Abstract
Toxoplasmosis is a parasitic disease usually in adults without clinical symptoms. Toxoplasmosis is caused by Toxoplasma gondii when exposed to infected cat feces, polluted soil, and water or uncooked meat. This study aimed to use chitosan nanogel (CsNg) to load Nepeta cataria essential oils (NCEO) to improve the effectiveness of its antiparasitic properties. CsNg was prepared by sol–gel method using sodium tripolyphosphate (TPP) as a linking agent. NCEO was characterized using GC–MS analysis and structural studies of NCEO-CsNg were carried out by FTIR, SEM, and DLS techniques. After that, anti-Toxoplasma activity of NCEO-CsNg, NCEO, CsNg, and spiramycin (Spn, positive control) were examined ex vivo and in vivo on the infected Balb/c mice. According to the GC–MS profile, major bioactive compounds of NCEO were nepetalactone (64.58%), caryophyllene oxide (4.31%), 1,8-cineole (3.86%), and crypton (3.46%). SEM exhibited successful entrapment of NCEO into CsNg as the morphology and size of CsNg changed. FTIR confirmed the presence of NCEO functional groups incorporated into porous CsNg. Toxoplasma inhibition of NCEO-CsNg, NCEO, CsNg, and spiramycin occurred in 75, 40, 200, and 30 µg/ml, respectively, for 60-min in vitro exposure. In vivo challenge assay experiment showed that maximum survival time was 10 and 9 days for those infected mice treated with NCEO-CsNg and spiramycin and the least was 6 for the untreated group (negative control). The results concluded that NCEO-CsNg has potential use as an antiparasitic agent in animals and humans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Toxoplasmosis is a zoonotic parasitic disease caused by Toxoplasma gondii from Apicomplexa phylum. The severity of the disease often depends on the immune response of the host. Toxoplasma can remain latent in brain and muscular tissues for a long time [1]. Therefore, those patients with impaired immune systems may be at risk for a fatal form of the disease. Human infection with Toxoplasma gondii can occur by consuming contaminated meat, dairy products and by ingesting water, soil, vegetables containing oocysts. Congenital transmission of Toxoplasma to the fetus is one of the most serious types of disease, leading to adverse consequences [2]. Toxoplasmosis treatments include the use of dihydrofolate reductase (DHFR) inhibitors, including pyrimethamine (PYR). Common treatments for toxoplasmosis include the use of dihydrofolate reductase (DHFR) inhibitors, including pyrimethamine (PYR). Although these drugs are effective against the active tachyzoites form of Toxoplasma, they are unable to inhibit bradyzoites and sporozoites. Therefore, a combination formula of trimethoprim and sulfamethoxazole is often recommended against T. gondii infections. However, one of the main challenges in combination therapy is the emergence of complications such as bone marrow suppression and renal dysfunction [3]. Therefore, the priority in efficient treatment against toxoplasmosis is to find new drugs with minimal side effects. Today, herbal metabolites are known as valuable alternatives for treating many infectious diseases [4]. Various plant-derived essential oils from Mentha piperita, Thymus vulgaris, Origanum vulgare, Ocimum basilicum, Laurus nobilis, Nigella sativa, Petroselinum crispum, and Rosmarinus officinalis have been used against microbial and fungal pathogens [5,6,7].
The antiparasitic activity of herbal metabolites has been investigated in numerous studies. In this regard, the essential oils of Mentha pulegium, Cinnamomum zeylanicum, Origanum vulgare, Curcuma longa, and Rosmarinus officinalis have been used against Leishmania [8,9,10]. Nepeta is one of the valuable medicinal plants belonging to the Lamiaceae family, widely used in traditional medicine. This genus is the closest subfamily Nepetoideae to the tribe Mentheae. This plant contains 280 species mostly used in pharmaceutical, food, and some ornamental plants [11]. Some species belonging to the genus Nepeta in traditional medicine are antibacterial, antifungal, antiseptic, anti-inflammatory, antioxidant, insect repellent, sedative, cholesterol-lowering, sedative, anti-asthma, analgesic, diuretic, antiseptics, antipyretics, and herbicides [12].
Currently, nanomaterial-based drug formulations, such as nanohydrogels, are being developed [13]. Encapsulation of bioactive compounds and drugs can prolong their release, which directly affects their activity and stability [14, 15]. Cs is a carbohydrate polymer with low toxicity for medical applications. Cs-based nanohydrogels form porous composites, encapsulating hydrophobic compounds such as essential oils, thus increasing the bioavailability and stability of these drugs in the body. Recently, Cs nanoparticles and their derivatives have been used in numerous studies as drug delivery systems [16]. In this research, a Cs-based nanogel was fabricated by the sol–gel method for loading the NCEO and then evaluating its anti-Toxoplasma activity. For this, firstly, the nanogels’ physicochemical properties and cytotoxicity were then examined. Finally, it was evaluated for anti-Toxoplasma activity in vitro and in vivo.
