Key summary points
To identifying tools for the reliable and systematic evaluation of oral health in older inpatients as well as to addressing the association between oral health and patients’ prognosis as measured by the Comprehensive Geriatric Assessment (CGA)-based Multidimensional Prognostic Index (MPI).
AbstractSection FindingsValid oral health examinations can be performed in older inpatients and are associated with individual multidimensional prognosis.
AbstractSection MessageOral health should be assessed and incorporated into clinical decisions to improve patients’ prognosis and prevention.
Abstract
Purpose
There is clear evidence for an association between oral health and systemic illnesses, geriatric syndromes, and mortality. Frail and multimorbid older people often suffer from insufficient oral health care, but standardized dental examinations are not routinely performed in clinical settings. The aim of this study was to verify the practicability of in-hospital oral health examinations and to identify their association with patients’ prognosis as assessed by means of the Comprehensive Geriatric Assessment (CGA)-based Multidimensional Prognostic Index (MPI).
Methods
One hundred hospitalized patients aged 65 years and older (mean age 76.9 years (SD 6.4); 58.2% male, 41.8% female) underwent a CGA-based MPI calculation at discharge with subdivision into three mortality risk groups (MPI-1, low risk, score 0–0.33; MPI-2, moderate risk, score 0.34–0.66; MPI-3, high risk, score 0.67–1). To identify the current oral health status and the Oral Health-related Quality of Life (OHRQoL), three oral health examinations were performed. Information on survival, the incidence of oral diseases, dental appointments, and treatments up to 6 months after discharge were collected.
Results
All oral health examinations were feasible during hospitalization and were associated with MPI prognosis, even though they were not associated with 6-month mortality. The MPI could not predict the use of dental health care or treatment, as, irrespective of MPI and oral health examinations, dental services were underutilized during follow up.
Conclusion
Besides MPI evaluation, oral health examinations should be implemented into an inhospital course to improve clinical decision-making as well as secondary and tertiary prevention of oral health- and related systemic diseases.
Trial Registration Number
German Clinical Trials Register: DRKS00013607 (07.02.2019, retrospectively registered).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite the increasing awareness of the need for dental care improvement in older subjects, the oral health (OH) status is still largely neglected in the clinical setting as well as in the mindset and training of many healthcare practitioners [1, 2]. Over the past years, several studies have shown that reduced OH is associated with poor general health, performance capability, and quality of life [3,4,5]. A bidirectional relationship could be shown for periodontitis and diabetes [3], and associations have been observed between OH and atherosclerosis and cardiovascular diseases [4]. Indeed, poor OH has been recently proposed as a geriatric syndrome [6]. A large body of evidence recognizes poor OH as a risk factor for aspiration pneumonia and related death [7]. Caries, periodontal disease, and tooth loss lead in the long term to masticatory deficiency, which in turn is associated with cognitive impairment [8], malnutrition [9], and lower quality of life [5]. In summary, poor OH has been shown to be associated with poor health outcomes [10, 11]. Accordingly, the World Health Organization has designated OH as an essential determinant of quality of life, overall health, and happiness [12].
The systematic evaluation of the oral cavity is often not part of the routine examination carried out in older inpatients outside of geriatric settings. The current problem-oriented behavior largely overcoming preventive dental visits, however, yields a great challenge for the healthcare systems. The already high, rapidly increasing number of older adults with demanding dental needs exacerbates the consequences of poor prevention [13]. A systematic OH screening in older multimorbid patients admitted to the hospital could at least in part compensate for the above-mentioned challenges. In addition, as OH contributes substantially to the general health and quality of life of older multimorbid patients, it may impact on overall prognosis, but this has not been demonstrated up to date. To fill this gap of knowledge, the present observational prospective study was designed to investigate the association between OH and a Comprehensive Geriatric Assessment (CGA)-based prognosis evaluation by means of the Multidimensional Prognostic Index (MPI). This is an established tool validated in several thousand older patients worldwide to predict short- and long-term mortality among other outcomes in older subjects [14]. It has been applied in several acute and chronic diseases (e.g. pneumonia [15], dementia [16], chronic kidney disease [17], and transient ischemic attack [18]) and can help healthcare professionals to improve clinical decisions [19,20,21]. The aim of the present study was to evaluate the presence and characteristics of the relationship between OH as assessed by means of specific OH evaluation instruments and individual overall prognosis measured by the MPI.
Patients and methods
Patients
Between December 2017 and March 2019, 209 consecutive patients admitted to the Department II of Internal Medicine of the University of Cologne, Germany, were screened for inclusion in the prospective observational EUROpean Study Of Older Subjects With Atrial Fibrillation (EUROSAF). Patients were included if aged 65 years and older, with a documented diagnosis of non-valvular atrial fibrillation and willing/able to participate. Exclusion criteria were (1) refusal to participate (n = 78), (2) inability to consent (n = 8), (3) inability to speak German or speech disorder (n = 17), and (4) repeated impossibility to meet the patient for recruitment (n = 6). Patients were asked to undergo an additional OH examination and upon consent, a final sample of 100 participants was included in the present analysis.
