Abstract
Brief meditations led by audio versus visual stimuli can lead to differential effects on mood and cognition in healthy people. We examine whether similar effects were evident amongst schizophrenia patients. Forty-three patients underwent either 30-min image- (e.g. a mountain stream; n = 15) or audio-led (e.g. running water; n = 15) meditations or waited 30 min without instructions (n = 13). Prior to and following the meditation/wait, participants completed a self-report measure of positive and negative affect and the Trail Making Test to measure attentional shifting abilities. Participants who underwent a visual-led meditation were significantly more positive than those who underwent an audio-led meditation or if they did not meditate. Irrespective of meditation modality, participants showed significant improvement in attentional shifting abilities. Brief meditative practice amongst patients with schizophrenia may have immediate effects on mood and cognition. Future research must explore these effects in larger mindfulness programmes and with longer follow-up assessments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mindfulness—a meditation-based psychotherapy involving awareness and non-judgemental acceptance of internal and external experiences—has been found to have small-to-moderate effects in the treatment of the positive and negative symptoms that are common in schizophrenia (Khoury et al. 2013a; Louise et al. 2018). Mindfulness is particularly effective at improving the negative symptoms encountered in schizophrenia (Khoury et al. 2013a) with effect sizes that are comparable with mindfulness for other psychiatric disorders (Khoury et al. 2013b) and other cognitive-behavioural psychotherapies for schizophrenia (Wykes et al. 2008). However, these effect sizes are nonetheless in the small-to-moderate range, suggesting that there is a need to improve mindfulness’ effects on the symptoms found within schizophrenia. In order to achieve this, the underlying mechanisms of mindfulness and the factors which moderate its effectiveness must be examined (Hölzel et al. 2011). To that end, studies have examined variations of mindfulness where different elements are emphasised, such as compassion towards the self (Johnson et al. 2011) or acceptance of psychotic experiences (Gaudiano and Herbert 2006). Nevertheless, meditation remains the foundation of mindfulness and yet there is limited research into what aspect of meditation contributes towards mindfulness’ success amongst people with schizophrenia.
Campillo et al. (2018) suggested that meditation activities are typically prompted by a combination of audio (e.g. a single tone) and visual stimuli (e.g. printed mandalas) that are presented simultaneously (Segal et al. 2002). They therefore examined whether audio or visual meditation prompts showed superior effects in terms of mood and cognition. They found that healthy participants who underwent a 30-min audio-led meditation (e.g. tones and nature sounds) showed a significant reduction in negative affect, measured using the Positive and Negative Affect Schedule (PANAS; Watson et al. 1988) whereas participants prompted by visual stimuli (e.g. mandalas and landscapes) showed no such reduction. Despite these between-group effects, both groups showed significant improvements in measures of executive functioning such as a measure of attentional shifting, the Trail Making Test (TMT; Reitan and Wolfson 1993), and a measure of working memory, The Digit Span (DS) subscale of the Wechsler Memory Scale (Wechsler 1997). This suggests that there are modality-dependent effects of a brief meditation on mood and modality-independent effects on executive functioning. No study has yet examined whether these effects are replicable amongst clinical groups for whom problematic negative affect and executive functioning are common, such as amongst people with schizophrenia (Blanchard et al. 1998; Kerns et al. 2008). The present investigation therefore examined the effects of brief audio- and visually led meditations on mood and executive functioning in people with diagnoses of schizophrenia.
It is worth noting also that there is some evidence that mindfulness practice has also been associated with some detrimental effects amongst people with schizophrenia. In particular, meditation has been associated with feelings of depersonalisation or derealisation that can be unwanted or distressing (Cebolla et al. 2017), and this may be particularly so for people with schizophrenia who are already prone to experiencing these symptoms (Sethi and Bhargava 2003; Walsh and Roche 1979; Yorston 2001). However, the evidence for the negative side effects of meditation amongst people with schizophrenia is mixed (Antonova et al. 2016; Shonin et al. 2014). Given these mixed findings, dismantling studies such as the present investigation are necessary not only as a way to find out which aspects of mindfulness-based practice are most effective but also to explore whether some aspects of these practices can be detrimental.
