Key summary points
To determine the association between visual acuity and contrast sensitivity with frailty measures
AbstractSection FindingsOlder adults with poor contrast sensitivity are significantly more likely to be frail (OR: 5.34, p = 0.004). No association was identified between visual acuity and frailty (p = 0.241).
AbstractSection MessagePoor contrast sensitivity is significantly associated with frailty.
Abstract
Purpose
Using data from the Malaysian Elders Longitudinal Research (MELoR), this study investigated the association between visual function (visual acuity and contrast sensitivity) and frailty in a group of urban-dwelling older adults.
Methods
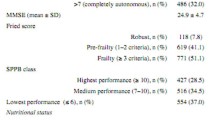
This was a cross-sectional study. 1332 participants aged ≥ 55 years were selected by random sampling from the parliamentary electoral register. Only 1274 participants completed the frailty assessment and 1278 participants completed the contrast sensitivity assessment. Impaired vision was defined as a Snellen visual acuity of worse than 6/12 in the better eye. Poor contrast sensitivity was defined as a score on the Pelli Robson chart of lower than 1.65. Frailty was defined with the Fried’s phenotype criteria. Inter-group comparisons were determined with the independent T-test for continuous variables and the Pearson’s Chi-squared test for categorical variables. The odds ratio (OR) with 95% confidence interval (CI) was used to evaluate the cross-sectional association between frailty and visual function.
Results
The mean age of participants was 68.8 ± 7.5 years, of which 58.1% (774) were women. Impaired vision and poor contrast sensitivity were present in 187 (14%) and 271 (21.2%) subjects respectively. 73 (5.8%) individuals were classified as frail, 1161 (91.0.%) pre-frail, and 40 (2.8%) non-frail. There was no significant difference in frailty phenotypes between those with good and impaired vision (p = 0.241). Fried’s component of handgrip strength, gait speed and exhaustion were significantly better in those with good visual function (p < 0.05). Participants with poor contrast sensitivity were significantly more likely to be frail (OR: 5.34, p = 0.004).
Conclusion
Poor contrast sensitivity was significantly associated with frailty. This highlights the importance of incorporating assessment of contrast sensitivity in those at risk of frailty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is estimated that 285 million people worldwide are visually impaired, with blindness affecting 39 million and low vision further 246 million individuals. An estimated 90% of visually impaired individuals live in developing countries, while older persons comprise 82% of individuals living with blindness [1]. The Malaysian National Eye Survey 1996 reported a prevalence of blindness and low vision in the general population as 0.2% and 2.44% respectively [2]. However, the prevalence of blindness and low vision has increased to 1.2% and 5.4% respectively based on the 2014 National Eye Survey (NES 2) with the majority of both groups aged 50 years old and above [3]. The causes of low vision include glaucoma, diabetes, age-related macular degeneration, cataracts, retinal disease and uncorrected refractive errors. The relationship between increasing age and visual impairment as well as its observed increasing prevalence are concerning for a developing country like Malaysia as it is experiencing rapid population ageing [4].
An expanding older population is also expected to lead to an increase in the number of people vulnerable to a decline in health and function or frailty [5]. Frailty has been defined as a clinically recognizable state of increased vulnerability resulting from age-associated decline in reserve and function across multiple physiological systems [6]. Fried and colleagues have proposed an operational definition, or ‘phenotype,’ of frailty based on five criteria commonly used by researchers [7]. The criteria are slow gait speed, low physical activity, unintentional weight loss, self-reported exhaustion and muscle weakness. Individuals who fulfil three or more of these five criteria are considered frail.
Visual impairment in older adults has been associated with increased risk of adverse health outcomes including functional [8] and cognitive decline [9]. However, little is known about the relationship between visual function (vision and contrast sensitivity) and frailty. A study conducted in Hong Kong reported an independent association between visual acuity and frailty detected with the FRAIL scale [10]. The Beaver Dam Eye Study in Australia also found an association between frailty and poor visual function [5]. Another cross-sectional study involving community-dwelling older adults in England reported that an increased risk of developing the state of pre-frail or frail among older adults with poor visual acuity over a four- year follow-up period [11]. The latter study utilized self-reported symptoms of visual difficulties or disease. Another study which included objective determination of visual acuity suggested that those living with visual impairment are three times more likely to be pre-frail and four times more likely to be frail [12]. All but one study used visual acuity as a measure of visual function but not contrast sensitivity. The importance of contrast sensitivity as a influencing factor for the quality of vision is gaining prominence. Previous studies have detected the effects of reduced contrast sensitivity on activities of daily living like difficulty with reading [13], face recognition [14], driving [15], and mobility [16].
