curra M, Gregianin LJ, Daudt LE, Wagner VP, Martins MAT, et al. New photobiomodulation protocol prevents oral mucositis in hematopoietic stem cell transplantation recipients-a retrospective study. Lasers Med Sci. 2017:1–9.
Salvador DRN, Soave DF, Sacono NT, De Castro EF, Silva GBL, E Silva LP. Effect of photobiomodulation therapy on reducing the chemo-induced oral mucositis severity and on salivary levels of CXCL8/interleukin 8, nitrite, and myeloperoxidase in patients undergoing hematopoietic stem cell transplantation: a randomized clinical tr. Lasers Med Sci. 2017:1–10.
Zadik Y, Arany PR, Fregnani ER, Antunes HS, Bensadoun RJ, Gueiros LA. Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. 2019;27:3969–83.
ATJDL B. Harrison’s manual of oncology. 2008. https://doi.org/10.1016/j.ijrobp.2008.03.023.
Whitehead VM, Shuster JJ, Vuchich MJ, Mahoney DH Jr, Lauer SJ, Pagamento C, et al. Accumulation of methotrexate and methotrexate polyglutamates in lymphoblasts and treatment outcome in children with B-progenitor-cell acute lymphoblastic leukemia: a Pediatric Oncology Group study. Leukemia. 2005;19:533–6.
Naidu MUR, Ramana GV, Rani PU, Mohan IK, Suman A, ROY P. Chemotherapy-induced and/or radiation therapy-induced oral mucositis-complicating the treatment of cancer. Neoplasia. 2004;6:423–31.
Epstein JB, Thariat J, Bensadoun RJ, Barasch UM, Murphy BA, Kolnick G, et al. Oral complications of cancer and cancer therapy : from cancer treatment to survivorship. Cancer J Clin. 2012;62:400–22.
Batlle M, Morgades M, Vives S, Ferrà C, Oriol A, Sancho JM, et al. Usefulness and safety of oral cryotherapy in the prevention of oral mucositis after conditioning regimens with high-dose melphalan for autologous stem cell transplantation for lymphoma and myeloma. Eur J Haematol. 2014;93:487–91.
Code Availability
Not applicable.
Author information
Authors and Affiliations
Contributions
Viviane Almeida Sarmento conceived the study and was in charge of overall direction and planning. Davi Silva Carvalho Curi drafted the manuscript with support from Mrs. Sarmento. Thaiane Dantas Dias dos Santos carried out the experiment. Renata Portela de Rezende carried out the experiment. Liliane Lins-Kusterer supervise the project and contributed to the analysis of the results. Patrícia Leite-Ribeiro helped supervise the project and contributed to the final version of the manuscript. All authors have contributed to the manuscript in significant ways, and they have reviewed and agreed upon the manuscript content.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the Research Ethics Committee of university hospital (number 1.158.496). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no conflict of interest.
The authors confirm that this work is original and has not been published elsewhere, nor is it currently under consideration for publication by another journal in either electronic or printed version.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Sarmento, V.A., Curi, D.S.C., dos Santos, T.D.D. et al. Oral Mucositis in Patients with Hematologic Malignancies Undergoing Chemotherapy. SN Compr. Clin. Med. 3, 2149–2153 (2021). https://doi.org/10.1007/s42399-021-01000-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-01000-4