Although this investigation used only a single session of meditation training and brief interventions such as these have been associated with improved negative affect and executive functioning (Campillo et al. 2018), the intention of this investigation is not to suggest that brief interventions are sufficient to exert sustained improvement in clinical populations where long term practice would be necessary (Kral et al. 2018; Lai et al. 2015). Instead, the present investigation aimed to dismantle mindfulness-based interventions to examine which aspects of these interventions are most (or least) effective so that future applications of mindfulness for clinical populations, such as those with diagnoses of schizophrenia, might adapt and improve mindfulness based on these insights. In particular, we examined whether people who underwent a brief audio-led meditation showed improvement in negative affect relative to those who underwent a visual-led meditation. In addition, besides these modality-dependent effects, the present investigation also examined whether there were modality-independent effects of a brief meditation on executive functioning, measured in terms of performance in the TMT and a measure of Digit Span. In order to examine the effects of both interventions on mood and executive functioning, irrespective of their modality, the present investigation also included a passive control group that did not meditate. No change in any dependent variable was expected for participants in the control group. In line with previous research with healthy participants (Campillo et al. 2018), both meditation groups were expected to show an improvement in TMT performance, whereas only participants in the audio group were expected to show a significant improvement in affect.
Method
Participants
Forty-three patients (Mage = 38.1; females = 34.9%) from the mental health unit associated with the second author, diagnosed by their current psychiatrist or psychologist as having schizophrenia in accordance with the Diagnostic and Statistical Manual, 4th Edition, Text Revision (DSM-IV-TR; American Psychiatric Association 2000) criteria (paranoid = 62.5%; undifferentiated = 37.5%), were invited to participate. There were no differences between the groups in terms of their mean age, F(2, 41) = 0.01, P = .992, η2 = .00, or the proportion of females, χ2(2) = 1.189, P = .552. Participants with neurological damage or disability, recent changes in medication or a history of epilepsy or alcohol or substance abuse were excluded. All participants were receiving long-term antipsychotic medication and within this 58.3% of participants were also taking antidepressants. Participants were not receiving any other form of psychological intervention at the time of the study; 12.5% of participants had obtained university-level education.
Measures
Mood
Mood was assessed using the Spanish PANAS (Sandin et al. 1999) where participants rated how true each of ten positive (e.g. inspired) and ten negative (e.g. distressed) mood-related words were of them. The Spanish PANAS has previously shown good psychometric properties in non-clinical populations (Ortuño-Sierra et al. 2015; Robles and Paez 2003; Sandin et al. 1999) and people with schizophrenia (Magallares et al. 2013; Pérez-Garín et al. 2017). In the current study, internal consistency was reasonable (pre-intervention Cronbach’s alpha: positive affect = .67; negative affect = .67) (Taber 2018).
Executive Functioning
The TMT assessed general processing speed (part A; TMTa) and the ability to shift attention (part B; TMTb). In part A, participants drew a line between the numbers 1 to 25 distributed randomly on paper. In part B, participants alternately drew a line between numbers (1–13) and letters (A–L) (e.g. 1-A–2-B etc.). The speed with which participants completed each task was measured and performance in TMTa was subtracted from TMTb in order to quantify participants’ attentional shifting abilities, independent of their psychomotor coordination abilities. The Digit Span test was used to assess working memory. Participants listened to number sequences of increasing length. After each sequence, participants verbalised the numbers in forward or backward order. The total number of correct sequences across both orders was measured.
Intervention
A full description of the intervention is given elsewhere (Campillo et al. 2018). In short, participants were, individually, presented with images or sounds and were told verbally by the experimenter to sustain their attention on each of them as they were presented; if they became distracted by other thoughts, they were to notice what distracted them and then move back to the stimuli non-judgementally. The visual group were presented five images from each of three categories—colours, mandalas and landscapes—and the auditory group were presented with five sounds from each of three similar categories—single-instrument sounds, meditation mantras associated with visual mandalas and landscape sounds (e.g. running water). Each stimulus was presented for 2 min such that the meditation was 30 min in length.
