Abstract
Stunning advances in treatment modalities implemented in children with hematological malignancies have led to 5-year overall survival rates exceeding 85%. However, this growing population of long-term survivors has raised significant concerns about their fertility status throughout adulthood, while specific treatment- and non-treatment-related factors appear to possibly affect fertility through distinct mechanisms. We aimed to comprehensively review the published literature on the association between treatment-related factors and risk of impaired fertility in childhood hematological cancer survivors. We searched PubMed up to March 2021 to identify eligible studies published during the last two decades. A narrative synthesis of the results was performed, although no meta-analysis was feasible due to the small number of studies and the large heterogeneity of evidence. Five studies on 2020 survivors of childhood leukemia were deemed eligible. The qualitative data synthesis showed significant fertility deficits in survivors treated with cranial radiotherapy and chemotherapy for childhood leukemia. Two studies examined biochemical measures of reduced ovarian reserve, providing some evidence that the levels of anti-Müllerian hormone can be used as a proxy for diminished ovarian reserve. The current findings should facilitate the delivery of age- and gender-appropriate interventions to optimize reproductive outcomes in childhood hematological cancer survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past few decades, significant advances in the management of childhood hematological malignancies have been achieved resulting in 5-year overall survival rates exceeding 85–95% [1], with novel therapeutic interventions accounting for this achievement [2]. On the other hand, this development has led to a growing number of patients who, while subsequently becoming long-term survivors reaching adulthood, will be in need of specialized care and counseling regarding specific life events, such as family and reproductive health issues. In the meantime, the increasing number of long-term survivors has raised significant concerns with regard to their fertility status [3]. Crucially, the treatments administered to these patients are highly gonadotoxic, resulting in disease-free patients facing fertility issues later on in their adult life. For these reasons, the choice of fertility preservation for these patients is extremely important [3].
Specific treatment- and non-treatment-related factors may potentially affect fertility through distinct mechanisms [4]. In particular, chemotherapeutic agents have a large number of gonadotoxic effects [5, 6]. Among these, alkylating agents, especially cyclophosphamide, may damage primordial follicles and subsequently cause amenorrhea, ovarian damage, early menopause and, thus, infertility [7]. In males, these agents cause damage to sperm function, including morphological abnormalities or loss of motility. The sperm count may recover after cytotoxic therapy, but there might be a period of azoospermia, which can be long and may cause morphological abnormalities, or the sperm might plateau in the oligospermia range [8]. Anthracyclines may also contribute to ovarian damage [8]. Other drugs such as methotrexate, vincristine, bleomycin, dactinomycin, and fluorouracil present lower to no risk of amenorrhea and infertility [9].
The term ovarian reserve refers to the number of primordial follicles that exist in the ovaries and play a pivotal role in fertility [10]. Functioning of the ovaries can be clinically monitored through the regularity of menstrual cycles experienced by a woman, but this does not always reflect the patient’s ovarian reserve and fertility. Notably, women with a regular cycle can potentially have diminished ovarian reserve [11]. Various methods for measuring ovarian reserve are applied, such as measurement of the levels of inhibin B, estradiol, anti-Müllerian hormone (AMH), follicle-stimulating hormone (FSH), and ovarian antral follicle count [12]. Overall, previous studies so far have reached inconclusive results primarily due to the limited number of participants, selection bias, and low power.
We aimed to comprehensively review published evidence on the fertility status of survivors of childhood hematological malignancies. We further aimed to determine whether there are specific treatment- and non-treatment-related factors linked to impaired fertility among childhood cancer survivors.
Methods
Search strategy
The present systematic review was performed following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Supplementary Table 1) [13].