Assessment of participants
Geriatric assessment
MPI
The MPI calculation [14] as an index representing mortality prognosis was performed one the day prior to discharge. The MPI is based on a standardized CGA including eight domains: (1) Cumulative Illness Rating Scale (CIRS) [22], (2) Exton Smith Scale (ESS) [23] for the assessment of pressure ulcer risk, (3) Mini Nutritional Assessment Short Form (MNA-SF) [24], (4) Katz’s Activities of Daily Living (ADL) [25], (5) Lawton’s Instrumental Activities of Daily Living (IADL) [26], (6) Short Portable Mental Status Questionnaire (SPMSQ) [27], (7) number of drugs including over the counter (OTC) drugs, and (8) cohabitation status. For each domain, a tripartite hierarchy was used, i.e. 0 = no problems, 0.5 = minor problems, and 1 = major problems based on the conventional cut- off points. The sum of the calculated scores from the eight domains was divided by 8 to obtain the final MPI risk score. The MPI is expressed as a continuous value from 0 = lowest risk to 1 = highest risk of mortality. Appropriate validated cut-off have been calculated to identify three levels of mortality risks as follows: MPI-1, 0–0.33 = low risk, MPI-2, 0.34–0.66 = moderate risk, and MPI-3, 0.67–1, high risk [14].
OH examinations
The OH examinations included the Kayser-Jones Brief Oral Health Status Examination (BOHSE) [28], Decayed, Missing, or Filled Teeth Index (DMFT) [29], the Geriatric Oral Health Assessment Index (GOHAI) [30, 31], and a self-developed OH questionnaire (OHQ). The rationale for the choice of the used instruments was to employ validated, simple and accessible instruments that also can be performed in long-term care by non-dental professionals with the goal of implementation into clinical routine. Examinations were conducted by one dentist in the patient’s rooms. Depending on physical condition, the examination was performed lying or sitting in bed.
BOHSE
The BOHSE is a ten-item examiner-rated screening examination that was originally developed for nursing staff to assess the condition of the oral cavity, surrounding tissues, and teeth. It has been chosen for use in this study because it is a simple and accessible instrument that represents a good overview of all aspects of OH [28]. The ten categories are (1) lymph nodes, (2) lips, (3) tongue, (4) tissue inside the cheek, floor, and roof of mouth, (5) gums between teeth and/or under artificial teeth, (6) saliva, (7) condition of natural teeth, (8) condition on artificial teeth (9) pairs of teeth in chewing position (natural or artificial) and (10) oral cleanliness. Each item is rated on a 3-point scale (0, 1, 2) from 0 = normal/healthy to 2 = problematic/unhealthy. The final score is the sum from the 10 categories ranged from 0 = very healthy to 20 = very unhealthy [28]. While the cumulative score is important in assessing OH, the score for each item must be considered individually. If any category contains a score of 1 or 2, referral to a dentist is recommended.
DMFT
The DMFT Index is widely used to describe the past and present dental caries experience [29]. DMFT is a validated tool for younger and older subjects [13, 32]. It is applied to the permanent dentition and is expressed as the total number of teeth that are decayed (D), missing (M) or filled (F). The final score ranges from 0 to 28 (third molars were excluded).
GOHAI
The Geriatric Oral Health Assessment Index (GOHAI) is a validated instrument that assesses self-perception of OH. Besides measuring the individual’s perception of oral functional problems, it also estimates the psychological impact associated with oral disease. The GOHAI consists of 12 questions focusing on three dimensions: (1) Physical function (chewing, pronunciation, and swallowing); (2) Psychological function (pre-occupation or interest in OH, dissatisfaction with one's appearance, self-perception in terms of OH, and avoidance of social interactions due to oral problems); (3) Pain or discomfort (use of medications to relieve pain or discomfort in the oral cavity). According to Atchison et al., in our study, the questions were measured using a 5-point Likert scale (always 5; often 4; sometimes 3; seldom 2; never 1) [30]. In the original publication of the German version of the GOHAI [31] used in this publication, a forward translation was performed by a bilingual professional translator whose first language was German. This version was revised and scrutinized for specific dental terms by clinicians, before back-translation into English by a bilingual professional translator whose first language was English. The original English version, the back-translated version, and the German version were revised by three professional translators and scrutinized for changes in sense. The German version of the GOHAI showed sufficient reliability, validity, and responsiveness to be used as a measure of Oral Health-related Quality of Life (OHRQoL) in longitudinal studies of older persons [31] and was therefore used in this study.
OHQ
A self-developed specific OH questionnaire (OHQ) with seven binary questions (yes/no) collected information during the patient’s hospital stay regarding toothlessness, presence of dentures, swallowing disorders, taste disturbance, bleeding gums, tooth loss, and periodontitis treatment during the last 12 months.
