Abstract
Purpose
To investigate the association between vision and hearing impairment and falls in community-dwelling adults aged ≥ 50 years.
Methods
This is a prospective study on 50,986 participants assessed in Waves 6 and 7 of the Survey of Health, Ageing and Retirement in Europe. At baseline, we recorded socio-demographic data, clinical factors and self-reported vision and hearing impairment. We classified participants as having good vision and hearing, impaired vision, impaired hearing or impaired vision and hearing. We recorded falls in the six months prior to the baseline and 2-year follow-up interviews. The cross-sectional and longitudinal associations between vision and hearing impairment categories and falls were analysed by binary logistic regression models; odds ratios (OR) and 95% confidence intervals (CI) were calculated. All analyses were adjusted for socio-demographic and clinical factors.
Results
Mean age was 67.1 years (range 50–102). At baseline, participants with impaired vision, impaired hearing, and impaired vision and hearing had an increased falls risk (OR (95% CI)) of 1.34 (1.22–1.49), 1.34 (1.20–1.50) and 1.67 (1.50–1.87), respectively, compared to those with good vision and hearing (all p < 0.001). At follow-up, participants with impaired vision, without or with impaired hearing, had an increased falls risk of 1.19 (1.08–1.31) and 1.33 (1.20–1.49), respectively, compared to those with good vision and hearing (both p < 0.001); hearing impairment was longitudinally associated with falls in middle-aged women.
Conclusion
Vision impairment was cross-sectionally and longitudinally associated with an increased falls risk. This risk was highest in adults with dual sensory impairment.
Key summary points
To investigate the relationship between self-reported vision and hearing impairment and falls risk in community-dwelling adults aged ≥ 50 years in the cross-national Survey of Health, Ageing and Retirement in Europe (SHARE).
AbstractSection FindingsSelf-reported vision impairment, versus no impairment, was cross-sectionally and longitudinally associated with an increased falls risk in adults, independent of age, sex, self-rated health, co-morbidities and medications. The risk was highest when vision and hearing impairment coincided.
AbstractSection MessageSimple questions on self-reported sensory impairment can be used to assess the risk of falls in adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vision impairment [1, 2], hearing impairment [1, 3, 4] and falls [5,6,7,8,9] are common among adults, with their prevalence increasing with age. About one in three older adults fall each year [5] and 5–10% of falls leads to a major injury [6, 7, 9]. In this way, falls are a serious public health issue, leading to increased morbidity, mortality, institutionalisation and health care cost [8, 9]. Both injurious and non-injurious falls can result in fear of falling, reduced quality of life, loss of confidence and independence [9]. Therefore, identifying potentially modifiable and common risk factors for falls is crucial.
Vision impairment has been associated with an increased falls risk [5, 9, 10]. However, previous reports examining the association between objective measures of vision components and falls risk have yielded conflicting results [5, 9,10,11,12,13,14,15] partly because vision includes many components, such as visual acuity, visual field, depth perception and contrast sensitivity [11,12,13,14,15]. In the Blue Mountains Eye Study, poor visual acuity was associated with an increased falls risk among adults aged 49 years and older [13]; however, this association was not linear and might have been mediated by reduced depth perception [9, 11]. Indeed, reduced depth perception has been prospectively associated with recurrent falls [9, 12]. In the Blue Mountains Eye Study and in the Los Angeles Latino Eye Study, visual field impairments were associated with an increased falls risk [13, 14]; yet, diseases known to affect the visual field and acuity, such as macular degeneration, were not [13]. Moreover, a few studies suggested that contrast sensitivity may be more important than visual acuity in predicting falls [11]. On the other hand, self-reported vision—as assessed by simple, brief, inexpensive questions—could be a global measure of all vision components and may predict falls risk beyond visual acuity [15]. Yet, few prospective studies have investigated the association between self-reported vision and falls risk in adults [16,17,18,19,20]. Hearing impairment has also been associated with an increased falls risk [10]. Auditory inputs contribute to spatial awareness [21]; in contrast, hearing impairment has been correlated with greater postural instability and falls [21,22,23]. Adults with hearing impairment may invest more attentional and cognitive resources into hearing, leaving fewer resources available for balance control [22]. In addition, hearing impairment often coincides with vestibular impairment [22]. Yet, the association between hearing and falls is still controversial [10, 18,19,20,21,22,23,24,25,26,27,28,29,30]. Moreover, few studies on this association were longitudinal [18,19,20, 23, 25, 26, 28,29,30] or examined self-reported hearing [18,19,20, 27, 29]. Furthermore, few studies have examined the effect of dual sensory impairment—vision and hearing impairment—on falls risk [28,29,30]. Yet, dual sensory impairment will become more common with the ageing of the population worldwide [1,2,3,4]. At present, dual sensory impairment affects about 8% of community-dwelling Americans aged 70 years or older [31]. Moreover, with an increasing trend towards virtual consultations, these impairments will be more frequently assessed by self-report in the future.
The aim of this study was to examine whether visual and hearing impairment, either alone or together, were cross-sectionally and longitudinally associated with risk of falls in community-dwelling men and women aged 50 years and older, independent of self-rated health, co-morbidities and medications.
Methods
Study design and population
The Survey of Health, Ageing and Retirement in Europe (SHARE) is a multidisciplinary and cross-national panel database of microdata on health, socio-economic status and social and family networks of individuals aged 50 years and older in European countries and Israel [32]. Started in 2004, SHARE comprises eight biennial survey waves. We conducted a prospective study using data from Waves 6 and 7 of SHARE [33, 34].
At baseline (Wave 6), 68,186 participants had a main interview. We excluded those younger than 50 years or of unknown age (n = 1015), those resident in a nursing home or unknown (n = 772) and those with missing data on either vision or hearing function (n = 206), or use of hearing aids or glasses (n = 5), or falls at baseline (n = 15) or other covariates (n = 93). At follow-up (Wave 7), we further excluded 15,094 participants who did not have a main interview (n = 14,779) or data on falls (n = 315).