We searched PubMed up to March 1, 2021, to identify eligible studies published during the last 20 years that examined fertility status in survivors exclusively of childhood hematological malignancies, as well as treatment- and non-treatment-related factors that may affect their fertility. Given the different treatment modalities used in the treatment of childhood hematological malignancies during the last couple of decades, studies published before 2001 were not considered in the present systematic review in order to ensure comparability of evidence across different study groups. The following MeSH terms were used: “infertile,” “sterile,” “children,” “leukemia,” “survivor,” “childhood cancer,” “childhood cancer therapy,” “childhood cancer treatment,” “ovarian reserve,” “ovarian function,” “ovarian insufficiency,” “childhood cancer survivor,” “female childhood cancer survivor,” “male childhood cancer survivor,” “long-term effects of childhood cancer,” “ovarian reserve for childhood cancer,” “premature ovarian insufficiency,” “childhood malignancy,” “childhood malignancies,” “ovarian dysfunction,” “chemotherapy,” “reproductive function,” “acute lymphocytic leukemia,” “acute myeloid leukemia,” (“childhood cancer” AND “ovarian reserve”), (“childhood cancer” AND “ovarian insufficiency”), (“childhood cancer” AND “ovarian function”), (“childhood cancer” AND “ovarian dysfunction”), (“childhood cancer” AND “ovarian insufficiency”), (“long-term effects” AND “ovarian reserve”), (“long-term effects” AND “ovarian insufficiency”), (“long-term effects” AND “ovarian function”), (“long-term effects” AND “dysfunction”), (“childhood malignancies” AND “ovarian reserve”), (“childhood malignancy” AND “ovarian reserve”), (“childhood malignancies” AND “reproductive function”), (“childhood malignancy” AND “ovarian reserve”), (“chemotherapy” AND “ovarian reserve”), (“ovarian reserve” AND (“childhood cancer” OR “childhood malignancy” OR “childhood malignancies” OR “acute lymphocytic leukemia” OR “acute myeloid leukemia” OR “AML”), (“childhood cancer” AND (“ovarian reserve” OR “ovarian function” OR “ovarian insufficiency” OR “ovarian dysfunction”). No restrictions were applied.
Two authors independently assessed all results for inclusion/exclusion criteria. Disagreements were resolved following consensus. The references of the selected articles were also manually searched for any additional potentially relevant articles (“snowball” procedure).
Inclusion/exclusion criteria
Eligible studies were cohort, case-control, and cross-sectional studies that examined fertility status in survivors of childhood hematological malignancies, which were defined as patients who have achieved complete remission after treatment and were assessed for their fertility status after they completed their treatment. Fertility impairment was defined by as follows: (1) parenthood/number of offspring or parenthood via assisted reproductive techniques/in vitro fertilization; (2) biochemical/hormonal evaluation (measuring FSH, LH, testosterone, AMH, inhibin B, estradiol); (3) evaluation of testicular and/or ovarian volume; (4) physical examination (Tanner stage, stage of puberty); or (5) histological changes in ovaries, testes, or semen as provided by the available studies. Studies examining leukemia diagnosed during adulthood (>18 years) or during pregnancy were excluded. Moreover, studies assessing the fertility status in childhood leukemia cases immediately after the end of treatment were excluded. Case series, case reports, in vitro and animal studies, or cell cultures were also excluded. Studies were further assessed for overlapping populations. In such a case, the most recent or most complete publication was considered eligible for inclusion.
Data extraction and quality assessment
Two authors independently extracted relevant data from the eligible studies using a customized data extraction form. The following characteristics of the eligible studies were extracted: name of first author; publication year; country in which the study was conducted; study design; study period; exposure variables of interest; number of cases and controls; age range of participants; outcome variables and type of outcome assessment; and adjusting variables in the analysis.
The data extraction form also included a quality assessment of the eligible studies. Studies were rated as of good, fair, or poor quality based on the sample size, clear statement of the research objective, and utilization of appropriate outcome measures.
Data synthesis
A narrative synthesis of the results of the systematic review was performed so as to report the risk for infertility among childhood survivors of hematological malignancies. Studies were grouped separately by the type of fertility assessment (hormonal evaluation, physical examination, testicular volume, and parenthood) and by the type of exposure (chemotherapy, radiotherapy, and genetic factors) in order to secure homogeneity.
Thereafter, a quantitative synthesis was performed for the association of specific treatment- and non-treatment-related characteristics with risk of fertility impairment whenever three or more studies assessing the same exposure and outcome measures were available. The odds ratios (OR) and their respective 95% confidence intervals (CI) were used for the effect of specific chemotherapeutic agents, radiotherapy, or genetic factors on fertility status. Between-study heterogeneity was measured using Cochran’s Q statistic and by calculating I-squared. Significance level was set at p < 0.10. Random-effect models were applied in all analyses, irrespective of the I-squared estimate. For the overall effect, the statistical significance level was set at p < 0.05. Meta-analyses were conducted using the STATA software.
Results
Study characteristics
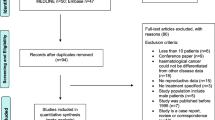
The initial literature search yielded 5081 articles, while one study was additionally identified through the “snowball” procedure (Fig. 1). Following title and abstract screening, 305 articles were selected for full-text review. Thirty-eight studies were excluded for specific reason(s), as summarized in Supplementary Table 2. Notably, 16 studies examined fertility status in all cancer survivors without distinction of childhood hematological malignancies, and were thus excluded [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. Five eligible studies were finally selected for inclusion in the present systematic review.
