Abstract
Efficient and accurate computational model for blood flow dynamics (hemodynamics), is essential for determining optimal treatment strategy, diagnosis, and pathology identification of cardiovascular diseases (CVDs). The focus of the present review paper is to discuss on critical aspects of hemodynamics. Various numerical methods for computational hemodynamics are examined—addressing three key modeling choices. First, the relevance of non-Newtonian hemorheological models in varying vascular conditions is presented. Second, an assessment of single-phase versus multiphase modeling’s validity, for different arterial geometries, is presented. Lastly, investigation on the impact of arterial wall elasticity on blood flow patterns is carried out and a discussion on the necessity of fluid–structure interaction (FSI) model is presented. By surveying diverse scenarios of blood flow modeling, presented in recent literature, it is observed that non-Newtonian behavior significantly impacts severely stenosed arteries or those with low diameters and Womersley numbers, while larger arteries exhibit characteristics similar to Newtonian fluids. Differences between single-phase and multiphase modeling vary with arterial configurations, showcasing notable particle migration effects in curved and branched arteries. Additionally, arterial wall elasticity’s influence varies across scenarios—highlighting the importance of FSI, particularly in diseased states. The article identifies crucial areas for future research to enhance CFD-based hemodynamic modeling, emphasizing the integration of multiphase simulation with non-linear elastic arteries, considering surrounding tissue effects in FSI, innovating patient-specific CAD geometries, and developing faster computational techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cardiovascular diseases (CVDs) encompass a range of conditions affecting the heart and blood vessels. They are a leading cause of mortality worldwide, claiming millions of lives annually. According to a recent survey by American Heart Association1, CVDs account for nearly 18 million deaths each year—representing about 31% of all global deaths. Among these fatalities, Coronary Artery Disease (CAD)Footnote 12, stroke, heart failure, and hypertensive heart disease are prevalent contributors. These statistics underscore the critical need for innovative approaches in managing and preventing CVDs.
Computational modeling of blood flow, within the human vasculature has emerged as a pivotal tool in modern medicine. It basically involves a computer program-based solution of governing physics-based mathematical model, to obtain blood flow velocities and pressure at numerous discrete locations and time instants inside human vasculature. This technology offers numerous advantages, which significantly impact the diagnosis, treatment, and understanding of cardiovascular conditions. One key advantage lies in the realm of surgery planning, where computational models can aid in selecting appropriate implants.Footnote 2 The model involves simulation of blood flow patterns and predicting the behavior of various prosthetic devices within the vascular system3. This enables surgeons to personalize treatments, optimizing the choice of implants for individual patients and enhancing surgical outcomes. Moreover, these models play a pivotal role in the development of new diagnostic devices4,5. By simulating blood flow under various conditions, researchers can design and test diagnostic tools that accurately detect anomalies in circulation—enabling earlier and more precise diagnosis of cardiovascular issues. Understanding the possibility of plaque growth is another crucial aspect facilitated by computational modeling. These models simulate the flow of blood, highlighting regions susceptible to plaqueFootnote 3 accumulation6,7. This knowledge allows for better prediction of potential blockages, aiding in preventive measures and targeted treatments to mitigate the risk of arterial blockages and related complications. Furthermore, computational models provide insights into hemodynamicsFootnote 48,9,10,11, elucidating the complex interplay between blood flow and vessel structure. This understanding helps in predicting potential complications post-surgery, optimizing treatment strategies, and advancing our comprehension of cardiovascular physiology12.
Computational fluid dynamics (CFD) for modeling blood flow in human vasculature involves several key steps13. First, in the pre-processing step, geometric reconstruction of the vasculature is done using idealized geometries or from medical imaging data like magnetic resonance imaging (MRI)Footnote 5 or computed tomography (CT) scans.Footnote 6 Thereafter, the geometry is meshed, that involves subdividing the flow domain into small elements for calculations. Boundary conditions like blood pressure and flow rates are set and governing fluid flow equations are solved using numerical methods. Finally, in the post-processing step, the results are analyzed to understand blood flow patterns, pressure distributions, and shear stresses within the vessels. The analysis leads to crucial insights for medical interventions and device design. Before delving further into computational models along with their challenges and current state of art, it is essential to understand human vasculature and complexities which may arise in defining the governing physics-based mathematical model.
The human vasculature system comprises arteries, veins, and capillaries—forming an intricate network responsible for transporting blood throughout the body, as shown in Fig. 1 (Chapter 2—Tu et al.14). Arteries carry oxygenated blood away from the heart, branching into smaller vessels called arterioles. On the other hand, veins return de-oxygenated blood back to the heart, with venules connecting to larger veins. Vessels vary in diameter, from large arteries like the aorta (2 cm) to tiny capillaries (10 \(\upmu\)m)15, and are crucial for nutrient exchange. The Reynolds number Re,Footnote 7 which signifies the flow regime, varies widely within the vasculature, ranging from 20 (arterioles) to 2000 (aorta) due to changes in velocity and diameter. Arteries possess elasticity, allowing them to expand and contract in response to blood flow changes and maintain a steady circulation. Further, blood is a complex fluid, comprising of plasma, red blood cells (RBCs), white blood cells (WBCs), and platelets16; as shown in Fig. 2. Its behavior is challenging to model computationally due to its non-Newtonian nature, exhibiting varying viscosity and flow properties under different conditions. Moreover, accounting for factors like the pulsatile nature of blood flow, vessel compliance,Footnote 8 and the dynamic interaction between blood and vessel walls adds complexity to accurate computational modeling of blood flow in these intricate networks. Achieving precise simulations necessitates sophisticated models that consider these multifaceted characteristics.
Human vasculature system consisting of arteries, veins, and connecting capillaries (adapted from17 and modified suitably).
Composition of human blood (modified from source: Zuzanna K. Filutowska, https://commons.wikimedia.org/w/index.php?curid=29764058).
The above discussion shows that there are multiple physics (involving two-phase composition, flexibility of artery, elasticity of RBCs, and shear-dependent viscosityFootnote 9) which need to be considered for computational solutions. After the rapid development in computer hardware and processing speed during recent decades, CFD modeling for physiological flows (air flow in respiratory system, blood flow in circulatory system) has progressed to a large extent. Summary of literature survey on CFD studies for blood flow modeling in human vasculature is presented in Table 1. The table shows that different authors have worked on different arterial systems with some assuming single phase, rigid walls, and constant viscosity. It becomes important to understand which assumptions can be made for a particular artery under study so as to obtain accurate results with optimal computational cost. In this regard, there are several papers2,6,18,19 which discuss the latest trends in physiological modeling and the realistic computational models. However, as per our knowledge, many of these are restricted to one particular artery type or deal with a single type of modeling variation (example, single and multi-phase, rigid and compliant). In an effort to address this disparity, the present article undertakes a comprehensive examination of blood flow modeling techniques and attempts to offer recommendations regarding assumptions that can be made for relevant flow and geometric parameters.
The present article provides a comprehensive literature review on three crucial choices (during computational modeling of human vasculature)—single-phase versus multi-phase flow, Newtonian versus non-Newtonian hemorheology, and the need for modeling fluid–structure interaction (FSI). First, the review is focused on whether the intricate motion of RBCs within blood vessels requires a multi-phase model or if single-phase modeling suffices to capture the essence of blood rheology and hemodynamic variables. Further, the review explores significance of shear rate-dependent blood viscosity and the role of red blood cell (RBC) elasticity in shaping hemorheologicalFootnote 10 dynamics. Finally, the influence of flow-induced periodic arterial deformation-based vibration on hemodynamics is presented, which leads to further investigation into the most suitable material models for the studied artery network. Through an interconnected exploration of these inquiries, this review seeks to highlight the state of the art while navigating the challenges that underlie computational hemodynamics in human vasculature.
The present article is on reviewing and comparing computational modeling techniques and assumptions for blood flow in human vasculature. Our main focus is on arteries since major abnormalities occur here and veins follow similar modeling techniques with outline as follows: Sect. 2 presents the governing equations for simulating single/two-phase blood flow in flexible artery, along with the coupling between artery vibrations and blood flow parameters. Section 3 presents the variations in blood flow modeling using single and two-phase approach, along with suitable conditions where single-phase approach can yield accurate results. In order to close the stress tensor discussed in mathematical model, Sect. 4 discusses the rheology of blood and different non-Newtonian models of varying complexities, which can be used to model the viscosity of blood and elasticity of RBC particles. Further, Sect. 4.3 presents a comparison of Newtonian and non-Newtonian models for different arteries and flow conditions so as to gage the necessity of such complex models. After discussing blood flow modeling and variations of viscous stress formulation, Sect. 5 attempts to answer the last research question regarding necessity of including fluid–structure interaction (FSI) in the numerical model. In this section, a comparison of rigid modeling and compliant artery modeling (with linear and non-linear material) is provided so that readers can understand suitability of lower end models depending on the case being studied.
2 Mathematical Model
Blood is commonly treated as single fluid with homogeneous distribution of all particles due to similar properties of RBCs and plasma. However, in several cases, this assumption does not remain valid and blood is treated as mixture of mainly plasma and RBC since platelets and WBCs constitute to only 1% of total volume. Considering this into account, mathematical formulation for blood flow, artery deformation, and the resulting fluid–structure interaction are presented in separate subsections below.