Follow-up
All participants received phone interviews 6 months after discharge. Beyond verification of survival, binary (yes/no) questions about dental appointments and treatments, tooth loss, oral pain, gum bleeding, satisfaction with dental protheses (dentures, bridges, crowns, and dental implants), and xerostomia within the 6 months after the initial evaluation was collected.
Registration, participant consent, and ethics
The study is registered at the German Clinical Trials Register (DRKS00013607) and the authors declare that the experiments respect the ethical standards for human experimentation that are stated in the Declaration of Helsinki of 1975, as revised in 2000, as well as the national law. The study was approved by the Ethical Committee of the University Hospital of Cologne, Germany, and each patient or proxy respondent signed informed consent.
Statistical analysis
Descriptive statistics were expressed using the absolute number and relative frequencies for the description of categorical variables and mean (SD) or median (IQR) for continuous variables.
To test associations between MPI risk group at discharge and demographical and clinical characteristics, Chi-Square test or Fisher’s exact test for categorical variables, univariate ANOVA or Kruskal–Wallis test for continuous variables were used after testing for normal distribution. p values were analyzed for patients who did not die during hospitalization.
For follow-up at 6 months both MPI risk groups at discharge and BOHSE groups were tested for associations towards clinical outcomes as described above.
Odds ratios to express the associations between BOHSE, DMFT, GOHAI, and MPI scores at discharge were calculated using a multivariate ordered logistic regression analysis adjusted for age, gender, and years of education.
Two-tailed probabilities with a significant level alpha of 0.05 were considered for all tests.
Results
Demographics
The demographic and clinical characteristics of the patients according to the MPI group are described in Table 1. Nine patients died during hospitalization.
The mean age was 76.9 years (SD 6.4) with a median of 12 years of education (IQR 1–3). 41.8% of the patients were women. The median length of hospital stay was 11 days (IQR 6–21) and was significantly associated with the MPI (p = 0.004). As expected, the prevalence of cardiovascular, respiratory, musculoskeletal, and kidney diseases was relatively high in this patient sample (Table 1). The strongest associations according to MPI group were found for hypertension (p = 0.038), upper gastrointestinal tract disease (p = 0.013), and psychiatric disease (p = 0.023). Every patient had at least 3 or more medications prescribed at discharge. Most of the patients (59/91; 64.8%) took more than 9 medications [mean (SD) = 9.6 (2.7)]. Yet, a significant statistical association between MPI groups and medication use could not be detected (p = 0.228). Physical immobility was significantly increased in higher MPI groups (MPI-1 = 0.0%; MPI-2 = 32.8%; MPI-3 = 73.3%; p < 0.0001).
OH examinations
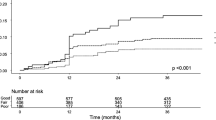
OH examinations were carried out within temporal and methodological frames compatible with the clinical routine in all patients who had signed the informed consent. OH examination indices and OHQ results according to the MPI group are displayed in Table 1. BOHSE, DMFT and GOHAI are presented as a box-plots according to MPI risk groups in Fig. 1.
BOHSE
The median BOHSE score was 5 (IQR 3–8). Higher MPI groups were correlated with a higher BOHSE score (p = 0.001), displaying more OH problems (Fig. 1). BOHSE subgroup saliva demonstrated a significant increase from 0 (tissues moist, saliva free-flowing and watery; IQR 0–0) for MPI-1 to 1 (tissues dry and sticky; IQR 0–1) for MPI- 3 (p = 0.029). A closer look at the MPI subitems revealed significant associations of BOHSE to ADL/ IADL. BOHSE increased from 5 (IQR 3–6) for ADL 0 (no problems) to 7.5 (IQR 3.75–10.25) for ADL 1 (major problems) (p = 0.003) and from 5 (IQR 2–6) for IADL 0 (no problems) to 6 (IQR 3–9) for IADL 1 (major problems) (p = 0.029).
GOHAI
The median GOHAI score was 54 (IQR 48–56). Higher MPI groups were associated with lower GOHAI score (p < 0.001) (Fig. 1), displaying lower OHRQoL. For MPI subitems the GOHAI score decreased from 55 (IQR 50.25–57) for ADL 0 (no problems) to 48 (IQR 41.5–54.25) for ADL 1 (major problems) (p = 0.005).
DMFT
The median value of DMFT Index was 18 (IQR 10–28) and showed an increase according to higher MPI, but without statistical significance (p = 0.072) (Fig. 1). Median M (missing) increased from 9 (IQR 5–23) for MPI-1 to 23 (IQR 10–28) for MPI- 3, without showing statistical significance (p = 0.172). Overall median for D (decayed) was 0 (IQR 0–2; p = 0.885).
OHQ
The occurrence of a swallowing disorder and taste disturbance was significantly associated with a higher MPI (p = 0.006; p = 0.019). All other items of the OHQ showed no significant association with MPI risk groups (Table 1).