The descriptive characteristics of the eligible studies are presented in Table 1. Four studies were of case-control design yielding 544 survivors of childhood hematological malignancies and 429 controls [30,31,32,33], while the fifth study was cross-sectional based on 1476 childhood leukemia survivors [34]. Two studies were conducted in the USA [31, 32], one in Germany [34], one in the UK [30], and one in the five Nordic countries (Denmark, Finland, Iceland, Norway, and Sweden) [33]. All studies were of fair quality, which was mainly compromised by the small, by necessity, sample size.
Narrative synthesis
Regarding the exposures of interest, the UK study examined the effect of chemotherapy and cranial/spinal RT on the fertility status of female survivors of childhood acute lymphoblastic leukemia (ALL; Table 1). Fertility was assessed through hormonal and biochemical measures. The results of this study showed that treatment for childhood ALL can lead to subtle ovulatory disorders in some patients, probably related to cranial radiotherapy (RT) [30].
The two studies conducted in the USA also examined the association between cranial radiotherapy (RT) used in boys and girls treated for ALL and their fertility status, which was assessed through pregnancy/birth history (Table 1). The first study showed that married men treated before the age of 10 years with high-dose cranial RT had only 9% of the fertility of controls, namely, ever fathering a pregnancy (relative ratio [RR]: 0.09, 95% CI: 0.01–0.82) [31]. By contrast, high-dose cranial RT at older ages was not associated with a significant fertility deficit (RR: 0.56, 95% CI: 0.25–1.28). In the second study, significant fertility deficits, namely, ever being pregnant, were found in female ALL survivors treated with cranial RT at any dose around the time of menarche (relative fertility: 0.27, 95% CI: 0.09, 0.82) [32].
The remaining two studies assessed the effect of chemotherapy on fertility status, as presented in Table 1. Specifically, the multicenter Nordic study from Denmark, Finland, Iceland, Norway, and Sweden examined whether childhood acute myeloid leukemia (AML) survivors treated with the NOPHO-AML-84/88/93 chemotherapy protocol had biochemical signs of reduced ovarian reserve after treatment completion or adverse pregnancy outcomes [33]. The serum levels of FSH, luteinizing hormone (LH), testosterone, estradiol, sex hormone binding globulin (SHBG), inhibin A and B, and testicular volumes were within normal ranges. Likewise, the pregnancy rates were comparable in cases and controls. By contrast, the AMH levels decreased in five of 40 post-pubertal females. Lastly, the large cross-sectional German study in 1476 leukemia survivors examined the effect of chemotherapy treatment on clinical signs of impaired fertility, such as menstruation, previous fertility testing, attempts to conceive, and pregnancy outcomes. This study showed that the frequency of suspected infertility in leukemia survivors was 25% (95% CI: 14–36%) [34].
Quantitative synthesis
The small number of identified eligible studies on our research question combined with the large heterogeneity of data on the exposure and outcome variables of interest did not allow for a quantitative synthesis of the results.
Discussion
Main findings
In the present systematic review, more than 5000 original studies were screened with the aim of assessing the fertility status of childhood hematological cancer survivors who completed treatment with chemotherapy and/or radiotherapy. Despite the abundance of evidence, only five studies examined the potential association between treatment-related factors and impaired fertility in survivors exclusively of childhood hematological malignancies. Moreover, the heterogeneity of data was such that it did not allow for a quantitative synthesis of the results. The qualitative data synthesis showed significant fertility deficits in survivors treated with cranial radiotherapy and chemotherapy for childhood leukemia. Two studies examined biochemical measures of reduced ovarian reserve, providing some evidence on the hypothesis that the levels of anti-Müllerian hormone can be used as a proxy for diminished ovarian reserve.
Effect of chemotherapy on fertility
Several chemotherapeutic agents are used in the treatment of pediatric hematological malignancies. Among these, alkylating agents are the most commonly used as primary treatment option. However, such agents have been associated with DNA damage and can induce apoptosis through covalent binding of alkyl groups to cellular macromolecules [9]. Current treatment protocols proactively restrict the cumulative doses of these agents and/or choose alkylating agents with more favorable toxicity profiles [35, 36]. It is worth mentioning that combined alkylating agents may be routinely used for the treatment of advanced stage or high-risk patients, such as the COPP (cyclophosphamide, Oncovin [vincristine], procarbazine, and prednisone) regimen used in the treatment of Hodgkin lymphoma [36].