2.1 Hemodynamics
The governing compressible Navier–Stokes equation for two-phase mixture of RBC and plasma is given as follows28: Continuity:
Momentum:
Equation of state:
where k = (plasma, RBCs), \(\rho\) is the density, \(\epsilon\) is the volume fraction of each phase (0 \(\le\) \(\epsilon _k\) \(\le\) 1), T is the temperature, \(\phi _\mathrm{mix}\) is the mixture property, and \(\overrightarrow{u}\) is the velocity. Further, p is the pressure common to both phases, \(\overline{\overline{\tau }}\) is the viscous stress tensor,Footnote 11\(\overrightarrow{g}\) is the gravity force, n is total number of phases (two here), and \(\overrightarrow{F}\) is the shear lift force; found using Saffman-mei inertial lift force model29. Further, \(\beta _{lm}\) is the interphase momentum exchange coefficientFootnote 12 with l and m being the indices of plasma and RBCs, respectively (since there are only two phases involved here). It should be noted that the volume fractions of all phases must sum to unity i.e., \(\epsilon _\mathrm{plasma} + \epsilon _\mathrm{RBC} = 1\). For each phase k, the stress tensor \(\overline{\overline{\tau }}\) is given as:
where \(\mu _k\) and \(z_k\) are the shear and bulk viscosity of each phase, respectively. The bulk viscosity \(z_k\) is usually treated as zero. Shear viscosity is considered constant for a Newtonian fluid assumption whereas it is modeled as function of hematocrit (RBC concentration) and shear rate for non-Newtonian flow. Discussion on rheology of blood is presented separately in Sect. 4. Further, the interface momentum exchange coefficient \(\beta _{lm}\) can be determined as follows:
where \(d_\mathrm{RBC}\) \(\approx\) 8 mm (RBC diameter), and \(\phi\) \(\approx\) 1 (shape factor). The drag coefficient \(C_d\) is given by:
where
Thus, using the above constitutive relations (Eqs. 4, 5, 6), the mass and momentum conservation equations (Eqs. 1, 2) can be obtained in a closed form.
It should noted that these equations can be further simplified by using single phase approximation and incompressibility.Footnote 13 In this approach, the whole blood is considered to be a single fluid with constant density and constant/spatio-temporally varying viscosity. Thus, for single fluid model, the generalized governing equations presented above can be simplified by setting \(\epsilon _1\) = 1 and \(\epsilon _i\) = 0 (\(i \ne 1\)). Further, the interface momentum exchange can also be ignored. The new set of governing equations for incompressible blood flow are given as follows:
where \(\overline{\overline{\tau }}\) is modeled using Eq. (4) with k = blood. This approach of blood flow modeling has been used over a long time and is validated with in vivo experiments and MRI measurements22,30. The single fluid modeling works, especially in case of large arteries with high Re flows due to the fact that RBCs are very small in size (8 \(\mu\)m) as compared to artery diameter (2 mm–2 cm) and move freely with plasma, without actually imparting any effect on plasma. If objective of the study is to understand blood flow patterns and trend of hemodynamic parameters (so as to see which areas are more prone to damage), the single fluid approach is more suitable as it takes less computational time. A comparison of multiphase and single fluid models are presented elaborately in Sect. 3.
2.2 Artery Deformation-Based Structural Dynamics
Arteries in human vasculature are found to be flexible in nature and act as capacitor which store blood during systolic phase by expanding and release it during diastolic phase by contracting. This helps in reduction of high temporal variation of blood pressure. Thus, it becomes important to model arterial deformations in order to obtain hemodynamic variables accurately. For a general compressible solid, the Lagrangian framework-basedFootnote 14 governing momentum equations is given as:
where \(\rho _s\) is the density, \(\overrightarrow{d}\) is the displacement vector, \(\overline{\overline{\tau }}_s\) is the Cauchy stress tensor, and \(\overrightarrow{f}_s^B\) is the body force vector for solid element s. There are two types of non-linearity while modeling structural deformation. First is a relation between stress tensor \(\overline{\overline{\tau }}_s\) and strain \(\epsilon _s\), which is decided by choice of linear or non-linear material modeling. Second is the choice of relation between strain \(\epsilon _s\) and displacement gradients which lead to geometric linear or non-linear model. Generally, material non-linearity is decided by the response of material to applied load, i.e., the resulting stress–strain graph while geometric non-linearity is considered when structural displacements are larger (> 10% of length scale). For compliant artery and veins-based circulatory system, a detailed discussion on need for structural modeling along with suitable material modeling schemes are presented in Sect. 5.
2.3 Fluid–Structure Interface Coupling
Once arterial deformations are modeled along with blood flow, it becomes utmost important to consider the effect of arterial deformation on the flow and flow-induced load on the artery. Thus, there is a two-way coupling between fluid and structural dynamics that needs to be ensured through suitable interface coupling given as follows:
-
1.
Continuity of velocity At the fluid–solid interface if, velocity of the fluid flow \(\overrightarrow{u}_{f,if}\) is equal to the structural velocity \(\overrightarrow{u}_{s,if}\) given as
$$\begin{aligned} \overrightarrow{u}_{f,if} = \overrightarrow{u}_{s,if} \end{aligned}$$(9)where the subscript f and s represent fluid and solid respectively.
-
2.
Force balance For the bodies to be in equilibrium, a balance between hydrodynamic and elastic forces is ensured normal to the interface given as
$$\begin{aligned} {[}\overline{\overline{\tau }}_{s,if}] \cdot \hat{{n}}_{s,if} + [\overline{\overline{\tau }}_{f,if}] \cdot \hat{{n}}_{f,if} = 0 \end{aligned}$$(10)where at the interface, \(\hat{{n}}^s_{if}\) and \(\hat{{n}}^f_{if}\) represent outward normal unit vector at the solid and fluid subdomains, respectively.
Commonly, the above interfacial boundary conditions are implemented with fluid-dynamic pressure and viscous stress for obtaining structural displacements, which in turn is used to enforce the continuity of the fluid velocity at the interface31.
3 Computational Hemodynamics: Whether Multiphase Model is Required?
As discussed in the introduction (Sect. 1), blood consists of particles (RBCs, WBCs, and platelets) that are suspended in liquid plasma. Since plasma constitutes more than 50% volume fraction and RBCs around 45%, blood can be modeled using the Eulerian-Eulerian two-phase model; described in Jung et al.28. The corresponding governing equations are already presented in Sect. 2 (Eqs. 1, 2). However, RBCs can be considered to have similar properties of plasma and a single fluid approach may also be used, especially when shear rate and diameter are higher (governing equations presented in Sect. 2). Thus, it becomes important to understand the right choice of computational approach for the artery being studied and also desired application for which simulations are being carried out. In order to address this issue, a literature survey of single-fluid and multiphase (mostly RBC–plasma mixture) models along with a discussion on suitability of single versus multi-phase modeling, are presented below.
Although single-fluid models have advantages, the movement of particles (specifically RBCs) within the blood cannot be understood using such models—discussed in Sect. 2. It is known that atherosclerosisFootnote 15 initiates in humans with monocytes adhering to the endothelium,Footnote 16 yet despite decades of research7, the exact trigger for this response remains unknown. It tends to localize near arterial side branches and the inner curvature, where hemodynamic stresses significantly influence the early stages of CVDs. Predicting particle accumulation could be an initial step toward comprehending atherogenesis,Footnote 17 aligning with clinical observations. Thus, in order to understand the pathogenesis (process by which a disease or disorder develops) behind atherosclerosis and to correlate it with hemodynamic parameters, it becomes essential to understand the concentration difference in particles and/or to see where the particles are staying for long time. A multiphase simulation is required to achieve the above objective. Gidaspow32 provides a comprehensive description of multiphase flow, highlighting the primary distinction from a single-phase model—the inclusion of volume fraction for each phase and mechanisms facilitating the exchange of mass, momentum, and energy between these phases. A brief review of multiphase modeling for blood-flow simulations and observations reported are presented below.
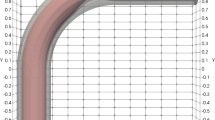
Jung et al.28 presented a multiphase transient non-Newtonian three-dimensional CFD model, for pulsatile flow in a curved coronary artery. Their model (similar to Eqs. 1–6) was formulated using the concepts developed during 30 years of biomedical CFD modeling and 20 years of multiphase research, especially in Eulerian–Eulerian phase modeling. Their simulations showed that RBC volume fractions were highest on the inside curvature, and secondary flows weakened during diastole—increasing RBC buildup. They reported that particulate buildup on inside curvature correlates with lower wall shear stress. Further, two-phase non-Newtonian viscosity model also predicted a greater shear thinning as compared to single-fluid model. These predictions provide insight into how blood-borne particulates interact with artery walls and hence, multiphase models have relevance for understanding atherogenesis since clinical observations show that atherosclerotic plaques generally form on the inside curvatures of arteries. On a similar line, Kim et al.33 investigated the influence of mechanical factors on the hemodynamics of a curved coronary artery—using multiphase non-Newtonian fluid simulations of pulsatile flow. It was reported that the high hematocrit levels induce secondary flow, and RBC viscosity as well as Wall Shear StressFootnote 18 (WSS) vary with hematocrit level. It was argued by the authors that although all models have a good approximation in blood-flow behavior, the multiphase non-Newtonian viscosity model is optimal—to demonstrate effects of changes in hematocrit and provides a better simulation of realistic blood flow analysis. Huang et al.34 discussed the use of a multiphase kinetic theory model to simulate pulsatile flow in a coronary artery. They showed that the multiphase kinetic theory model accurately computes viscosity and migration of red blood cells. WSS and its gradients were highest on inside area of maximum curvature. Thus, the multiphase kinetic theory model has been shown to compute correctly the viscosity of RBCs and their migration away from vessel walls: the Fahraeus–Lindqvist effect35.
While multi-phase blood flow simulations offer detailed analysis, our survey reveals minimal differences in WSS compared to single-phase models, especially for large arteries (\(\ge\) 2 mm). This suggests that, for these vessels, prominent hemodynamic parameters can be calculated accurately using single-phase models, while accurate physical description of hemodynamic characteristics necessitates multiphase/multi-component modeling. However, multiphase may be necessary to dynamically model the growth of stenosis since plaque growth is caused by WSS variation, which in turn varies with plaque build-up level. For example, Jung et al.36 used multiphase modeling to analyze hemodynamics in a non-uniform right coronary artery. They computed RBC build-up and WSS variation along its length. Interestingly, despite non-uniform geometry, regions with high curvature showed both increased RBC build-up and WSS. This suggests factors like flow reversal and secondary flow might also play a role in RBC distribution. Such simulations are complex to model37,38,39 and require larger computational cost and are currently under development.