2 Materials and methods
2.1 Materials, parasite, and cell line preparation
Chitosan powder (Cs, medium molecular weight) and tripolyphosphate (TPP) were bought from Sigma Co (USA). Nepeta cataria was purchased from a local market in Khorramabad, Lorestan Province, Iran. Characterization was carried out in the phytochemistry section of Razi Herbal Medicines Research Center. The Vero cell line was prepared from the cell collection of Pasture Institute, Tehran, Iran.
2.2 Animal studies permission
Animal experiments were performed according to animal ethics permission with code: IR.LUMS.REC.1398.272 from the animal ethics committee of Lorestan University of Medical Sciences. All experiments were carried out based on the standard protocols for the care and use of laboratory animals. In this study, 60 male BALB/C mice (50–60 days aged) were used for all experiments purchased from the Pasteur Institute of Iran. Thirty mice were used for tissue analysis. Another 30 mice were used to evaluate the infection challenge assay for the survival time of the mice.
2.3 Extraction and characterization of N. cataria essential oil (NCEO)
To extract the NCEO, the hydrodistillation method was applied using a Clevenger apparatus. Phytochemical compositions of NCEO were identified by GC–MS analysis. For this, a GC–MS system was Agilent 6890 N GC apparatus coupled with Agilent 5973 MSD operating in electron ionization (EI) mode at 70e, fitted with an HP-5 column (30 m × 0.25 mm, i.d., film thickness, 0.25 µm) and SPB-1 column (30 m × 0.25 mm, i.d., film thickness, 0.25 µm). The column temperature was adjusted from 35 to 240 °C with the 2 °C/min scanning time and finally kept at 230 °C for 30 min. The injector and interface temperatures were programmed at 250 °C. Carrier gas (helium) was adjusted to a constant flow rate of 0.9 ml/min. The NCEO components were identified based on the NIST GC retention data webbook and Wiley 7 n/NIST05 mass spectra libraries.
2.4 NCEO loading in Cs-based nanogel (NCEO-CsNg)
The NCEO-CsNg were constructed as described aforementioned [17]. Briefly, 0.6 g of chitosan was added to 50 ml of distilled water containing 1% glacial acetic acid. After 1 h, 200 µl of Tween-20 was added to the solution mixture and stirred at 60 °C for 1 h. The crude NCEO was gently dropped into the stirring mixture. The most efficient formulation was obtained by a set of NCEO concentrations including 100, 150, 200, 250, 350, and 500 µg per 50 ml of 1.2% chitosan. A volume of 20 ml of tripolyphosphate (TPP) solution (1% w/v) was drop-wisely added into the mixture and stirred for 1 h. After that, the synthesized nanogel was separated by centrifugation at 10,000 rpm for 15 min at 4 °C. Finally, nanogel was washed by distilled water and dispersed in phosphate buffer solution (PBS) until performing experiments. Figure 1 represents a graphical schematic of Cs-nanogel fabrication along with the NCEO encapsulation.
2.5 Structural analyses of NCEO-CsNg
The formation of NCEO-CsNg was studied using analytical instruments. Morphological studies were performed by scanning electron microscopy (SEM) images that were prepared using a Fe-SEM (TESCAN, MIRA3, Czech Republic). The size distribution of CsNg and NCEO-CsNg was determined by dynamic light scattering (DLS) on Malvern 4700 PS/MW instrument. Fourier transform infrared spectra were conducted using an FTIR spectrometer (Thermo Nicolet AVATAR, USA) from 4000 to 400 cm−1 with a resolution of 4 cm−1 [17].
2.6 Loading and release study of NCEO-CsNPs
Amounts of the NCEO loaded into CsNg were quantified in terms of the presence of nepetalactone as the major component of NCEO. This measurement was carried out during the synthesis of NCEO-CsNg with different ratios of the formulation compartment. After the centrifugation of synthesized NCEO-CsNg, the unloaded NCEO was determined into the supernatant through spectrophotometric absorbance at 228 nm. Loading efficiency was determined with the following equation [13]:
where C0 and Cs are the initial concentration of NCEO and unloaded NCEO in the supernatant, respectively.
