Abstract
Purpose
Few studies have focused on thyroid function in children with isolated pituitary hypoplasia (IPH). The purpose of this study was to investigate thyroid function in children with short stature accompanied by IPH and evaluate the values of thyroid function for the diagnosis of IPH.
Methods
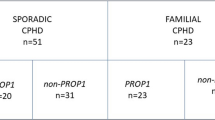
This was a retrospective observational study. A total of 100 children with short stature accompanied by IPH were enrolled. Among them, 68 children presenting with isolated growth hormone deficiency (IGHD) were chosen as the IPH group. Sixty-eight age-matched and sex-matched IGHD children without pituitary abnormalities were chosen as the control group. Clinical, hormonal, and imaging parameters were analyzed. The diagnostic value of thyroid function for IGHD children with IPH was evaluated.
Results
Children in the IPH group had significantly lower height standard deviation score (HSDS), HSDS-target height standard deviation score (THSDS), free thyroxine (FT4), insulin-like growth factor-1 standard deviation score (IGF-1SDS), and pituitary height than the control subjects (p = 0.027, p = 0.033, p < 0.001, p = 0.03, and p < 0.001, respectively). The value of the area under the curve (AUC) was 0.701 (95% CI 0.614–0.788, p < 0.001) when the cut-off value for FT4 was ≤ 16.43 pmol/L and the sensitivity and specificity were 72.1 and 61.8%, respectively. FT4 levels were positively correlated with FT3, GH peak, and IGF-1 SDS levels in all children with short stature accompanied by IPH (p < 0.001, p = 0.009, and p = 0.01, respectively).
Conclusion
IGHD children with IPH had lower FT4 levels than IGHD children without pituitary abnormalities. FT4 levels may have diagnostic value for IGHD children with IPH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The causes of short stature are various. Further medical investigation should be considered when a patient’s height is two standard deviations (SD) below the mean height for age and sex (less than the 3rd percentile). The pituitary gland is important in controlling growth and development and in regulating the functions of the other endocrine glands. Abnormal pituitary development is an important cause of short stature in children. Pituitary hypoplasia is defined as pituitary height greater than 2 SD below that of the age-matched and sex-matched population [1]. Pituitary hypoplasia may present as isolated pituitary hypoplasia (IPH) or in association with other pituitary anomalies, such as pituitary stalk interruption syndrome (PSIS), this disorder being characterized by a classic triad of a very thin or absent pituitary stalk, anterior pituitary hypoplasia or aplasia, and an ectopic posterior pituitary. In contrast, IPH shows only a morphogenetic defect and is not accompanied by the other morphologic abnormalities found in PSIS. The most frequent pituitary abnormality is IPH [2], which usually presents with isolated growth hormone deficiency (IGHD). PSIS often presents with multiple pituitary hormone deficiency (MPHD). The incidence of IPH has been observed to be higher than that of PSIS among patients with growth hormone deficiency (GHD) accompanied by hypothalamic-pituitary abnormalities [3]. However, IPH also affects thyroid function in addition to growth hormone (GH) levels [4]. Moreover, it was reported that 5.1% of patients with IGHD at baseline eventually developed MPHD during the course of follow-up [3].
Early diagnosis and appropriate treatment are important for children with IPH, with magnetic resonance imaging (MRI) often proving to be a useful diagnostic tool for detecting abnormalities of hypothalamic-pituitary structures. However, MRI scans are not always effective in IGHD children for several reasons. First, pituitary shape and size vary among normal subjects of identical age and gender and even in the same subject at different stages [5]. Thus, it is difficult to distinguish between IPH and a pituitary with delayed development using MRI. Second, in IGHD children with growth hormone-releasing hormone receptor (GHRHR) mutations, pituitary MRI is generally normal at a young age [6], the height of the anterior pituitary tending to increase during puberty [7]. The size of the anterior pituitary in patients with gene mutations usually evolves over time. Third, MRI scans are reviewed by different radiologists, which may lead to inconsistent results, while IPH may be neglected by radiologists [8]. It is therefore important to find indicators that can be combined with MRI for the diagnosis of IPH.
Most studies that have examined the GH-insulin-like growth factor 1 (IGF-1) axis in GHD children with pituitary hypoplasia showed that GH secretion is closely related to pituitary height [1, 8]. There are many studies in children with complex pituitary hypoplasia such as PSIS [4, 9]. However, 63% of IPH patients showed normal GH levels [1]. Few studies have focused on the hypothalamic-pituitary-thyroid (HPT) axis and on the significance of thyroid function in children with IPH. Therefore, the purpose of this study was to investigate thyroid function in children with short stature accompanied by IPH and to evaluate the value of thyroid function for the diagnosis of IPH.