Early detection of frailty is vital to prevent complications which will otherwise burden both health and social care systems. This study was conducted to determine the potential relationship between visual function and the development of frailty among community-dwelling older adults.
Methods
This was a cross-sectional sub-study of the Malaysian Elders Longitudinal Research (MELoR) conducted from June 2013 to December 2015. The study population consisted of 8769 individuals aged 55 years and older selected from the electoral rolls of the parliamentary constituencies of Petaling Jaya North, Petaling Jaya South and Lembah Pantai through simple random sampling. Of these, only 5815 participants had a contactable address, and 3334 met the inclusion criteria and had invitations sent out. Written informed consent was obtained. The study was conducted in accordance with the Declaration of Helsinki and ethical approval was granted by the Medical Research Ethics Committee of the University of Malaya Medical Centre (ethics approval number MREC 943.6).
Best-corrected visual acuity at four meters was determined for each eye with the LogMAR chart. Contrast sensitivity was measured binocularly at one meter with the Pelli Robson chart. The luminance of the measurement environment was in accordance with the manufacturers’ recommendations. All participants were literate. Impaired vision was defined as a Log MAR score of less than 0.3 [17]. For contrast sensitivity, a cut-off value of 1.65 was utilized, below which individuals were considered to have poor contrast sensitivity [5]. Participants with impaired vision or poor contrast sensitivity were referred to the ophthalmology clinic for further evaluation and management.
Frailty was determined by the Fried’s phenotype which included the components of weight loss, weak handgrip strength, slow walking speed, reported exhaustion and low physical activity. The presence of weight loss was defined as an unintentional weight loss of ≥ 4.5 kg for the past one year. Grip strength was assessed using the Jamar handheld dynamometer, with measurements obtained from each hand using Roberts protocol [18]. Participants were required to sit with shoulders fully adducted and elbows held at 90 degrees of flexion. The maximum handgrip strength from the six measurements, three from each hand, was used for analysis. Weak handgrip strength was determined using the 25th centile cut-off of less than 15 kg in women and less than 20 kg in men [18]. Walking speed was measured over 15 feet (4.75 m) at usual pace, while a slow walking speed was defined using the 75th centile cut-off of over seven seconds. Exhaustion was defined using a score of 3 or 4 from the Centre for Epidemiological Studies Depression (CESD) scale. Participants were asked the following question: I feel full of energy these days, with the answer categories: 1 'Often', 2 'Sometimes', 3 'Not often', 4 'Never’. A score of 3 or 4 points was defined as positive for presence of exhaustion. Physical activity was measured with the international physical activity questionnaire (IPAQ). The kilocalorie expenditure per week was estimated based on a published formula. Participants were considered to have low physical activity when they engage in less than three days of vigorous-intensity activity per week or less than five days of moderate-intensity activity per week [19]. Frailty was defined as the presence of three or more of the five components. Pre-frailty was defined as the presence of one or two components and non-frail was defined as having none of the five components. The presence of falls was identified through a self-reported history of at least one fall in the preceding 12 months.
Data were analyzed using SPSS version 25 (SPSS, Inc., Chicago, IL, USA). The quantitative variables were summarized in terms of mean and standard deviation while the qualitative variables were summarized as frequencies and percentages. The independent sample t-test and Pearson’s chi-squared test were used to determine differences between group. All significant values were set at p < 0.05. Multinomial regression was used to determine the odds ratio with 95% confidence intervals.
Results
Out of the 1565 participants who completed the interview session for the demographic data in the MELoR study, 1332 participants had complete vision data, 1278 participants had complete contrast sensitivity data and 1274 participants completed frailty assessments.
Compared to participants with normal vision, those with impaired vision were older and more likely to have no formal or primary education, diabetes mellitus (41.3%) and hypertension (38.9%). Significant ethnic differences existed, with Malay ethnicity associated with increased likelihood of impaired vision (43.3%) (Table1).