The release kinetics were examined in the normal saline (NS) to simulate in vitro release of NCEO from CsNg. A mass of 20 mg of NCEO-CsNg was placed in a dialysis bag with a cut-off molecular weight of 14 kDa and submerged in the NS under constant stirring at room temperature. The amount of NCEO released out of the dialysis bag was determined using a spectrophotometer at 228 nm at a certain regular time as described by Cai et al. based on the presence of nepetalactone derivatives [18]. Finally, the cumulative amount of the released was calculated by the following equation:
where Mt and M0 are the cumulative weight of NCEO at the time interval sampling and the initial amount of the NCEO loaded in the CsNg, respectively.
2.7 Cytotoxicity assay of NCEO-CsNg
Cytotoxicity of all used formulations was examined on the Vero cell line as described by Danielson et al. [19]. For this, different doses of NCEO, NCEO-CsNg, and Cs at 10–500 µg/ml, along with spiramycin at 30 µg/ml as a positive control, were used. Briefly, Vero cells (105 cells per well) were cultured in 96-well plates containing DMEM (Invitrogen, Carlsbad, CA) supplemented with 10% FBS (TaKaRa, Japan) and 1% penicillin/streptomycin (BioBasic Inc, Canada) and incubated at 37 °C under a humidified atmosphere in 5% CO2 until reached 70% confluency. After that, different doses of each formulation were added to the wells and incubated at 37 °C for 8 h in 5% CO2. The cytotoxicity was measured by adding 10 µl (5 mg/ml) of MTT solution (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) to the wells and incubated for 4 h. Next, the process was stopped and 100 µl DMSO was added to each well to dissolve precipitated dye [10]. The absorbance of the wells was determined using a microplate reader at 590 nm. The viable cells were determined using Eq. 2 and IC50 of each formulation was calculated using the GraphPad Prism 8.0.1 software (San Diego, USA).
2.8 T. gondii RH strain preparation
T. gondii RH-type was gifted from the Department of Parasitology, School of Medicine, Lorestan University of Medical Sciences. T. gondii RH-type tachyzoites were revived by injecting intraperitoneally in Balb/c mice. To separate active tachyzoites, the infected mice were sacrificed and their peritoneal fluid was taken and washed three times with normal saline. The count of tachyzoites was determined by a hemocytometer after staining with trypan blue dye [7].
2.9 Intracellular anti-Toxoplasma of NCEO-CsNg
The effect of NCEO-CsNg (75 µg/ml), NCEO (40 µg/ml), Cs (200 µg/ml), and spiramycin (30 µg/ml) against Toxoplasma-infected Vero cells were examined. For this, 105 cells were seeded in a 96-well plate containing DMEM supplemented with 10% FBS. After reaching 70% confluency, 105 active tachyzoites were added to the grown cells and the plate was incubated at the same conditions for 24 h. To ensure maximum tachyzoite infection, the cells were monitored under a reverse light microscope. After that, extracellular tachyzoite and other contaminants were removed from the wells by removing the culture medium and washing with sterile PBS. The cells were then treated with formulations at certain doses in DMEM supplemented with 10% FBS and incubated at 37 °C for 48 h. Finally, cell viability was assessed by MTT assay as described previously. The therapeutic efficacy was calculated as follows [20]:
where At and Au are absorbance intensity related to treated infected cells and untreated infected cells, respectively.
2.10 Ex vivo anti-Toxoplasma activity of NCEO-CsNg
The effects of different formulations were studied on Toxoplasma tachyzoites in a 96-well plate containing DMEM supplemented with 10% FBS. For this, 105 parasites were added to each well and treated with one dose of NCEO-CsNg (75 µg/ml), NCEO (40 µg/ml), or CsNg (200 µg/ml). Spiramycin was selected as a positive control at 30 µg/ml. After 2-h incubation, vital tachyzoites were counted using a hemocytometer slide after trypan-blue staining. Mortality percent was determined by the following equation [21]:
2.11 In vivo anti-Toxoplasma activity of NCEO-CsNg
2.11.1 Challenge assay and survival study
The anti-toxoplasmosis efficacy of all formulations was studied on male BALB/c mice aged 50–60 days and weighing about 20–25 g. Sixty mice were randomly divided into 6 groups (n = 10), which included groups treated with NCEO-CsNg, NCEO, CsNg, and spiramycin. The two groups were considered as positive and negative controls. Five groups were infected intraperitoneally with 100 μl sterile PBS containing 2500 active tachyzoites of T. gondii RH strain and only one group was considered as uninfected control. After 4 h, all treatments were prepared in sterile PBS as calculated by IC50 and then adjusted based on reported LD50 in literature [22, 23]. Therefore, administrated doses of NCEO-CsNg, NCEO, and CsNg were administrated as 75, 40, and 200 µg per mouse, respectively. Spiramycin (300 µg/ml/mouse) was administered orally and control groups (positive and negative) received no treatment [24]. The mice were housed in standard conditions according to the protocol of the Animal Care and Ethics Committee. During the treatments, daily monitoring was performed and the survival rate was calculated based on the following equation:
2.11.2 Monitoring of tachyzoites in tissues
According to the previous experiment, 30 mice were divided into 6 groups. Mice infected with tachyzoite and treated with the formulations were sacrificed on the fifth day. After that, tissue samples such as liver and spleen were taken. Also, peritoneal tachyzoites were harvested and counted. For visualization and counting, tissue smears were prepared on glass slides and stained using Giemsa solution (5%). Enumeration was performed based on the mean parasite numbers on the 5 different fields under the light microscope.