Therefore, this study includes 50,986 participants, aged 50 years or older at baseline (Wave 6), who were followed up (Wave 7) and had complete data of interest. These participants were residents from 18 countries (Austria, Belgium, Croatia, Czech Republic, Denmark, Estonia, France, Germany, Greece, Israel, Italy, Luxembourg, Poland, Portugal, Slovenia, Spain, Sweden and Switzerland). Figure 1 details the flow-chart of study inclusion criteria.
Those 15,094 participants who were lost to follow-up between Waves 6 and 7 were older, more likely to be men, and report falls and vision impairment, with or without hearing impairment, at baseline, compared to those 50,986 participants who were included in our study (Supplementary Table 1).
Demographic and clinical characteristics
Baseline interviews (Wave 6) were carried out from January to November 2015 and the following variables were collected: age, sex, self-rated health, self-reported co-morbidities, medications and falls.
Self-rated health was assessed by asking the participants: “Would you say your health is …”; options were: “excellent”, “very good”, “good”, “fair” or “poor”. We dichotomised self-rated health as good (“excellent” or “very good” or “good”) versus poor (“fair” or “poor”).
Co-morbidities were assessed by asking the participants: “Has a doctor ever told you that you had/ do you currently have any of the conditions on this card?”; a show-card with multiple non-mutually exclusive options was presented to the participants. We focussed on these co-morbidities: heart attack, hypertension, high cholesterol, stroke, diabetes, chronic lung disease, cancer, Parkinson’s, cataracts, hip fracture, other fractures, cognitive impairment, affective / emotional disorder, any arthritis (including rheumatoid arthritis and osteoarthritis / other rheumatism).
Similarly, medications were assessed by asking: “Do you currently take drugs, at least once a week, for problems mentioned on this card?” and a list was shown. Based on previous literature [9, 10], we selected these medications: anti-hypertensives, drugs for pain (including drugs for joint pain and those for other pain) and psychotropic drugs (including drugs for sleep problems and those for anxiety or depression).
Falls at baseline were assessed by asking the participants: “For the past six months at least, have you been bothered by any of the health conditions on this card?”; options included: “falling down”, “fear of falling down”, “dizziness, faints or blackouts”, “fatigue” or “none” (participants could choose more than one option). Falls at baseline were dichotomised as “no” (no falls) versus “yes” (one or more falls).
Vision and hearing impairment
Distant and close vision, respectively, were assessed by asking the participants: “How good is your eyesight for seeing things at a distance, like recognising a friend across the street – wearing glasses or contact lenses if needed? Would you say it is…” and “How good is your eyesight for seeing things up close, like reading ordinary newspaper print – wearing glasses or contact lenses if needed? Would you say it is…” options included: “excellent”, “very good”, “good”, “fair” or “poor”. We dichotomised vision as good (if both distant and close vision were “excellent” or “very good” or “good”) versus impaired (if distant and or close vision were “fair” or “poor”).
Similarly, hearing was assessed by asking the participants: “Is your hearing [using a hearing aid as usual]…” options were: “excellent”, “very good”, “good”, “fair” or “poor”. We dichotomised hearing as good (“excellent” or “very good” or “good”) versus impaired (“fair” or “poor”).
Finally, we classified the participants into the following four categories: (1) good vision and hearing, (2) impaired vision only, (3) impaired hearing only and (4) impaired vision and hearing (dual sensory impairment). Moreover, we recorded whether participants usually wore glasses (or contact lenses) or hearing aids.
Falls
Follow-up interviews (Wave 7) were conducted from February 2017 to January 2019 and the participants were again asked the question: “For the past six months at least, have you been bothered by any of the health conditions on this card?”; options included: “falling down”. Our outcome of falls at follow-up was dichotomised as “no” (no falls) versus “yes” (one or more falls).
Statistical analyses
All analyses were performed in the total population and in men and women, separately.
We reported the baseline characteristics of the study population by sex and across categories of vision and hearing impairment, respectively. We tested for differences in baseline characteristics using Pearson’s chi-square test for categorical variables, t-test or analysis of variance (ANOVA) for age (used as a continuous variable), as appropriate.
Binary logistic regression models were used to assess the cross-sectional and longitudinal association between visual and hearing impairment categories at baseline (determinant) and falls at follow-up (outcome). The “good vision and hearing” category was the reference. We performed our cross-sectional and longitudinal analyses in two and three steps, respectively. First, we adjusted our analyses for age and sex (Model 1) and then further added self-rated health, co-morbidities, medications, use of glasses and use of hearing aids (Model 2); in longitudinal analyses, we finally further adjusted for falls at baseline, as a marker of frailty (Model 3). In our Models of adjustment, we used age as a continuous variable. We separately entered each co-morbidity and medication variable in Model 2.
We repeated the cross-sectional and longitudinal analyses in the sample of participants aged 80 years and older. Further longitudinal analyses were performed by stratifying the participants into two age groups: aged 50–64 years versus aged 65 years and older. Further analyses were performed after excluding participants who reported falls at baseline or those who were followed up after 2017. All analyses were performed using SPSS 25.
Ethics
SHARE obtained institutional review board approval by the University of Mannheim (Waves 1–4) and the Max Planck Society (Wave 4 and the continuation of the project) [32,33,34].
Results
Characteristics at baseline
In our study population, mean age was 67.1 (standard deviation (SD) 9.5; range 50–102) years and 28,868 (56.6%) participants were women. A total of 11,290 (22.1%) participants reported vision impairment and 9782 (19.2%) reported hearing impairment. When combining data, 33,767 (66.2%) participants reported good vision and hearing, 7437 (14.6%) impaired vision only, 5929 (11.6%) impaired hearing only and 3853 (7.6%) impaired vision and hearing (Table 1). Women were more likely to report vision impairment, while men hearing impairment (both p < 0.001). Supplementary Table 2 details the characteristics of participants aged 80 years and older at baseline.