The above discussed multiphase models consider two different mass and momentum conservation equations, which need to be solved simultaneously. They also involve several constitutive relations for shear lift force, interface momentum exchange—making the computations complex and time-consuming. A relatively simpler approach involves using a single phase approach, with fluid as plasma, and modeling RBC (Hematocrit) concentration using Philips diffusive flux model40—a scalar transport equation. Thus, one needs to solve single set of mass and momentum equations along with an equation for hematocrit given as
where \(\phi\) is the volume fraction of RBCs. Further, \(N_c\), \(N_{\mu }\), and \(N_g\) are the contributions to the diffusive flux from particle collisions, spatial variation of viscosity, and gravitational force, respectively. These terms can be expanded in terms of geometric and flow parameters as:
where a is the radius of RBC (assumed sphere), \(K_c\) \(\approx\) 0.43, and \(K_{\mu }\) \(\approx\) 0.62 are empirically determined coefficients. Further, \(\rho _{f0}\) and \(\rho _{s0}\) are the density of plasma and RBC, respectively.
Using the above model, Wu et al.26 presented numerical simulation of blood flow in a sudden expansion channel and a curved coronary artery, focusing on the movement of red blood cells and the formation of atherosclerotic plaque. First, they showed that velocity profiles in sudden expansion flow agree with experiments. For the idealized curved coronary artery, they found that the RBCs move toward and concentrate near the inner surface, where the viscosity is higher and the shear stress lower similar to the phenomenon observed using Eulerian–Eulerian multiphase model. Thus, for micro-level arterial network, the diffusive flux model can be successfully applied. A similar model was used by Yadav et al.41 to simulate blood flow even at mesoscaleFootnote 19 (10–300 \(\upmu\)m). Through comparison with experiments, it was shown that such models could accurately predict flow patterns for smaller capillary vessels. Although the above works are mostly for coronary artery and microchannels, several other studies have performed multiphase simulations in carotid42,43 and femoral44,45 arteries also.
Based on literature survey for single and multiphase blood-flow modeling, it can be observed that hemodynamic parameters like WSS, Oscillatory Shear Index (OSI),Footnote 20 and wall shear stress gradient (WSSG) can be accurately calculated using single fluid model, especially for larger arteries like carotid, femoral, and aorta. However, the particle motion cannot be tracked accurately (even using Lagrangian tracking through single fluid results) and there may be errors \(\ge\) 5% for small arteries and veins. Thus, a judicious choice is needed to decide whether single fluid model is sufficient or multiphase (computationally more expensive) is necessary-based on the application of the study.
4 Role of Rheology of Blood and its Constituents on Computational Hemodynamics
Apart from the multiphase versus single phase modeling discussed in the above section, determination of appropriate model for viscous stress tensor \(\overline{\overline{\tau }}\) is equally important. As discussed in Sect. 1, the blood consists of various small particles like RBC, WBC, and platelets-suspended in liquid plasma. The interaction between RBCs and plasma leads to major changes in the effective viscosity of the blood flowing in artery of diameter D. At very small shear rateFootnote 21\(\dot{\gamma }\), RBCs aggregate with each other forming cylinder-like structures—called as rouleaux, which resist the blood flow and lead to increased viscosity. As the \(\dot{\gamma }\) increases, these stacked-up RBCs slowly disaggregate, which allows the blood to move freely; thus resulting in reduction in viscosity. With increasing \(\dot{\gamma }\), after a critical shear rate \(\dot{\gamma }_c\), the RBCs completely disaggregate into single structures, align with the flow and make the blood to have constant viscosity \(\mu _{\infty }\). Thus, it can be concluded that blood is a shear-thinning fluid.Footnote 22 This is verified by an experiment performed by Chien46 where normal RBCs suspended in plasma (NRP), and normal and hardened RBCs suspended in 11% albumin-Ringer (NRaR, HRaR) solution are subjected to varying shear rate inside a tube, and corresponding viscosity is measured using rheometer. Figure 3a shows the variation of viscosity with shear rate for these three different type of solutions. It can be observed that the NRPs, which indicate actual blood have a shear thinning property i.e, the viscosity is found to decrease with shear rate and attain a constant value after \(\dot{\gamma }\) = 100 s\(^{-1}\). For hardened and/or albumin-Ringer solution suspended RBCs, the aggregation is not possible and hence a constant viscosity is observed.
Apart from shear rate, viscosity is also affected by the hematocrit (RBC concentration) and the diameter of artery. The hematocrit increases the viscosity while the diameter change has a non-linear effect. At very small diameters (d < \(d_1\)), the viscosity increases exponentially with reduction in diameter. This is because the diameter of artery becomes close to RBC diameter and hence a very high resistance for fluid flow is observed. At d > \(d_1\), with increasing diameter, the viscosity increases due to reduction of cell-free region—formed due to shear-induced migration.Footnote 23 For smaller diameter arteries (\(d_1\) \(\le\) d \(\le\) \(d_2\)), the RBCs radially migrate toward the center of the artery and lead to a cell-free zone near wall, thus causing decrease in viscosity. When the diameter increases beyond micro-scale, this effect is not observed and hence viscosity reaches to a constant level with increased value. This is schematically shown in Fig. 3b where the zones of shear-induced migration are demarcated through values of \(d_1\) and \(d_2\).
Other than the artery diameter, hematocrit, and shear rate, viscosity is also affected by physiological pulsatile flow behavior, health and complacency of artery, temperature of blood; however, these effects are much smaller. The various non-Newtonian models and their formulation are presented below. The elastic behavior of RBCs also lead to change in viscosity and is discussed separately. Finally, a CFD literature-based discussion on efficacy of various models is presented.
Variation of blood viscosity with a shear rate \(\dot{\gamma }\) for three different types of plasma, and b vessel diameter for three different hematocrit levels \(\phi\) of normal RBCs suspended in plasma (NRP) (obtained from data presented in Chien46).
4.1 Non-Newtonian Models
Assuming the blood to be a continuum,Footnote 24 the Newtonian model employs a constant/hematocrit level-based viscosity in the momentum conservation equation for hemodynamics (Eq. 2). In case of non-Newtonian models, the viscosity is a function of shear rate and/or hematocrit. The simplest non-Newtonian formulation is power law model, where an exponential curve is fit to the experimental data of viscosity variation with respect to (w.r.t.) shear rate \(\dot{\gamma }\) given as
where \(\mu _0\) = 0.035 Pa s\(^n\) and n = 0.647. A major disadvantage with this model is its inability to accurately predict viscosity at low and high shear rate. The model predicts unbounded viscosity at zero shear rate and zero viscosity when \(\dot{\gamma }\) \(\rightarrow\) \(\infty\), which is unrealistic. Hence, several other non-Newtonian models were formulated using the \(\dot{\gamma }\) and hematocrit \(\phi\), and the most commonly used models are summarized in Table 2. It can be observed that all the models use shear rate \(\dot{\gamma }\) as input parameter in the definition while the Quemada model includes the RBC concentration \(\phi\) along with shear rate. Apart from these shear-thinning models for viscosity, the thixotropic nature (time-dependent viscosity) of blood are modeled by several works48,49,50 but a generalized power law (where the constant \(\mu _0\) depends on shear rate) is commonly used given as
where the parameters \(\mu _0\), \(n_1\), and \(n_2\) are given in Braun and Rosen49. Each of these models is evaluated against the Newtonian model-based CFD simulations in different arterial networks along with experiments, and the observations are presented in Sect. 4.3—to understand the significance/non-significance of non-Newtonian modeling.
4.2 Viscoelastic Behavior of Blood Constituents
In many situations, blood behaves as a viscoelastic fluid, i.e., it exhibits both viscous and elastic behavior. This unique property is crucial for its efficient flow through the intricate vascular network, and its ability to adapt to various physiological conditions. As it is generally understood and discussed in the above section, viscosity is related to the resistance of a fluid to relative velocity between the adjacent layers of the flowing fluid. In blood, viscosity arises primarily from the presence of plasma, a protein-rich fluid that surrounds the red blood cells. Plasma’s viscosity contributes to the overall resistance to blood flow, particularly in narrow capillaries. Elasticity, on the other hand, describes a material’s ability to store and release energy upon deformation. In blood, RBCs play the primary role in imparting elasticity. These cells, being flexible and deformable, can temporarily change shape to navigate through narrow capillaries (when shear rate is low) and return to their original shape as they exit. This elastic behavior allows blood to flow smoothly through small vessels without significant energy loss. The viscoelastic nature was first discussed in the works of Thurston et al.55. Later, for simulating viscoelastic blood, several other works were performed56,57 to come up with suitable mathematical model.
Although viscoelastic nature of blood leads to modeling complexity, it is particularly important in several physiological situations; like discussed here for four such situations. First, for microcirculation in tiny capillaries (where red blood cells are tightly packed), blood elasticity enables them to deform and squeeze through these narrow passages, ensuring efficient delivery of oxygen and nutrients to tissues. Second, for hemodynamics, the elastic recoil of RBCs contributes to the pulsatile flow of blood—helping to maintain blood pressure and facilitate blood movement. Third, blood filtration in the kidneys, where elasticity of RBCs allows them to pass through the glomerular filtration barrier while retaining larger molecules like proteins; and fourth, blood coagulation during blood clot formation, where the elasticity of RBCs helps to concentrate clotting factors and promote clot formation at the site of injury.