2.12 Statistical analyses
Statistical analyses were performed based on at least triplicates and differences between groups were determined by one-tail ANOVA with significant distances of p value < 0.05.
3 Results and discussion
3.1 Characterization of NCEO chemical compositions
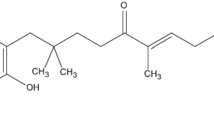
Table 1 represents the GC–MS profile of NCEO. Thirty compounds were characterized in the NCEO in which major compounds were nepetalactone (64.58%), caryophyllene oxide (4.31%), 1,8-cineole (3.86%), and then crypton (3.46%). Studies have indicated that bioactive metabolites present in Nepeta species potential activity against various pathogens such as bacteria, fungi, and parasites. Giarratana et al. reported that NCEO possessed significant inhibition against various helminths such as Anisakis, Contraceacum, Pseudoterranova, and Hysterothylacium [25]. Furthermore, the major compounds of NCEO, namely, nepetalactone and β-caryophyllene derivatives, were found to have broad-spectrum inhibition against human and phytopathogenic bacteria and fungi [26,27,28,29]. According to the study of Portapilla et al., β-caryophyllene oxide derivatives could inhibit malaria infection caused by especially Trypanosoma cruzi [30]. As it turned out, the majority of the compounds in NCEO are nepetalactone and β-caryophyllene derivatives. As a result, the biological properties of NCEO can be attributed to these compounds.
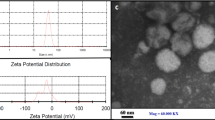
3.2 Characterization of NCEO-CsNg
The morphological characteristics and particle size distribution of NCEO-CsNg were analyzed by SEM and DLS techniques. As shown in Figs. 2a and b, the CsNg surface is rough, whereas with NCEO entrapment, the CsNg surface appears to be smoothed. Particle size distribution of CsNg and NCEO-CsNg can be seen in Fig. 2c and d. Based on the measurements, CsNg showed a Z-average of 64.39 nm, while the size of NCEO-loaded CsNg possessed an average size of 69.65 nm in diameter. The mean size of CsNg was increased with the loading of NCEO content. Since the DLS technique measured the particle size in an aqueous solution, Z-average obtained was higher than the particle size measured via SEM images. As stated in studies, polymeric hydrogels in an aqueous phase swelled and their hydrodynamic diameter was significantly increased. However, the hydrodynamic diameter of the Ng systems could affect by the hydrophobicity of the NCEO content. Therefore, entrapment of the hydrophobic molecules into the polymeric hydrogels might condense the hydrogel structure. Here, the diameters of CsNg compared with NCEO-loaded CsNg showed no significant increase due to the NCEO entrapment into the CsNg structure caused increasing the CsNg condensation [17]. The shift of the polydispersity index (PDI) from 0.385 to 0.562 with the incorporation of NCEO into porous CsNg caused a reduction in monodispersity of the NPs and then slightly increased in Z-average, indicating the condensation of the size dimension of NPs [15].
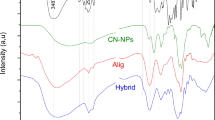
3.3 FTIR analysis of NCEO-CsNg
FT-IR spectra of CsNg, NCEO, and NCEO-CsNg showed the possible functional groups involved in the formation of NCEO-loaded CsNg. As seen in Fig. 3, CsNg appeared specific peaks at 3492 cm−1, corresponding to OH and N–H stretching bands and a stretching band was observed at 2925 cm−1 relating to the absorption of aliphatic C–H symmetric peaks. Also, a specific peak at 889 cm−1 confirms the presence of glucose ring. The presence of the new bending bands at 1633 and 1254 cm−1 could be related to the electrostatic linking between amid II (NH2) and polyphosphate (P–O) groups from Cs and TPP [31]. Loading of NCEO in CsNg resulted in a significant shift and intensity in some peaks, such as an increase of C–H stretching peak at 2950 cm−1 and the appearance of the carboxylic bond at 2097 cm−1, attributing to the presence of NCEO functional groups [32].