Participants with good vision and hearing were the youngest and least likely to report poor health, co-morbidities and medications; in contrast, those with impaired vision and hearing were the oldest and most likely to report poor health, co-morbidities and medications (all p < 0.001, Table 2). The frequencies of poor health, co-morbidities and medications were intermediate among participants with impaired vision only or impaired hearing only. Similar findings were observed in both sexes (Supplementary Table 3 for men and 4 for women).
Most participants wore glasses (n = 43,251, 84.8%); a minority used hearing aids (n = 3162, 6.2%). In particular, hearing aids were used by 1133 (11.6%) participants reporting hearing impairment.
Cross-sectional analyses
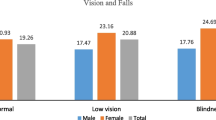
At the baseline interview, 3472 (6.8%) participants—in particular, 1006 (4.5%) men, 2466 (8.5%) women, 932 (15.8%) of those aged 80 years and older—reported falls.
In age- and sex-adjusted analyses (Model 1), participants with impaired vision only, impaired hearing only or impaired vision and hearing, respectively, had an increased falls risk compared to those with good vision and hearing (Table 3). After full adjustment (Model 3), participants with impaired vision only, impaired hearing only and impaired vision and hearing, respectively, had an increased risk of falls of 1.34 (1.22–1.49), 1.34 (1.20–1.50) and 1.67 (1.50–1.87), compared to those with good vision and hearing (all p < 0.001, Table 3). These findings were consistent in both sexes (Table 3).
Among participants aged 80 years and older, those with dual sensory impairment had an increased risk of falls of 1.40 (1.15–1.71), compared to those with good vision and hearing, after full adjustment (Supplementary Table 5). This association was consistent in women aged 80 years and older.
Longitudinal analyses
Mean time interval between baseline and follow-up interview was 24.5 (SD 3.6) months. At the follow-up interview, 4214 (8.3%) participants—in particular, 1351 (6.1%) men, 2863 (9.9%) women, 1136 (19.2%) of those aged 80 years and older at baseline—reported falls.
Covariates and falls risk
In our total study population, these covariates were longitudinally associated with increased falls risk, after full adjustment (Model 3): older age, female sex (versus male), poor self-rated health (versus good), falls at baseline (versus no falls), ischemic heart disease, stroke, diabetes, chronic lung disease, Parkinson’s disease, hip fracture, other fracture, affective or emotional disorder, any arthritis, use of drugs for pain (versus no use), use of psychotropic drugs (versus no use) and use of glasses (versus no use) (Supplementary Table 6). Hearing aids use was not prospectively associated with falls risk.
Vision and hearing impairment and falls risk
In age- and sex-adjusted analyses (Model 1), we observed longitudinal associations between vision and or hearing impairment and risk of falls. Participants with impaired vision only, impaired hearing only and impaired vision and hearing had an increased risk (OR (95% CI)) of falls of 1.58 (1.45–1.73), 1.39 (1.26–1.54) and 2.30 (2.08–2.53), respectively, compared to those with good vision and hearing (Table 4).
Impaired hearing only was associated with an increased falls risk, independent of age, sex, self-rated health, co-morbidities and medications (Model 2), but this association lost statistical significance after further adjustment for baseline falls (Model 3, Table 4).
After full adjustment (Model 3), participants with impaired vision only and those with impaired vision and hearing had an increased risk of falls of 1.19 (1.08–1.31) and 1.33 (1.20–1.49), respectively, compared to those with good vision and hearing (Table 4). Similar findings were observed in both sexes.
After exclusion of participants reporting falls at baseline, impaired vision only, impaired hearing only and dual sensory impairment were all associated with an increased falls risk (Supplementary Table 7).
Age-stratified results
Supplementary Table 8 presents the fully adjusted age-stratified longitudinal associations between vision and or hearing impairments and risk of falls. Among participants aged 50–64 years, impaired vision only, impaired hearing only and impaired vision and hearing were all associated with an increased falls risk, compared to good vision and hearing (Supplementary Table 8). All these findings were consistent among women aged 50–64 years. Among men aged 50–64 years, dual sensory impairment was associated with an increased falls risk.
Among participants aged 65 years and older, impaired vision, with or without impaired hearing, was associated with an increased risk of falls, compared to good vision and hearing; in contrast, no association was found between impaired hearing only and falls (Supplementary Table 8).
Among participants aged 80 years and older, no longitudinal association between any sensory impairment and falls risk was observed, after full adjustment (Supplementary Table 9).
Discussion
In this large population-based cross-European study, vision impairment, with or without hearing impairment, was cross-sectionally and longitudinally associated with an increased risk of falls in community-dwelling adults aged 50 years and older. The risk of falls was highest when vision impairment coincided with hearing impairment. In contrast, hearing impairment, without vision impairment, was cross-sectionally but not longitudinally associated with an increased falls risk. All these associations were independent of age, sex, self-rated health, co-morbidities, medications and previous falls and consistent in both middle-aged and older adults.
There is a vast literature on vision and falls [5, 9,10,11,12,13,14,15,16,17,18,19,20]. However, few population-based studies have explored the association between self-reported vision impairment and falls risk [15,16,17,18,19,20]. Of these, a few only assessed cross-sectional associations [15, 16]; others investigated longitudinal associations, with conflicting results [17,18,19,20]. Among older community-dwelling Chinese women, self-reported vision was correlated with future indoor injurious falls, but not independent of covariates [17]. Among Australian older men and women, self-reported vision impairment was prospectively associated with increased falls risk [18]. In a Brazilian study, self-reported vision impairment was prospectively associated with falls and recurrent falls in community-dwelling older adults, independent of covariates, while self-reported hearing impairment was not [19].