Procedure
Participants completed each measure prior to group randomisation (control n = 13; audio n = 15; visual n = 15) and immediately after the intervention. Control participants sat in a waiting room whilst the intervention groups completed their meditations. The sessions were performed by a clinical psychologist embedded within the clinic in which participants were being treated and who is a certified deliverer and teacher of mindfulness.
Data Analysis
Before analyses, each dependent variable was examined for skewness (≥ 2 to < 2 cut-off) and kurtosis (≥ 7 to <7 cut-off) to examine the extent to which they conformed to the assumptions of normality (West et al. 1995). Each dependent variable fell within the required cut-offs and so no transformation was necessary. Four mixed ANOVA were performed for each of the dependent variables (positive affect, negative affect, TMT and Digit Span). These included a within-subject factor (time) with two levels to measure change from pre- to post-intervention and a between-subject factor (group) with three levels for differences between groups (control, audio, visual). Greenhouse-Geisser-corrected F values are presented. In all analyses, a significant interaction between time and group was expected. Significant main or interacting effects were followed up with pairwise comparisons with estimated marginal means. These pairwise comparisons are first presented with raw p values and, where there is evidence of significant effects, Bonferroni-corrected values are also presented. Cohen’s d values, based on the mean and standard deviations, are also given for these pairwise tests.
Results
See Table 1 for means and Table 2 for a summary of ANOVA statistics. The data are available online at https://osf.io/x5h6w/.
Mood
The ANOVAs for change in positive and negative affect between groups showed a significant interaction for change in positive affect across the intervention between groups. The interaction for negative affect did not reach significance (p = .052). There were no significant main effects of time or group in either ANOVA. Given the trend-level interaction effect for negative affect, pairwise comparisons were performed between groups at pre- and post-test. Prior to Bonferroni correction, the visual group showed significantly lower negative affect at pre-test compared with the control group (estimated mean difference = − 3.49, SE = 1.41, p = .017 (95% CI, − 6.33, − 0.65), d = − 0.59); however, this effect was not significant after Bonferroni correction (p = .258; 95% CI, − 7.88, 0.89). There were no other group differences at either time point prior to correction.
To examine the significant interaction between group and time in the positive affect ANOVA, follow-up pairwise comparisons with estimated marginal means showed that, prior to correction, there were no significant differences between any of the groups at pre-intervention (lowest p = .447, for difference between visual and control group). By post-intervention, the visual group was significantly more positive than the audio group (estimated mean difference = 4.67, SE = 1.23, p < .001 (95% CI, 2.18, 7.15), d = 0.82). The visual group was also significantly more positive than the control group (estimated mean difference = 3.34, SE = 1.95, p = .012 (95% CI, 0.76, 5.92), d = 0.60). There were no significant differences between the audio and control groups (estimated mean difference = 1.32, SE = 1.28, p = .306 (95% CI, − 3.90, 1.26), d = 0.21). After Bonferroni correction, the difference between the visual and audio groups maintained its significance (p = .007; 95% CI, 0.83, 8.51) whereas the difference between the visual and control groups was no longer significant (p = .186; 95% CI, − 0.64, 7.33).
Executive Functioning
Analyses of the TMT difference score showed a significant main effect of time and a significant group by time interaction. At pre-intervention, pairwise comparisons prior to correction showed that the visual group was significantly slower than the control group (estimated mean difference = 15.75, SE = 5.83, p = .010 (95% CI, 3.96, 27.53), d = 0.47) and the audio group (estimated mean difference = 15.69, SE = 5.62, p = .008 (95% CI, 4.33, 27.04), d = 0.49). However, neither of these effects was maintained after Bonferroni correction (lowest p = .151; 95% CI, − 2.45, 33.94), for the difference between visual and audio groups). Prior to correction, there was no significant difference between the audio and control groups (estimated mean difference = 0.06, SE = 5.83, p = .992 (95% CI, − 11.72, 11.84), d = 0.00).
