Abstract
Single-photon emission computed tomography combined with computed tomography (SPECT/CT) has revolutionized nuclear medicine. Nevertheless, the addition of CT has increased the patients' exposure. We aimed to evaluate the contribution of low-dose CT scans to the total effective dose for 123I-metaiodobenzylguanidine SPECT/CT examination in a pediatric population. The mean effective doses of SPECT, CT, and SPECT/CT were 4.96 mSv, 0.69 mSv, and 5.64 mSv, respectively. The CT effective dose was significantly lower than the SPECT one. The mean of the additional radiation exposure due to CT was 14% (2–37%). This radiation dose is not negligible. However, taking into account the benefit of hybrid imaging, this additional radiation remains justifiable.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neuroblastoma is the most common malignant neoplasm in childhood [1]. It arises from primitive neuroblasts of the embryonic neural crest, and therefore, can occur anywhere within the sympathetic nervous system [2]. It synthesizes, stores, and releases catecholamines and their precursors. The radiolabelled metaiodobenzylguanidine (mIBG), an analog of guanethidine which is taken up by tumors derived from the neural crest, has excellent sensitivity and near-absolute specificity in the imaging of neuroblastoma [3]. It is used at different stages of the disease: initial diagnosis, therapeutic evaluation and search for recurrence. For the initial extension assessment, it makes it possible to establish the extension assessment and assess tumor avidity. For the therapeutic evaluation, it makes it possible to evaluate the response of the primary tumor and of the metastatic lesions, with high specificity. In fact, it is not affected by post-treatment changes. For the search for recurrence, it makes it possible to establish the assessment of extension of recurrence. In addition, it can select eligible patients for internal vectorized radiotherapy with 131I-mIBG, by assessing the number and the avidity of lesions [4, 5]. Moreover, it has prognostic value. In fact, recently, scores have been validated to quantify bone metastases. A significant reduction after chemotherapy of mIBG avid metastases has a better prognosis [6, 7].
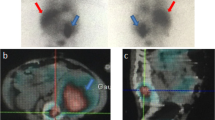
The mIBG scintigraphy is a functional imagery, poor in anatomical landmarks. The tomographic acquisition, single-photon emission computed tomography (SPECT), improves the localization of anomalies. Currently, hybrid imaging (SPECT/CT) combining SPECT and Computed Tomography (CT), which provides anatomical information, increases the performance of scintigraphy [8, 9]. It also makes it possible to differentiate the pathological foci from those which are physiological. In addition, the CT, which allows attenuation correction, improves the quality of images [10].
For neuroblastoma, it has been proven in the literature that SPECT/CT can provide additional diagnostic advantages over diagnostic CT and detected more functioning lesions than planar imaging [8, 9, 11]. The study by Ben-Sellem et al., including 56 SPECT/CT performed in 40 children, objected that SPECT/CT provided additional information in 88% of the examinations, which was crucial in 20% of the cases. It better characterized the lesions and their locoregional extension (44 cases) and better staged lymph node involvement (28 cases). It detected new lesions (33 cases) and ruled out nine false positives [10]. The study by Theerakulpisut et al., including 86 SPECT/CT, objected that hybrid imaging diagnosed additional lesions in 23.2% of cases, better localized lesions in 21.1% of cases, characterized suspicious lesions in 85.7% of cases and confirmed the metabolic nature of the anatomical lesions in 94.4% of cases [12]. Additional information provided by SPECT/CT over planar images was also objectified by Nadel in 29% of cases and by Liu et al. in 39% of cases [13, 14].
However, the addition of even a low-dose CT, sufficient for the anatomic referencing of SPECT lesions and for the attenuation correction [15, 16], increases the overall delivered dose of radiation [17].
Children represent a population that is particularly sensitive to ionizing radiation, characterized by increased radiosensitivity of certain tissues compared to adults, a long life expectancy, with a consequent higher probability of developing cancer [18,19,20]. It is, therefore, necessary to keep the radiation dose as low as reasonably achievable (ALARA).