There is growing literature on hearing impairment and falls. Hearing impairment was objectively measured in most studies [23,24,25,26, 28, 30], self-reported in a few [17,18,19,20, 27] or both measured and self-reported in another [29]. Among Chinese older women, self-reported hearing impairment was not prospectively associated with indoor injurious falls, after adjustment for covariates [17]. Moreover, self-reported hearing impairment was longitudinally associated with an increased falls risk among adults of population-based studies from Australia and the Netherlands [18, 20], but not from Brazil [19]. In NHANES, hearing loss was independently associated with falls over the preceding 12 months, among adults aged 40–69 years [24]. In the Health ABC study, moderate-or-greater hearing impairment was longitudinally associated with incident frailty and falls among high-functioning, community-dwelling older adults; hearing aid use did not modify the risk of frailty or falls [25]. In the Finnish Twin Study on Aging, older women with hearing impairment had higher falls risk at 1-year follow-up, compared to those with good hearing; this was partially explained by worse postural control in those with hearing impairment [23]. In the Blue Mountains Eye Study, objectively measured hearing loss was not associated with greater falls incidence, while self-perceived hearing impairment was [29]. Other studies did not show any association of hearing impairment with falls [26, 27]. Hearing sensitivity was not prospectively associated with falls risk among older women in the Study of Osteoporotic Fractures [26]. In the National Health Interview Survey, self-reported hearing impairment was not independently associated with nonfatal fall-related injury, among community-dwelling Americans aged 18 years and older [27].
Few prospective studies assessed the effect of dual sensory impairment on falls risk [28,29,30]. In the Finnish Twin Study on Aging, co-existing vision and hearing impairment were associated with greater risk for falls among older women, compared to vision impairment alone; co-existing sensory deficits showed an additional effect on fall risk [28]. In the Blue Mountains Eye Study, co-existing vision and hearing impairment was correlated with a twofold increased risk of two or more falls over a 5-year follow-up [29]. In contrast, a multicentre Nordic hospital-based prospective study found that combined vision and hearing impairment was not independently associated with falls over three months, among adults aged 75 years and older [30].
The above-described discrepancies among studies may be related to differences in the age-, sex- and ethnic composition of the study population [1,2,3,4, 18], study design (cross-sectional or longitudinal), setting (population-based or hospital based) and variability in the measurement and classification of vision and hearing impairment (objective measures or self-report; different threshold for defining impairment). In particular, studies in older [17, 19, 26, 30] or frailer, hospitalised [30] populations may fail to show independent associations between sensory impairment and falls, due to more competing risk factors for falls in these populations. The relative importance of sensory impairment as a falls risk factor may be greater in middle-aged than in older adults and similarly, in community-dwelling adults than in frail, hospitalised adults. Consistent with this, in our study, isolated hearing impairment was independently associated with an increased falls risk in adults aged 50–64 years but not in those aged 65 years and older. Globally, our study population was younger than those of other studies [17, 19, 26, 30]. Moreover, a few previous studies with non-significant findings were relatively small and possibly lacked statistical power [17, 19, 30]. Furthermore, the relationships between sensory impairment and falls risk may be graded [11, 24]; if this holds true, the finding of associations and their strength may vary according to the definition and measurement of sensory impairment.
Furthermore, our study examined both cross-sectional and longitudinal associations; the strength of associations became attenuated in longitudinal analyses. During the 2-year follow-up, many participants with good vision and hearing at baseline may have become sensory impaired; in contrast, most of those with sensory impairment at baseline may not have recovered their function. In this way, the contrast between participants with and without sensory impairment at baseline may reduce longitudinally; moreover, competing risk factors for falls become more prevalent as the study population ages. As a consequence, the cumulative incidence of falls throughout the 2-year follow-up may differ more than that in the six months preceding the follow-up interview. The duration of follow-up may influence the longitudinal associations between sensory impairment and falls risk; the longer the follow-up, the more attenuated the associations. This could contribute to discrepancies across longitudinal studies with follow-up of different durations [17,18,19,20, 23, 25, 26, 28, 29].
Age, sex and ethnicity may influence the prevalence of sensory impairment [1,2,3,4], the rate of falls [10] and possibly the relationship between sensory impairment and falls and contribute to heterogeneity of findings among studies.
In our population-based study of middle-aged and older adults, the rate of falls was about 7–8% in the six months prior to the baseline and follow-up interview, respectively. These were lower compared to falls rates of about 25–27% in the previous twelve months, in previous studies of community-dwelling middle-aged and older adults [13,14,15]. This might be due to healthy respondent bias or cohort effect (contemporary adults may be healthier than adults of the eighties [5]). In line with previous literature, older age and female sex were falls risk factors, independent of co-morbidities, in our study [10].
The prevalence of self-reported vision impairment (22.1%) in our European population-based study was intermediate between those of reports from the U.S. and UK [16, 35], and that of a Chinese study [36]. Our prevalence of hearing impairment (19.2%) was lower than that of a sample of adults over 60 years in the English Longitudinal Study of Ageing [37]. In line with previous reports, women in our study were more likely to report vision impairment, while men hearing impairment [1,2,3,4, 18]. In our study, hearing aids were used only by 11.6% participants reporting impaired hearing; similarly, studies from the U.S. reported underuse of hearing aids [3].
In our study, use of glasses was prospectively associated with increased falls risk, independent of vision impairment. Of note, a few randomised controlled trials showed that comprehensive vision and eye assessment, with appropriate treatment and provision of glasses if needed, did not reduce [38], or could even increase [39, 40], the falls risk in older adults. Older adults may need a considerable period of time to adjust to new eyeglasses and could be at greater risk of falling during this time [39]. We could not find any association between use of hearing aids and falls; however, given the low frequency of hearing aids use, our study might have been underpowered.
Different, non-mutually exclusive explanations for the association between vision and hearing loss and falls have been proposed.