After introduction of the viscoelasticity concept for blood by Thurston55, Oldroyd56 gave an empirical model to evaluate stress tensor—by fitting the experimental curves with proposed model. This model effectively represents how blood’s viscosity decreases with increasing shear rates—known as shear-thinning behavior—along with the elasticity of blood particles. However, it fell short as it did not account for variation of relaxation timesFootnote 25 with shear rates that contradicted the experimental findings. The model devised by Anand and Rajagopal57, within the general thermodynamic framework outlined in Rajagopal and Srinivasa58, incorporates variation of relaxation times with the shear rate. This formulation yields favorable conformity with empirical observations in both steady Poisuelle and oscillatory flow scenarios. In general, the deviatoric stress tensor \(\overline{\overline{\tau }}\) (Eq. 2) can be modeled as a combination of viscous (\(\overline{\overline{\tau }}_s\)) and elastic (\(\overline{\overline{\tau }}_e\)) stress, i.e., \(\overline{\overline{\tau }}\) = \(\overline{\overline{\tau }}_s\) + \(\overline{\overline{\tau }}_e\), where
and \(\overline{\overline{\tau }}_e\) satisfies Oldroyd-B type constitutive equation, given as
where \(\overline{\overline{D}}\) and \(\overline{\overline{W}}\) are symmetric and anti-symmetric part of velocity gradients, \(\mu _e\) is the elastic viscosity co-efficient, and \(\lambda _1\) is the relaxation time (\(\approx\) 0.06s). The above equation is solved along with standard mass and momentum conservation laws to obtain the complete viscoelastic response of blood. Many authors have performed such investigations, but mostly in a single phase setting. Apart from the above presented visco-elastic models, the most accurate method would be to actually introduce RBCs in blood and model their deformation dynamics numerically. RBCs continuously change the shape depending on shear rates in the stream and can be simulated using the models presented in Hoque et al.59,60 and Fedosov et al.61 etc., especially for micro-vessels. However, it should be noted that these simulations encounter a large variation in the scale (\(\mu\)m to cm) and can be difficult to model computationally—due to high computational cost and stability issues. In order to access whether such involved modeling is necessary or not, a brief survey of literature for such comparisons and major observations presented are discussed below.
Bodner et al.62 performed a comparative CFD study between Newtonian, simplified non-Newtonian (without elastic stress), and generalized Oldroyd-B model, by performing blood flow simulations in axisymmetric stenosed artery and patient-specific carotid bifurcation. It was reported that blood flow in medium-sized blood vessels exhibits shear-thinning and viscoelastic behavior, and these non-Newtonian effects were influenced by low flow rate. This was proved by comparing normalized difference between the solutions of Newtonian and generalized Oldroyd-B model, as shown in Fig. 4. A similar study63 discussed the effects of shear-thinning and viscoelastic properties on blood flow in abdominal aortic aneurysms, under different flow rates. Their results showed that the blood shear-thinning behavior and viscoelasticity cannot be neglected especially for low shear rates conditions. Further, Chen et al.64 studied the effects of hematocrit, plasma concentration, and frequency of sinusoidal oscillatory shear flow on the viscoelasticity of human blood. They also demonstrated that the viscous and elastic component increased exponentially at higher hematocrit levels; and exponential decrease in viscous and elastic components of blood with increased frequency of shear flow. Thus, from the above studies, it can be concluded that the viscoelastic non-Newtonian modeling is necessary for blood flow in (a) low/medium size vessels (d \(\le\) 2 mm), (b) low flow rate condition, and (c) low Womersley (Wo) number.Footnote 26
For steady flow in axisymmetrically stenosed artery, contour map of normalized difference between the solutions of generalized Oldroyd-B and Newtonian models with flow rate a Q = 0.5 cm\(^3\)/s, b Q = 1 cm\(^3\)/s, and c Q = 2 cm\(^3\)/s (Figure adapted from Bodnar et al.62 with permission from Elsevier).
4.3 CFD-Based Comparison of Viscosity Models
The above sub-sections presented various non-Newtonian models for hemodynamic analysis. Since implementation of these schemes comes with increased modeling complexity and computational cost, it is important to understand whether they are necessary for artery and flow conditions under consideration. Thus, a CFD-based comparison of such models with Newtonian counterpart is presented here. Neofytou65 performed two-dimensional CFD simulation on an indented (constricted) channel with moving top wall (where indentation is present). The wall moved with two different time-periods (Strouhal numberFootnote 27St): 0.05 and 0.368, and four different viscosity models were used: (a) Newtonian, (b) power law, (c) Casson, and (d) Quemada. For a constant inlet velocity, the author observed that non-Newtonian effects are more clearly visible for St = 0.05. Also, the maximum and minimum WSS values are underpredicted with Newtonian and power law viscosity model, whereas Casson and Quemada models give similar values of WSS for both values of St. Thus, for flexible walls with lower elasticity, the author concluded that it is important to consider a good non-Newtonian viscosity model to predict the hemodynamics accurately.
Apart from the two-dimensional model, for rigid model of CCA, Razavi et al.66 performed axisymmetricFootnote 28 CFD simulations with four different stenosis levels and seven different viscosity models: Newtonian, power law, generalized power law, Casson, Carreau, Carreau–Yasuda, and Walburn–Schneck models. A pulsatile flow based on physiological conditions was used at the inlet of artery. Along with hemodynamic parameters, they defined a parameter, termed as global non-Newtonian Importance Factor (NNIF), and was calculated at different time instants of cardiac cycle. They observed a deviation from Newtonian behavior during lower velocity, i.e., during diastolic phase.Footnote 29 Further, they observed that the non-Newtonian behavior is over-estimated by the power law model while under-estimation by generalized power law and Casson models. The Carreau and Carreau–Yasuda model gave moderate NNIF values during lower shear rates only, and hence were suggested to be better models. For hemodynamic parameters WSS and OSI, they found almost same results from all the models except power law and Casson model; indicating Newtonian behavior of blood at most of the time instants.
In order to understand whether non-Newtonian model is really necessary for large arteries, Arzani67 performed a CFD investigation on patient-specific carotid-artery aneurysm using Newtonian, Carreau–Yasuda and a novel hybrid viscosity model. The novel model was developed, using Lagrangian tracking-based Residence Time (RT) of RBCs in aneurysm sacs. The author argued that apart from lower shear rate (<50 s\(^{-1}\)), the amount of time spent by RBCs in recirculation zone also matters since rouleaux formation and RBC aggregation takes around 5–10 s. The main motivation behind author’s argument was the observation made in rheology experiments, where shear-thinning behavior was observed after some time—when shear rate went below threshold. This was attributed to the reason that some time is required for RBC to aggregate and increase the effective viscosity. Hence, if the RT > RT\(_{th}\) (either 5 or 10 s), the non-Newtonian model is activated. The results obtained for pulsatile blood flow in aneurysm sac indicate that the non-Newtonian behavior is rarely achieved for large arteries (like carotid). Further, the hemodynamic indicators like WSS, time-averaged WSS (TAWSS), and OSI remain almost same, between the Newtonian and proposed hybrid non-Newtonian model, since the RT remains below 5 s for most of the locations during pulsatile cardiac cycle.
Most of the studies on viscosity models involved CFD (discussed above), while the in vitro measurements were missing. Recently, for effect on different viscosity models on the hemodynamics of patient-specific left anterior descending (LAD) coronary, Abbasian et al.68 performed a systematic investigation using CFD, and compared their results with 4D MRI. The arterial mid-point flow velocity, obtained using 16 different viscosity models, for three atherosclerotic patient arteries were compared with clinical measurements using 4D MRI. They observed that Newtonian model provides accurate results in the proximal region of atherosclerosis while the Casson, Carreau–Yasuda, and Quemada model compare better, with the clinically measured velocities, in the distal region. Further, the time-averaged hemodynamic parameter, calculated using Newtonian model, compared well with those calculated using Casson, Carreau–Yasuda, and Quemada model, whereas the instantaneous hemodynamic parameters like WSS, OSI varied significantly for Newtonian model. Thus, the clinical measurements were used as benchmark to understand which viscosity model is best suitable for performing CFD study in coronary arteries—most susceptible to plaque deposition.
For understanding the limitations of non-Newtonian models and their deviations from Newtonian counterparts, Karimi et al.69 performed a CFD study on patient-specific geometry of aortic arch, obtained using CT scan, for nine different viscosity models for blood. The artery is modeled as rigid and an idealized transient inflow velocity, with zero-gage pressure at outlets, is specified. The NNIF is obtained by measuring the difference between WSS of various non-Newtonian models with a Newtonian model (constant viscosity \(\mu\) = 0.0035 Pas). It is observed that the cross model has largest deviation from Newtonian model while the other viscosity models yield closer results with Newtonian models. It is suggested by the authors that since these models are developed by a curve fitting procedure on experimental data obtained from steady flow cases, it is better to avoid cross type-of-models where deviations are high. Instead, the Carreau and generalized power law, which consider Newtonian viscosity at high shear rates, are more realistic, especially in large arteries where the flow is Newtonian in most of the flow domain.
Finally, Yilmaz et al.70 provided a review of various rheological models, proposed for modeling blood in human vasculature. The authors discuss about the composition of blood; and critically review the commonly used (in CFD) viscosity models (Newtonian and non-Newtonian), thixotropic properties, and elastic models (Olroyd-B, yield stress formulation). They highlight main issues and future scope, including (1) dependence of critical shear rate for dis-aggregation of RBC on the hematocrit level, (2) dependence of viscosity on pulsatile flow period and setup, (3) inability to measure threshold time for occurrence of aggregation so that non-Newtonian behavior is predicted accurately, and (4) measurement of thixotropic properties of blood. A summary of all the above discussed literature is presented in Table 3. The table shows that, for large arteries (carotid, aorta) involving transient flow, the non-Newtonian behavior is diminished while the blood-flow strongly deviates from constant viscosity for small arteries (d < 2 mm). Further, Quemada and Carreau–Yasuda model are found to be best suited for non-Newtonian modeling while power law and its derived models are found to have abnormal deviation in hemodynamics.
5 Role of Fluid–Structure Interaction in Computational Hemodynamics for Complaint Vasculature
Computational fluid–structure interaction (CFSI) is a multi-physics problem which involves deformation of solid due to fluid forcing and simultaneous change in region of fluid flow due to solid movement. Blood moves out of aorta with a high pressure since it has to be transported to other regions of body while it comes back from capillary and veins with lower pressure. During the systolic phase (high flow rate), high blood pressure experiencing artery expands and later contracts elastically to serve two purposes: (a) lower the sudden impact of high pressure load on the artery wall and (b) store some amount of blood (by expanding) so that during diastolic phase (very low flow rate), this additional blood may be supplied to organs by gradual contraction so as to avoid oxygen deprivation in the organs. Thus, it can be observed that FSI modeling in elastic arteries becomes essential to capture the hemodynamics accurately. From the prediction of aneurysm rupture to calculation of correct blood flow rate in aortic dissection, elastic wall modeling has been observed to yield more accurate outcomes (in comparison with in vivo measurements) discussed in the next subsections.