In comparison with participants with normal contrast sensitivity, those with poor contrast sensitivity were older, and more likely to have no formal or only primary education and diabetes. A history of falls was significantly more reported among participants with poor contrast sensitivity (Table 1).
Seventy-three (5.73%) participants were classified as frail, 1006 (90.98%) pre-frail and 40 (3.14%) non-frail. No significant relationship existed between frailty and visual impairment (p = 0.241). However, individual component comparisons found slow gait speed (p < 0.001), weak handgrip (p < 00.001) and exhaustion (p = 0.028) to be significantly more common among those with visual impairment (Table 2). Significant associations existed between frailty and impaired contrast sensitivity (p = 0.001) (Table 3). Additionally, four out of five components: slow gait speed (p < 0.001), weak handgrip (p < 0.001), exhaustion (p = 0.032) and low physical activity (p = 0.042) were associated with poor contrast sensitivity.
Multinomial regression analysis revealed no significant association between impaired vision with pre-frail or frail compared to non-frail individuals. Poor contrast sensitivity was significantly associated with the presence of frailty (OR 5.34, 95% CI 1.71–16.69). The association remained after further adjustment for age and diabetes (OR 5.13, 95% CI 0.92–19.14). The association was, however, no longer significant when controlled for level of education (p = 0.07) (Table 4).
Discussion
Contrast sensitivity is closely associated with frailty in our population of older urban-dwelling adults. Reduced visual acuity was, on the contrary, not associated with frailty. After controlling for age and diabetes, older adults with impaired contrast sensitivity remained 5.13 times more likely to be frail according to Fried’s criteria. Impaired contrast sensitivity was also associated with increased risk of self-reported falls.
Few studies to date have investigated the association between contrast sensitivity and frailty measures. The Beaver Dam Eye Study found those with greater frailty scores were likely to have impaired vision and reduced contrast sensitivity. The visual function variables utilized within the study are significantly correlated slow gait speed, low expiratory flow rate, poor handgrip strength and inability to perform chair stand. Each component of the frailty phenotype was also significantly associated with both impaired vision and reduced contrast sensitivity [15]. A 10-year follow-up study found an association between frailty and age-related cataract, which is known to affect contrast sensitivity more than visual acuity [20]. In our study, the association between reduced contrast sensitivity and the presence of frailty remained after adjustments for age and the presence of diabetes mellitus. However, the association was attenuated by adjusting for education level, implying a lower education level may account for the increased likelihood of frailty in individuals with poorer contrast sensitivity. The significant association between lower education level and both reduced visual acuity and poorer contrast sensitivity was in agreement with another similar study which established that impaired near visual acuity is associated with frailty [21]. This was an expected finding since lower education level negatively influences healthcare access and awareness [22].
Based on our study, individuals with reduced contrast sensitivity were at greater odds of being frail. This may be explained at a molecular level by the age-related reduction in the number of rods at the parafovea [23]. Contrast sensitivity measures the ability to distinguish between finer and finer increments of light versus dark, as opposed to visual acuity which measures the ability to read increasingly smaller letters on the visual acuity chart. Reduced contrast sensitivity is also associated with diabetes, which has been attributed to structural changes within the inner-retina which also affects the magnocellular and parvocellular pathways [24]. Worsening contrast sensitivity with age may also be due to neural factors like the reduction of retinal illuminance by senile miosis or optical factors such as increased higher-order aberrations [25].
In our study, the association between contrast sensitivity and frailty was independent of age and diabetes status. Contrast sensitivity appears to more accurately reflect real-life conditions from a visual perspective. It not only determines how patients see under high contrast conditions but also under real-world low contrast conditions [26]. Contrast sensitivity has a stronger association with visual tasks entailing distance judgments and mobility than conventional visual acuity testing [27, 28]. As a result, this causes worsening engagement in physical activities, thus contributing to the development of frailty.
Our cross-sectional analysis found no association between reduced visual acuity and frailty. Reduced visual acuity was only associated with slowness, handgrip and exhaustion but not physical activity and weight loss. This was similar to the findings of a large population study conducted in France by Zoler et al. which did not find a significant relationship between frailty and vision impairment [29]. This is in contrast with Swenor et al. who reported a 3.2 times increased likelihood of being pre-frail and frail with visual impairment compared to those without visual impairment [12]. Liljas et al. found participants also found a doubling in risk of becoming pre-frail and frail with visual impairment [11]. In these two studies, poor vision was self-reported while frailty was defined by the combination of pre-frail and frail. A study conducted in community-dwelling older persons in Hong Kong also found an independent association between visual impairment and frailty [10]. The FRAIL criteria rather than the Fried criteria were employed here. The differences in measurements, therefore, limits comparisons between these studies and ours.