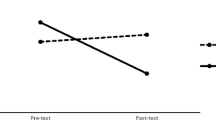
At post-intervention, the audio group were significantly quicker than the control group (estimated mean difference = − 22.81, SE = 5.83, p < .001 (95% CI, − 34.59, − 11.03), d = − 1.04), and this effect maintained its significance after Bonferroni correction (p = .005, 95% CI, − 41.01, − 4.61). Prior to correction, the visual group also differed significantly from the control group (estimated mean difference = − 14.72, SE = 5.83, p = .016 (95% CI, − 26.51, − 2.94), d = − 0.55); however, this effect was not significant after correction (p = .234; 95% CI, − 32.92, 3.48). Prior to correction, the visual group did not differ significantly from the audio group (estimated mean difference = 8.08, SE = 5.62, p = .158 (95% CI, − 3.27, 19.44), d = 0.36). See Fig. 1.
The ANOVA for digit span showed a significant main effect of time, such that participants’ Digit Span improved from pre- to post-intervention, but there was no main effect of group or interaction between time and group.
Discussion
The present investigation examined the possible differential effects of brief audio- and visually led meditations on mood and executive functioning amongst people with schizophrenia. Participants who completed a brief audio-led meditation reported becoming significantly less positive over time whereas participants who underwent a visually led meditation became more positive. Also, participants in both meditation groups showed improvement in their performance, relative to controls, in a measure of attentional shifting, the Trail Making Test. There was no evidence that meditative practice influenced negative affect or working memory.
The findings regarding positive and negative affect contrast partially with findings from elsewhere with healthy participants (Campillo et al. 2018). In this previous investigation, participants in both meditation groups showed a decrease in positive affect and participants in the audio-led meditation group showed a greater decrease in negative affect than participants in the visually led meditation group. In the present investigation, the mixed ANOVA for negative affect did not show any main or interacting effects of group and time, suggesting that none of the groups showed a marked or differential change in negative affect across time. Although the interaction for group and time approached significance, follow-up pairwise comparisons with estimated marginal means suggested that, after correction, there were no significant differences between groups at any time. However, the visually led group showed a significant improvement in positive affect whereas the audio-led group showed a significant decrease in positive affect. Campillo et al. (2018) suggested that audio-led meditations lead to a more rapid improvement in affect than visually led meditations. The findings presented here suggest that amongst participants with schizophrenia, this may not be the case. These detrimental effects in terms of positive mood in the audio-led group appear to be consistent with other studies that suggest that meditative practice may have some undesirable consequences amongst people with schizophrenia (Sethi and Bhargava 2003; Walsh and Roche 1979; Yorston 2001). That no change in negative affect was observed across any of the groups may suggest that negative affect is more resilient to change amongst people with schizophrenia than is the case amongst healthy people. However, these effects must first be replicated in single- and multi-session versions of mindfulness before these conclusions can be confirmed.
The analysis of participants’ responses in the Trail Making Test suggested that participants in both meditation groups improved in their attention shifting abilities from pre-intervention to post-intervention. This finding is in line with those of Campillo et al. (2018) with healthy participants. These findings support the suggestion that brief meditative practice can have beneficial effects on attentional shifting, an important aspect of executive functioning known to be impaired amongst people with schizophrenia (Kerns et al. 2008). This effect also appears to be irrespective of the cues used to lead the meditation.
That TMT, but not Digit Span, performance improved suggests that amongst people with schizophrenia, a brief meditation influences shifting abilities but does not influence working memory. This contrasts with the findings of Campillo et al. (2018). It may be that amongst patients with schizophrenia, for whom working memory problems are particularly pervasive (Forbes et al. 2009), these problems may be less susceptible to change than in healthy participants, especially after only a brief meditation. It is of note that TMT performance improved in both groups, but positive affect only improved in one group. This discrepancy between change in TMT performance and affect replicates the findings of Campillo et al. (2018) and those of others that suggest TMT performance is poorly associated with measures of affect and psychopathology (Smitherman et al. 2007). Although a brief meditation of any modality may lead to improvements in executive functioning, amongst people with schizophrenia it is specifically visually led meditations that can have a beneficial influence on positive affect.