Materials and methods
Study subjects
This was a retrospective observational study. The study included children with short stature accompanied by IPH and was conducted from 2014 to 2018 in our Department of Pediatric Endocrinology, Linyi People’s Hospital, Linyi, Shandong Province, China. A total of 100 children who fulfilled the following criteria were enrolled: height less than the 3rd percentile and pituitary height less than − 2 SD compared to the age-matched and sex-matched population [10]. Patients with autoimmune thyroid disease and other systemic illnesses and endocrinological diseases were excluded. No patient had received any thyroid hormone replacement therapy. Among children with short stature accompanied by IPH, 68 children presented with IGHD (39 boys and 29 girls; mean age, 6.30 ± 3.83 years) and 15 children presented with MPHD (10 boys and 5 girls; mean age, 6.92 ± 5.76 years), while 17 children showed no pituitary hormone deficiencies (12 boys and 5 girls; mean age, 4.85 ± 3.19 years). Most of the children with short stature accompanied by IPH presented with IGHD and were chosen as the IPH group. Sixty-eight age-matched and sex-matched IGHD children without pituitary abnormalities (42 boys and 26 girls; mean age, 6.96 ± 3.18 years) were enrolled as controls (control group).
Study protocol
The following parameters were collected at baseline: birth history, chronological age (CA), height, height standard deviation score (HSDS), parental heights, target height standard deviation score (THSDS), HSDS-THSDS, weight, body mass index (BMI), BMI standard deviation score (BMISDS), free triiodothyronine (FT3), free thyroxine (FT4), thyrotropin (TSH), IGF-1, IGF-1 standard deviation score (IGF-1SDS), GH peak, bone age (BA), BA-CA, and pituitary height. Clinical, hormonal, and imaging parameters were compared between the IPH group and the control group. The diagnostic value of thyroid function for IGHD children with IPH was evaluated. The correlations between thyroid hormones and other parameters in all children with short stature accompanied by IPH were analyzed.
Levothyroxine sodium treatment was added when the FT4 level was below the lowest third of the normal range (≤ 15.2 pmol/L) at baseline and during follow-up. Thyroid function was reassessed every 3 months after recombinant human GH (rhGH) therapy. The following data of children in the two groups who underwent rhGH treatment and were followed up for 1 year were recorded: first-year height velocity, first-year HSDS gain, and the number of children without thyroxine therapy whose FT4 level was more than 15.2 pmol/L. The study was approved by the Ethics Committee of the Linyi People’s Hospital. All participants’ parents gave informed written consent.
Methods
Height and weight were measured to the nearest 0.1 cm and 0.1 kg, respectively, with the subject dressed only in light underwear without shoes. Target height was calculated using the following equation: target height = [father’s height (cm) + mother’s height (cm) + 13 cm (boys) or − 13 cm (girls)]/2. BMI was calculated as weight in kilograms divided by height in meters squared. HSDS, THSDS, and BMISDS were calculated based on Chinese standards [11].
Serum FT3, FT4, and TSH levels were measured with an automated chemiluminescent immunoassay system (Advia Centaur, Siemens, Healthcare Diagnostics, USA). Reference ranges were 3.5–6.5 pmol/L for FT3, 11.5–22.7 pmol/L for FT4, and 0.35–5.5 mIU/L for TSH. The sensitivity of FT3, FT4, and TSH was 0.3 pmol/L, 1.3 pmol/L, and 0.001 mIU/L, respectively. The intra-assay and inter-assay coefficients of variation were less than 3.0 and 4.0%, respectively. Serum IGF-1 level was measured by chemiluminescence assay (IMMULITE 2000, Siemens, Healthcare Diagnostics, USA). Sensitivity was 20 ng/mL. The intra-assay and inter-assay coefficients of variation were less than 4.0 and 4.0%, respectively. IGF-1 SDS was calculated according to a matched normal population of the same age and gender to minimize the confounding effects of age and sex [12]. Serum GH level was measured using chemiluminescence assay (Cobas E170, Roche Diagnostics, Germany). The sensitivity of GH was 0.1 ng/mL. The intra-assay and inter-assay CVs for the assays were < 4.0 and < 5.0%, respectively. GH secretion was determined at 0, 30, 60, 90, 120, and 150 min after two stimulation tests (arginine test and levodopa test). GH peak > 10 ng/mL should be considered normal.