CFSI involves coupled solutions to Navier–Stokes equations (through computational fluid dynamics—CFD) and structural momentum conservation laws (through computational structure dynamics—CSD). As discussed in a recent review article on CFSI methodologies and applications by Morab and Sharma71, there have been numerous works72,73,74 in the area of development of CFSI algorithms and solvers. All these numerical works are classified based on the way coupling between fluid and solid is achieved, and also on the way in which the grid is generated and gets deformed. FSI can be modeled using a monolithic or partitioned approaches. The monolithic approach involves formulating a single equation for fluid and structure75; however, these methods are limited to linear deformation problems and need to be modified or changed completely for different problems, whereas the partitioned approach involves separate equations that lead to a coupled solution of the existing fluid and solid solvers discussed by Hughes et al.76 and Trepanier et al.77, using the finite element (FE) and finite volume (FV) discretization methods, respectively. Further, a classification based on the type of mesh generated to solve fluid solid interactions leads us to body conforming and non-conforming type mesh (Fig. 5). In case of body conforming type system78, the interface between fluid and solid is considered to be a physical boundary. In most of the cases, fluid particles are tracked through Eulerian approach whereas solid movement is tracked via Lagrangian formulation, and the mesh is regenerated and/or deformed as per solid deformation. In case of non-conforming mesh methods79,80, the interface conditions are not treated as physical boundary conditions for fluid and solid domain. They are treated in governing equations itself so as to give the same effect of boundary conditions (no slip and specified traction). The major advantage with these methods is that, though fluid and solid are discretized quite differently, a static initial mesh is used for an FSI problem; thus, re-meshing is not needed that reduces the computational cost. Efficient mathematical formulation of governing equation for accurate interface conditions needs to be considered.
Illustration of various meshing techniques employed in CFSI problems (Adapted from Xu and Yang81 with permission from Elsevier).
From the above discussion, it can be noticed that there are many techniques, which have different time complexities,Footnote 30 to model interaction of blood flowing through lumenFootnote 31 with elastic artery wall. It becomes important to first understand whether modeling vessel wall deformation is really necessary or not, and second, choose the optimum method so that accurate results with minimum computational time are obtained. Thus, a detailed literature survey for different computational techniques and their outcomes is presented in a separate subsection below.
5.1 Studies on Computational Hemodynamics with FSI
Hirschhorn et al.82 provided a comprehensive review of various FSI works performed for Cardiovascular flows. They presented various methodologies to model the multi-physics problem of arterial deformation and blood flow. They reported that the immersed boundary method (IBM), which can handle large deformation, is gaining popularity with improvement in computational power. Further, a review of FSI models applied to understand blood-flow in vascular aneurysms, cardiac valves, prosthetic valves, atherosclerosis regions, and stented artery was detailed along with relevant literature between 2017 to 2019.
Blood flow in compliant/flexible aortic dissection was numerically modeled using two-phase (RBC suspended in plasma) non-Newtonian model (Carreau–Yasuda) by Qiao et al.24. The mixture model for two-phase flow, along with empirical models for shear lift force and interface momentum exchange was employed for spherical RBC particles suspended uniformly in plasma at the inlet. arbitrary Lagrangian Eulerian (ALE) method was employed for FSI modeling, with artery (structure) modeled as linear isotropic material. From the multi-physics simulations, it was observed that, although TAWSS did not vary much between single, multiphase, and rigid models, OSI varied significantly between single and multiphase non-Newtonian models while a small difference with rigid model was observed. Overall, the authors concluded that consideration of multi-phase model can alter the hemodynamics and lead to different conclusion on the pathogenesis of atherosclerosis. Further, in order to understand the effect of arterial elasticity and blood visco-elasticity, Bilgi and Atalik83 performed FSI simulation with Newtonian and non-Newtonian Oldroyd-B model. They reported that von-Mises stresses on arterial wall increase with fluid’s elasticity and hence may increase in arterial deformations. This study was performed for aneurysm; however, no such study was found for stenosis.
In order to improve the accuracy of computational results, Baumler et al.84 performed a two-way coupled FSI simulation on pre-stressed aortic archFootnote 32 with true and false lumen separated by flexible aortic dissection. The main motivation of the work was to come up with an accurate model, which could predict flow velocity and deformations in aorta so that the hemodynamics, after a surgery, can be predicted well using the CT scan geometry. The pre-stressing of artery was performed to adjust the CT scan-based geometry with the diastolic load which is present during image capture. Further, a non-linear hyper-elastic model for aortic dissection and artery wall, with elastic modulus varying from 20 to 800 kPa, was considered for simulation. A comparison of velocity and deformation results with 4D MRI measurements (in vivo) showed that the optimized numerical model was able to capture maximum deformations and systolic velocities with a good accuracy, which were underpredicted by non-pre-stressed and untethered numerical simulations.Footnote 33 The results of FSI model showed low TAWSS values in false lumen regions, thus making them prone to endothelium degeneration. Further, the false lumen flow rate was observed to decrease with increasing elastic modulus, indicating pathogenesis for atherosclerosis.
It is important to understand whether a complete FSI simulation or a standalone CFD and/or CSD simulations are sufficient to predict artery rupture in aneurysms. This would lead to reduction of computational cost, which is extremely necessary in a clinical setup. In order to gage this, Valencia et al.85 performed a comparative hemodynamic study on patient-specific cerebral aneurysm geometry using coupled FSI (with a constant elasticity for artery), purely CFD, and purely CSD (with different elastic models) studies. Their CSD model considered segment of aneurysm and complete aneurysm model as two cases with multiple elastic models like hyper-elastic, Mooney–Rivlin, modified MR with experimental data, etc. They observed that CSD and CFD simulations underpredicted the effective stress values as compared to the coupled FSI simulations. Further, there were changes in hemodynamic parameters along with effective stress values for CSD model—with constant elasticity and various non-linear material models. These deviations were minor as compared to a 63% increase in stress observed for a hypertensive artery. Thus, the authors highlighted that the use of FSI simulations with non-linear material modeling can yield similar results as compared to a simpler model for normal physiological loads, but consideration of proper pressure boundary condition (like WindkesselFootnote 34 model) is highly essential.
In order to understand the role of arterial elasticity on low-density lipoprotein (LDL) uptake in left coronary artery (LCA), Chen et al.25 performed FSI simulations on a patient-specific LCA geometry with four cases involving rigid artery, flexible artery with different thickness, and two different blood pressure levels. It was reported that the elastic nature of artery introduced complex flow patterns which reduced the LDL accumulation. Thus, consideration of rigid models can lead to over-prediction of LDL prediction and lead to unnecessary medical treatments. Further, the authors also reported that hypertension (modeled using high blood pressure) can lead to larger changes in LDL accumulation, as compared to that in the rigid versus compliant model.
Chiastra et al.86 investigated the importance of considering flexible nature of artery while computing hemodynamic factors in a stented coronary artery, to monitor a patient for post-surgery complications. Using a commercial software ADINA, they performed two-way coupled FSI simulations for coronary artery with two different stent materials. Further, the results were compared with same geometries modeled as rigid (without deformations). They found that, for idealized models of a stented coronary artery, the rigid wall assumption for fluid dynamic simulations appears adequate when the aim of the study is the analysis of near-wall quantities like WSS. The authors compared the results of fluid–structure interaction (FSI) and corresponding rigid wall models, focusing on the analysis of the WSS distribution. They found that the trends in terms of instantaneous and time-averaged WSS were similar—between compliant and rigid wall cases. Further, between the FSI and the rigid wall cases, the difference of percentage area exposed to TAWSS < 0.4 Pa was about 1.5% for cobalt–chromium (CoCr) and 1.0% for poly-l-lactide (PLLA) stents.
In order to understand the effect of arterial flexibility and RBC movement on the resulting hemodynamics for multiple stenosed coronary arteries, Athani et al.87 performed multi-phase FSI simulations on patient-specific Left Coronary Artery (LCA). The fluid domain was solved, using a finite volume-based commercial software (Fluent R2020), with multi-phase modeling performed using the mixture model. The fluid (blood) and the solid (wall) domains were fully coupled using the ANSYS FSI solver. They evaluated hemodynamic parameters, such as WSS, pressure, velocity, in the patient’s left coronary artery while considering the walls to be rigid and flexible. They found overestimation of hemodynamic descriptors for the rigid models as compared to the FSI models. The region of larger displacement occurs at the pre-stenosis area as compared to the other area of the left coronary artery model. They observed an increase in blood flow velocity across the restricted regions (stenosis) in the LCA, and the recirculation zone at the post-stenosis and bifurcation regions was noted.
5.2 Linear and Non-linear Material Model for Artery
From the extensive review of CFSI modeling methods for blood flow, it is understood that blood flow patterns, accumulation of blood particles and hemodynamic parameters change significantly due to arterial deformations. Hence, consideration of FSI is necessary for both conductingFootnote 35 and distributingFootnote 36 vessels. Apart from selection of suitable FSI and rheological model for blood, it is also very important to model the artery wall deformation accurately. As discussed in Sect. 2, the constitutive relation between \(\sigma\) and \(\epsilon\) are different for linear and non-linear material models. A brief description of these material models is presented in Table 4. For the commonly used linear material model, the stress is related linearly with strain using elasticity matrix \([\varvec{D}]\), which can be calculated using Hooke’s law for plain-strain/stress cases. For non-linear artery model, the stress tensor is defined in terms of derivative of strain–energy function W, which is a non-linear function of strain field \(\varvec{E}\). Although non-linear material models are found to be more realistic and provide closer results with in vivo observations, the associated modeling is mathematically challenging and computationally very expensive. Also, it is reported in the literature that, as we move away from heart, the arteries become thick and have lesser deformation—due to which linear models can be valid. Hence, a brief literature survey of effect of different artery wall model on resulting deformation accuracy is presented below, which enables selection of an appropriate model that is suitable for the artery under investigation.