The aim of this study was to evaluate the contribution of CT scans to the total effective dose for 123I-mIBG SPECT/CT examination in a pediatric population.
Materials and methods
Study population
We prospectively studied a series of 30 children followed for neuroblastoma and benefiting from a 123I-mIBG scintigraphy, necessarily including in its protocol at least one SPECT/CT acquisition.
Patients were divided into five groups: group A (age ≤ 2.5 years), group B (2.5 years < age ≤ 7.5 years), group C (7.5 years < age ≤ 12.5 years), group D (12.5 years < age ≤ 17.5 years), and group E (17.5 years < age ≤ 18 years). The examination was carried out with a hybrid machine combining a dual-headed SPECT unit and an integrated 2-slice CT scanner (Symbia T E-Cam, Siemens Healthcare Erlangen Germany). Thyroid blockage, crucial in protecting the thyroid from unnecessary radiation mainly in children, was achieved by taking potassium iodide for 5 days (3 days before and 2 days after the radiopharmaceutical injection). 123I-mIBG was injected into a peripheral vein. The administration was slow, to avoid the potential side effects of mIBG (vomiting, tachycardia, pallor, and abdominal pain). The activity injected depended on the age of the patient (Table 1). A series of images was acquired 24 h later.
123 I-mIBG SPECT/CT imaging protocol
The energy window was 159 keV ± 10%. For children under 15 years of age, static acquisitions were made in anterior and posterior incidences, sweeping the whole body. The acquisition/image time was 600 s. The matrix was 256 × 256. The zoom was adapted to age. For the rest of the patients, a whole-body scan was performed. The scanning speed was 8 cm/min. The matrix was 256 × 1024. In some cases, the scanning was supplemented by a centered static image (600 s, 256 × 256 matrix).
The SPECT consisted of the acquisition of 32 projections of 40 s/head, with a total of 64 projections over 360. The acquisition matrix was 128 × 128. The energy window was 159 keV ± 10%. The tomoscintigraphic reconstruction used a filtered back projection and the images were smoothed with a Butterworth filter. The SPECT was instantly followed by CT acquisition, where the parameters were: tube voltage of 130 kV; 2 × 2.5 mm collimation; pitch of 1.5; slice thickness of 1 mm; matrix of 512 × 512 and acquisition time of 2.4 s.
This low-dose CT protocol provides acceptable image quality for this hybrid examination.
Dosimetric study
The contribution of the effective dose of 123I-mIBG scintigraphy for each patient was calculated by multiplying the average administered activity for all patients by the conversion factors “effective dose per unit of administered activity” [15] listed in the International Commission on Radiological Protectin [21].
The effective dose from the CT portion of the examination was calculated from the product of the dose length product (DLP) and a body-region-specific conversion factor k (mSv.mGy−1.cm−1) [22]. DLP is a value given, for each patient, by the machine’s acquisition station. It depends on the scan length and the acquisition parameters.
The total effective dose of SPECT/CT (ESPECT/CT) is the sum of the effective doses ESPECT and ECT [15].
The percentage contribution of the additional radiation of the CT (%ECT) is given by the following equation:
Statistical analysis
Quantitative variables were expressed using means ± standard deviation. For qualitative variables, an evaluation of frequencies was used. Means were compared using the Student t test. A p value of less than 0.05 was considered statistically significant.
Results
The mean age was 5.27 years, ranging from 8 months to 18 years. Patients were 19 boys and 11 girls. The sex ratio F:M was 1.7. There were 10 children in group A, 13 in group B, 5 in group C, and 1 in groups D and E.
Table 1 displays, for each group, the average activity of 123I-mIBG injected, the conversion factors “effective dose per unit of administered activity” used, the effective dose for SPECT portion of the examination and the Diagnostic Reference Levels (DRLs) set by two references: the version 214 of the European Association of Nuclear Medicine (EANM 2014) and the North American guidelines. The average effective dose was 4.96 ± 1.93 mSv (range 2.886–7.548 mSv). Group A was the most exposed to radiation. It exceeded the DRLs set by the EANM 2014 and the North American guidelines.