BA was determined by radiograph of the left hand and wrist according to the method of Greulich and Pyle. BA-CA was calculated. Pituitary MRI was performed using a 3.0-T scanner (Siemens, Erlangen, Germany) in the sagittal and coronal planes on T1-weighted and T2-weighted imaging with 3-mm slice thickness. The height of the pituitary gland was recorded.
Statistical analysis
Normality of variable data was assessed using the Kolmogorov–Smirnov test. All measurement data were normally distributed. Normally distributed variables were expressed as the mean ± standard deviation (mean ± SD). Two independent-sample t tests were used to compare differences between the IPH group and the control group. Categorical variables were compared using the chi-square test. A receiver operating characteristic (ROC) curve was constructed and the area under the curve (AUC) was calculated to predict the presence of IPH. Pearson’s correlations were used for parametric variables. Paired data before and after treatment were analyzed with parametric tests (paired t tests). Data analysis was performed using the standard computer software SPSS version 19.0 (SPSS Inc. Chicago, USA). A two-tailed p-value < 0.05 was considered statistically significant.
Results
Gestational age, modes of delivery, and small for gestational age (SGA) data were recorded. In the IPH group and the control group, the proportion of full-term age was 97.1 and 95.6%, and preterm age was 2.9 and 4.4%, respectively; the proportion of vaginal delivery was 54.4 and 58.8%; cesarean section delivery was 44.1 and 39.7%; emergency delivery was 1.5 and 0%; breech delivery was 0 and 1.5%, respectively; and the proportion of SGA was 11.8 and 8.8%, respectively. There were no significant differences in the proportion of gestational age, modes of delivery, and SGA between the two groups (all p > 0.05). In all children with short stature accompanied by IPH (61 boys and 39 girls; mean age, 6.14 ± 4.08 years), the proportion of full-term age was 95.0%, preterm age was 5.0%, vaginal delivery was 55.0%, cesarean section delivery was 43%, emergency delivery was 1.0%, footling breech delivery was 1.0%, and SGA was 16.2%.
In the IPH group, the patients had significantly lower HSDS, HSDS-THSDS, FT4, IGF-1SDS, and pituitary height than the control subjects (p = 0.027, p = 0.033, p < 0.001, p = 0.03, and p < 0.001, respectively). There were no significant differences in sex, age, BA, BA-CA, THSDS, BMISDS, FT3, TSH, and GH peak between the IPH group and the control group (all p > 0.05) (Table 1). In all children with short stature accompanied by IPH, the mean HSDS was − 2.72 ± 1.07, mean THSDS was − 0.51 ± 0.76, mean HSDS-THSDS was − 2.21 ± 1.22, mean BMISDS was − 0.28 ± 1.29, mean BA 4.74 ± 3.60 years, mean BA-CA was − 1.41 ± 1.68 year, mean FT3 level was 5.98 ± 1.09 pmol/L, mean FT4 level was 15.59 ± 3.49 pmol/L, mean TSH level was 3.07 ± 1.43 mIU/L, mean GH peak level was 6.66 ± 5.47 μg/L, and mean IGF-1SDS was − 1.46 ± 2.06. At baseline, FT4 levels below the lowest third of the normal range were found in 38 children with short stature accompanied by IPH (38.0%). The relations between all parameters were analyzed. FT4 levels were positively correlated with FT3, GH peak, and IGF-1SDS levels (p < 0.001, p = 0.009, and p = 0.01, respectively) (Fig. 1).
Correlations between FT4 level and GH peak and IGF-1 SDS levels. FT4 level was positively correlated with GH peak level (r = 0.258, p = 0.009) and IGF-1 SDS level (r = 0.255, p = 0.01), respectively. FT4 free thyroxine, GH peak growth hormone peak, and IGF-1 SDS insulin-like growth factor 1 standard deviation score
ROC curves were used to evaluate FT4 and IGF-1SDS for the identification of IPH. The AUC indicated the clinical usefulness of FT4 and IGF-1SDS diagnostic power. The value of the AUC was 0.701 (95% CI 0.614–0.788, p < 0.001), when the cut-off value for FT4 was ≤ 16.43 pmol/L and the sensitivity and specificity were 72.1 and 61.8%, respectively (Fig. 2). The value of the AUC for IGF-1SDS was 0.583 (95% CI 0.487–0.679, p = 0.096).