3.4 Loading and release study of NCEO-CsNPs
The loading efficiency of NCEO in CsNg was examined based on the change of NCEO concentration that maximum capacity of the CsNg was estimated to be 68% of 200 µl initial concentration. The release rate of NCEO from CsNg was determined at a regular interval of 10 min for 2 h. As seen in Fig. 4, about 60% of loaded NCEO was released at 30 min. After that, the release reached stable release status. The total amounts of released NCEO were found to be about 77%.
The release rate of NCEO from CsNg could be affected by multiple parameters, including loading capacity and hydrophobic interactions between the essential oil and Cs porous structure. As stated in some literature, the release kinetics could be directly affected by the swelling and degradation of the compacted Cs-TPP hydrogel [17, 33, 34]. Our results indicated that the chitosan-TPP complex could control the release of NCEO. Hence, such releasing pattern could be desirable to increase the formulation’s antiparasitic efficacy and decrease the cytotoxicity of NCEO on the host cells.
3.5 Intracellular anti-Toxoplasma activity of NCEO-CsNg
To examine the effects of NCEO and NCEO-CsNg against the intracellular infection of T. gondii, cytotoxicity of the drug formulations was evaluated on the Vero cells. The results showed that NCEO (IC50 = 65.84 µg/ml) had toxicity effect more than NCEO-CsNg (IC50 = 111.9 µg/ml) and CsNg (IC50 = 298.8 µg/ml) (Fig. 3A). Therefore, used doses for all treatments in anti-Toxoplasma studies were about 2/3 of the IC50 values. As seen in Fig. 3B, among the treatments, the highest anti-Toxoplasma activity was obtained for NCEO-CsNg at 75 µg/ml, while no significant difference with spiramycin (positive control). As it turned out, the encapsulation of the NCEO in CsNg resulted in reducing its cytotoxicity (Fig. 4). Besides, sustained release of the NCEO significantly increases its anti-Toxoplasma efficiency [35].
3.6 Ex vivo anti-Toxoplasma activity of NCEO-CsNg
T. gondii tachyzoites RH strain obtained from infected mice were treated with different formulations at a concentration below IC50 value (Fig. 5). The greatest anti-Toxoplasma activity was obtained in those groups treated with NCEO, NCEO-CsNg, and spiramycin at 40, 75, and 30 µg/ml, respectively. Due to direct contact of drugs with tachyzoites, anti-Toxoplasma efficacy of all formulation exhibited no significant differences. However, as expected, the CsNg-treated group showed the least anti-Toxoplasma activity. In this regard, several studies have confirmed the strong effect of plant essential oils against parasites, especially Toxoplasma. Among the most important compounds, derivatives of lactones, polyphenols, and terpenoids have significant anti-parasitic properties. Similarly, Atolani et al. showed that the essential oil of Cola gigantean has strong anti-Toxoplasma properties [36]. Another study showed that ethanol extract of Piper sarmentosum could inhibit potential T. gondii tachyzoites ex vivo [37]. Our results showed that encapsulation of the NCEO into CsNg does not affect anti-Toxoplasma activity in vitro due to direct interaction between bioactive metabolites with the parasites was reduced. However, after 60 min of treatment, the highest parasitic inhibition was observed at the presence of the NCEO-CsNg (Fig. 6).
3.7 In vivo anti-Toxoplasma activity of NCEO-CsNg
The therapeutic activity of all formulations is presented in Fig. 7A and B. The results showed that 50% of infected-untreated mice were dead after a 5-day infection, while NCEO-CsNg- and NCEO-treated groups had survival time up to 8 days (Fig. 7A). As shown in Fig. 7B, cumulative survival was calculated based on the area under the curve (AUC) of survival charts, indicating the maximum survival time for the NCEO-CsNg-treated group followed by the NCEO and spiramycin (Spn) groups.
In addition to survival monitoring in the in vivo challenge assay, Toxoplasma counts in the liver, spleen, and peritoneal fluid were determined in the treated and untreated groups (see Table 2). Indeed, the group treated with NCEO-CsNg had the fewest tachyzoites. Following that, spiramycin and NCEO showed the lowest tachyzoite infectivity. Figure 8 showed that the spread of Toxoplasma tachyzoite in the tissues of NCEO-CsNg-treated mice was lower than that of the untreated group. So far, several studies have confirmed the effect of plant-derived essential oils on Toxoplasma activity. According to a study by Oliveira et al., two essential oils, estragole and thymol, exhibit the infection of T. gondii tachyzoites in pregnant mice [38]. Khamesipour et al. reported that Dracocephalum kotschyi essential oils significantly increase the survival time of Toxoplasma-infected mice [39]. As claimed by Teimouri et al., Cs alone could inhibit the infection process of Toxoplasma in the mice [40]. Besides, encapsulation of essential oils in the nanostructure of Cs resulted in lowering host toxicity with creating a sustained-release status. Here, our results demonstrate two occurrences with NCEO encapsulation in CsNg, including a synergetic effect and sustainability of the formulation against infection of T. gondii tachyzoites.