For artery wall modeling, nonlinear and linear models have been compared in several studies. The choice between these models depends on factors, such as accuracy, ease of implementation, and computational costs. Nama et al.94 presented a systematic comparison between linear and non-linear artery wall modeling approaches, including membrane, shell, and 3D solid formulations. The comparison is presented in an idealized bifurcation model for regionally varying wall thickness, while incorporating the effect of external tissue surrounding the vessel wall. It was reported by authors that although membrane model gave comparable results with available axisymmetric solutions, they failed to converge for bifurcation geometries. Shell models with linear elastic model, which have fewer degrees of freedom, yield closer results with 3D solid model (P2 wedge-type) and hence can be considered optimal for simulation of artery wall response.
Solovyova et al.95 compared the use of the linear and nonlinear models, for artery wall modeling, in the context of blood flow and pulse wave propagation. They presented a brief review of the nonlinear models, and applied both 2D linearized and 1D nonlinear models in their study. They reported that nonlinear models better describe degenerated pathological walls while linear models satisfactorily describe healthy elastic walls. On a contrary note, Baier et al.96 linearized the general non-linear elastic model and compared the displacements with those obtained nonlinear model. Authors reported that linear model matches well with nonlinear model in normal physiological conditions while intima layerFootnote 37 shows deviation in large deformation cases (abnormal physiological loads). Oshima and Tori97 performed FSI simulations, for blood flow in patient-specific aneurysm with linear and general non-linear model for artery wall deformations. Their comparison between artery wall model showed that linear model over-predicts the wall stresses and can lead to high rupture-risk prediction. From the above literature survey, it can be observed that linear models can be considered in healthy artery (with normal physiological loads) while they might lead to lower deformations in highly calcified arteries and those with aneurysms. Regarding choice of suitable non-linear artery model, there is no single consensus and is generally suggested that specific artery parameters may be considered—in the constitutive relation of a general non-linear artery model.
6 Concluding Remarks and Future Outlook
Understanding the complexities of blood-flow dynamics within the human vasculature is important for understanding numerous physiological and pathological phenomena. In this comprehensive review, we present computational fluid dynamics (CFD) modeling techniques applied to blood flow, aiming to address crucial questions shaping the contemporary research. Our investigation centers on three critical decisions one has to make while modeling hemodynamics in human vasculature. First, the relevance of non-Newtonian models in varying vascular conditions and the alterations required to incorporate the viscoelastic nature of red blood cells (RBCs). Second, the validity of single-phase assumptions versus multiphase modeling, particularly concerning arterial geometries and potential particle migration effects; and third, the impact of arterial wall elasticity on blood flow patterns—in order to understand whether a rigid wall assumption suffices or a fluid–structure interaction (FSI) model is required.
Based on an extensive survey of literature encompassing diverse scenarios in blood flow modeling within human vasculature, several key insights have emerged. First, the significance of non-Newtonian blood behavior becomes pronounced in specific conditions: notably, severely stenosed arteries fostering recirculation zones or those with diameters below 4 mm and low Womersley numbers Wo. In these cases, viscoelastic models exhibit substantial deviations from simple Newtonian models, surpassing a 10% difference in predicted outcomes. Conversely, larger arteries like the carotid and aorta, experiencing highly pulsatile flows with elevated Wo, maintain characteristics similar to Newtonian fluids. Secondly, the debate between single-phase and multiphase modeling reveals subtle differences. While straight arteries with stenosis or aneurysms show minimal distinction between these approaches, curved and branched arteries showcase noteworthy particle migration effect that influences hemodynamic parameters. Interestingly, single-phase equations, when integrated with the Philips diffusive flux model, yield promising results as compared to two-phase models; especially in certain arterial configurations. Lastly, the role of arterial wall elasticity manifests differently across various scenarios. Complaint arterial models, as compared to rigid models in larger arteries or those lacking elastin, maintain similar hemodynamics. However, instances, such as hypertension and simulations of blood-flow in smaller arteries, underscore the significance of fluid–structure interaction (FSI) in altering hemodynamic patterns. Based on the literature survey, a brief summary of appropriate physiological modeling techniques is presented in Table 5.
In conclusion, the choice of modeling approach for blood flow in human vasculature must be judiciously tailored to the specific vascular scenario under consideration. Non-Newtonian modeling gains prominence in narrower or more pathological vessels, while the choice between single-phase and multiphase modeling hinges on the vascular geometry and potential particle migration effects. Furthermore, the influence of arterial wall elasticity, particularly in diseased states, underscores the relevance of FSI in accurately simulating hemodynamics, thus showing the multifaceted nature of blood-flow modeling within the human vasculature. Although significant progress has been made in computational modeling, clinical implementation of such studies have been rarely observed. In this regard, future studies can work on following aspects to take CFD-based hemodynamics closer to the medical industry.
-
1.
The integration of multiphase simulation with non-linear elastic arteries as well as non-Newtonian viscoelastic modeling remains a critical frontier, particularly in scenarios involving small hypertensive vessels. While some efforts have been made24, a robust solver that considers both artery non-linearity and viscoelasticity is yet to be developed.
-
2.
Current FSI simulations often overlook the influence of surrounding tissue on vibrations, neglecting its impact based on material properties. Future studies should delve into accounting for these effects for a more comprehensive understanding.
-
3.
Patient-specific CAD geometries from CT images face hurdles in approval and acquisition time. While idealized models are commonly used, innovative approaches, like artificial stenosis generation (proposed in Doutel et al.98) and neural networks offer promising avenues to create realistic yet computationally feasible models.
-
4.
The role of various physics aspects, such as Magneto hydro dynamics (MHD)Footnote 38 and porous walls, remains largely unexplored in hemodynamic modeling—presenting an opportunity for deeper investigations.
-
5.
Application of CFD models for clinical use demands less time-consuming approaches. Assessing the viability of Reduced Order Models (ROMs) for predicting hemodynamics and exploring Physics Informed Neural Networks (PINN) for multi-physics simulations could offer faster computational solutions.
Lastly, effective implementation of computational models for diagnosis and treatment heavily relies on seamless collaboration between medical practitioners and engineers. Ensuring a continuous and productive interaction between these domains is essential for a meaningful progress in this field. These forward-looking perspectives aim to address current limitations and pave the way for more comprehensive, clinically applicable, and efficient CFD-based hemodynamic modeling in human vasculature.
Data availability
The data presented here is obtained from previously published works, which are cited at appropriate locations in text.
Notes
Narrowing or blockage of the coronary arteries, which supply blood to the heart muscle.
Tiny, expandable metal mesh tubes that are placed inside a blocked artery during angioplasty.
Fatty deposit made up of cholesterol, cellular waste products, calcium, and fibrin, blocking blood flow in arteries.
Study of blood flow dynamics within animal vessels.
Use of a strong magnetic field and radio waves to create detailed images of the organs and tissues within the body. MRI can help with viewing injuries, tumors, certain heart problems, and more.
Diagnostic imaging exam that uses X-ray technology to produce images of the inside of the body.
Non-dimensional flow parameter signifying ratio of inertial to viscous forces. Calculated as Re = \(U D/\nu\), where U is characteristic flow velocity, D is artery diameter, and \(\nu\) is kinematic viscosity of blood.
Ability of arteries to expand and contract in response to changes in blood pressure, allowing them to accommodate varying blood flow.
Measure of a fluid’s resistance to deformation under stress.
Study of the fluid properties of blood and its characteristics.
Tensors can be thought of as multidimensional arrays of numbers that transform in a specific way under changes of coordinates.
In multiphase flow, especially when dealing with two or more phases (such as gas–liquid or liquid–solid), the movement and interaction between these phases affect their velocities and distribution. The momentum exchange coefficient helps describe how momentum is transferred between these phases during their interaction.
Property of having negligible changes in density under normal variations in pressure or temperature.
The Lagrangian framework follows individual particles or elements within a system as they move through space and time. It tracks the properties of these elements as they evolve.
A chronic and progressive condition characterized by the buildup of plaque inside the arteries.
The endothelium is a thin layer of flat cells that lines the inner surface of your blood vessels.
Atherogenesis is the complex process by which fatty deposits, called plaques, build up inside the walls of arteries.
WSS refers to the force per unit area exerted by the flowing blood against the endothelial layer (inner lining) of the vessel walls. It is calculated as WSS = \(\mu \frac{\partial u_{t}}{\partial y}\), where \(u_t\) is velocity component tangential to artery wall and n is the normal distance from artery wall.
Mesoscale flow refers to fluid motion occurring at an intermediate scale between the microscale (very small, such as molecular or particle-level interactions) and macroscale (larger, such as the scale of weather systems or ocean currents). Validity of continuum hypothesis starts to break down in these scales.
OSI is a parameter used in the study of fluid dynamics, particularly in the context of blood flow, which describes the directional changes in shear stress on the endothelial lining of blood vessels during the cardiac cycle.
Shear rate is a fundamental parameter used to describe the rate at which adjacent layers of fluid move relative to each other in a flow field. It represents the velocity gradient or the change in velocity per unit distance between fluid layers.
Shear-thinning fluid is a type of non-Newtonian fluid whose viscosity decreases as the shear rate increases i.e., as more force or shear stress is applied, it becomes easier to deform or flow.
Under normal conditions, RBCs tend to align themselves in the center of blood vessels as they flow through. This phenomenon, known as the ‘margination’ or ‘shear-induced migration’ of RBCs, is a result of the shear forces within the blood vessel. The higher shear stress near the vessel walls encourages RBCs to migrate toward the center of the vessel, away from the slower-moving boundary layer near the walls.
Conceptual model used in fluid mechanics that treats a fluid as a continuous substance without any gaps or discontinuities at the microscopic level. It’s based on the idea that within a fluid, the properties, such as velocity, pressure, density, and temperature, vary continuously throughout space and time.
relaxation time refers to the characteristic time it takes for the blood to return to its resting state or original configuration after experiencing a disturbance or change in flow conditions.
The Womersley number (Wo) is a dimensionless number used in fluid dynamics to characterize the unsteadiness of pulsatile flow, particularly in blood flow analysis. It is a dimensionless expression of the pulsatile flow frequency in relation to viscous effects. It is calculated as Wo = \(R \sqrt{\omega /\nu }\), where R is radius of artery, \(\omega\) is angular frequency of pulsation, and \(\nu\) is kinematic viscosity of fluid.