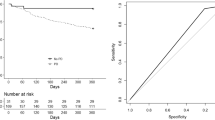
Multivariate ordered logistic regression
A multivariate ordered logistic regression model (Fig. 2) adjusted for age, gender, and years of education showed a significant association between all OH indices and MPI subgroups. For one unit increase in BOHSE, the odds of being allocated to a severe MPI risk group versus the combined moderate and mild categories were 1.34 greater (p < 0.001). For one unit increase in DMFT Index, the odds of a higher MPI group versus a lower MPI group was 1.06 greater (p = 0.047). In addition, each increase in GOHAI was significantly associated with a lower risk of higher MPI (OR 0.87, p < 0.001) (Fig. 2).
Follow-up
A relatively high number of 26 patients were lost at follow-up. 6/26 patients refused to participate in the phone follow-up. The rest was not reached after calling four times within the frame of two months. As a result, the final sample size for follow-up at 6 months included 65 patients. All-cause mortality at 6 months was 16/65 (24.6%). The descriptive statistics of follow-up outcomes according to MPI risk score are presented in Table 2.
About a quarter of the 49 patients (13/49; 26.5%) had a dental appointment in the 6 months follow-up period. Fisher’s exact test showed no significant association of dental appointments with MPI scores (Table 2). Overall, three-quarter of the patients (36/49; 73.5%) claimed to be satisfied with their dental prostheses. Patients in the MPI-3 group were more satisfied (4/5; 80%) than patients belonging to MPI-2 (23/30; 76.7%) and MPI-1 (9/14; 64.3%). Half of the patients (26/49; 53.1%) indicated to suffer from xerostomia, decreasing for patients from MPI-1 (8/14; 57.1%) to MPI-3 (1/5; 20.0%). Nevertheless, neither satisfaction with dental protheses nor xerostomia were significantly associated to MPI (p = 0.708; p = 0.360) or BOHSE category (p = 0.073; p = 0.516). The same applies to dental treatments, tooth loss, tooth pain, and bleeding gums (Table 2).
A multivariate ordered logistic regression model (Table 3) adjusted for age, gender and years of education shows that only the MPI score was associated with mortality at 6 months (OR 1.46, 95% CI 1.00–2.14, p = 0.051) with the highest area under the curve (AUC) (73.3%). On the other side, both BOHSE (OR 1.08, 95% CI 0.88–1.31, p = 0.462), DMFT (OR 1.02, 95% CI 0.95–1.10, p = 0.484) and GOHAI (OR 0.94, 95% CI 0.86–1.03, p = 0.156) did not demonstrate a significant association with mortality at 6 months.
Discussion
In the present study, it was possible to show that an OH examination is feasible in older inpatients and yields important additional information on conditions of accepted relevance for overall health status and well-being [12]. Even though feasibility was not statistically measured, all OH examinations showed a good level of practicability in hospital routine: they were not particularly time-consuming (10–15 min for all of them), nor costly, nor difficult to accept by patients. Although the OH evaluation slightly prolonged the overall patients’ assessment, the benefit of OH-related diagnosis overcomes the minimal negative effects of time loss. One of the main results of this study is that poorer OH and MPI are associated with each other independent of age, gender, and education, suggesting that OH impacts the individual multidimensional prognosis. The MPI-based prognosis has already been associated with several acute and chronic diseases (e.g. pneumonia [15], dementia [16], chronic kidney disease [17], and transient ischemic attack [18]). The present study shows an additional association of the MPI with OH. This finding is relevant since poor OH affects a great number of persons and this number will massively increase in the next years [33]. All tested OH indices indicate a significant correlation to MPI. BOHSE showed the strongest association to individual MPI values. Since BOHSE comprehends a multidimensional approach to the oral cavity, considering not only the condition of natural or artificial teeth but also of surrounding tissues (lips, tongue, cheek) and moistening of oral mucosa, it might be a relevant and daily applicable option to represent OH status. Originally, BOHSE was developed for nurses to screen nursing home residents. Since in Germany dentists and the dental team are not operationalized part of the in-hospital geriatric team, the implementation of a practical instrument like BOHSE, which can be used by non-dental professionals, might partially compensate this lack and allow adequate screening of an important domain of health in advanced age. However, besides sensitizing caring staff for OH, the ultimate goal should remain the implementation of the dentist’s expertise into the daily routine of geriatric inpatients.
The impact of OH on overall health and prognosis has become more important in recent years, but there is a lack of studies especially for the group of vulnerable elders with care needs. However, as more and more interrelationships are emerging, especially from periodontitis to general diseases and chronic inflammation [3, 4, 7, 34], more research is needed. In some studies, poor OH and swallowing dysfunction were identified as independent risk factors for reduced quality of life and mortality in older patients [10, 11, 35]. Because of these correlations, reduced OH may have an impact on mortality and prognosis. In this study, we could not show an association with mortality, probably due to the small sample size and the short observation period. To clarify this question, further studies are needed that take these increased sample sizes in a longitudinal study design into account. Nevertheless, all OH parameters were associated with MPI total score and MPI subitems. This may show an indirect association to prognosis, because the MPI itself is a validated tool to predict short- and long-term mortality in older persons, as it has been shown in this study, too. As stated above, poor OH is already discussed as a new potential geriatric syndrome [6, 36]. Meyer et al. have shown that many geriatric syndromes have a prognostic relevance and suggested an implementation to improve clinical decision-making and management of older patients [37]. The same seems to apply to OH.