The relationship between falls and frailty have been previously established [30,31,32]. Reduced contrast sensitivity, and not poor visual acuity, has also been found to be significantly related to the risk of recurrent falls [33]. The findings in our study are consistent with this previous study which also found that the presence of a history of falls in the past 12 months was significantly more reported in participants with poor contrast sensitivity. Falls are significantly associated with increased healthcare costs, as they may lead to long-term disabilities in the older persons which in turn are associated with increased frailty.
The low response rate within the sample population may limit the representativeness of the study with those who are frail more likely to be excluded, though it is not possible to confirm this suspicion. The Fried phenotype only considers the physical dimension and does not take into account non-physical aspects of frailty such as psychosocial aspects and cognitive impairment. The inclusion of other frailty indices should, therefore, be considered in future such studies. However, the Fried criteria remain the most widely used, hence allowing for direct comparisons with other studies. Potentially confounding variables such as health behaviour were also not controlled within this study. Causal relationship cannot be determined with a cross-sectional study design. The relationship between contrast sensitivity and frailty, therefore, needs to be confirmed in future prospective studies.
In conclusion, reduced contrast sensitivity is associated with physical frailty measured with the Fried criteria. Future studies should seek to determine whether early recognition and treatment of those with poor contrast sensitivity could potentially reduce the burden of frailty in our society.
Availability of data and materials
Available.
Code availability
SPSS version 25 (SPSS, Inc., Chicago, IL, USA).
References
Bourne RRA, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB et al (2017) Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health 5(9):e888–e897
Zainal M, Ismail SM, Ropilah AR, Elias H, Arumugam G, Alias D et al (2002) Prevalence of blindness and low vision in Malaysian population: results from the National Eye Survey 1996. Br J Ophthalmol 86(9):951–956
Chew FLM, Salowi MA, Mustari Z, Husni MA, Hussein E, Adnan TH et al (2018) Estimates of visual impairment and its causes from the National Eye Survey in Malaysia (NESII). PLoS ONE 13(6):e0198799
Tey NP, Siraj SB, Kamaruzzaman SB, Chin AV, Tan MP, Sinnappan GS et al (2016) Aging in Multi-ethnic Malaysia. Gerontologist 56(4):603–609
Klein BE, Klein R, Knudtson MD, Lee KE (2003) Relationship of measures of frailty to visual function: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc 101:191–6 (discussion 6–9)
Xue QL (2011) The frailty syndrome: definition and natural history. Clin Geriatr Med 27(1):1–15
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56(3):M146–M156
Reuben DB, Mui S, Damesyn M, Moore AA, Greendale GA (1999) The prognostic value of sensory impairment in older persons. J Am Geriatr Soc 47(8):930–935
Maharani A, Dawes P, Nazroo J, Tampubolon G, Pendleton N, Sense-Cog WPg (2018) Visual and hearing impairments are associated with cognitive decline in older people. Age Ageing 47(4):575–581
DKY M (2018) Visual impairment contributes to frailty among a group of healthy community dwelling older population. J Geriatr Med Gerontol 4(2): 4:041
Liljas AEM, Carvalho LA, Papachristou E, De Oliveira C, Wannamethee SG, Ramsay SE et al (2017) Self-reported vision impairment and incident prefrailty and frailty in English community-dwelling older adults: findings from a 4-year follow-up study. J Epidemiol Community Health 71(11):1053–1058
Swenor BK, Lee MJ, Tian J, Varadaraj V, Bandeen-Roche K (2019) Visual Impairment and Frailty: Examining an understudied relationship. J Gerontol A Biol Sci Med Sci
Brussee T, van den Berg TJ, van Nispen RM, van Rens GH (2017) Associations between spatial and temporal contrast sensitivity and reading. Optom Vis Sci 94(3):329–338