A non-dimensional frequency parameter given by St = fD/u, where f is frequency of flow pulsation (Hz), D is arterial Diameter, and u is characteristic flow velocity.
Axisymmetric simulations are a type of computational modeling used to study fluid flow around bodies that possess axial symmetry. In these simulations, instead of modeling an entire 3D domain, a 2D cross section is employed and rotated around an axis to represent the complete geometry.
This phase occurs when the heart relaxes. The left ventricle relaxes and refills with blood from the atria. Blood continues to flow through the arteries, but the pressure and velocity are lower compared to systole (heart contraction)
Time complexity refers to the computational efficiency of an algorithm, representing how the execution time of the algorithm grows concerning the input size. It helps in understanding how an algorithm’s performance scales as the size of the input increases.
The lumen of an artery is the hollow space inside the vessel through which blood flows.
A curved structure that arises from the ascending aorta (artery coming out from heart), takes a sweeping arch-like shape, and then descends through the thorax.
Tethered numerical simulations in fluid–structure interaction (FSI) involve modeling the interaction between fluids and structures, where one or more solid structures are connected to the fluid domain by tethers or cables. This is implemented by giving Dirichlet boundary condition for deformation at atleast one end.
A windkessel, which translates to “air chamber" in German, is a component in various systems that acts as a reservoir to dampen pressure fluctuations and ensure a smoother flow of fluid.
vessels carrying blood from heart to other arteries.
vessels carrying blood from main artery to arterioles and capillaries.
The intima is the innermost layer of an artery. It is composed of endothelial cells that line the interior surface of the blood vessel.
Magneto hydro dynamics (MHD) is a field of study that examines the behavior of electrically conducting fluids, such as plasmas, liquid metals, or electrolytes, in the presence of magnetic fields. It combines principles from fluid dynamics, electromagnetism, and plasma physics.
References
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN (2019) Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation 139(10):e56–e528
Carvalho V, Pinho D, Lima RA, Teixeira JC, Teixeira S (2021) Blood flow modeling in coronary arteries: a review. Fluids 6(2):53
Conti M, Long C, Marconi M, Berchiolli R, Bazilevs Y, Reali A (2016) Carotid artery hemodynamics before and after stenting: a patient specific CFD study. Comput Fluids 141:62–74
Seo JH, Mittal R (2012) A coupled flow-acoustic computational study of bruits from a modeled stenosed artery. Med Biol Eng Comput 50(10):1025–1035
Zhu C, Seo JH, Bakhshaee H, Mittal R (2017) A computational method for analyzing the biomechanics of arterial bruits. J Biomech Eng 139(5):051008
Ku DN (1997) Blood flow in arteries. Annu Rev Fluid Mech 29(1):399–434
Steinman DA (2002) Image-based computational fluid dynamics modeling in realistic arterial geometries. Ann Biomed Eng 30:483–497
Papathanasopoulou P, Zhao S, Köhler U, Robertson MB, Long Q, Hoskins P, Yun Xu X, Marshall I (2003) MRI measurement of time-resolved wall shear stress vectors in a carotid bifurcation model, and comparison with CFD predictions. J Magn Reson Imaging 17(2):153–162
Marshall I, Zhao S, Papathanasopoulou P, Hoskins P, Xu XY (2004) MRI and CFD studies of pulsatile flow in healthy and stenosed carotid bifurcation models. J Biomech 37(5):679–687
Moore JA, Steinman DA, Ethier CR (1997) Computational blood flow modelling: errors associated with reconstructing finite element models from magnetic resonance images. J Biomech 31(2):179–184
Carvalho V, Rodrigues N, Ribeiro R, Costa PF, Teixeira JC, Lima RA, Teixeira SF (2021) Hemodynamic study in 3D printed stenotic coronary artery models: experimental validation and transient simulation. Comput Methods Biomech Biomed Eng 24(6):623–636
Levick JR (2013) An introduction to cardiovascular physiology. Butterworth-Heinemann, Oxford
Reid L (2021) An introduction to biomedical computational fluid dynamics. Biomed Vis 10:205–222
Tu J, Inthavong K, Wong KKL (2015) Computational hemodynamics-theory, modelling and applications. Springer, Berlin
Zamir M (1999) On fractal properties of arterial trees. J Theor Biol 197(4):517–526
Robertson AM, Sequeira A, Kameneva MV (2008) Hemorheology. Hemodyn Flows 63–120
Commons W Blood Vessels. Based on a diagram in my Biology textbook, and some others. https://upload.wikimedia.org/wikipedia/commons/3/3f/Blood_vessels_%28retouched%29_-en.svg
Pandey R, Kumar M, Majdoubi J, Rahimi-Gorji M, Srivastav VK (2020) A review study on blood in human coronary artery: numerical approach. Comput Methods Progr Biomed 187:105243
Anor T, Grinberg L, Baek H, Madsen JR, Jayaraman MV, Karniadakis GE (2010) Modeling of blood flow in arterial trees. Wiley Interdiscipl Rev Syst Biol Med 2(5):612–623
Wu J, Liu G, Huang W, Ghista DN, Wong KK (2015) Transient blood flow in elastic coronary arteries with varying degrees of stenosis and dilatations: CFD modelling and parametric study. Comput Methods Biomech Biomed Eng 18(16):1835–1845
Lorenzini G, Casalena E (2008) CFD analysis of pulsatile blood flow in an atherosclerotic human artery with eccentric plaques. J Biomech 41(9):1862–1870
Rayz VL, Boussel L, Acevedo-Bolton G, Martin AJ, Young WL, Lawton MT, Higashida R, Saloner D (2008) Numerical simulations of flow in cerebral aneurysms: comparison of CFD results and in vivo MRI measurements. J Biomech Eng. https://doi.org/10.1115/1.2970056
Dennis KD, Kallmes DF, Dragomir-Daescu D (2017) Cerebral aneurysm blood flow simulations are sensitive to basic solver settings. J Biomech 57:46–53
Qiao Y, Zeng Y, Ding Y, Fan J, Luo K, Zhu T (2019) Numerical simulation of two-phase non-Newtonian blood flow with fluid–structure interaction in aortic dissection. Comput Methods Biomech Biomed Eng 22(6):620–630
Chen X, Zhuang J, Huang H, Wu Y (2021) Fluid–structure interactions (FSI) based study of low-density lipoproteins (LDL) uptake in the left coronary artery. Sci Rep 11(1):4803
Wu W-T, Aubry N, Antaki JF, Massoudi M (2020) Simulation of blood flow in a sudden expansion channel and a coronary artery. J Comput Appl Math 376:112856
Bruneau DA, Steinman DA, Valen-Sendstad K (2023) Understanding intracranial aneurysm sounds via high-fidelity fluid–structure-interaction modelling. Commun Med 3(1):163
Jung J, Lyczkowski RW, Panchal CB, Hassanein A (2006) Multiphase hemodynamic simulation of pulsatile flow in a coronary artery. J Biomech 39(11):2064–2073
Xie H, Zhang Y (2017) The effect of red blood cells on blood heat transfer. Int J Heat Mass Transf 113:840–849
Ku JP, Elkins CJ, Taylor CA (2005) Comparison of CFD and MRI flow and velocities in an in vitro large artery bypass graft model. Ann Biomed Eng 33:257–269
Morab SR, Sharma A, Murallidharan JS (2024) Fully finite volume method on a curvilinear grid-based arbitrary Lagrangian Eulerian approach for computational fluid flexible-structure interaction. Comput Phys Commun 296:109054
Gidaspow D (1994) Multiphase flow and fluidization: continuum and kinetic theory descriptions. Academic Press, Cambridge
Kim YH, VandeVord PJ, Lee JS (2008) Multiphase non-Newtonian effects on pulsatile hemodynamics in a coronary artery. Int J Numer Methods Fluids 58(7):803–825
Huang J, Lyczkowski RW, Gidaspow D (2009) Pulsatile flow in a coronary artery using multiphase kinetic theory. J Biomech 42(6):743–754
Fahraeus R, Lindqvist T (1931) The viscosity of the blood in narrow capillary tubes. Am J Physiol-Legacy Content 96(3):562–568
Jung J, Hassanein A, Lyczkowski RW (2006) Hemodynamic computation using multiphase flow dynamics in a right coronary artery. Ann Biomed Eng 34:393–407
Cilla M, Pena E, Martinez MA (2014) Mathematical modelling of atheroma plaque formation and development in coronary arteries. J R Soc Interface 11(90):20130866
Pleouras DS, Sakellarios AI, Tsompou P, Kigka V, Kyriakidis S, Rocchiccioli S, Neglia D, Knuuti J, Pelosi G, Michalis LK (2020) Simulation of atherosclerotic plaque growth using computational biomechanics and patient-specific data. Sci Rep 10(1):17409
Filipovic N, Teng Z, Radovic M, Saveljic I, Fotiadis D, Parodi O (2013) Computer simulation of three-dimensional plaque formation and progression in the carotid artery. Med Biol Eng Comput 51:607–616
Phillips RJ, Armstrong RC, Brown RA, Graham AL, Abbott JR (1992) A constitutive equation for concentrated suspensions that accounts for shear-induced particle migration. Phys Fluids A 4(1):30–40
Yadav SP, Sharma A, Agrawal A (2023) Accurate modeling of blood flow in a micro-channel as a non-homogeneous mixture using continuum approach-based diffusive flux model. Phys Fluids 35(4)
Sia SF, Zhao X, Yu Y, Zhang Y (2019) Multiphase particle-in-cell simulation in severe internal carotid artery stenosis. Powder Technol 358:62–67
Melka B, Adamczyk WP, Rojczyk M, Nowak ML, Gracka M, Nowak AJ, Golda A, Bialecki RA, Ostrowski Z (2020) Numerical investigation of multiphase blood flow coupled with lumped parameter model of outflow. Int J Numer Methods Heat Fluid Flow 30(1):228–244
Melka B, Gracka M, Adamczyk W, Rojczyk M, Golda A, Nowak AJ, Białecki RA, Ostrowski Z (2018) Multiphase simulation of blood flow within main thoracic arteries of 8-year-old child with coarctation of the aorta. Heat Mass Transf 54:2405–2413