ROC curve for FT4 level in predicting IPH. The value of the AUC was 0.701 (95% CI 0.614–0.788, p < 0.001) when the cut-off value for the FT4 was ≤ 16.43 pmol/L and the sensitivity and specificity were 72.1% and 61.8%, respectively. Abbreviations: ROC: receiver operating characteristic; AUC: area under the curve; FT4: free thyroxine; IPH: isolated pituitary hypoplasia
In the IPH group, 10 children did not receive rhGH therapy and 10 children were lost to follow-up. Forty-eight children completed the first-year follow-up. In the control group, there were 17 children who did not receive rhGH therapy and six children who were lost to follow-up. Forty-five children completed the first-year follow-up. At baseline, the number of FT4 levels ≤ 15.2 pmol/L in the IPH group (n = 19) was higher than that in the control group (n = 8) (p = 0.021). After 3 months, 6 months, 9 months, and 12 months of rhGH therapy, the number of children without thyroxine therapy whose FT4 > 15.2 pmol/L in the IPH group was lower than that in the control group (p = 0.021, p = 0.011, p = 0.002, and p = 0.009, respectively). There were two children (4.2%) who developed secondary hypothyroidism in the IPH group during the first-year rhGH therapy. Central hypothyroidism was not found in the control group. First-year height velocity and first-year HSDS gain showed no significant difference between the two groups (both p > 0.05) (Table 2).
Discussion
In this study, we investigated clinical, hormonal, and imaging parameters in the IPH group and the control group, evaluated the diagnostic value of FT4 for the identification of IGHD children with IPH, and analyzed the correlations between FT4 level and other parameters in 100 children with short stature accompanied by IPH. We found that IGHD children with IPH exhibited a lower level of FT4 than IGHD children without pituitary abnormalities. The cut-off value of FT4 level for the diagnosis of IPH was no more than 16.43 pmol/L. Sensitivity and specificity were 72.1 and 61.8%, respectively. Serum FT4 levels were positively correlated with serum GH peak and IGF-1 levels.
In a prior study, no apparent differences in breech presentation, cesarean section, or birth weight SDS were reported between GHD children with IPH and without pituitary abnormalities, although the author did not provide statistical data [13]. Our data also demonstrated that there was no significant difference in birth history between the IPH group and the control group. Molecular defects in genes may shed light on the pathogenesis of IPH [14].
Deal et al. reported that patients with IPH had lower levels of baseline HSDS, HSDS-THSDS, IGF-1SDS, and GH peaks than patients with idiopathic GHD [3]. Our findings are consistent with those of their study, with the exception of the peak value of GH. There was no difference in the peak value of GH between the IPH group and the control group. This may be due to inherent differences in subjects. In their study, 24.4% of patients with IPH had MPHD. However, there was no child who had MPHD in our IPH group. Children with MPHD have more severe GHD [15]. In addition, discrepancies between GH and IGF-1 secretion have been found in many studies. GH sensitivity is different in individuals, and the results of GH provocation tests are not always consistent with GH secretion [16].
FT4 levels may be helpful in distinguishing congenital central hypothyroidism from mild congenital thyroidal hypothyroidism [17]. Structural hypothalamic-pituitary abnormalities could affect the function of the HPT axis, resulting in central hypothyroidism, which is characterized by insufficient TSH secretion and low levels of thyroid hormones. In this case, FT4 concentrations are low, whereas TSH concentrations may be low, normal, or even slightly elevated. The FT4 level is more sensitive than the TSH level in the assessment of central hypothyroidism [18]. However, in most patients with central hypothyroidism, thyroid function may range from mild to moderately severe. FT4 levels may also be at a low-normal level in central hypothyroidism [19]. In our study, FT4 levels in the IPH group were lower than those in the control group within the normal range. It has been reported that central hypothyroidism should be taken into account in patients with pituitary abnormalities when FT4 levels decrease by more than 20% along with low or normal TSH levels during follow-up [20]. In addition, low FT4 levels at initiation of rhGH therapy are a predictor of the presence of structural pituitary abnormalities and the diagnosis of MPHD in children with IGHD [21]. Our results revealed an additional role of FT4, pointing strongly to the predictive value of FT4 for the early diagnosis of IPH. References for serum FT4 level at baseline and targets of serum FT4 level during rhGH therapy in IGHD children have not been defined [22], nor, importantly, those in IGHD children with IPH. The present study demonstrated that the cut-off value of FT4 ≤ 16.43 pmol/L was adequate for the early diagnosis of IPH, thus providing a preliminary reference for clinical practice.