First, vision and hearing may be needed for mobility. Vision contributes to the maintenance of balance and control of postural sway when standing [11, 41]. Indeed, sway increases with eyes closed compared with eyes open; sway is a strong risk factor for future falls [11, 41, 42]. Various components of vision are crucial for mobility. Depth perception, i.e. the ability to accurately judge distances and perceive spatial relationship, is required for navigating through obstacles in the environment [9, 12]. Contrast sensitivity is important in detecting indoor and outdoor hazards, such as steps, curbs, pavement cracks or clutter [12]. Lower visual field may be needed to detect objects in the environment that could be tripped over when walking [12]. Visual field–both central and peripheral–is important to assess ground surfaces and moving pedestrians or vehicles [14]. Similarly, hearing contributes to spatial awareness and postural stability [21, 22].
Second, vision and hearing deficits may increase the cognitive load; adults with these deficits may invest more cognitive resources in vision and hearing and less in mobility tasks requiring attention [21, 22]. The cognitive load may be greater in outdoor environments, due to more unpredictable hazards, such as other pedestrians or traffic, compared to indoor environments. Thus, adults with sensory impairments may have greater difficulty outdoors than indoors.
Third, shared pathological pathways may underlie both vision and hearing impairment and falls; for example, cardiovascular risk factors and diseases—such as diabetes mellitus—are common risk factors for both sensory impairments and falls [2, 3, 10]. Yet, in our study, the association between vision impairment and falls risk remained significant, though attenuated, after adjustment for co-morbidities. Likewise, ageing is associated with both sensory deficits and falls [1,2,3,4,5]; yet, the correlation between sensory impairment and falls in our study was independent of age and consistent among participants aged 50–64 years. Moreover, hearing and vestibular impairment frequently coincide; the association of hearing impairment with increased falls risk may be partly explained by concomitant vestibular dysfunction; yet, hearing per se may affect balance and falls risk [21, 22].
Finally, vision and hearing impairment may be causally linked to fear of falling [43], social isolation, depression [36], frailty [25, 35, 37] and cognitive decline [44]; longitudinal associations between sensory impairment and the latter have been shown by observational studies; causality has not been proven yet.
The findings of this study have clinical implications. Some causes of visual and hearing impairment in older adults may be preventable or treatable; however, it is unknown whether treating them could reduce falls risk in adults. Randomised trials from England found that first eye cataract surgery reduced the risk of falls and fractures in older women [45], while second eye cataract surgery did not [46]. Moreover, a large retrospective cohort study from Australia reported an increased risk of injurious falls after first- and second eye cataract surgery [47].
Healthy lifestyle behaviours—use of hats and sunglasses for UV protection and smoking cessation—may promote eye health [48]. Similarly, limiting exposure to harmful noise—in the workplace and during leisure—may reduce noise-induced hearing loss [3]. It is unclear whether targeting cardiovascular risk factor and diseases may have beneficial effects on hearing; although a correlation between diseases such as diabetes and hearing loss is established, causality is not established [3].
Furthermore, our study supports the use of simple questions on self-reported sensory impairment to accurately assess the falls risk of community-dwelling adults. This is relevant for large scale screening and remote consultations.
Major strengths of our study are the large multinational sample size, the inclusion of both men and women of a wide age range, the cross-sectional and longitudinal design, the standardised methods for data collection and the adjustment for many covariates. In particular, we included and specifically reported on adults aged 50–64 years, while many previous studies only focused on older adults [16, 19, 25, 30]. Indeed, we showed that vision and dual sensory impairment were longitudinally associated with falls also among middle-aged adults. Moreover, by performing longitudinal analyses, we could show that vision and hearing impairment preceded the falls (temporality of association). By adjusting for many covariates, we showed that most associations between sensory impairment and falls became attenuated but remained significant; this implies that these associations are partly mediated by concomitant co-morbidities and medications yet persist beyond these.
Our study has certain limitations. First, causality cannot be inferred given the observational nature of this study; we cannot determine the mechanistic pathways through which vision and hearing impairment are associated with falls risk. Second, vision and hearing impairment were self-reported; objective measures were not available. Yet, self-reported hearing is an accurate measure [49] and self-reported vision may be more comprehensive than objective measures of separate vision components. Moreover, screening for sensory impairment using simple questions is brief, inexpensive and reproducible in large scale studies, mass screening in the community or remote consultations. Third, falls were retrospectively self-reported; falls, especially non-injurious falls, could be underreported. However, screening for falls using a single question is less costly and more applicable to large populations than falls diaries. Although the SHARE questionnaire does not include a definition of “falling down”, “falling down” was separately included among a list of physical health issues; based on this and on checking the translations of the questionnaire, we deem it unlikely that participants may have reported falls due to external forces (accidents, violence) or separate health issues (syncope and seizures). Moreover, the SHARE questionnaire does not distinguish outdoor and indoor falls or injurious and non-injurious falls. As a result, we could not explore whether sensory impairments may be greater risk factors for outdoor falls, compared to indoor falls. Nor could we explore whether sensory impairments may affect the risk of injury, following falls [11], maybe by reducing self-protection abilities. Fourth, we cannot exclude residual confounding; for instance, both hearing impairment and falls may be correlated with vestibular impairment. Fifth, we cannot exclude a healthy respondent bias as suggested by the lower rates of falls in our study; given this and the relatively small sample of participants aged 80 years and older, our study might lack statistical power to detect longitudinal associations between sensory impairment and falls risk in the oldest old. Sixth, those participants who were lost to follow-up, compared to those included in the analyses, were older, with a greater burden of sensory impairment, co-morbidities and previous falls and likely at greater falls risk; as a result, our associations might have been attenuated. Finally, our study included only community-dwelling adults; this may limit the generalisability of our findings to institutionalised populations, who have different falls risk profiles compared to those in the community [10, 50].