In the present study, about two-thirds of the patients had moderate or severe oral care problems. Patients with higher MPI scores even required extended dental care and treatment and quoted less OHRQoL, as shown by higher BOHSE/ DMFT scores and lower GOHAI scores. Because only 26.5% of patients undergoing follow-up reported having visited dental offices, it is difficult to obtain significant associations for MPI groups. Nevertheless, as another key finding, dental services were generally underutilized in practice, irrespective of the MPI discharge group. It is well known that older, frail, and multimorbid patients refrain from dental care [38]. According to scientific epidemiologic and psychosocial literature, older adults are faced with numerous barriers to OH care including (1) income and education, (2) availability of dental and medical insurance, (3) urban vs. rural residence, (4) systemic and functional health, and (5) oral health literacy (OHL) [39]. When addressing these barriers in the present patient population, systemic and functional health as well as OHL appear to have the greatest impact on underused dental services. In fact, median GOHAI scores decreased with higher MPI scores but overall the former indicated overall good OHRQoL. On the other hand, median BOHSE increased with higher MPI scores, indicating increasing OH problems. These apparently contradictory results have been found in several other studies, confirming that older people’s subjective needs and perceived symptoms may differ from the objective clinical assessment of OH [35, 40]. The same applies to the yet underrecognized OH problem of dry mouth. Since it is well known that dry mouth problems are highly prevalent in the older population, this factor should be co-evaluated in future studies to more comprehensively address the prognostic signature of OH—especially in the context of polymedication, multimorbidity, reduced OH prognosis, and quality of life.
Studies have shown that dental visits can influence individual perceptions of the dentition and the frequency of dental visits has been shown to be a significant predictor of perceived OH status in older subjects [41]. Also in the scientific literature, there is an evident lack of patient-centered outcome parameters addressing the awareness of patients regarding their own OH including especially patients with cognitive decline. It is highly important to raise awareness for oral diseases and motivate patients and caregivers to comply with their needs. The newest research on global OH explicitly favors oral disease prevention and health promotion to cure oral diseases [33]. A recently published solution in an outpatient setting suggests that general practitioners, as a group of doctors that senior citizens are most likely to visit throughout their lives, could serve as an interface to dentistry. For this purpose, a very simple and practical instrument—the geriatric outpatient oral health screening (GAMS)—was developed and validated [42]. The GAMS focuses on dental aspects relevant for geriatric patients, such as chewing problems, pain, periodontitis, bad breath or dry mouth in dichotomous questions [42]. Even if legal and administrative conditions in Germany do not yet make this transfer practice possible, this would be a desirable process in the long term. To achieve this goal in a clinical setting, the implementation of a routine, feasible OH screening—like BOHSE for example or the described GAMS—during hospitalization could be helpful. After examination, patients should be informed about their OH status to improve OHL. To increase the chances of further and regular dental appointments, discharge records should contain information about the OH results obtained and a referral to the general dentist. Here, a long-term goal should be the implementation of intersectoral healthcare settings including specific structures for OH evaluation in advanced age. One good example of one possible approach is the study from Martín et al. [43] who investigated older residents with oropharyngeal dysphagia admitted to an intermediate care unit. A minimal-massive intervention (MMI) approach, including OH and hygiene recommendations as well as evaluation and treatment of swallowing dysfunction and nutritional status, increased survival, reduced respiratory infections, and improved nutrition and functional status [43].
This study has several limitations. One limitation of the study is that the sample is a subpopulation from the EUROSAF study which evaluates the clinical benefit/risk ratio of anticoagulant treatments of older persons aged 65 or older with atrial fibrillation. Therefore, the study population does not necessarily represent the general population and may contain a selection/sampling bias. However, while caution in interpretation and generalization of the results is necessary, the distribution of the MPI values suggests enough variability to guarantee the interpretation of the observations and their possible use in clinical practice.
A general weakness of questionnaires (OHQ, GOHAI, phone interviews) is of course the reliability of the patients’ statements. Nevertheless, for healthcare- and quality of life-related outcomes in advanced age, self-/interview-administered questionnaires are established and commonly used [44].
Furthermore, only one dentist provided all services to the patients. Regarding the external validity of this data, there might be person-dependent differences in quality regarding the treatment success achieved. On the other hand, with the same dentist performing all examinations, inter-examiner differences were eliminated.
Even though the three OH examinations showed significant results in association to MPI, it should be noted that there are more valid OH indicators, such as the plaque index (PI) [45], gingivitis index (GI) [46], Quigley- Hein index (QHI) [47], papilla bleeding index (PBI) [48] and oral hygiene index (OHI) [49]. These indices might allow a more differentiated assessment of the OH status. The rationale for the choice of the used instruments was to employ validated, simple and accessible instruments that also can be performed in long-term care by non-dental professionals with the goal of implementation into clinical routine.