Table 2 shows, for each anatomical region scanned and for each group, the mean and the interval of DLPs. Then, we compared them to the DRLs [23]. No patient exceeded these values.
The average effective dose due to CT portion was 0.689 ± 0.226 mSv. Table 3 details the mean and the interval of these doses, for each anatomical region scanned and for each group. The lowest value was for the head–neck region due to the lower weighting factors of the irradiated tissues in this region. Figure 1 shows that this dose increased with age. The average effective dose induced by SPECT/CT examination was 5.64 ± 1.89 mSv. Table 4 details the mean and the interval of these doses, for each anatomical region scanned and for each group. The highest value was for the group A, followed by group B (Fig. 2). The average contribution of CT scans to the total effective dose for SPECT/CT examination was 14 ± 7%, and ranged from 2 to 37%. The CT doses were significantly lower than the radiopharmaceutical administered doses (p < 0.05). Table 5 details this contribution for each anatomical region scanned and for each group. The lowest value was for group A. This contribution increased with age (Fig. 3).
Discussion
The results presented in this study demonstrate that the addition of CT in the SPECT/CT hybrid imaging increases patient radiation dose. In fact, the total effective dose for SPECT-CT examination is the sum of the effective dose induced by radiopharmaceutical injected to patient and the effective dose induced by CT portion. The effective dose is an important parameter for comparing the doses and the risks of ionizing radiation due to the various diagnostic examinations.
The effective dose induced by the 123I-mIBG scintigraphy was calculated as the product of the average of administered activity and the effective dose per unit administered activity. The latest factor, determined from the ICRP 80 [15] depends on age. The effective dose induced by the 123I-mIBG scintigraphy is as well an age-dependent factor. It ranged between 2.52 and 7.55 mSv, with an average of 4.96 mSv. It is higher than that obtained by Michael et al. (2.6–2.9 mSv) [24]. Children under 2.5 years of age (group A) were the most exposed to radiation. The effective dose for the 10 patients of this group exceeded the dose limits set by the EANM 2014 (5.1 mSv) and the North American guidelines (3.5 mSv). For the group B (children over 2.5 years and under 7.5 years of age), this dose exceeded the North American guidelines but remained lower than the EANM 2014 dose. For all older patients (groups C, D, and E), it was below the thresholds proposed by these two organizations. Besides age, this effective dose also depends on the radiopharmaceutical administered. It was higher for 131I tracers than for 99mTc ones. Among 99mTc tracers, it was the highest for the 99mTc-MIBI (MethoxyIsoButylIsonitrile) [16, 17].
To estimate the effective dose induced by the CT, we used the DLP method. Like other dose-calculation methods, such as the CTExpo [25] and ImpacDose [26] programs, the DLP method shares similar uncertainties [27, 28]. We chose it for its simplicity of use. It is based on the product of two age-dependent parameters: the conversion factor k and the DLP. The first parameter takes into account the variation in the biological sensitivity of the different organs. Therefore, it depends on the anatomical region explored. It is the highest for the abdomino-pelvic region, which is the most radiosensitive. Several k conversion coefficients for diagnostic CT were published [15, 29, 30], where our choice was the ICRP 80 publication [21]. The DLP, provided by the scanner, depends on the length of the irradiated region. For the same region, it increases with age. For the 30 patients of our study, the DLP values were lower than the DRLs [23], regardless of the age and the region explored. In this study, the effective dose induced by the CT ranged from 0.17 to 1.68 mSv, with an average 0.69 mSv. It was lower for the head–neck region than abdomino-pelvic one. These values are within the range of the effective doses induced by low-dose CTs published by other authors. Vallin et al. found, for pediatric population, the value of 1.1 mSv for chest scan and 1.3 mSv for abdomen and pelvic scan [31]. Montes et al. found that the average effective dose of CT of 145 adult SPECT/CT examinations varied depending on the region explored, lower (0.6 mSv) for the head–neck region (three examinations) and higher (1.2 mSv) for neck–thorax (71 examinations) and abdomino-pelvis (57 examinations) regions. It depends also on the scanned length; it was 2.6 mSv for whole body [15]. Values found by Sawyer et al., on phantoms, were 0.1 mSv for a head scan, 0.9 mSv for a chest scan and 1.5 mSv for an abdomino-pelvic scan [28]. Those found by Brix et al. for whole-body imaging were 5 mSv [32].