4 Conclusions
This study presented a Cs-based formulation for loading NCEO as a factor that improves its stability and release. The results showed that the NCEO loaded in the CsNg had less cytotoxicity and higher efficacy against acute experimental toxoplasmosis. The contact time of the drug with the parasite is prolonged due to the sustained release of NECO from CsNg, and hence, its therapeutic efficacy is improved. Taken together, the current study offers a new perspective for developing drug formulations to inhibit Toxoplasma infection. Additionally, an effective combination therapy plan can be established by encapsulating various drugs in Cs-based nanohydrogels.
References
C. Dard, C. Swale, M.P. Brenier-Pinchart, D.C. Farhat, V. Bellini, M.G. Robert et al., A brain cyst load-associated antigen is a Toxoplasma gondii biomarker for serodetection of persistent parasites and chronic infection. BMC Biol. 19, 25 (2021)
L. Mandelbrot, Congenital toxoplasmosis: what is the evidence for chemoprophylaxis to prevent fetal infection? Prenat. Diagn. 40(13), 1693–1702 (2020)
Ovung, A., Bhattacharyya, J. Sulfonamide drugs: structure, antibacterial property, toxicity, and biophysical interactions. Biophys. Rev. 13, 259–272 (2021). https://doi.org/10.1007/s12551-021-00795-9
K. Cheraghipour, L. Masoori, B. Ezzatpour, M. Roozbehani, A. Sheikhian, V. Malekara, M. Niazi, O. Mardanshah, K. Moradpour, H. Mahmoudvand, The experimental role of medicinal plants in treatment of Toxoplasma gondii infection: a systematic review. Acta. Parasitol. 66, 303–328 (2021)
M.A. Dawood, M.F. El Basuini, A.I. Zaineldin, S. Yilmaz, M. Hasan, E. Ahmadifar et al., Antiparasitic and antibacterial functionality of essential oils: an alternative approach for sustainable aquaculture. Pathogens. 10(2), 185 (2021)
Costa C. M. De Souza, M.G. da Cruz, T.B.C. Lima, L.C. Ferreira, A.S. Ventura, F. Brandão, R, et al, Efficacy of the essential oils of Mentha piperita, Lippia alba and Zingiber officinale to control the acanthocephalan Neoechinorhynchus buttnerae in Colossoma macropomum. Aquac. Rep. 18, 100414 (2020)
R.F. Mady, W. El-Hadidy, S. Elachy, Effect of Nigella sativa oil on experimental toxoplasmosis. Parasitol. Res. 115, 379–390 (2016)
A. Bouyahya, A. Et-Touys, Y. Bakri, A. Talbaui, H. Fellah, J. Abrini, N. Dakka, Chemical composition of Mentha pulegium and Rosmarinus officinalis essential oils and their antileishmanial, antibacterial and antioxidant activities. Microb. Pathog. 111, 41–49 (2017)
C.E.D.L. Da Silva, J. Oyama, F.B.P. Ferreira, M.P. de Paula Lalucci-Silva, T.V.A. Lordani, R.C.D.L. da Silva et al., Effect of essential oils on Leishmania amazonensis: a systematic review. Parasitology 147(13), 1392–1407 (2020)
A.M. Teles, T.D.D.S. Rosa, A.N. Mouchrek, A.L. Abreu-Silva, K.D.S. Calabrese, F. Almeida-Souza, Cinnamomum zeylanicum, Origanum vulgare, and Curcuma longa essential oils: chemical composition, antimicrobial and antileishmanial activity. Evid-Based. Complement. Alternat. Med. 2019, 2421695 (2019)
A. Sharma, R. Cooper, G. Bhardwaj, D.S. Cannoo, The genus Nepeta: traditional uses, phytochemicals and pharmacological properties. J. Ethnopharmacol 268(25), 113679 (2021)
I. Süntar, S.M. Nabavi, D. Barreca, N. Fischer, T. Efferth, Pharmacological and chemical features of Nepeta L genus: its importance as a therapeutic agent. Phytother. Res. 32(2), 185–198 (2018)
G.A. Soto-Chilaca, B. Mejía-Garibay, R. Navarro-Amador, N. Ramírez-Corona, E. Palou, A. López-Malo, Cinnamaldehyde-loaded chitosan nanoparticles: characterization and antimicrobial activity. Biointerface. Res. App. Chem. 9(4), 4060–4065 (2019)