Another limitation is the relatively low sample size at 6 months follow-up, with 16 patients deceased during follow-up and 26 patients lost at follow-up. However, these are percentages known from previous studies [50] and represent the expected dropout-rates when performing studies with multimorbid patient groups [37].
Conclusion
Inpatient OH examinations evaluated in the present study appear to represent a practical instrument in this highly vulnerable population and showed a strong impact on personal prognosis. Nevertheless, dental services were underutilized irrespectively of MPI values. These findings suggest the urgent need for the implementation of a routine, feasible OH screening in the clinical setting. Post-discharge referral to a dental professional or a comprehensive multidisciplinary clinical management involving OH might improve secondary and tertiary prevention of both oral and systemic diseases and strengthen patient awareness for OH. More research is needed with larger patient samples to address the multidimensional mechanisms linking OH to the individual long-term prognosis.
Code availability
All analyses were performed using STATA software (version 14.1, StataCorp., College Station, TX, USA) and SPSS software (Statistical Package for Social Sciences, SPSS Inc., Chicago, IL, USA, version 26.0).
References
Binkley C, Furr LA, Carrico R, McCurren C (2004) Survey of oral care practices in US intensive care units. Am J Infect Control 32:161–169. https://doi.org/10.1016/j.ajic.2003.05.001
Ástvaldsdóttir Á, Boström A-M, Davidson T, Gabre P, Gahnberg L, Englund GS, Skott P, Ståhlnacke K, Tranæus S, Wilhelmsson H, Wårdh I, Östlund P, Nilsson M (2018) Oral health and dental care of older persons—a systematic map of systematic reviews. Gerodontology 35:290–304. https://doi.org/10.1111/ger.12368
Graziani F, Gennai S, Solini A, Petrini M (2018) A systematic review and meta-analysis of epidemiologic observational evidence on the effect of periodontitis on diabetes An update of the EFP-AAP review. J Clin Periodontol 45:167–187. https://doi.org/10.1111/jcpe.12837
Aarabi G, Eberhard J, Reissmann DR, Heydecke G, Seedorf U (2015) Interaction between periodontal disease and atherosclerotic vascular disease—fact or fiction? Atherosclerosis 241:555–560. https://doi.org/10.1016/j.atherosclerosis.2015.04.819
Kimura Y, Wada T, Ishine M, Ishimoto Y, Kasahara Y, Hirosaki M, Konno A, Nakatsuka M, Sakamoto R, Okumiya K, Otsuka K, Matsubayashi K (2009) Community-dwelling elderly with chewing difficulties are more disabled, depressed and have lower quality of life scores. Geriatr Gerontol Int 9:102–104. https://doi.org/10.1111/j.1447-0594.2008.00489.x
van der Putten G-J, de Baat C, Visschere LD, Schols J (2014) Poor oral health, a potential new geriatric syndrome. Gerodontology 31:17–24. https://doi.org/10.1111/ger.12086
van der Maarel-Wierink CD, Vanobbergen JNO, Bronkhorst EM, Schols JMGA, de Baat C (2013) Oral health care and aspiration pneumonia in frail older people: a systematic literature review. Gerodontology 30:3–9. https://doi.org/10.1111/j.1741-2358.2012.00637.x
Kossioni AE (2018) The association of poor oral health parameters with malnutrition in older adults: a review considering the potential implications for cognitive impairment. Nutrients. https://doi.org/10.3390/nu10111709
Huppertz VAL, van der Putten G-J, Halfens RJG, Schols JMGA, de Groot LCPGM (2017) Association between malnutrition and oral health in dutch nursing home residents: results of the LPZ study. J Am Med Dir Assoc 18:948–954. https://doi.org/10.1016/j.jamda.2017.05.022
Klotz A-L, Hassel AJ, Schröder J, Rammelsberg P, Zenthöfer A (2018) Is compromised oral health associated with a greater risk of mortality among nursing home residents? A controlled clinical study. Aging Clin Exp Res 30:581–588. https://doi.org/10.1007/s40520-017-0811-y
Hägglund P, Koistinen S, Olai L, Ståhlnacke K, Wester P, Levring Jäghagen E (2019) Older people with swallowing dysfunction and poor oral health are at greater risk of early death. Community Dent Oral Epidemiol 47:494–501. https://doi.org/10.1111/cdoe.12491
Haumschild MS, Haumschild RJ (2009) The importance of oral health in long-term care. J Am Med Dir Assoc 10:667–671. https://doi.org/10.1016/j.jamda.2009.01.002
Jordan RA, Bodechtel C, Hertrampf K, Hoffmann T, Kocher T, Nitschke I, Schiffner U, Stark H, Zimmer S, Micheelis W, DMS V Surveillance Investigators’ Group (2014) The fifth german oral health study (Fünfte Deutsche Mundgesundheitsstudie, DMS V)—rationale, design, and methods. BMC Oral Health 14:161. https://doi.org/10.1186/1472-6831-14-161