The total effective dose ranged from 3.26 and 8.34 mSv. It was higher for the younger category (under two years and a half). The average was 5.64 mSv. This value depends on the nuclear tracers. In a pediatric study including 78 Positron Emission Tomography coupled with CT (PET/CT) with 18F-FDG (2-deoxy-2-fluorine-18fluoro-d-glucose), the average effective dose was 24.8 mSv and ranged from 6.2 to 60.7 mSv [33].
To quantify the additional radiation induced by the CT, we calculated the percentage of the effective dose induced by CT to the total dose delivered by the hybrid imaging. This value increased with age. It ranged from 2 to 37%, with an average of 14%. This value depends on the examination carried out, in particular, the length explored by the CT. In SPECT/CT examination, often only one region is explored by the CT. This value remains relatively low compared to the effective dose induced by the radiopharmaceutical administration, such as in our study. Law et al. got the same value (14%) for an adult population benefiting from breast lymphoscintigraphy in search of the sentinel node of breast cancer [34]. Other studies in adults have found higher values: 60% for 99mTc-MDP (methylene diphosphonate), 65% for 99mTc-MIBI and 42% for 131I-mIBG [16, 17]. For PET/CT, the region explored by CT often extends from the vertex to mid-thigh. Therefore, the CT additional radiation increases considerably. It reached 66% in the study of Quin et al. [35], 76.7% in the study of Khamwan et al. [36] and 78.2% in the study of Paiva et al. [37]. There are several ways to reduce CT doses. The implementation of these methods requires close collaboration between medical physicists, manufacturers, radiologists, technologists, and referring physicians to be effective. We cited the optimized scanning parameters which include the tube current, tube voltage, filtration, collimation, reconstruction method, reconstruction filter, slice thickness, pitch, and scanning length. There are other parameters such as the automatic exposure control, the iterative image reconstruction and the adaptive collimation to reduce effect of ‘overscanning’ [24]. Another important parameter to reduce the dose delivered by the CT is the use of low-dose CT scan. The goal of adding the CT in hybrid imagery, notably SPECT/CT is to provide anatomical landmarks and to improve the quality of the images thanks to the attenuation correction. This can be achieved using a low-dose CT scan. On one hand, it has been demonstrated in phantoms that a low-dose CT scan can be adequately used for attenuation correction in SPECT and PET studies [3, 38], thereby reducing radiation exposure significantly. On the other hand, low-dose CT scans were useful for localizing the functional alterations found on SPECT images, despite the noisy images these CT scans yield.
The higher cell mitosis rate, the longer post-exposure life expectancy and the smaller body size make pediatric patients more radiosensitive. Therefore, special radiation protection measurements have to be taken into consideration [39]. Therefore, patients should not receive a radiation dose unless it is widely justified [15]. Once justified, it is essential to apply the ALARA principle of exposure to ionizing radiation without sacrificing diagnostic information. Several publications report that the radiosensitivity of pediatric patients is ten times greater than that of middle-aged adults. In addition, most CT services currently use pre-programmed CT protocols and do not consider protocols specific to age, weight, body size, and composition [39].