Previous studies have calculated alkylating agent dose scores to assess their adverse health effects among childhood cancer survivors, such as secondary malignancies or impaired fertility [37]. Treatment-related factors that have been associated with these outcomes include the cumulative dose, the specific alkylating agent, the length of treatment, age at treatment, and sex [38]. Consistent with the results of the present systematic review, previous studies on all cancer survivors have also shown signs of impaired fertility in both men and women [5, 39]. Notably, men treated with combined modality therapy that includes alkylating agents and pelvic/gonadal radiation may develop subclinical Leydig cell dysfunction characterized by borderline low testosterone, elevated LH, altered body composition, and bone mineral density deficits [40, 41]. In women, depletion of follicles by alkylating agents may affect both fertility and ovarian hormone production, since ovarian hormone production is directly linked to the maturation of primordial follicles [42]. Although girls usually maintain ovarian function with higher cumulative alkylating agent doses compared to boys, the risk of acute ovarian failure and premature menopause rises if treatment includes combined modality therapy with alkylating agent chemotherapy and abdominal/pelvic radiation or dose-intensive alkylating agents for myelo-ablative conditioning before hematopoietic stem cell transplantation [42,43,44].
Effect of radiotherapy on fertility
Cranial RT impairs hypothalamic-pituitary (HPT) gonadal axis function in a dose-related manner. Treatment-related factors involve the treatment volume, total dose, fractionation schedule, and age at treatment [45]. Historically, cranial RT at doses of 18 to 24 Gy was used to treat or prevent childhood central nervous system leukemia. Such doses were associated with altered pubertal timing (early, precocious, or rapid tempo) [45]. The present systematic review identified two studies that examined the effect of cranial RT on the fertility status of boys and girls, respectively, showing significant fertility deficits in both genders compared to healthy sibling controls.
Beyond cranial RT, other RT sites have also been significantly associated with impaired fertility in childhood hematological cancer survivors. In particular, primary gonadal injury in men treated for childhood hematological malignancies may occur when RT fields include the pelvis, gonads, or total body [46]. Moreover, sperm production is reduced in a dose-dependent fashion following RT. Notably, RT doses of 1 to 3 gray (Gy) usually induce reversible azoospermia, but higher doses (>3 Gy) may result in irreversible azoospermia [39, 46]. The radiation-induced injury to Leydig cells is associated with both the RT dose and the age at treatment. Testosterone production is typically normal in prepubertal boys treated with <12 Gy fractionated testicular RT. By contrast, gonadal failure occurs when prepubertal boys are treated with >20 Gy radiation to the testes [46]. In such cases, androgen therapy is required for masculinization. Leydig cell function is usually preserved in sexually mature males if radiation doses do not exceed 30 Gy [39, 40].
Cranial RT at doses of 18 to 24 Gy in girls may be associated with delayed adverse effects, such as decreased LH secretion, attenuated LH surge, and shorter luteal phases [44]. Short luteal phases have been linked to incipient ovarian failure and early pregnancy loss. The site of RT plays a significant role in the risk for primary gonadal injury [47]. Higher risk of primary gonadal injury exists if treatment fields include the lumbo-sacral spine, abdomen, pelvis, or total body. In addition, combined therapy including alkylating agent chemotherapy and RT in ovaries increases the risk for both acute ovarian failure and premature menopause. Prepubertal girls treated with 20 to 30 Gy abdominal radiation may fail to undergo or complete pubertal development [48]. Ovarian transposition to a region that is lateral or medial to the planned radiation volume may preserve ovarian function in young girls and adolescents who require pelvic radiation therapy for lymphoma [47, 48].
Strengths and limitations
The extensive literature search of almost 5000 articles and the systematic review process are considered to be the strengths of the present study. However, we should acknowledge that the systematic review of fertility status in childhood cancer survivors is a rather challenging field of research, mainly due to the large heterogeneity of available evidence and several inherent limitations of the individual studies. The assessment of exposure and outcome is perhaps the most important methodological limitation of the studies. The assessment of fertility status was highly heterogeneous across different study groups, including either clinical, biochemical, or histological measures. Likewise, the outcome assessment was also heterogeneously examined. Thus, in terms of risk characterization, the existing framework including these variations in exposure and outcome assessment has made it difficult to use epidemiological evidence when evaluating fertility status in childhood hematological cancer survivors. Another limitation is the limited number of studies examining exclusively survivors of childhood hematological malignancies. Of note, 16 identified studies examined the fertility status in all cancer survivors without distinction of childhood hematological malignancies and were therefore excluded as not applicable to our research question. Moreover, several relevant studies examining exclusively childhood leukemia survivors had been published before 2001 and were also excluded from the present review to ensure comparability of treatment modalities between different studies. Lastly, owing to the rarity of childhood leukemia, cohort studies represented a minority of this literature, with case-control studies accounting for the overwhelming majority of available evidence. Case-control evidence is prone to selection bias and is less robust as regards providing support to the causality of associations.