Although there is already evidence that brief meditations can lead to improvement in executive functioning (Tang et al. 2007) and its associated neural structures (Tang et al. 2010), it is currently unclear how much mindfulness training is needed to produce clinically meaningful improvement (Carmody and Baer 2009). Our study suggests that 30 minutes of meditation led by visual stimuli can lead to some enhancement in positive mood and that similarly brief meditations led by visual or audio stimuli may lead to improvements in attention. However, we would caution against interpreting the data presented here as evidence that such brief interventions are likely to lead to sustained improvement in any of these domains. Indeed, even eight sessions of mindfulness may be insufficient to exert long-term change in the neural structures associated with attention and negative affect (Kral et al. 2018). Relatedly, as no significant change in negative affect was observed in the present study, it may be that more meditation sessions are necessary in order to improve mood in this way. Future research could test whether full programmes of mindfulness-based cognitive therapy for schizophrenia which use solely audio- or visually led meditations show comparable effects as those presented here. There is also a need for studies with follow-up assessments such that the duration of the effects reported here can be observed. It would also be interesting to compare these deconstructed interventions with programmes which use combined audio and visual cues to lead meditations.
It is also of note that our investigation does not explore the effects of brief meditation on some core features of psychosis such as the experience of auditory or visual hallucinations and the extent to which these experiences are distressing and disruptive. In a recent investigation, a brief mindfulness intervention (four 1-h sessions) was associated with significant improvement in terms of the disruptiveness of the voices that participants hear (Louise et al. 2019). As in the present investigation, this brief intervention was also associated with a significant improvement in terms of attentional shifting. The authors concluded that this improved ability to shift attention might facilitate disengagement from hallucinations and might help people deal with the negative content of these experiences (Louise et al. 2019). Future larger-scale replications of this investigation might include similar hallucination-related outcome measures.
Several limitations must be noted. First, our investigation included a limited sample size. The design and sample size employed here replicates that of Campillo et al. (2018) and a post hoc power analysis showed that the present investigation had power greater than 80% to detect group differences in TMT performance and positive affect. However, it may be that the limited sample size explains why only a trend-level interaction effect was evident for negative affect and why there were no significant effects in the post hoc pairwise comparisons. It may be that for change in negative affect amongst people with schizophrenia, a smaller effect is expected and so a larger sample is warranted. Furthermore, it should be noted that although our measure of positive and negative affect is well validated in this population (Magallares et al. 2013; Pérez-Garín et al. 2017), in the present study, this measure showed only reasonable internal consistency. Our findings now warrant replication amongst larger clinical groups. Also, our investigation did not quantify differences between individuals or groups in the positive and negative subdimensions of schizophrenia. Although it is possible that our groups differed in this respect, especially given their limited sample sizes, research suggests that these subdimensions of schizophrenia may be unrelated to positive and negative affect (Mohn et al. 2018; Sovani et al. 2005). Participants in the present investigation were all taking medication and were stable at the time of the study, and so it is unlikely that there were substantial differences between participants in their positive and negative symptoms. Similarly, we did not account for within- or between-group differences in depressive symptoms, another common feature of schizophrenia which is more closely associated with positive and negative affect (Gozdzik-Zelazny et al. 2011; Ricarte et al. 2014; Zisook et al. 1999) and which has been found to be influenced by brief mindfulness interventions (Louise et al. 2019). Future investigations should account for these possible differences, perhaps by quantifying depressive symptoms with measures that capture the kinds of depressive symptoms that people with schizophrenia experience such as the Calgary Depression Scale for Schizophrenia (CDSS) (Addington et al. 1993).
Given that all participants were taking antipsychotic medication at the time of the investigation, it is possible that such medication might influence mood and executive functioning. However, as all participants were taking medication it is unlikely to explain any between-group differences that were observed. Also, although the measures of executive functioning employed here provided us with an adequate way to quantify attentional shifting and working memory abilities within a clinical setting, other measures such as the Attention Network Task (Fan et al. 2002) and measures of working memory that involve secondary tasks and which limit experimenter involvement (Unsworth et al. 2005) might prove fruitful in future replications of this investigation. In addition, our control group enabled us to examine to what extent our participants’ mood and attentional shifting ability changed following meditation relative to if they were doing nothing at all, akin to a wait-list control group in treatment research. However, as in the broader treatment literature, an active control comparison is needed in order to allow us to discern whether other factors, such as distraction or engagement in thinking about one’s thoughts, may have influenced the findings in our intervention groups.