In recent years, hybrid SPECT/CT imaging, by providing functional and anatomical fused images, combines the advantages of these two imaging methods: high anatomic resolution for the CT and good specificity for SPECT [15]. This has also been demonstrated for the 123I-mIBG scintigraphy in the management of neuroblastomas. Several studies have shown the contribution of hybrid imagery with 123I-mIBG in this cancer. In a study of 44 children, Nadel et al. suggested that the SPECT/CT has allowed completely staging or restaging 27 children. They have also found 29% value-added information [13]. This rate was 39% in the study of Liu et al. [14]. In another study including 86 SPECT/CT done in 36 patients, SPECT/CT detected additional lesions in 23.2% of cases, helped localize lesions in 21.1% of cases, resolved suspicious findings in 85.7% of cases, determined functional status of lesions on anatomical imaging in 94.4% of cases and changed diagnosis from a negative to a positive study in 19.5% of cases [12]. 123I-mIBG SPECT/CT hybrid imaging in children with neuroblastoma allows detection of new lesions, better characterisation of the lesion and its locoregional extension, and better lymph node staging. It, therefore, has an undeniable added value that improves the interpretation of planar imaging and influences patient management [10]. These potential benefits of this dual modality imaging justify the additional radiation induced by the CT in this pediatric population. However, to optimize this dose, it is recommended to use a low-dose CT scan.
To our knowledge, this is the first study in published literature that evaluates the dosimetry of 123I-mIBG SPECT/CT in a pediatric population. However, it has certain limitations that are required to be acknowledged. The first one is the small number of patients, although justified by the fact that the SPECT/CT is not systematically included in the 123I-mIBG scintigraphy protocol (requested according to the planar imaging results). The second one is the use of the DLP method which presents uncertainties. For more accurate estimations, it would be necessary to calculate the dose absorbed by the irradiated organs.
Conclusion
The CT of hybrid SPECT/CT systems enables, by fusing functional information from the SPECT and anatomical ones from the CT, to improve the quality of image and the diagnostic performances of scintigraphic imaging. We estimated the additional radiation exposure due to low-dose CT for SPECT/CT with 123I-mIBG in a pediatric population. The mean was 14%. In addition, the CT effective dose was significantly lower than the SPECT one. Given the potential benefits associated with this hybrid imaging, this relative increase is considered acceptable. Nevertheless, the “As Low as Reasonably Achievable (ALARA)” principle must be respected to ensure that the patient is not subjected to unnecessarily high levels of radiation.
References
David R, Lamki N, Fan S, Singleton EB, Eftekhari F, Shirkhoda A, Kumar R, Madewell JE. The many faces of neuroblastoma. Radiographics. 1989;9:859–82.
Maris JM, Hogarty MD, Bagatell R, Cohn SL. Neuroblastoma. The Lancet. 2007;369:2106–20.
Martin C. Effective dose: how should it be applied to medical exposures? Br J radiol. 2007;80:639–47.
Bar-Sever Z, Biassoni L, Shulkin B, Kong G, Hofman MS, Lopci E, et al. Guidelines on nuclear medicine imaging in neuroblastoma. Eur J Nucl Med Mol Imaging. 2018;45:2009–24.
Matthay KK, Shulkin B, Ladenstein R, Michon J, Giammarile F, Lewington V, Pearson ADJ, Cohn SL. Criteria for evaluation of disease extent by (123)I-metaiodobenzylguanidine scans in neuroblastoma: a report for the International Neuroblastoma Risk Group (INRG) task force. Br J Cancer. 2010;102:1319–26.
Yanik GA, Parisi MT, Shulkin BL, Naranjo A, Kreissman SG, London WB, et al. Semiquantitative mIBG scoring as a prognostic indicator in patients with stage 4 neuroblastoma: a report from the Children’s Oncology Group. J Nucl Med. 2013;54:541–8.
Ladenstein R, Lambert B, Pötschger U, Castellani MR, Lewington V, Bar-Sever Z, et al. Validation of the mIBG skeletal SIOPEN scoring method in two independent high-risk neuroblastoma populations: The SIOPEN/HR-NBL1 and COG-A3973 trials. Eur J Nucl Med Mol Imaging. 2018;45:292–305.