Conclusions
Despite the large heterogeneity of published data and some inherent limitations of original studies, the present results provide some evidence that exposure to specific therapeutic agents used in the treatment of childhood hematological cancers is significantly correlated with adverse reproductive outcomes. Specifically, treatment with HPT-gonadal cranial RT and chemotherapy increases the risk of infertility in survivors of childhood hematological cancers and thus should be proactively addressed to reduce cancer-related morbidity. Whenever possible, fertility preservation measures could be implemented when planned treatment for childhood cancer is anticipated to confer a significant risk of irreversible infertility. Such information is crucial for family planning and obstetrical management. In-depth research into the long-term adverse effects of treatment for childhood hematological cancers should be encouraged including large longitudinal datasets, long follow-up, and homogeneous assessment of exposures and outcomes to enable the comparability and generalizability of the existing evidence.
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
van Dorp W, Haupt R, Anderson RA, Mulder RL, van den Heuvel-Eibrink MM, van Dulmen-den BE, Su HI, Winther JF, Hudson MM, Levine JM, Wallace WH (2018) Reproductive function and outcomes in female survivors of childhood, adolescent, and young adult cancer: a review. J Clin Oncol 36(21):2169–2180. https://doi.org/10.1200/JCO.2017.76.3441
Wingo PA, Cardinez CJ, Landis SH, Greenlee RT, Ries LA, Anderson RN, Thun MJ (2003) Long-term trends in cancer mortality in the United States, 1930-1998. Cancer 97(12 Suppl):3133–3275. https://doi.org/10.1002/cncr.11380
Font-Gonzalez A, Mulder RL, Loeffen EA, Byrne J, van Dulmen-den BE, van den Heuvel-Eibrink MM, Hudson MM, Kenney LB, Levine JM, Tissing WJ, van de Wetering MD, Kremer LC, PanCare LC (2016) Fertility preservation in children, adolescents, and young adults with cancer: quality of clinical practice guidelines and variations in recommendations. Cancer 122(14):2216–2223. https://doi.org/10.1002/cncr.30047
Clark RA, Mostoufi-Moab S, Yasui Y, Vu NK, Sklar CA, Motan T, Brooke RJ, Gibson TM, Oeffinger KC, Howell RM, Smith SA, Lu Z, Robison LL, Chemaitilly W, Hudson MM, Armstrong GT, Nathan PC, Yuan Y (2020) Predicting acute ovarian failure in female survivors of childhood cancer: a cohort study in the Childhood Cancer Survivor Study (CCSS) and the St Jude Lifetime Cohort (SJLIFE). Lancet Oncol 21(3):436–445. https://doi.org/10.1016/S1470-2045(19)30818-6
Hudson MM (2010) Reproductive outcomes for survivors of childhood cancer. Obstet Gynecol 116(5):1171–1183. https://doi.org/10.1097/AOG.0b013e3181f87c4b
Vakalopoulos I, Dimou P, Anagnostou I, Zeginiadou T (2015) Impact of cancer and cancer treatment on male fertility. Hormones (Athens) 14(4):579–589. https://doi.org/10.14310/horm.2002.1620
Anderson RA, Clatot F, Demeestere I, Lambertini M, Morgan A, Nelson SM, Peccatori F, Cameron D (2021) Cancer survivorship: reproductive health outcomes should be included in standard toxicity assessments. Eur J Cancer 144:310–316. https://doi.org/10.1016/j.ejca.2020.11.032
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, Beck LN, Brennan LV, Oktay K, American Society of Clinical O (2006) American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol 24(18):2917–2931. https://doi.org/10.1200/JCO.2006.06.5888
Michalczyk K, Cymbaluk-Ploska A (2021) Fertility preservation and long-term monitoring of gonadotoxicity in girls, adolescents and young adults undergoing cancer treatment. Cancers (Basel) 13(2):202. https://doi.org/10.3390/cancers13020202
Lutchman Singh K, Davies M, Chatterjee R (2005) Fertility in female cancer survivors: pathophysiology, preservation and the role of ovarian reserve testing. Hum Reprod Update 11(1):69–89. https://doi.org/10.1093/humupd/dmh052