Misra J, Adhikary S, Shit G (2007) Multiphase flow of blood through arteries with a branch capillary: a theoretical study. J Mech Med Biol 7(04):395–417
Chien S (1970) Shear dependence of effective cell volume as a determinant of blood viscosity. Science 168(3934):977–979
Johnston BM, Johnston PR, Corney S, Kilpatrick D (2006) Non-Newtonian blood flow in human right coronary arteries: transient simulations. J Biomech 39(6):1116–1128
Huang C, Fabisiak W (1976) Thixotropic parameters of whole human blood. Thromb Res 8:1–8
Braun DD, Rosen MR (2013) Rheology modifiers handbook: practical use and application. Elsevier, Amsterdam
Rao MA (2010) Rheology of fluid and semisolid foods: principles and applications. Springer, Berlin
Walburn FJ, Schneck DJ (1976) A constitutive equation for whole human blood. Biorheology 13(3):201–210
Cho YI, Kensey KR (1991) Effects of the non-Newtonian viscosity of blood on flows in a diseased arterial vessel. Part 1: steady flows. Biorheology 28(3–4):241–262
Siauw W, Ng E, Mazumdar J (2000) Unsteady stenosis flow prediction: a comparative study of non-Newtonian models with operator splitting scheme. Med Eng Phys 22(4):265–277
Quemada D (1978) Rheology of concentrated disperse systems III. General features of the proposed non-Newtonian model. Comparison with experimental data. Rheologica Acta 17(6):643–653
Thurston GB (1979) Rheological parameters for the viscosity viscoelasticity and thixotropy of blood. Biorheology 16(3):149–162
Oldroyd JG (1950) On the formulation of rheological equations of state. Proc Roy Soc Lond Ser A Math Phys Sci 200(1063):523–541
Anand M, Rajagopal K (2004) A shear-thinning viscoelastic fluid model for describing the flow of blood. Int J Cardiovasc Med Sci 4(2):59–68
Rajagopal KR, Srinivasa AR (2000) A thermodynamic frame work for rate type fluid models. J Nonnewton Fluid Mech 88(3):207–227
Hoque SZ, Anand DV, Patnaik B (2022) A dissipative particle dynamics simulation of a pair of red blood cells in flow through a symmetric and an asymmetric bifurcated microchannel. Comput Part Mech 9(6):1219–1231
Hoque SZ, Anand DV, Patnaik B (2018) The dynamics of a healthy and infected red blood cell in flow through constricted channels: a DPD simulation. Int J Numer Methods Biomed Eng 34(9):3105
Fedosov DA, Caswell B, Karniadakis GE (2010) A multiscale red blood cell model with accurate mechanics, rheology, and dynamics. Biophys J 98(10):2215–2225
Bodnár T, Sequeira A, Prosi M (2011) On the shear-thinning and viscoelastic effects of blood flow under various flow rates. Appl Math Comput 217(11):5055–5067
Elhanafy A, Guaily A, Elsaid A (2019) Numerical simulation of blood flow in abdominal aortic aneurysms: effects of blood shear-thinning and viscoelastic properties. Math Comput Simul 160:55–71
Chen H, Zhong G, Li L, Chen Z, Xue Z (1988) The viscoelasticity of human blood at low shear rate. In: Proceedings of the annual international conference of the IEEE engineering in medicine and biology society. IEEE, pp 705–706
Neofytou P (2004) Comparison of blood rheological models for physiological flow simulation. Biorheology 41(6):693–714
Razavi A, Shirani E, Sadeghi M (2011) Numerical simulation of blood pulsatile flow in a stenosed carotid artery using different rheological models. J Biomech 44(11):2021–2030
Arzani A (2018) Accounting for residence-time in blood rheology models: do we really need non-Newtonian blood flow modelling in large arteries? J R Soc Interface 15(146):20180486
Abbasian M, Shams M, Valizadeh Z, Moshfegh A, Javadzadegan A, Cheng S (2020) Effects of different non-Newtonian models on unsteady blood flow hemodynamics in patient-specific arterial models with in-vivo validation. Comput Methods Progr Biomed 186:105185
Karimi S, Dabagh M, Vasava P, Dadvar M, Dabir B, Jalali P (2014) Effect of rheological models on the hemodynamics within human aorta: CFD study on CT image-based geometry. J Nonnewton Fluid Mech 207:42–52
Yilmaz F, Gundogdu MY (2008) A critical review on blood flow in large arteries; relevance to blood rheology, viscosity models, and physiologic conditions. Korea-Australia Rheol J 20(4):197–211
Morab SR, Sharma A (2020) An overview of computational fluid structure interaction: methods and applications. arXiv preprint arXiv:2006.04068
Bazilevs Y, Takizawa K, Tezduyar TE (2013) Computational fluid–structure interaction: methods and applications. Wiley, Hoboken
Bazilevs Y, Hsu M-C, Benson DJ, Sankaran S, Marsden AL (2009) Computational fluid–structure interaction: methods and application to a total cavopulmonary connection. Comput Mech 45:77–89
De Hart J, Baaijens F, Peters G, Schreurs P (2003) A computational fluid–structure interaction analysis of a fiber-reinforced stentless aortic valve. J Biomech 36(5):699–712
Michler C, Hulshoff S, Van Brummelen E, De Borst R (2004) A monolithic approach to fluid–structure interaction. Comput Fluids 33(5–6):839–848
Hughes TJ, Liu WK, Zimmermann TK (1981) Lagrangian–Eulerian finite element formulation for incompressible viscous flows. Comput Methods Appl Mech Eng 29(3):329–349
Trepanier J, Reggio M, Zhang H, Camarero R (1991) A finite-volume method for the Euler equations on arbitrary Lagrangian–Eulerian grids. Comput Fluids 20(4):399–409
Hirt CW, Amsden AA, Cook J (1974) An arbitrary Lagrangian–Eulerian computing method for all flow speeds. J Comput Phys 14(3):227–253
Peskin CS (2002) The immersed boundary method. Acta Numerica 11:479–517
Thekkethil N, Sharma A (2019) Level set function-based immersed interface method and benchmark solutions for fluid flexible–structure interaction. Int J Numer Methods Fluids 91(3):134–157
Xu Z, Yang Y (2020) The hybrid dimensional representation of permeability tensor: a reinterpretation of the discrete fracture model and its extension on nonconforming meshes. J Comput Phys 415:109523
Hirschhorn M, Tchantchaleishvili V, Stevens R, Rossano J, Throckmorton A (2020) Fluid–structure interaction modeling in cardiovascular medicine-a systematic review 2017–2019. Med Eng Phys 78:1–13
Bilgi C, Atalık K (2020) Effects of blood viscoelasticity on pulsatile hemodynamics in arterial aneurysms. J Nonnewton Fluid Mech 279:104263
Bäumler K, Vedula V, Sailer AM, Seo J, Chiu P, Mistelbauer G, Chan FP, Fischbein MP, Marsden AL, Fleischmann D (2020) Fluid–structure interaction simulations of patient-specific aortic dissection. Biomech Model Mechanobiol 19(5):1607–1628
Valencia A, Munoz F, Araya S, Rivera R, Bravo E (2009) Comparison between computational fluid dynamics, fluid–structure interaction and computational structural dynamics predictions of flow-induced wall mechanics in an anatomically realistic cerebral aneurysm model. Int J Comput Fluid Dyn 23(9):649–666
Chiastra C, Migliavacca F, Martínez MÁ, Malvè M (2014) On the necessity of modelling fluid–structure interaction for stented coronary arteries. J Mech Behav Biomed Mater 34:217–230
Athani A, Ghazali NNN, Badruddin IA, Usmani AY, Kamangar S, Anqi AE, Ahammad NA (2021) Two-phase non-Newtonian pulsatile blood flow simulations in a rigid and flexible patient-specific left coronary artery (LCA) exhibiting multi-stenosis. Appl Sci 11(23):11361
Born M, Huang K (1996) Dynamical theory of crystal lattices. Oxford University Press, Oxford
Vorp DA, Rajagopal K, Smolinski PJ, Borovetz HS (1995) Identification of elastic properties of homogeneous, orthotropic vascular segments in distension. J Biomech 28(5):501–512
Chuong CJ, Fung YC (1983) Three-dimensional stress distribution in arteries. J Biomech Eng. https://doi.org/10.1115/1.3138417
Bathe K-J, Zhang H (2004) Finite element developments for general fluid flows with structural interactions. Int J Numer Methods Eng 60(1):213–232
Zahedmanesh H, Lally C (2009) Determination of the influence of stent strut thickness using the finite element method: implications for vascular injury and in-stent restenosis. Med Biol Eng Comput 47:385–393
Loree HM, Grodzinsky AJ, Park SY, Gibson LJ, Lee RT (1994) Static circumferential tangential modulus of human atherosclerotic tissue. J Biomech 27(2):195–204
Nama N, Aguirre M, Ortigosa R, Gil AJ, Humphrey JD, Figueroa CA (2023) A systematic comparison between membrane, shell, and 3D solid formulations for non-linear vascular biomechanics. arXiv e-prints, 2301
Solovyova H, Kizilova N, Mizerski J (2016) Nonlinear model of blood flow through stenosed coronary arteries. In: Proceedings of the 5th international conference on nonlinear dynamics. ND-KhPI2016
Baier-Saip JA, Baier PA, Schilling K, Oliveira JC (2017) Approximate artery elasticity using linear springs. J Med Biol Eng 37:899–911
Torii R, Oshima M, Kobayashi T, Takagi K, Tezduyar TE (2008) Fluid-structure interaction modeling of a patient-specific cerebral aneurysm: influence of structural modeling. Comput Mech 43:151–159
Doutel E, Carneiro J, Campos J, Miranda J (2018) Artificial stenoses for computational hemodynamics. Appl Math Model 59:427–440
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no Conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morab, S.R., Sharma, A. & Murallidharan, J.S. Computational Hemodynamics in Human Vasculature: A Review on Role of Rheology, Multiphase Flow, and Fluid–Structure Interaction. J Indian Inst Sci 104, 13–38 (2024). https://doi.org/10.1007/s41745-024-00425-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41745-024-00425-9