Pilotto A, Ferrucci L, Franceschi M, D’Ambrosio LP, Scarcelli C, Cascavilla L, Paris F, Placentino G, Seripa D, Dallapiccola B, Leandro G (2008) Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res 11:151–161. https://doi.org/10.1089/rej.2007.0569
Pilotto A, Addante F, Ferrucci L, Leandro G, D’Onofrio G, Corritore M, Niro V, Scarcelli C, Dallapiccola B, Franceschi M (2009) The multidimensional prognostic index predicts short- and long-term mortality in hospitalized geriatric patients with pneumonia. J Gerontol A Biol Sci Med Sci 64:880–887. https://doi.org/10.1093/gerona/glp031
Pilotto A, Sancarlo D, Panza F, Paris F, D’Onofrio G, Cascavilla L, Addante F, Seripa D, Solfrizzi V, Dallapiccola B, Franceschi M, Ferrucci L (2009) The Multidimensional Prognostic Index (MPI), based on a comprehensive geriatric assessment predicts short- and long-term mortality in hospitalized older patients with dementia. J Alzheimer’s Dis 18:191–199. https://doi.org/10.3233/JAD-2009-1139
Pilotto A, Sancarlo D, Aucella F, Fontana A, Addante F, Copetti M, Panza F, Strippoli GFM, Ferrucci L (2012) Addition of the Multidimensional Prognostic Index to the estimated glomerular filtration rate improves prediction of long-term all-cause mortality in older patients with chronic kidney disease. Rejuvenation Res 15:82–88. https://doi.org/10.1089/rej.2011.1210
Sancarlo D, Pilotto A, Panza F, Copetti M, Longo MG, D’Ambrosio P, D’Onofrio G, Ferrucci L, Pilotto A (2012) A Multidimensional Prognostic Index (MPI) based on a comprehensive geriatric assessment predicts short- and long-term all-cause mortality in older hospitalized patients with transient ischemic attack. J Neurol 259:670–678. https://doi.org/10.1007/s00415-011-6241-4
Bureau M-L, Liuu E, Christiaens L, Pilotto A, Mergy J, Bellarbre F, Ingrand P, Paccalin M, MPI_AGE Project Investigators (2017) Using a multidimensional prognostic index (MPI) based on comprehensive geriatric assessment (CGA) to predict mortality in elderly undergoing transcatheter aortic valve implantation. Int J Cardiol 236:381–386. https://doi.org/10.1016/j.ijcard.2017.02.048
Meyer AM, Becker I, Siri G, Brinkkötter PT, Benzing T, Pilotto A, Polidori MC (2019a) New associations of the Multidimensional Prognostic Index. Z Gerontol Geriatr 52:460–467. https://doi.org/10.1007/s00391-018-01471-6
Pilotto A, Panza F, Sancarlo D, Paroni G, Maggi S, Ferrucci L (2012) Usefulness of the multidimensional prognostic index (MPI) in the management of older patients with chronic kidney disease. J Nephrol 25(Suppl 19):S79-84. https://doi.org/10.5301/jn.5000162
Linn BS, Linn MW, Gurel L (1968) Cumulative Illness Rating Scale. J Am Geriatr Soc 16:622–626. https://doi.org/10.1111/j.1532-5415.1968.tb02103.x
Bliss MR, McLaren R, Exton-Smith AN (1966) Mattresses for preventing pressure sores in geriatric patients. Mon Bull Minist Health Public Health Lab Serv 25:238–268
Sancarlo D, D’Onofrio G, Franceschi M, Scarcelli C, Niro V, Addante F, Copetti M, Ferrucci L, Fontana L, Pilotto A (2011) Validation of a Modified-Multidimensional Prognostic Index (m-MPI) including the Mini Nutritional Assessment Short-Form (MNA-SF) for the prediction of one-year mortality in hospitalized elderly patients. J Nutr Health Aging 15:169–173. https://doi.org/10.1007/s12603-010-0293-5
Katz S, Downs TD, Cash HR, Grotz RC (1970) Progress in development of the index of ADL. Gerontologist 10:20–30. https://doi.org/10.1093/geront/10.1_part_1.20
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186. https://doi.org/10.1093/geront/9.3_Part_1.179
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23:433–441. https://doi.org/10.1111/j.1532-5415.1975.tb00927.x
Kayser-Jones J, Bird WF, Paul SM, Long L, Schell ES (1995) An instrument to assess the oral health status of nursing home residents. Gerontologist 35:814–824. https://doi.org/10.1093/geront/35.6.814
Larmas M (2010) Has dental caries prevalence some connection with caries index values in adults? Caries Res 44:81–84. https://doi.org/10.1159/000279327
Atchison KA, Dolan TA (1990) Development of the Geriatric Oral Health Assessment Index. J Dent Educ 54:680–687
Hassel AJ, Rolko C, Koke U, Leisen J, Rammelsberg P (2008) A German version of the GOHAI. Community Dent Oral Epidemiol 36:34–42. https://doi.org/10.1111/j.1600-0528.2007.00351.x
De Angelis F, Basili S, Giovanni F, Dan Trifan P, Di Carlo S, Manzon L (2018) Influence of the oral status on cardiovascular diseases in an older Italian population. Int J Immunopathol Pharmacol 32:394632017751786. https://doi.org/10.1177/0394632017751786