Webb ALM, Hibbard PB (2019) The effect of facial expression on contrast sensitivity: a behavioural investigation and extension of Hedger, Adams & Garner (2015). PLoS ONE 14(11):e0205621
Spreng L, Favrat B, Borruat F-X, Vaucher P (2018) Cross-sectional study assessing the addition of contrast sensitivity to visual acuity when testing for fitness to drive. BMJ Open 8(1):e018546
Marron JA, Bailey IL (1982) Visual factors and orientation-mobility performance. Am J Optom Physiol Opt 59(5):413–426
Tielsch JM, Sommer A, Witt K, Katz J, Royall RM (1990) Blindness and visual impairment in an American urban population. Baltimore Eye Survey Arch Ophthalmol 108(2):286–290
Lam NW, Goh HT, Kamaruzzaman SB, Chin AV, Poi PJ, Tan MP (2016) Normative data for hand grip strength and key pinch strength, stratified by age and gender for a multiethnic Asian population. Singapore Med J 57(10):578–584
https://www.physiopedia.com/images/c/c7/Quidelines_for_interpreting_the_IPAQ.pdf
Klein BE, Klein R, Knudtson MD (2006) Frailty and age-related cataract. Ophthalmology 113(12):2209–2212
Varadaraj V, Lee MJ, Tian J, Ramulu PY, Bandeen-Roche K, Swenor BK (2019) Near Vision Impairment and Frailty: Evidence of an Association. Am J Ophthalmol 208:234–241
Cohen AK, Syme SL (2013) Education: a missed opportunity for public health intervention. Am J Public Health 103(6):997–1001
Curcio CA, Millican CL, Allen KA, Kalina RE (1993) Aging of the human photoreceptor mosaic: evidence for selective vulnerability of rods in central retina. Invest Ophthalmol Vis Sci 34(12):3278–3296
Montesano G, Gervasoni A, Ferri P, Allegrini D, Migliavacca L, De Cilla S et al (2017) Structure-function relationship in early diabetic retinopathy: a spatial correlation analysis with OCT and microperimetry. Eye (Lond) 31(6):931–939
Sieiro RdO, Coelho LM, Boas PCV, Fonseca SC, Souza SR, Guimarães TdP (2016) Avaliação da função de sensibilidade ao contraste em diferentes faixas etárias nas médias e altas frequências espaciais. Revista Brasileira de Oftalmologia 75:296–299
Regan D, Neima D (1983) Low-contrast letter charts as a test of visual function. Ophthalmology 90(10):1192–1200
Eshraghi H, Sanvicente CT, Gogte P, Waisbourd M, Lee D, Manzi RRS, Leiby BE, Richman J, Wizov SS, Spaeth GL (2019) Measuring contrast sensitivity in specific areas of vision: a meaningful way to assess quality of life and ability to perform daily activities in glaucoma. Ophthalmic Epidemiol 26(5):301–310
Rubin GS, Roche KB, Prasada-Rao P, Fried LP (1994) Visual impairment and disability in older adults. Optom Vis Sci 71(12):750–760
Soler V, Sourdet S, Balardy L, Abellan van Kan G, Brechemier D, Rouge-Bugat ME et al (2016) Visual impairment screening at the geriatric frailty clinic for assessment of frailty and prevention of disability at the gerontopole. J Nutr Health Aging 20(8):870–877
Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA et al (2007) Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci 62(7):744–751
Ensrud KE, Ewing SK, Taylor BC, Fink HA, Cawthon PM, Stone KL et al (2008) Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med 168(4):382–389
Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA et al (2009) A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc 57(3):492–498
Salonen L, Kivela SL (2012) Eye diseases and impaired vision as possible risk factors for recurrent falls in the aged: a systematic review. Curr Gerontol Geriatr Res 2012:271481
Funding
This study was initially funded by a Ministry of Higher Education High Impact Research Grant (UM.C/625/1/HIR/MOHE/ASH/02), and has since received continued funding from the Ministry of Higher Education Long Term Research Grant Scheme (LRGS/1/2019/UM//1/1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and ethical approval was obtained from the Medical Research Ethics Committee of the University Malaya Medical Centre. (ethic approval number 943.6).
Consent to participate
Consent taken from all the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amir, N.N., Kamaruzzaman, S.B., Effendi-Tenang, I. et al. Contrast sensitivity is associated with frailty. Eur Geriatr Med 12, 313–319 (2021). https://doi.org/10.1007/s41999-021-00450-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00450-2