In this large cross-European study of community-dwelling adults, vision and dual sensory impairment were longitudinally associated with an increased falls risk, independent of age, sex, subjective health, co-morbidities and previous falls. Hearing impairment, without vision impairment, was longitudinally associated with an increased falls risk among women aged 50–64 years. Simple questions on self-reported sensory impairment can be used to assess the falls risk in adults. This is relevant for large scale screening of populations and useful for the increasing need of virtual consultations.
Data availability
Data are available upon request from the SHARE website (see http://www.share-project.org/data-access/user-registration.html).
Code availability
Not applicable.
References
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020 Oct 17;396(10258):1204–1222. doi: https://doi.org/10.1016/S0140-6736(20)30925-9. (Erratum in: Lancet. 2020 Nov 14;396(10262):1562. PMID: 33069326; PMCID: PMC7567026).
Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, Das A, Jonas JB, Keeffe J, Kempen JH, Leasher J, Limburg H, Naidoo K, Pesudovs K, Silvester A, Stevens GA, Tahhan N, Wong TY, Taylor HR; Vision Loss Expert Group of the Global Burden of Disease Study. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017 Dec;5(12):e1221-e1234. doi: https://doi.org/10.1016/S2214-109X(17)30393-5. (Epub 2017 Oct 11. PMID: 29032195).
Cunningham LL, Tucci DL (2017) Hearing Loss in Adults. N Engl J Med 377(25):2465–2473. https://doi.org/10.1056/NEJMra1616601(PMID:29262274;PMCID:PMC6457651)
Lin FR, Thorpe R, Gordon-Salant S, Ferrucci L. Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol A Biol Sci Med Sci. 2011 May;66(5):582–90. doi: https://doi.org/10.1093/gerona/glr002. (Epub 2011 Feb 27. PMID: 21357188; PMCID: PMC3074958).
Tinetti ME, Speechley M, Ginter SF (1988) Risk factors for falls among elderly persons living in the community. N Engl J Med 319(26):1701–1707. https://doi.org/10.1056/NEJM198812293192604 (PMID: 3205267)
Kelsey JL, Procter-Gray E, Hannan MT, Li W. Heterogeneity of falls among older adults: implications for public health prevention. Am J Public Health. 2012 Nov;102(11):2149–56. doi: https://doi.org/10.2105/AJPH.2012.300677. Epub 2012 Sep 20. PMID: 22994167; PMCID: PMC3469772.
Tinetti ME, Doucette J, Claus E, Marottoli R (1995) Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc 43(11):1214–1221. https://doi.org/10.1111/j.1532-5415.1995.tb07396.x (PMID: 7594154)
Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc. 2018 Apr;66(4):693–698. doi: https://doi.org/10.1111/jgs.15304. (Epub 2018 Mar 7. PMID: 29512120; PMCID: PMC6089380).
Nevitt MC, Cummings SR, Kidd S, Black D (1989) Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA 261(18):2663–2668 (PMID: 2709546)
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E (2010) Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology 21(5):658–668. https://doi.org/10.1097/EDE.0b013e3181e89905 (PMID: 20585256)
Harwood RH (2001) Visual problems and falls. Age Ageing 30(Suppl 4):13–18. https://doi.org/10.1093/ageing/30.suppl_4.13 (PMID: 11769782)
Lord SR, Dayhew J (2001) Visual risk factors for falls in older people. J Am Geriatr Soc 49(5):508–515. https://doi.org/10.1046/j.1532-5415.2001.49107.x (PMID: 11380741)
Ivers RQ, Cumming RG, Mitchell P, Attebo K (1998) Visual impairment and falls in older adults: the blue mountains eye study. J Am Geriatr Soc 46(1):58–64. https://doi.org/10.1111/j.1532-5415.1998.tb01014.x (PMID: 9434666)
Patino CM, McKean-Cowdin R, Azen SP, Allison JC, Choudhury F, Varma R; Los Angeles Latino Eye Study Group. Central and peripheral visual impairment and the risk of falls and falls with injury. Ophthalmology. 2010 Feb;117(2):199–206.e1. doi: https://doi.org/10.1016/j.ophtha.2009.06.063. (Epub 2009 Dec 23. PMID: 20031225; PMCID: PMC2819614).
Yip JL, Khawaja AP, Broadway D, Luben R, Hayat S, Dalzell N, Bhaniani A, Wareham N, Khaw KT, Foster PJ. Visual acuity, self-reported vision and falls in the EPIC-Norfolk Eye study. Br J Ophthalmol. 2014 Mar;98(3):377–82. doi: https://doi.org/10.1136/bjophthalmol-2013-304179. (Epub 2013 Dec 12. PMID: 24338086; PMCID: PMC3933174).
Ehrlich JR, Hassan SE, Stagg BC. Prevalence of Falls and Fall-Related Outcomes in Older Adults with Self-Reported Vision Impairment. J Am Geriatr Soc. 2019 Feb;67(2):239–245. doi: https://doi.org/10.1111/jgs.15628. (Epub 2018 Nov 13. PMID: 30421796; PMCID: PMC6367006).
Hu J, Xia Q, Jiang Y, Zhou P, Li Y. Risk factors of indoor fall injuries in community-dwelling older women: a prospective cohort study. Arch Gerontol Geriatr. 2015 Mar-Apr;60(2):259–64. doi: https://doi.org/10.1016/j.archger.2014.12.006. (Epub 2014 Dec 30. PMID: 25591845).
Lopez D, McCaul KA, Hankey GJ, Norman PE, Almeida OP, Dobson AJ, Byles JE, Yeap BB, Flicker L (2011) Falls, injuries from falls, health related quality of life and mortality in older adults with vision and hearing impairment–is there a gender difference? Maturitas 69(4):359–364. https://doi.org/10.1016/j.maturitas.2011.05.006 (Epub 2011 Jun 12 PMID: 21664773)
Perracini MR, Ramos LR. Fatores associados a quedas em uma coorte de idosos residentes na comunidade [Fall-related factors in a cohort of elderly community residents]. Rev Saude Publica. 2002 Dec;36(6):709–16. Portuguese. doi: https://doi.org/10.1590/s0034-89102002000700008. (PMID: 12488937).