Watt RG, Daly B, Allison P, Macpherson LMD, Venturelli R, Listl S, Weyant RJ, Mathur MR, Guarnizo-Herreño CC, Celeste RK, Peres MA, Kearns C, Benzian H (2019) Ending the neglect of global oral health: time for radical action. Lancet 394:261–272. https://doi.org/10.1016/S0140-6736(19)31133-X
Müller F (2015) Oral hygiene reduces the mortality from aspiration pneumonia in frail elders. J Dent Res 94:14S-16S. https://doi.org/10.1177/0022034514552494
Barbe AG, Heinzler A, Derman S, Hellmich M, Timmermann L, Noack MJ (2017) Hyposalivation and xerostomia among Parkinson’s disease patients and its impact on quality of life. Oral Dis 23:464–470. https://doi.org/10.1111/odi.12622
Halpern LR (2020) The Geriatric Syndrome and Oral Health: navigating oral disease treatment strategies in the elderly. Dent Clin N Am 64:209–228. https://doi.org/10.1016/j.cden.2019.08.011
Meyer AM, Becker I, Siri G, Brinkkötter PT, Benzing T, Pilotto A, Polidori MC (2019b) The prognostic significance of geriatric syndromes and resources. Aging Clin Exp Res. https://doi.org/10.1007/s40520-019-01168-9
Dolan TA, Atchison K, Huynh TN (2005) Access to dental care among older adults in the United States. J Dent Educ 69:961–974
Kiyak HA, Reichmuth M (2005) Barriers to and enablers of older adults’ use of dental services. J Dent Educ 69:975–986
Tenani CF, De Checchi MHR, Bado FMR, Ju X, Jamieson L, Mialhe FL (2019) Influence of oral health literacy on dissatisfaction with oral health among older people. Gerodontology. https://doi.org/10.1111/ger.12443
Gift HC, Atchison KA, Drury TF (1998) Perceptions of the natural dentition in the context of multiple variables. J Dent Res 77:1529–1538. https://doi.org/10.1177/00220345980770070801
Barbe AG, Spiritus S, Hagemeier A, Noack MJ, Röhrig G (2020) Oral health assessment of seniors under outpatient care by family doctors: development and validation of the geriatric outpatient oral health screening. Z Gerontol Geriatr. https://doi.org/10.1007/s00391-020-01730-5
Martín A, Ortega O, Roca M, Arús M, Clavé P (2018) Effect of a minimal-massive intervention in hospitalized older patients with oropharyngeal dysphagia: a proof of concept study. J Nutr Health Aging 22:739–747. https://doi.org/10.1007/s12603-018-1043-3
Schofield P (2018) The assessment of pain in older people: UK national guidelines. Age Ageing 47:i1–i22. https://doi.org/10.1093/ageing/afx192
Silness J, Löe H (1964) Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22:121–135. https://doi.org/10.3109/00016356408993968
Löe H, Silness J (1963) Periodontal disease in Pregnancy I. Prevalence and severity. Acta Odontol Scand 21:533–551. https://doi.org/10.3109/00016356309011240
Turesky S, Gilmore ND, Glickman I (1970) Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol 41:41–43. https://doi.org/10.1902/jop.1970.41.41.41
Saxer UP, Mühlemann HR (1975) Motivation and education. SSO Schweiz Monatsschr Zahnheilkd 85:905–919
Greene JC (1960) Nutrition in a collegiate basic nursing curriculum. Nurs Outlook 8:314–315
Barbe AG, Küpeli LS, Hamacher S, Noack MJ (2020) Impact of regular professional toothbrushing on oral health, related quality of life, and nutritional and cognitive status in nursing home residents. Int J Dent Hyg. https://doi.org/10.1111/idh.12439
Acknowledgements
The preliminary results of the present study were presented at the 14th International Congress of the European Geriatric Medicine Society (EuGMS) in Berlin in October 2018.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
NN, AMM, and MCP conceived and designed the clinical trial. NN, LP, AH, and JV performed the experiments. NN and GS analysed the data. NN wrote the paper. NN, AMM, AGB, and MCP helped with the conception of the manuscript. NN, AMM, GS, LP, AH, JV, TB, AP, AGB, and MCP made critical revisions.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethical Committee of the University Hospital of Cologne, Germany (the study is registered at the German Clinical Trials Register: DRKS00013607) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Each patient or proxy respondent signed informed consent.
Consent for publication
Each author gave his consent to the publications of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Noetzel, N., Meyer, A.M., Siri, G. et al. The impact of oral health on prognosis of older multimorbid inpatients: the 6-month follow up MPI oral health study (MPIOH). Eur Geriatr Med 12, 263–273 (2021). https://doi.org/10.1007/s41999-020-00427-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-020-00427-7