Finally, our study used the same stimuli employed by Campillo et al. (2018) in order to examine whether the effects observed in that study with healthy participants replicated in our study with clinical participants. However, an important limitation of both investigations is that the stimuli used in the audio and visual conditions were not first matched for complexity. This is because the stimuli were deconstructed from the audio and visual components of typical meditation stimuli (e.g., the visual and audio stimuli associated with a river). It must be noted that if the stimuli differed in terms of their complexity it is unlikely that we would see similar effects in both intervention groups in terms of their improvement in TMT performance, as stimuli that differ in complexity may have been more or less taxing for participants. Future investigations should nonetheless examine whether the effects observed here are replicable with novel stimuli that are matched for complexity, in order to establish that any group difference in our outcome measures is not a function of the complexity of the stimuli used in the meditations.
In overview, the evidence presented here suggests that a brief meditation can lead to significant improvement in areas of executive functioning amongst people with schizophrenia. Also, meditations which are led by visual stimuli seem to be particularly effective at improving positive affect. Although the findings of this dismantling study are promising, it is unlikely that such a brief intervention is likely to lead to sustained change in people with schizophrenia. As such, future research comparing audio and visual modalities within full mindfulness programmes and with follow-up assessments are warranted.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders, fourth edition, text revision (DSM-IV-TR). American Psychiatric Association.
Blanchard, J. J., Mueser, K. T., & Bellack, A. S. (1998). Anhedonia, positive and negative affect, and social functioning in schizophrenia. Schizophrenia Bulletin, 24(3), 413–424.
Addington, D., Addington, J., & Maticka-Tyndale, E. (1993). Assessing depression in schizophrenia: The Calgary depression scale. The British Journal of Psychiatry, 163, 39–44.
Antonova, E., Amaratunga, K., Wright, B., Ettinger, U., & Kumari, V. (2016). Schizotypy and mindfulness: Magical thinking without suspiciousness characterizes mindfulness meditators. Schizophrenia Research: Cognition, 5, 1–6. https://doi.org/10.1016/j.scog.2016.05.001.
Campillo, E., Ricarte, J. J., Ros, L., Nieto, M., & Latorre, J. M. (2018). Effects of the visual and auditory components of a brief mindfulness intervention on mood state and on visual and auditory attention and memory task performance. Current Psychology, 37(1), 357–365. https://doi.org/10.1007/s12144-016-9519-y.
Carmody, J., & Baer, R. A. (2009). How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology, 65(6), 627–638. https://doi.org/10.1002/jclp.20555.
Cebolla, A., Demarzo, M., Martins, P., Soler, J., & Garcia-Campayo, J. (2017). Unwanted effects: Is there a negative side of meditation? A multicentre survey. PLoS One, 12(9). https://doi.org/10.1371/journal.pone.0183137.
Fan, J., McCandliss, B. D., Sommer, T., Raz, A., & Posner, M. I. (2002). Testing the efficiency and independence of attentional networks. Journal of Cognitive Neuroscience, 14(3), 340–347. https://doi.org/10.1162/089892902317361886.
Forbes, N. F., Carrick, L. A., McIntosh, A. M., & Lawrie, S. M. (2009). Working memory in schizophrenia: A meta-analysis. Psychological Medicine, 39(6), 889–905. https://doi.org/10.1017/S0033291708004558.
Gaudiano, B. A., & Herbert, J. D. (2006). Acute treatment of inpatients with psychotic symptoms using acceptance and commitment therapy: Pilot results. Behaviour Research and Therapy, 44(3), 415–437. https://doi.org/10.1016/j.brat.2005.02.007.
Gozdzik-Zelazny, A., Borecki, L., & Pokorski, M. (2011). Depressive symptoms in schizophrenic patients. European Journal of Medical Research, 16(12), 549–552. https://doi.org/10.1186/2047-783X-16-12-549.
Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–559. https://doi.org/10.1177/1745691611419671.