van Beek RD, van den Heuvel-Eibrink MM, Laven JS, de Jong FH, Themmen AP, Hakvoort-Cammel FG, van den Bos C, van den Berg H, Pieters R, de Muinck Keizer-Schrama SM (2007) Anti-Mullerian hormone is a sensitive serum marker for gonadal function in women treated for Hodgkin’s lymphoma during childhood. J Clin Endocrinol Metab 92(10):3869–3874. https://doi.org/10.1210/jc.2006-2374
Rossi BV, Missmer S, Correia KF, Wadleigh M, Ginsburg ES (2012) Ovarian reserve in women treated for acute lymphocytic leukemia or acute myeloid leukemia with chemotherapy, but not stem cell transplantation. ISRN Oncol 2012:956190. https://doi.org/10.5402/2012/956190
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Group P-P (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Akar B, Doger E, Cakiroglu Y, Corapcioglu F, Sarper N, Caliskan E (2015) The effect of childhood cancer therapy on ovarian reserve and pubertal development. Reprod Biomed Online 30(2):175–180. https://doi.org/10.1016/j.rbmo.2014.10.010
Bath LE, Wallace WH, Shaw MP, Fitzpatrick C, Anderson RA (2003) Depletion of ovarian reserve in young women after treatment for cancer in childhood: detection by anti-Mullerian hormone, inhibin B and ovarian ultrasound. Hum Reprod 18(11):2368–2374. https://doi.org/10.1093/humrep/deg473
Brougham MF, Crofton PM, Johnson EJ, Evans N, Anderson RA, Wallace WH (2012) Anti-Mullerian hormone is a marker of gonadotoxicity in pre- and postpubertal girls treated for cancer: a prospective study. J Clin Endocrinol Metab 97(6):2059–2067. https://doi.org/10.1210/jc.2011-3180
Chemaitilly W, Li Z, Krasin MJ, Brooke RJ, Wilson CL, Green DM, Klosky JL, Barnes N, Clark KL, Farr JB, Fernandez-Pineda I, Bishop MW, Metzger M, Pui CH, Kaste SC, Ness KK, Srivastava DK, Robison LL, Hudson MM et al (2017) Premature ovarian insufficiency in childhood cancer survivors: a report from the St. Jude Lifetime Cohort. J Clin Endocrinol Metab 102(7):2242–2250. https://doi.org/10.1210/jc.2016-3723
Elchuri SV, Patterson BC, Brown M, Bedient C, Record E, Wasilewski-Masker K, Mertens AC, Meacham LR (2016) Low anti-Mullerian hormone in pediatric cancer survivors in the early years after gonadotoxic therapy. J Pediatr Adolesc Gynecol 29(4):393–399. https://doi.org/10.1016/j.jpag.2016.02.009
El-Shalakany AH, Ali MS, Abdelmaksoud AA, Abd El-Ghany S, Hasan EA (2013) Ovarian function in female survivors of childhood malignancies. Pediatr Hematol Oncol 30(4):328–335. https://doi.org/10.3109/08880018.2013.778927
George SA, Williamson Lewis R, Schirmer DA, Effinger KE, Spencer JB, Mertens AC, Meacham LR (2019) Early detection of ovarian dysfunction by anti-Mullerian hormone in adolescent and young adult-aged survivors of childhood cancer. J Adolesc Young Adult Oncol 8(1):18–25. https://doi.org/10.1089/jayao.2018.0080
Gracia CR, Sammel MD, Freeman E, Prewitt M, Carlson C, Ray A, Vance A, Ginsberg JP (2012) Impact of cancer therapies on ovarian reserve. Fertil Steril 97(1):134–140.e131. https://doi.org/10.1016/j.fertnstert.2011.10.040
Green DM, Kawashima T, Stovall M, Leisenring W, Sklar CA, Mertens AC, Donaldson SS, Byrne J, Robison LL (2009) Fertility of female survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol 27(16):2677–2685. https://doi.org/10.1200/JCO.2008.20.1541
Larsen EC, Muller J, Schmiegelow K, Rechnitzer C, Andersen AN (2003) Reduced ovarian function in long-term survivors of radiation- and chemotherapy-treated childhood cancer. J Clin Endocrinol Metab 88(11):5307–5314. https://doi.org/10.1210/jc.2003-030352
Lunsford AJ, Whelan K, McCormick K, McLaren JF (2014) Antimullerian hormone as a measure of reproductive function in female childhood cancer survivors. Fertil Steril 101(1):227–231. https://doi.org/10.1016/j.fertnstert.2013.08.052
