Abstract
Magnesium (Mg)-based material systems offer great potential for healing bone fracture and defects, in terms of reduced stress shielding effect and non-toxicity, due to their biodegradability and biocompatibility. However, an issue with controlling degradation rate of Mg in an intraosseous (occurring within bone) environment has impeded their application in orthopaedics. As a solution to this problem, Mg can be combined with other corrosion-resistant and bioactive materials to form composite. Hydroxyapatite (HA) is an attractive bioceramic for implants due to its similar chemical composition to the apatite found in bone. Thus, incorporation of HA in Mg assists in enhancing multiple engineering properties that are critical for its widespread use in orthopaedic application. Tremendous improvement in the mechanical and degradation properties of HA-reinforced Mg composite, along with their impressive biocompatibility, has led to further interest in research, which has resulted in some clinical trials of Mg–HA-based composites, as well. This review article summarises researches, carried out till date on Mg–HA-based composite, with a special focus on significant role of HA in tuning the degradation and mechanical behaviour of Mg-based materials. The detailed summary on biocompatibility of Mg–HA-based composites has also been covered. A comprehensive understanding on biocompatibility and degradation behaviour of Mg–HA system is needed to assess the potential of these composites in orthopaedic application. However, such review is missing in available literatures. On the basis of current studies available on Mg–HA-based composites for orthopaedic application, guidelines for future application in clinical trials have also been framed and presented in this review article.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Bone is a load-bearing composite, which is quite susceptible to fracture in adverse conditions. Bone grafting is a surgical procedure to fix the damaged or defective bones by regeneration. The use of autograft provides calcium-based scaffolds, necessary for the support and new bone growth.1 This surgical procedure has recognized advantages, e.g. no risk of disease transmission and high potential for new bone growth. However, the incidences associated with it, e.g. pain, infection, numbness and donor-site morbidity; restrict its widespread use in the biomedical application.1 Materials that accelerate the fracture healing and bone regeneration have tremendous potential for orthopaedic application. In this connection, synthetic biomaterials are the only hope for the contribution to human kind. The market value of biomaterials has increased enormously over the last few years.2 The major part of the market of biomaterials belongs to orthopaedic biomaterials.3 Hence, it is of much interest in the field of biomaterials research.
Orthopaedic biomaterials are divided in two categories. The first one is implants and fixture accessories, which are produced from metals, ceramic and polymers. The second category includes scaffolds for tissue regeneration. Clinically used metallic orthopaedic materials include titanium (Ti), stainless steel and cobalt–chromium alloys. These commercially available orthopaedic materials face major drawbacks in terms of stress shielding and revision surgery (in case of fracture fixing temporary implants), as they are not biodegradable and have much higher mechanical properties than bone.4 These challenges have driven the research towards search for alternatives in form of biodegradable biomaterials, which would not only overcome the shortcoming of bio-inert (Ti, Co–Cr, SS) materials but also degrades with regeneration of bone over a given period of time. The candidates for biodegradable implant materials can be polymers, metals, ceramics or a combination, in forms of composites.