Positive correlations were found between FT4 level and values of GH peak and IGF-1 in this study, our findings being consistent with those of previous reports [23]. Pituitary hypoplasia can affect both the GH-IGF-1 axis and HPT axis, thereby interfering with GH and TSH secretion and resulting in decreased IGF-1 and FT4 levels [24]. Moreover, thyroid hormone can stimulate the expression of the IGF-1 receptor, presenting with low IGF-1 levels in hypothyroidism [25]. FT4 level was not correlated with pituitary height in our study. This is probably because thyrotropes are the least abundant cell type, amounting to approximately 5–8% of all the anterior pituitary cells, and are rarely completely depleted [26].
Deal et al. also reported that the ratio of males to females was approximately 2:1 in patients with pituitary abnormalities, with 24.4% of patients exhibiting MPHD. In their study, the mean levels of HSDS were − 2.7 (− 3.5 to − 2.1), HSDS-THSDS was − 2.4 (− 3.3 to − 1.6), GH peak was 4.2 (1.3 to 6.5), and IGF-1SDS was − 2.4 (− 4.5 to − 1.5). First-year growth velocity was 8.5 (6.7 to 10.5) cm and first-year HSDS gain was 0.5 (0.2 to 0.9) [3]. In our study, the ratio of boys to girls with IPH was 61:39, similar to that of other reports [27]. The incidence of children with IPH who exhibited MPHD was 15.0%, while it was 9.1% in another report [28]. Mean values of HSDS, HSDS-THSDS, GH peak, and IGF-1SDS in our study were slightly higher than those in the above studies, as our series included children with IPH who showed normal GH secretion. First-year growth velocity was 8.94 ± 1.85 cm, similarly to their result, while first-year HSDS gain (0.39 ± 0.46) was slightly lower than that in their study, this possibly being due to higher height gain in children with MPHD than in children with IGHD [3].
rhGH therapy increases the conversion of T4 to T3, leading to hypothyroidism [29]. Growth hormone deficiency may mask central hypothyroidism. It was reported that 41% of patients tended to present with new deficiencies within the first year of rhGH treatment. The conversion time lasted up to 6 years (mean 2.1 ± 0.93 year). Central hypothyroidism was the most frequently recorded new deficiency (25.0%), followed by central hypogonadism (13.0%) and hypoadrenalism (12.0%) [30]. In the present study, there were only two children (4.2%) with central hypothyroidism during the first year of rhGH therapy in the IPH group. One reason was that thyroxine was added when the FT4 level was below the lowest third of the normal range during our follow-up. Another possible explanation was that our duration of follow-up was relatively short [31].
However, our study has some potential limitations. First, pituitary height may not fully reflect the degree of pituitary hypoplasia. The volume of the pituitary could not be measured in this study due to the limited equipment conditions. Second, the follow-up time was relatively short. Third, this was a retrospective study. Many patients did not receive rhGH therapy and were lost to follow-up.
Conclusion
In conclusion, our results showed that IGHD children with IPH had lower FT4 levels than IGHD children without pituitary abnormalities. The cut-off value of FT4 ≤ 16.43 pmol/L was adequate for the early diagnosis of IPH. FT4 levels were positively correlated with GH peak and IGF-1 levels. It was thus determined that FT4 has predictive value for the early diagnosis of IPH. In future studies, larger prospective and well-controlled clinical trials are required to further confirm our current findings.