Johnson, D. P., Penn, D. L., Fredrickson, B. L., Kring, A. M., Meyer, P. S., Catalino, L. I., & Brantley, M. (2011). A pilot study of loving-kindness meditation for the negative symptoms of schizophrenia. Schizophrenia Research, 129(2–3), 137–140. https://doi.org/10.1016/j.schres.2011.02.015.
Kerns, J. G., Nuechterlein, K. H., Braver, T. S., & Barch, D. M. (2008). Executive functioning component mechanisms and schizophrenia. Biological Psychiatry, 64(1), 26–33. https://doi.org/10.1016/j.biopsych.2008.04.027.
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., et al. (2013b). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771. https://doi.org/10.1016/j.cpr.2013.05.005.
Khoury, B., Lecomte, T., Gaudiano, B. A., & Paquin, K. (2013a). Mindfulness interventions for psychosis: A meta-analysis. Schizophrenia Research, 150(1), 176–184. https://doi.org/10.1016/j.schres.2013.07.055.
Kral, T. R. A., Schuyler, B. S., Mumford, J. A., Rosenkranz, M. A., Lutz, A., & Davidson, R. J. (2018). Impact of short- and long-term mindfulness meditation training on amygdala reactivity to emotional stimuli. NeuroImage, 181, 301–313. https://doi.org/10.1016/j.neuroimage.2018.07.013.
Lai, C., MacNeil, B., & Frewen, P. (2015). A comparison of the attentional effects of single-session mindfulness meditation and Fp-HEG neurofeedback in novices. Mindfulness, 6(5), 1012–1020. https://doi.org/10.1007/s12671-014-0347-6.
Louise, S., Fitzpatrick, M., Strauss, C., Rossell, S. L., & Thomas, N. (2018). Mindfulness- and acceptance-based interventions for psychosis: Our current understanding and a meta-analysis. Schizophrenia Research, 192, 57–63. https://doi.org/10.1016/j.schres.2017.05.023.
Louise, S., Rossell, S. L., & Thomas, N. (2019). The acceptability, feasibility and potential outcomes of an individual mindfulness-based intervention for hearing voices. Behavioural and Cognitive Psychotherapy, 47(2), 200–216. https://doi.org/10.1017/S1352465818000425.
Magallares, A., Perez-Garin, D., & Molero, F. (2013). Social stigma and well-being in a sample of schizophrenia patients. Clinical Schizophrenia & Related Psychoses, 10(1), 51–57. https://doi.org/10.3371/csrp.mape.043013.
Mohn, C., Olsson, A. K., & Helldin, L. (2018). Positive and negative affect in schizophrenia spectrum disorders: A forgotten dimension? Psychiatry Research, 267, 148–153. https://doi.org/10.1016/j.psychres.2018.05.060.
Ortuño-Sierra, J., Santarén-Rosell, M., de Albéniz, A. P., & Fonseca-Pedrero, E. (2015). Dimensional structure of the Spanish version of the Positive and Negative Affect Schedule (PANAS) in adolescents and young adults. Psychological Assessment, 27(3), e1–e9. https://doi.org/10.1037/pas0000107.
Pérez-Garín, D., Molero, F., & Bos, A. E. R. (2017). The effect of personal and group discrimination on the subjective well-being of people with mental illness: The role of internalized stigma and collective action intention. Psychology, Health & Medicine, 22(4), 406–414. https://doi.org/10.1080/13548506.2016.1164322.
Reitan, R. M., & Wolfson, D. (1993). The Halstead-Reitan neuropsychological test battery: Theory and clinical interpretation. Tucson: Neuropsychology Press.
Ricarte, J. J., Hernández, J. V., Latorre, J. M., Danion, J. M., & Berna, F. (2014). Rumination and autobiographical memory impairment in patients with schizophrenia. Schizophrenia Research, 160(1–3), 163–168. https://doi.org/10.1016/j.schres.2014.10.027.
Robles, R., & Paez, F. (2003). Estudio sobre la traducción al Español y las propiedades psicométricas de las escalas de Afecto Positivo y Negativo (PANAS). Salud Mental, 26(1), 69–75.