Tromp AM, Smit JH, Deeg DJ, Bouter LM, Lips P (1998) Predictors for falls and fractures in the Longitudinal Aging Study Amsterdam. J Bone Miner Res 13(12):1932–1939. https://doi.org/10.1359/jbmr.1998.13.12.1932 (PMID: 9844112)
Campos J, Ramkhalawansingh R, Pichora-Fuller MK (2018) Hearing, self-motion perception, mobility, and aging. Hear Res 369:42–55. https://doi.org/10.1016/j.heares.2018.03.025 (Epub 2018 Mar 31 PMID: 29661612)
Jiam NT, Li C, Agrawal Y (2016) Hearing loss and falls: a systematic review and meta-analysis. Laryngoscope 126(11):2587–2596. https://doi.org/10.1002/lary.25927 (Epub 2016 Mar 24 PMID: 27010669)
Viljanen A, Kaprio J, Pyykkö I, Sorri M, Pajala S, Kauppinen M, Koskenvuo M, Rantanen T. Hearing as a predictor of falls and postural balance in older female twins. J Gerontol A Biol Sci Med Sci. 2009 Feb;64(2):312–7. doi: https://doi.org/10.1093/gerona/gln015. (Epub 2009 Jan 31. PMID: 19182227; PMCID: PMC2655032).
Lin FR, Ferrucci L (2012) Hearing loss and falls among older adults in the United States. Arch Intern Med 172(4):369–371. https://doi.org/10.1001/archinternmed.2011.728. PMID:22371929;PMCID:PMC3518403
Kamil RJ, Betz J, Powers BB, Pratt S, Kritchevsky S, Ayonayon HN, Harris TB, Helzner E, Deal JA, Martin K, Peterson M, Satterfield S, Simonsick EM, Lin FR; Health ABC study. Association of Hearing Impairment With Incident Frailty and Falls in Older Adults. J Aging Health. 2016 Jun;28(4):644–60. doi: https://doi.org/10.1177/0898264315608730. Epub 2015 Oct 5. PMID: 26438083; PMCID: PMC5644033.
Purchase-Helzner EL, Cauley JA, Faulkner KA, Pratt S, Zmuda JM, Talbott EO, Hochberg MC, Stone K, Newman A (2004) Hearing sensitivity and the risk of incident falls and fracture in older women: the study of osteoporotic fractures. Ann Epidemiol 14(5):311–318. https://doi.org/10.1016/j.annepidem.2003.09.008 (Erratum.In:AnnEpidemiol.2004Sep;14(8):625. PMID: 15177269)
Heitz ER, Gianattasio KZ, Prather C, Talegawkar SA, Power MC (2019) Self-reported hearing loss and nonfatal fall-related injury in a nationally representative sample. J Am Geriatr Soc 67(7):1410–1416. https://doi.org/10.1111/jgs.15849 (Epub 2019 Mar 8 PMID: 30848835)
Kulmala J, Viljanen A, Sipilä S, Pajala S, Pärssinen O, Kauppinen M, Koskenvuo M, Kaprio J, Rantanen T (2009) Poor vision accompanied with other sensory impairments as a predictor of falls in older women. Age Ageing 38(2):162–167. https://doi.org/10.1093/ageing/afn228 (Epub 2008 Nov 13 PMID: 19008307)
Gopinath B, McMahon CM, Burlutsky G, Mitchell P (2016) Hearing and vision impairment and the 5-year incidence of falls in older adults. Age Ageing 45(3):409–414. https://doi.org/10.1093/ageing/afw022 (Epub 2016 Mar 5 PMID: 26946051)
Grue EV, Ranhoff AH, Noro A, Finne-Soveri H, Jensdóttir AB, Ljunggren G, Bucht G, Björnson LJ, Jonsén E, Schroll M, Jónsson PV (2009) Vision and hearing impairments and their associations with falling and loss of instrumental activities in daily living in acute hospitalized older persons in five Nordic hospitals. Scand J Caring Sci 23(4):635–643. https://doi.org/10.1111/j.1471-6712.2008.00654.x (Epub 2009 Nov 12 PMID: 19068040)
Crews JE, Campbell VA (2004) Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Public Health 94(5):823–829. https://doi.org/10.2105/ajph.94.5.823. (PMID:15117707;PMCID:PMC1448344)
Borsch-Supan A, Brandt M, Hunkler C, et al. SHARE Central Coordination Team. Data Resource Profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol 2013;42:992–1001.
Börsch-Supan, A. (2019). Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 6. Release version: 7.1.0. SHARE-ERIC. Data set. DOI: https://doi.org/10.6103/SHARE.w6.710
Börsch-Supan, A. (2020). Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 7. Release version: 7.1.1. SHARE-ERIC. Data set. DOI: https://doi.org/10.6103/SHARE.w7.711
Liljas AEM, Carvalho LA, Papachristou E, De Oliveira C, Wannamethee SG, Ramsay SE, Walters KR. Self-reported vision impairment and incident prefrailty and frailty in English community-dwelling older adults: findings from a 4-year follow-up study. J Epidemiol Community Health. 2017 Nov;71(11):1053–1058. doi: https://doi.org/10.1136/jech-2017-209207. (Epub 2017 Aug 10. PMID: 28798152; PMCID: PMC5847099).