Franzius C, Hermann K, Weckesser M, Kopka K, Juergens KU, Vormoor J, Schober O. Whole-body PET/CT with 11c-metahydroxyephedrine in tumors of the sympathetic nervous system: feasibility study and comparison with 123I-mIBG SPECT/CT. J Nucl Med. 2006;47:1635–42.
Fukuoka M, Junichi T, Takafumi M, Seigo K. Comparison of diagnostic value of 123I-mIBG and high-dose 131I-mIBG scintigraphy including incremental value of SPECT/CT over planar image in patients with malignant pheochromocytoma/paraganglioma and neuroblastoma. Clin Nucl med. 2011;36:1–7.
Ben-Sellem D, Ben-Rejeb N. Does the incremental value of 123I-Metaiodobenzylguanidine SPECT/CT over planar imaging justify the increase in radiation exposure? Nucl Med Mol Imaging. 2021;55:173–80.
Rozovsky K, Koplewitz BZ, Krausz Y, Revel-Vilk S, Weintraub M, Chisin R, Klein M. Added value of SPECT/CT for correlation of mIBG scintigraphy and diagnostic CT in neuroblastoma and pheochromocytoma. AJR Am J Roentgenol. 2008;190:1085–90.
Theerakulpisut D, Raruenrom Y, Wongsurawat N, Somboonporn C. Value of SPECT/CT in diagnostic 131I-mIBG scintigraphy in patients with neuroblastoma. Nucl Med Mol imaging. 2018;52:350–8.
Nadel HR. SPECT/CT in pediatric patient management. Eur J Nucl Med Mol imaging. 2014;41:104–14.
Liu B, Servaes S, Zhuang H. SPECT/CT mIBG imaging is crucial in the follow-up of the patients with high-risk neuroblastoma. Clin Nucl Med. 2018;43:232–8.
Montes C, Tamayo P, Hernandez J, Gomez-Caminero F, Garcia S, Martin C, Rosero A. Estimation of the total effective dose from low-dose CT scans and radiopharmaceutical administrations delivered to patients undergoing SPECT/CT explorations. Ann Nucl Med. 2013;27:610–7.
Larkin AM, Serulle Y, Wagner S, Noz ME, Friedman K. Quantifying the increase in radiation exposure associated with SPECT/CT compared to SPECT alone for routine nuclear medicine examinations. Int J Mol Imaging. 2011;2011:897202–6.
Sharma P, Sharma S, Ballal S, Bal C, Malhotra A, Kumar R. SPECT/CT in routine clinical practice: increase in patient radiation dose compared with SPECT alone. Nucl Med Commun. 2012;33:926–32.
Kleinerman RA. Cancer risks following diagnostic and therapeutic radiation exposure in children. Pediatr radiol. 2006;36:121–5.
Kutanzi KR, Lumen A, Koturbash I, Miousse IR. Pediatric exposures to ionizing radiation: carcinogenic considerations. Int J Environ Res Public Health. 2016;13:1057.
Yagui A, Malthez ALMC, Filipov D. Dose evaluation in pediatric gastrointestinal fluoroscopy. Radiat Phys Chem. 2020;167:108384.
ICRP. Radiation dose to patients from radiopharmaceuticals:(addendum 2 to ICRP publication 53) ICRP publication 80 approved by the commission in september 1997. Ann ICRP. 1998;28:1.
European Guidelines on Quality Criteria for Computed Tomography. Report EUR 16262 (Brussels: EU). 2000.
Jodlr F. Arrêté du 24 october 2011 relatif aux niveaux de référence diagnostiques en radiologie et en médecine nucléaire. In: Ministere du Travail Dleedls, editor. Décrets, arrêtées, circulaires; 2011. pp. 1–6.
Gelfand MJ, Lemen LC. PET/CT and SPECT/CT dosimetry in children: the challenge to the pediatric imager. Semin Nucl Med. 2007;37:391–8.