A. Ghanbariasad, F. Amoozegar, M. Rahmani, E. Zarenezhad, M. Osanloo, Impregnated nanofibrous mat with nanogel of Citrus sinensis essential oil as a new type of dressing in cutaneous leishmaniasis. Biointerface. Res. Appl. Chem. 11(4), 11066–11076 (2021)
R.E. Tiplea, G.M. Lemnaru, R.D. Trușcă, A. Holban, M.G.A. Kaya, L.D. Dragu, D. Ficai, A. Ficai, C. Bleotu, Antimicrobial films based on chitosan, collagen, and ZnO for skin tissue regeneration. Biointerface. Res. Appl. Chem. 11(4), 11985–11995 (2021)
K. Cheraghipour, L. Masoori, F. Ezzatkhah, I. Salimikia, S. Amiri, A.S. Makenali et al., Effect of chitosan on Toxoplasma gondii infection: a systematic review. Parasite. Epidemiol. Control. 11, e00189 (2020)
B. Ashrafi, M. Rashidipour, A. Marzban, S. Soroush, M. Azadpour, S. Delfani, Mentha piperita essential oils loaded in a chitosan nanogel with inhibitory effect on biofilm formation against S. mutans on the dental surface. Carbohydr. Polym. 212, 142–149 (2019)
C. Cai, R. Ma, M. Duan, D. Lu, Preparation and antimicrobial activity of thyme essential oil microcapsules prepared with gum arabic. RSC. Adv. 9(34), 19740–19747 (2019)
J.J. Danielson, N. Perez, J.D. Romano, I. Coppens, Modelling Toxoplasma gondii infection in a 3D cell culture system in vitro: comparison with infection in 2D cell monolayers. PloS one. 13(12), e0208558 (2018)
A.A. Sharif, N.Z. Unyah, N. Nordin, R. Basir, M.N. Wana, A.A. Alapid, T. Mustapha, R.A. Majid, Susceptibility of Toxoplasma gondii to ethanolic extract of Tinospora crispa in vero cells. Evid-Based Complement. Alternat. Med. 18, 2019 (2019)
J. Chen, C. Huang, D. Zhu, L. Chen, J. Wang, X. Sun, L. Hu, Y. Duan, Excreted-secreted antigens of Toxoplasma gondii inhibit Foxp3 via IL-2Rγ/JAK3/Stats pathway. J. Cell. Biochem. 19(12), 10176–10185 (2018)
J.J. Zhu, X.P. Zeng, D. Berkebile, H.J. Du, Y. Tong, K. Qian, Efficacy and safety of catnip (Nepeta cataria) as a novel filth fly repellent. Med. Vet. Entomol. 23(3), 209–216 (2009)
N.A. Hagras, A.F. Allam, H.F. Farag, M.M. Osman, T.I. Shalaby, N.M. Mogahed, M.M. Tolba, A.Y. Shehab, Successful treatment of acute experimental toxoplasmosis by spiramycin-loaded chitosan nanoparticles. Exp. Parasitol. 1(204), 107717 (2019)
S.E. Etewa, D.A. El-Maaty, R.S. Hamza, A.S. Metwaly, M.H. Sarhan, S.A. Abdel-Rahman, G.M. Fathy, M.A. El-Shafey, Assessment of spiramycin-loaded chitosan nanoparticles treatment on acute and chronic toxoplasmosis in mice. J. Parasit. Dis. 42(1), 102–113 (2018)
F. Giarratana, D. Muscolino, G. Ziino, V. Lo Presti, R. Rao, V. Chiofalo et al., Activity of catmint (Nepeta cataria) essential oil against Anisakis larvae. Trop. Biomed. 34(1), 22–31 (2017)
A. Gormez, S. Bozari, D. Yanmis, M. Gulluce, G. Agar, F. Sahin, Antibacterial activity and chemical composition of essential oil obtained from Nepeta nuda against phytopathogenic bacteria. J. Essent. Oil Res. 25(2), 149–153 (2013)
T. Tsuruoka, D. Bekh-Ochir, F. Kato, S. Sanduin, A. Shataryn, A. Ayurzana, T. Satou, W. Li, K. Koike, The essential oil of Mongolian Nepeta sibirica: a single component and its biological activities. J. Essent. Oil Res. 24(6), 555–559 (2012)
A. Shakeri, F. Khakdan, V. Soheili, A. Sahebkar, R. Shaddel, J. Asili, Volatile composition, antimicrobial, cytotoxic and antioxidant evaluation of the essential oil from Nepeta sintenisii Bornm. Ind. Crops. Prod. 84, 224–229 (2016)
C. Jianu, R. Moleriu, D. Stoin, I. Cocan, G. Bujancă, G. Pop et al., Antioxidant and antibacterial activity of Nepeta faassenii Bergmans ex Stearn essential oil. Appl. Sci. (Switzerland). 11(1), 442–453 (2021)