Sandin, B., Chorot, P., Lostao, L., Joiner, T. E., Santed, M. A., & Valiente, R. M. (1999). The PANAS scales of positive and negative affect: Factor analytic validation and cross-cultural convergence. Psicothema, 11(1), 37–51.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York, NY: Guildford Press.
Sethi, S., & Bhargava, S. (2003). Relationship of meditation and psychosis: Case studies. Australian and New Zealand Journal of Psychiatry, 37(3), 382. https://doi.org/10.1046/j.1440-1614.2003.11721.x.
Shonin, E., Van Gordon, W., & Griffiths, M. D. (2014). Do mindfulness-based therapies have a role in the treatment of psychosis? Australian and New Zealand Journal of Psychiatry, 48(2), 124–127. https://doi.org/10.1177/0004867413512688.
Smitherman, T. A., Huerkamp, J. K., Miller, B. I., Houle, T. T., & O’Jile, J. R. (2007). The relation of depression and anxiety to measures of executive functioning in a mixed psychiatric sample. Archives of Clinical Neuropsychology, 22(5), 647–654. https://doi.org/10.1016/j.acn.2007.04.007.
Sovani, A., Thatte, S., & Deshpande, C. G. (2005). Felt affect in good- and poor-outcome schizophrenia. Indian Journal of Psychiatry, 47(1), 27–29. https://doi.org/10.4103/0019-5545.46070.
Taber, K. S. (2018). The use of Cronbach’s alpha when developing and reporting research instruments in science education. Research in Science Education, 48(6), 1273–1296. https://doi.org/10.1007/s11165-016-9602-2.
Tang, Y.-Y., Lu, Q., Geng, X., Stein, E. A., Yang, Y., & Posner, M. I. (2010). Short-term meditation induces white matter changes in the anterior cingulate. Proceedings of the National Academy of Sciences, 107(35), 15649–15652. https://doi.org/10.1073/pnas.1011043107.
Tang, Y.-Y., Ma, Y., Wang, J., Fan, Y., Feng, S., Lu, Q., et al. (2007). Short-term meditation training improves attention and self-regulation. Proceedings of the National Academy of Sciences, 104(43), 17152–17156. https://doi.org/10.1073/pnas.0707678104.
Unsworth, N., Heitz, R. P., Schrock, J. C., & Engle, R. W. (2005). An automated version of the operation span task. Behavior Research Methods, 37(3), 498–505.
Walsh, R., & Roche, L. (1979). Precipitation of acute psychotic episodes by intensive meditation in individuals with a history of schizophrenia. American Journal of Psychiatry, 136(8), 1085–1086. https://doi.org/10.1176/ajp.136.8.1085.
Watson, D., Clark, L. A., & Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. https://doi.org/10.1037/0022-3514.54.6.1063.
Wechsler, D. (1997). Wechsler memory scale-III. Madrid: Pearson.
West, S., Finch, J., & Curran, P. (1995). Structural equation models with nonnormal variables: Problems and remedies. In R. H. Hoyle (Ed.), Structural equation modeling: Concepts, issues, and applications; structural equation modeling: Concepts, issues, and applications.
Wykes, T., Steel, C., Everitt, B., & Tarrier, N. (2008). Cognitive behavior therapy for schizophrenia: Effect sizes, clinical models, and methodological rigor. Schizophrenia Bulletin, 34(3), 523–537. https://doi.org/10.1093/schbul/sbm114.
Yorston, G. A. (2001). Mania precipitated by meditation: A case report and literature review. Mental Health, Religion and Culture, 4(2), 209–213. https://doi.org/10.1080/713685624.
Zisook, S., McAdams, L. A., Kuck, J., Harris, M. J., Bailey, A., Patterson, T. L., et al. (1999). Depressive symptoms in schizophrenia. The American Journal of Psychiatry, 156(11), 1736–1743. https://doi.org/10.1176/ajp.156.11.1736.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barry, T.J., Hernandez-Viadel, J.V. & Ricarte, J.J. An Investigation of Mood and Executive Functioning Effects of Brief Auditory and Visual Mindfulness Meditations in Patients with Schizophrenia. J Cogn Ther 13, 396–407 (2020). https://doi.org/10.1007/s41811-020-00071-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41811-020-00071-w