Nagel HD. Radiation exposure in computed tomography: fundamentals, in influencing parameters, dose assessment, optimisation, scanner data, terminology. Eur Radiol. 2001;11:2644.
Kalender WA, Schmidt B, Zankl M, Schmidt M. A PC program for estimating organ dose and effective dose values in computed tomography. Eur radiol. 1999;9:555–62.
Gregory KJ, Bibbo G, Pattison JE. On the uncertainties in effective dose estimates of adult CT head scans. Med phys. 2008;35:3501–10.
Sawyer LJ, Starritt HC, Hiscock SC, Evans MJ. Effective doses to patients from CT acquisitions on the ge infinia hawkeye: a comparison of calculation methods. Nucl Med Commun. 2008;29:144–9.
Christner JA, Koer JM, McCollough CH. Estimating effective dose for CT using dose length product compared with using organ doses: consequences of adopting international commission on radiological protection publication 103 or dual-energy scanning. AJR Am J Roentgenol. 2010;194:881–9.
ICRP. Recommendations of the international commission on radiological protection. ICRP publication 103. Ann ICRP. 2007;37:1–332.
Vallin C, Blouin P, Venel Y, Maurin L, Sirinelli D. The use of computed tomography and nuclear medicine examinations in paediatric oncology: an analysis of practice in a university hospital. Diagnostic and interventional imaging. Diagn Interv Imaging. 2014;95:411–9.
Brix G, Lechel U, Glatting G, Ziegler SI, Münzing W, Müller SP, Beyer T. Radiation exposure of patients undergoing whole-body dual-modality 18F-FDG PET/CT examinations. J Nucl Med. 2005;46:608–13.
Chawla SC, Federman N, Zhang D, Nagata K, Nuthakki S, McNitt-Gray M, Boechat NI. Estimated cumulative radiation dose from PET/CT in children with malignancies: a 5-year retrospective review. Pediatr Radiol. 2010;40:681–6.
Law M, Ma WH, Leung R, Li S, Wong KK, Ho WY, Kwong A. Evaluation of patient effective dose from sentinel lymph node lymphoscintigraphy in breast cancer: a phantom study with SPECT/CT and ICRP-103 recommendations. Eur J radiol. 2012;81:e717–20.
Quinn B, Dauer Z, Pandit-Taskar N, Schoder H, Dauer LT. Radiation dosimetry of 18F-FDG PET/CT: incorporating exam-specific parameters in dose estimates. BMC Med imaging. 2016;16:41.
Khamwan K, Krisanachinda A, Pasawang P. The determination of patient dose from 18F-FDG PET/CT examination. Radiat Prot Dosim. 2010;141:50–5.
Paiva FG, do Carmo Santana P, Mourao AP. Evaluation of patient effective dose in a PET/CT test. Appl Radiat Isot. 2019;145:137–41.
Kumar S, Pandey AK, Sharma P, Malhotra A, Kumar R. Optimization of the CT acquisition protocol to reduce patient dose without compromising the diagnostic quality for PET-CT: a phantom study. Nucl Med Commun. 2012;33:164–70.
Karami V, Gholami M. Addressing as low as reasonably achievable (ALARA) in pediatric computed tomography (CT) procedures. J Res Med Dent Sci. 2018;6:104–14.
Funding
The work of this research project has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Naima Ben-Rejeb and Dorra Ben-Sellem declare that they have no competing interests.
Availability of data and material
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Code availability
Not applicable.
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki Declaration as revised in 2013 and its later amendments or comparable ethical standards.
Informed consent
It is a retrospective study that was approved by the hospital ethics committee and that did not require informed consent from patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ben-Rejeb, N., Ben-Sellem, D. Evaluation of the increase in radiation exposure in 123I-metaiodobenzylguanidine SPECT/CT in children. Chin J Acad Radiol 5, 29–36 (2022). https://doi.org/10.1007/s42058-021-00084-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42058-021-00084-0