Zhang Q, Cao GY, Yao SS, Wang C, Chen ZS, Hu YH, Xu B (2021) Self-reported vision impairment, vision correction, and depressive symptoms among middle-aged and older Chinese: Findings from the China health and retirement longitudinal study. Int J Geriatr Psychiatry 36(1):86–95. https://doi.org/10.1002/gps.5398 (Epub 2020 Oct 13 PMID: 32783270)
Liljas AEM, Carvalho LA, Papachristou E, Oliveira C, Wannamethee SG, Ramsay SE, Walters K. Self-Reported Hearing Impairment and Incident Frailty in English Community-Dwelling Older Adults: A 4-Year Follow-Up Study. J Am Geriatr Soc. 2017 May;65(5):958–965. doi: https://doi.org/10.1111/jgs.14687. Epub 2016 Dec 19. PMID: 27991672; PMCID: PMC5484326.
Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S (2002) Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 325(7356):128. https://doi.org/10.1136/bmj.325.7356.128 (PMID:12130606;PMCID:PMC117228)
Cumming RG, Ivers R, Clemson L, Cullen J, Hayes MF, Tanzer M, Mitchell P (2007) Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc 55(2):175–181. https://doi.org/10.1111/j.1532-5415.2007.01046.x (PMID: 17302652)
Haran MJ, Cameron ID, Ivers RQ, Simpson JM, Lee BB, Tanzer M, Porwal M, Kwan MM, Severino C, Lord SR (2010) Effect on falls of providing single lens distance vision glasses to multifocal glasses wearers: VISIBLE randomised controlled trial. BMJ 25(340):c2265. https://doi.org/10.1136/bmj.c2265 (Erratum.In:BMJ.2016May27;353:i3041.PMID:20501583;PMCID:PMC2876235)
Lord SR, Menz HB. Visual contributions to postural stability in older adults. Gerontology. 2000 Nov-Dec;46(6):306–10. doi: https://doi.org/10.1159/000022182 (PMID: 11044784).
Lord SR, Ward JA, Williams P, Anstey KJ (1994) Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc 42(10):1110–1117. https://doi.org/10.1111/j.1532-5415.1994.tb06218.x (PMID: 7930338)
Viljanen A, Kulmala J, Rantakokko M, Koskenvuo M, Kaprio J, Rantanen T (2013) Accumulation of sensory difficulties predicts fear of falling in older women. J Aging Health 25(5):776–791. https://doi.org/10.1177/0898264313494412 (Epub 2013 Jul 4 PMID: 23832841)
Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L (2011) Hearing loss and incident dementia. Arch Neurol 68(2):214–220. https://doi.org/10.1001/archneurol.2010.362 (PMID:21320988;PMCID:PMC3277836)
Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A, Masud T (2005) Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Ophthalmol 89(1):53–59. https://doi.org/10.1136/bjo.2004.049478 (PMID:15615747;PMCID:PMC1772474)
Foss AJ, Harwood RH, Osborn F, Gregson RM, Zaman A, Masud T (2006) Falls and health status in elderly women following second eye cataract surgery: a randomised controlled trial. Age Ageing 35(1):66–71. https://doi.org/10.1093/ageing/afj005 (PMID: 16364936)
Meuleners LB, Fraser ML, Ng J, Morlet N (2014) The impact of first- and second-eye cataract surgery on injurious falls that require hospitalisation: a whole-population study. Age Ageing 43(3):341–346. https://doi.org/10.1093/ageing/aft177 (Epub 2013 Nov 4 PMID: 24192250)
Mitchell P, Liew G, Gopinath B, Wong TY (2018) Age-related macular degeneration. Lancet 392(10153):1147–1159. https://doi.org/10.1016/S0140-6736(18)31550-2 (PMID: 30303083)
Ferrite S, Santana VS, Marshall SW (2011) Validity of self-reported hearing loss in adults: performance of three single questions. Rev Saude Publica 45(5):824–830. https://doi.org/10.1590/s0034-89102011005000050 (Epub 2011 Jul 29 PMID: 21808834)
Deandrea S, Bravi F, Turati F, Lucenteforte E, La Vecchia C, Negri E. Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta-analysis. Arch Gerontol Geriatr. 2013 May-Jun;56(3):407–15. doi: https://doi.org/10.1016/j.archger.2012.12.006. (Epub 2013 Jan 5. PMID: 23294998).
Acknowledgements
Dr Giulia Ogliari was supported by grant APP2380/N7359 (OSTEOPOROSIS & FALLS RESEARCH for “Improving Quality of Life in Older Patients”) by Nottingham Hospitals Charity. This paper uses data from SHARE Waves 6 and 7 (DOIs: 10.6103/SHARE.w6.710, 10.6103/SHARE.w7.711 ), see Börsch-Supan et al. (2013) for methodological details [Borsch-Supan A, Brandt M, Hunkler C, et al. SHARE Central Coordination Team. Data Resource Profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol 2013;42:992–1001]. The SHARE data collection has been funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA N°211909, SHARE-LEAP: GA N°227822, SHARE M4: GA N°261982, DASISH: GA N°283646) and Horizon 2020 (SHARE-DEV3: GA N°676536, SHARE-COHESION: GA N°870628, SERISS: GA N°654221, SSHOC: GA N°823782) and by DG Employment, Social Affairs & Inclusion. Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Funding
Dr Giulia Ogliari was supported by grant APP2380/N7359 (OSTEOPOROSIS & FALLS RESEARCH) by Nottingham Hospitals Charity.
Author information
Authors and Affiliations
Contributions
GO: study concept, data analysis, drafting the manuscript. JR, NQ, KAR, LLSH and TM: study concept, critical revision of manuscript for intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics approval
Institutional review board at University of Mannheim and Ethics Council of the Max Planck Society.
Consent to participate
This article uses anonymised data.
Consent for publication
Not applicable. Personal data were not identifiable during the analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ogliari, G., Ryg, J., Qureshi, N. et al. Subjective vision and hearing impairment and falls among community-dwelling adults: a prospective study in the Survey of Health, Ageing and Retirement in Europe (SHARE). Eur Geriatr Med 12, 1031–1043 (2021). https://doi.org/10.1007/s41999-021-00505-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00505-4