G.B. Portapilla, L.M. Pereira, R.A. Soldi, P.G.A. Filho, I.F.L. Gallo, G.C. Clososki et al., Activity of β-caryophyllene oxide derivatives against Trypanosoma cruzi, mammalian cells, and horseradish peroxidase. Rev. Bras. 30(6), 824–831 (2020)
A. Esmaeili, A. Asgari, In vitro release and biological activities of Carum copticum essential oil (CEO) loaded chitosan nanoparticles. Int. J. Biol. Macromol. 81, 283–290 (2015)
N.H. Rezazadeh, F. Buazar, S. Matroodi, Synergistic effects of combinatorial chitosan and polyphenol biomolecules on enhanced antibacterial activity of biofunctionalized silver nanoparticles. Sci. Rep. 10, 19615 (2020)
S.Y.B. de Carvalho, R.R. Almeida, N.A.R. Pinto, C. de Mayrinck, S.S. Vieira, J.F. Haddad et al., Encapsulation of essential oils using cinnamic acid grafted chitosan nanogel: preparation, characterization and antifungal activity. Int. J. Biol. Macromol. 166, 902–912 (2021)
A.M. Khalil, Interpenetrating polymeric hydrogels as favorable materials for hygienic applications. Biointerface. Res. Appl. Chem. 10(2), 5011–5020 (2020)
J. Ju, X. Chen, Y. Xie, H. Yu, Y. Guo, Y. Cheng, H. Qian et al., Application of essential oil as a sustained release preparation in food packaging. Trends Food Sci. Technol. 92, 22–32 (2019)
O. Atolani, H. Oguntoye, E. Areh, O. Adeyemi, L. Kambizi, Chemical composition, anti-Toxoplasma, cytotoxicity, antioxidant, and anti-inflammatory potentials of Cola gigantea seed oil. Pharm. Biol. 57(1), 154–160 (2019)
K. Devanthran, Z. Unyah, R.A. Majid, W.O. Abdullah, In vitro activity of Piper sarmentosum ethanol leaf extract against Toxoplasma gondii tachyzoites. Trop. J. Pharm. Res. 16(11), 2667–2673 (2017)
C.B. Oliveira, Y.S. Meurer, T.L. Medeiros, A.M. Pohlit, M.V. Silva, T.W. Mineo et al., Anti-Toxoplasma activity of estragole and thymol in murine models of congenital and noncongenital toxoplasmosis. J. Parasitol. 102(3), 369–376 (2016)
F. Khamesipour, S.M. Razavi, S.H. Hejazi, S.M. Ghanadian, In vitro and in vivo anti-Toxoplasma activity of Dracocephalum kotschyi essential oil. Food Sci. Nutr. 9, 522–531 (2021)
A. Teimouri, S.J. Azami, H. Keshavarz, F. Esmaeili, R. Alimi, S.A. Mavi et al., Anti-Toxoplasma activity of various molecular weights and concentrations of chitosan nanoparticles on tachyzoites of RH strain. Int. J. Nanomed. 13, 1341–1351 (2018)
Funding
The research was supported through a financial grant (grant number A-10–1503-1) by Lorestan University of Medical Sciences and has been fulfilled in Razi Herbal Medicines Research Center.
Author information
Authors and Affiliations
Contributions
K Ch contributed as supervisor of the whole project. M Z and M B contributed in laboratory investigations. P Sh contributed in data gathering. F Kh, M Z P, and A K A contributed to the development of the study design. M Gh assisted in performance of experiments. A M analyzed the data, prepared the graphs, and wrote the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Animal studies were conducted according to the ethical guidelines and approved by the Committee for the Purpose of Control and Supervision of Experiment on Animals in Lorestan University of Medical Sciences (Reference no. animal ethics permission with code: IR.LUMS.REC.1398.272).
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Cheraghipour, K., Zivdari, M., Beiranvand, M. et al. Encapsulation of Nepeta cataria essential oils in a chitosan nanocomposite with lethality potential against Toxoplasma gondii. emergent mater. 5, 653–663 (2022). https://doi.org/10.1007/s42247-022-00381-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42247-022-00381-z