References
Nagel BH, Palmbach M, Petersen D, Ranke MB (1997) Magnetic resonance images of 91 children with different causes of short stature: pituitary size reflects growth hormone secretion. Eur J Pediatr 156(10):758–763
Pampanini V, Pedicelli S, Gubinelli J, Scirè G, Cappa M, Boscherini B, Cianfarani S (2015) Brain magnetic resonance imaging as first-line investigation for growth hormone deficiency diagnosis in early childhood. Horm Res Paediatr 84(5):323–330
Deal C, Hasselmann C, Pfäffle RW, Zimmermann AG, Quigley CA, Child CJ, Shavrikova EP, Cutler GB Jr, Blum WF (2013) Associations between pituitary imaging abnormalities and clinical and biochemical phenotypes in children with congenital growth hormone deficiency: data from an international observational study. Horm Res Paediatr 79(5):283–292
Beck-Peccoz P, Rodari G, Giavoli C, Lania A (2017) Central hypothyroidism-a neglected thyroid disorder. Nat Rev Endocrinol 13(10):588–598
Delman BN, Fatterpekar GM, Law M, Naidich TP (2008) Neuroimaging for the pediatric endocrinologist. Pediatr Endocrinol Rev 5(Suppl 2):708–719
Alba M, Hall CM, Whatmore AJ, Clayton PE, Price DA, Salvatori R (2004) Variability in anterior pituitary size within members of a family with GH deficiency due to a new splice mutation in the GHRH receptor gene. Clin Endocrinol (Oxf) 60(4):470–475
Shohreh R, Sherafat-Kazemzadeh R, Jee YH, Blitz A, Salvatori R (2011) A novel frame shift mutation in the GHRH receptor gene in familial isolated GH deficiency: early occurrence of anterior pituitary hypoplasia. J Clin Endocrinol Metab 96(10):2982–2986
Zhang S, Cheng Y, Wang G, Feng Y (2017) Physical development of pituitary and pituitary hypoplasia in children from neonate to adolescent: MRI assessment and comparison. Int J Clin Exp Med 10(4):6360–6368
Li G, Shao P, Sun X, Wang Q, Zhang L (2010) Magnetic resonance imaging and pituitary function in children with panhypopituitarism. Horm Res Paediatr 73(3):205–209
Guangwu L, Tao Z, Ning Y, Feng C, Yifan S, Jieying D, Luodong Z, Yayun J (2005) MRI study of normal pituitary gland in stage of puberty. Chin J Radiol 39(10):1022–1027
Li H, Ji C, Zong X, Zhang Y (2009) Height and weight standardized growth charts for Chinese children and adolescents aged 0 to 18 ys. Chin J Pediatr 7(7):487–492
Isojima T, Shimatsu A, Yokoya S, Chihara K, Tanaka T, Hizuka N, Teramoto A, Tatsumi KI, Tachibana K, Katsumata N, Horikawa R (2012) Standardized centile curves and reference intervals of serum insulin-like growth factor-I (IGF-I) levels in a normal Japanese population using the LMS method. Endocr J 59(9):771–780
Child C, Leger J, Deal C, Benabbad I, Jia N, Blum W (2019) Birth and perinatal characteristics of children with congenital GH deficiency (GHD) due to abnormal pituitary development: data from a prospective, multinational observational study. J Endocr Soc 3(Suppl 1):SUN-244
Elizabeth M, Hokken-Koelega ACS, Schuilwerve J, Peeters RP, Visser TJ, de Graaff LCG (2018) Genetic screening of regulatory regions of pituitary transcription factors in patients with idiopathic pituitary hormone deficiencies. Pituitary 21(1):76–83
Sahakitrungrueng T, VichitSupornsilchai MD (2015) Growth hormone (GH) retesting and final adult height in childhood-onset GH deficiency (CO-GHD): experiences from King Chulalongkorn Memorial Hospital. Thailand J Med Assoc Thai 98(6):542–548
Smyczyńska J, Stawerska R, LewińskiA HM (2011) Do IGF-I concentrations better reflect growth hormone (GH) action in children with short stature than the results of GH stimulating tests? Evidence from the simultaneous assessment of thyroid function. Thyroid Res 4(1):6
Zwaveling-Soonawala N, van Trotsenburg ASP, Verkerk PH (2018) TSH and FT4 concentrations in congenital central hypothyroidism and mild congenital thyroidal hypothyroidism. J Clin Endocrinol Metab 103(4):1342–1348
Gangat M (2017) Radovick S (2017) Pituitary hypoplasia. Endocrinol MetabClin 46(2):247–257
Persani L, Brabant G, Dattani M, Bonomi M, Feldt-Rasmussen U, Fliers E, Gruters A, Maiter D, Schoenmakers N, van Trotsenburg ASP (2018) 2018 European Thyroid Association (ETA) Guidelines on the diagnosis and management of central hypothyroidism. Eur Thyroid J7(5):225–237
Alexopoulou O, Beguin CL, De Nayer PH, Maiter D (2004) Hypothyroidism at diagnosis and during follow-up in adult patients. Eur J Endocrinol 150(1):1–8