Nielsen SN, Andersen AN, Schmidt KT, Rechnitzer C, Schmiegelow K, Bentzen JG, Larsen EC (2013) A 10-year follow up of reproductive function in women treated for childhood cancer. Reprod Biomed Online 27(2):192–200. https://doi.org/10.1016/j.rbmo.2013.04.003
Nystrom A, Morse H, Nordlof H, Wiebe K, Artman M, Ora I, Giwercman A, Henic E, Elfving M (2019) Anti-Mullerian hormone compared with other ovarian markers after childhood cancer treatment. Acta Oncol 58(2):218–224. https://doi.org/10.1080/0284186X.2018.1529423
Thomas-Teinturier C, Allodji RS, Svetlova E, Frey MA, Oberlin O, Millischer AE, Epelboin S, Decanter C, Pacquement H, Tabone MD, Sudour-Bonnange H, Baruchel A, Lahlou N, De Vathaire F (2015) Ovarian reserve after treatment with alkylating agents during childhood. Hum Reprod 30(6):1437–1446. https://doi.org/10.1093/humrep/dev060
van den Berg MH, Overbeek A, Lambalk CB, Kaspers GJL, Bresters D, van den Heuvel-Eibrink MM, Kremer LC, Loonen JJ, van der Pal HJ, Ronckers CM, Tissing WJE, Versluys AB, van der Heiden-van der Loo M, Heijboer AC, Hauptmann M, JWR T, JSE L, CCM B, van Leeuwen FE et al (2018) Long-term effects of childhood cancer treatment on hormonal and ultrasound markers of ovarian reserve. Hum Reprod 33(8):1474–1488. https://doi.org/10.1093/humrep/dey229
van Dorp W, van den Heuvel-Eibrink MM, Stolk L, Pieters R, Uitterlinden AG, Visser JA, Laven JS (2013) Genetic variation may modify ovarian reserve in female childhood cancer survivors. Hum Reprod 28(4):1069–1076. https://doi.org/10.1093/humrep/des472
Bath LE, Anderson RA, Critchley HO, Kelnar CJ, Wallace WH (2001) Hypothalamic-pituitary-ovarian dysfunction after prepubertal chemotherapy and cranial irradiation for acute leukaemia. Hum Reprod 16(9):1838–1844. https://doi.org/10.1093/humrep/16.9.1838
Byrne J, Fears TR, Mills JL, Zeltzer LK, Sklar C, Meadows AT, Reaman GH, Robison LL (2004) Fertility of long-term male survivors of acute lymphoblastic leukemia diagnosed during childhood. Pediatr Blood Cancer 42(4):364–372. https://doi.org/10.1002/pbc.10449
Byrne J, Fears TR, Mills JL, Zeltzer LK, Sklar C, Nicholson HS, Haupt R, Reaman GH, Meadows AT, Robison LL (2004) Fertility in women treated with cranial radiotherapy for childhood acute lymphoblastic leukemia. Pediatr Blood Cancer 42(7):589–597. https://doi.org/10.1002/pbc.20033
Molgaard-Hansen L, Skou AS, Juul A, Glosli H, Jahnukainen K, Jarfelt M, Jonmundsson GK, Malmros J, Nysom K, Hasle H, Nordic Society of Pediatric H, Oncology (2013) Pubertal development and fertility in survivors of childhood acute myeloid leukemia treated with chemotherapy only: a NOPHO-AML study. Pediatr Blood Cancer 60(12):1988–1995. https://doi.org/10.1002/pbc.24715
Balcerek M, Reinmuth S, Hohmann C, Keil T, Borgmann-Staudt A (2012) Suspected infertility after treatment for leukemia and solid tumors in childhood and adolescence. Dtsch Arztebl Int 109(7):126–131. https://doi.org/10.3238/arztebl.2012.0126
Brancati S, Gozzo L, Longo L, Vitale DC, Russo G, Drago F (2021) Fertility preservation in female pediatric patients with cancer: a clinical and regulatory issue. Front Oncol 11:641450. https://doi.org/10.3389/fonc.2021.641450
Minard-Colin V, Brugieres L, Reiter A, Cairo MS, Gross TG, Woessmann W, Burkhardt B, Sandlund JT, Williams D, Pillon M, Horibe K, Auperin A, Le Deley MC, Zimmerman M, Perkins SL, Raphael M, Lamant L, Klapper W, Mussolin L et al (2015) Non-Hodgkin lymphoma in children and adolescents: progress through effective collaboration, current knowledge, and challenges ahead. J Clin Oncol 33(27):2963–2974. https://doi.org/10.1200/JCO.2014.59.5827
Tucker MA, Meadows AT, Boice JD Jr, Stovall M, Oberlin O, Stone BJ, Birch J, Voute PA, Hoover RN, Fraumeni JF Jr (1987) Leukemia after therapy with alkylating agents for childhood cancer. J Natl Cancer Inst 78(3):459–464