van Iersel L, van Santen HM, Zandwijken GRJ, Zwaveling-Soonawala N, Hokken-Koelega ACS, van Trotsenburg ASP (2018) Low FT4 concentrations around the start of recombinant human growth hormone treatment: predictor of congenital structural hypothalamic-pituitary abnormalities? Horm Res Paediatr 89(2):98–107
Martins MR, Doin FC, Komatsu WR, Barros-Neto TL, Moises VA, Abucham J (2007) Growth hormone replacement improves thyroxine biological effects: implications for management of central hypothyroidism. J Clin Endocrinol Metab 92(11):4144–4153
Takamizawa T, Horiguchi K, Nakajima Y, Okamura T, Ishida E, Matsumoto S, Yoshino S, Yamada E, Saitoh T, Ozawa A, Tosaka M, Yamada S, Yamada M (2019) Central hypothyroidism related to pituitary adenomas: low incidence of central hypothyroidism in patients with acromegaly. J Clin Endocrinol Metab 104(10):4879–4888
Wang L, Shao YY, Ballock RT (2010) Thyroid hormone-mediated growth and differentiation of growth plate chondrocytes involves IGF-1 modulation of beta-catenin signaling. J Bone Miner Res 25(5):1138–1146
Purandare A, Co Ng L, Godil M, Ahnn SH, Wilson TA (2003) Effect of hypothyroidism and its treatment on the IGF system in infants and children. J Pediatr Endocrinol Metab 16(1):35–42
Villalobos C, Núñez L, García-Sancho J (2004) Anterior pituitary thyrotropes are multifunctional cells. Am J Physiol Endocrinol Metab 287(6):E1166-1170
Grimberg A, Stewart E, Wajnrajch MP (2008) Gender of pediatric recombinant human growth hormone recipients in the United States and globally. J Clin Endocrinol Metab 93(6):2050–2056
AlJurayyan RNA, AlJurayyan NAM, Omer HG, Alissa SDA, AlOtaibi HMN, AlKhalifah RAH, Babiker AMI, Mohamed S (2017) Pituitary imaging in 129 children with growth hormone deficiency: a spectrum of findings. Sudan J Paediatr 17(1):30–35
Filipsson H, Johannsson G (2009) GH replacement in adults: interactions with other pituitary hormone deficiencies and replacement therapies. Eur J Endocrinol 161(Suppl 1):S85-95
Klose M, Jonsson B, Abs R, Popovic V, Koltowska-Häggström M, Saller B, Feldt-Rasmussen U, Kourides I (2009) From isolated GH deficiency to multiple pituitary hormone deficiency: an evolving continuum-a KIMS analysis. Eur J Endocrinol 161(Suppl 1):S75-83
Rose SR (2010) Improved diagnosis of mild hypothyroidism using time-of-day normal ranges for thyrotropin. J Pediatr 157(4):662–667
Acknowledgements
We gratefully acknowledge the support of the children and their parents who were involved in this study.
Funding
This study was supported by the Science and Technology Development Program of Linyi City (202020003) and Shandong Provincial Natural Science Foundation (ZR2020MH102).
Author information
Authors and Affiliations
Contributions
Dr. Yanyan Hu was responsible for the study execution, patient screening and enrolment, data collection and analysis, and writing of the manuscript. Prof. Xuemei Sun conceived and designed the study, supervised the execution of the study, and performed the final data analyses. Dr. Liping Zhu and Qiang Liu participated in patient screening and enrolment, and contributed to the writing of the manuscript. Dr. Yongzhen Xue contributed significantly to the revision of the manuscript. Prof. Guimei Li contributed significantly to the revision of the manuscript and provided funding for the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All procedures performed involving human participants were approved by the Ethics Committee of Linyi People’s Hospital, Linyi, Shandong Province, China and in accordance with the 1964 Declaration of Helsinki and its later amendments. This article does not contain any studies with animals performed by any of the authors. Our study was approved by the Pediatric Department of Linyi People’s Hospital.
Informed consent
All participants provided an informed consent before participating in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yanyan Hu, Xuemei Sun and Guimei Li contributed equally to this work and should be considered co-corresponding authors.
Rights and permissions
About this article
Cite this article
Hu, Y., Zhu, L., Liu, Q. et al. Thyroid function in children with short stature accompanied by isolated pituitary hypoplasia. Hormones 20, 707–713 (2021). https://doi.org/10.1007/s42000-021-00323-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-021-00323-0