Leroy C, Rigot JM, Leroy M, Decanter C, Le Mapihan K, Parent AS, Le Guillou AC, Yakoub-Agha I, Dharancy S, Noel C, Vantyghem MC (2015) Immunosuppressive drugs and fertility. Orphanet J Rare Dis 10:136. https://doi.org/10.1186/s13023-015-0332-8
Thomson AB, Critchley HO, Kelnar CJ, Wallace WH (2002) Late reproductive sequelae following treatment of childhood cancer and options for fertility preservation. Best Pract Res Clin Endocrinol Metab 16(2):311–334. https://doi.org/10.1053/beem.2002.0200
Ridola V, Fawaz O, Aubier F, Bergeron C, de Vathaire F, Pichon F, Orbach D, Gentet JC, Schmitt C, Dufour C, Oberlin O (2009) Testicular function of survivors of childhood cancer: a comparative study between ifosfamide- and cyclophosphamide-based regimens. Eur J Cancer 45(5):814–818. https://doi.org/10.1016/j.ejca.2009.01.002
Bramswig JH, Heimes U, Heiermann E, Schlegel W, Nieschlag E, Schellong G (1990) The effects of different cumulative doses of chemotherapy on testicular function. Results in 75 patients treated for Hodgkin’s disease during childhood or adolescence. Cancer 65(6):1298–1302. https://doi.org/10.1002/1097-0142(19900315)65:6<1298::aid-cncr2820650607>3.0.co;2-w
Johnston RJ, Wallace WH (2009) Normal ovarian function and assessment of ovarian reserve in the survivor of childhood cancer. Pediatr Blood Cancer 53(2):296–302. https://doi.org/10.1002/pbc.22012
Green DM, Sklar CA, Boice JD Jr, Mulvihill JJ, Whitton JA, Stovall M, Yasui Y (2009) Ovarian failure and reproductive outcomes after childhood cancer treatment: results from the Childhood Cancer Survivor Study. J Clin Oncol 27(14):2374–2381. https://doi.org/10.1200/JCO.2008.21.1839
Sklar CA, Mertens AC, Mitby P, Whitton J, Stovall M, Kasper C, Mulder J, Green D, Nicholson HS, Yasui Y, Robison LL (2006) Premature menopause in survivors of childhood cancer: a report from the childhood cancer survivor study. J Natl Cancer Inst 98(13):890–896. https://doi.org/10.1093/jnci/djj243
Gleeson HK, Shalet SM (2004) The impact of cancer therapy on the endocrine system in survivors of childhood brain tumours. Endocr Relat Cancer 11(4):589–602. https://doi.org/10.1677/erc.1.00779
Hahn EW, Feingold SM, Simpson L, Batata M (1982) Recovery from aspermia induced by low-dose radiation in seminoma patients. Cancer 50(2):337–340. https://doi.org/10.1002/1097-0142(19820715)50:2<337::aid-cncr2820500229>3.0.co;2-6
Oktem O, Kim SS, Selek U, Schatmann G, Urman B (2018) Ovarian and uterine functions in female survivors of childhood cancers. Oncologist 23(2):214–224. https://doi.org/10.1634/theoncologist.2017-0201
Zavras N, Siristatidis C, Siatelis A, Koumarianou A (2016) Fertility risk assessment and preservation in male and female prepubertal and adolescent cancer patients. Clin Med Insights Oncol 10:49–57. https://doi.org/10.4137/CMO.S32811
Author information
Authors and Affiliations
Contributions
MK and AK performed the literature search screening, data abstraction, and quality assessment; MK performed the narrative synthesis of the results; MK and AK drafted the initial version of the manuscript; SK conceived and designed the study. All authors drafted and critically revised the manuscript for important intellectual content, and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained from the ethics committee of the University of Athens. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 178 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karalexi, M.A., Kontogeorgi, A., Papaioannou, G. et al. Fertility status in childhood cancer survivors of hematological malignancies: a systematic review. Hormones 22, 211–221 (2023). https://doi.org/10.1007/s42000-023-00443-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-023-00443-9