1.1 Commercially Available Biomaterials for Orthopaedic Applications
Polymers, suitable for biomedical application, can be categorized as natural (biological nature) and synthetic, by their source of origin. The proteins, such as, collagen and gelatin come under the natural polymers. On the basis of degradation in in-vitro and in-vivo environment, these polymers can also be categorized in degradable and non-degradable polymers. Generally, degradation of these polymers in physiological solutions takes place by two basic mechanisms, i.e. passive hydrolysis and active enzymatic reactions.5 Poly (hydroxyl acids) is common class of synthetic polymers, which are synthesized by ring opening polymerization (ROP) and also polymerization by condensation. The above polymer undergoes bulk degradation. Once eroded, the monomer components are removed from body through natural pathways. The key advantages of this system are kinetic degradation and modifiable mechanical behaviour. However, the main drawbacks are the eroded products, leading to reduction in pH, which ultimately leads to inflammatory reaction, along with high bulk erosion.6 The other weaknesses include poor hydrophilicity and excessive degradation rate of this polymeric system. The application of polymers includes bone screws and plates for small implants. The most common polymers, available in this category, are PGA (polyglylolic acid), PLA (polylacticacid) and PLGA (polylactic-co-glycolide). PLA is often reinforced with HA or chitosan to modify the mechanical properties and osteocompatibility.7, 8
The silk fibroin (SF) is another available natural biodegradable polymer, produced from silkworms or spiders. SF acts as active sites for bone mineralization and bonding with bio molecules, leading to bone regeneration. The studies have shown that SF scaffolds perform better than PLA ones in rat model, in terms of expedited bone regeneration.9 In connection to this, SF solubility rate can be controlled from days to year.10, 11 Although several studies have shown successful in-vitro and in-vivo performance of silk-based biomaterials, none of these studies have proceeded for human trial.12 BioFixTM has recently launched its biodegradable bone fixation accessories made of PLGA 8218 (82% poly-l-lactide and 18% glycolide). As per the catalogue, they have claimed the retention of complete tensile strength and degradation resistance for 14 and 30 weeks, respectively (Online14). But the given initial tensile strength (65 MPa) and Young’s modulus (3.3–3.5 GPa) for these accessories are quite low as compared to the natural cortical bone (tensile strength: 38–283 MPa, young’s modulus: 5–23 GPa) for load-bearing applications (Online15).
The applications of ceramic biomaterials are growing tremendously. It is mainly because of its biocompatibility, better corrosion resistance in physiological environment and chemical similarity with natural bone minerals in some cases. These ceramic materials have tendency to be used as the bone substitute or to promote the bone regeneration.16 The derivatives of calcium phosphates, which are more relevant to chemistry of bone tissue, are hydroxyapatite (HA) and tricalcium phosphate (TCP). The processing of these materials is generally done through powder processing route. Sintering of final product decides its microstructure. The HA particles have comparatively low dissolution rate to TCP particles in the physiological environment.17, 18 In addition to that, it offers excellent osteoconductive properties and thus is favoured as suitable reinforcing materials for metal matrix composite. Further, the presence of HA, as a coating or reinforcement in metallic implant, provides nucleating sites for the growth of apatite crystals and also increases the growth rate of apatite layer on metallic implant surfaces, making them integrated to the bone structure. Thus, HA is being studied widely by many research groups to extract all its potential in orthopaedic applications.19,20,21 The only major limitation of HA is its high brittleness, which makes it inappropriate for load-bearing application.
Another available biodegradable ceramic is bioactive glass (BG). BG releases Na+ and Ca2+ ions during dissolution in the body fluids, which help in new bone growth. Besides being biocompatible, BG offers good bonding with the surrounding bone tissues. Brittleness is again the major limitation for BG materials to be used for load-bearing applications.22
1.2 Current Need of Biomaterials for Orthopaedic Applications
Metals and their alloys have been used widely over centuries for the load-bearing applications in orthopaedics (pins, plates, screws, knee or hip prostheses and dental implants, etc.), due to their excellent mechanical properties. Currently, three main types of metal systems, used in orthopaedics, are Ti-based alloys, Co-based alloys and stainless steel (SS). But studies revealed that SS is prone to corrosion in the physiological environment (simulated body fluid), due to the presence of significant quantity of chlorine in the human body.23,24 Still, SS is commonly used in implants due to their economic affordability. In the field of hip and knee joint prostheses or devices, Co-based alloys (Co–Cr and Co–Ni) are widely used due to their high wear resistance and biocompatibility.25 These alloys also offer high corrosion resistance and fatigue strength. There is a study showing Co–Cr-based alloys performed better in corrosion, as compared to stainless steel, demonstrating better performance in chlorine-rich environment. It is due to the formation of a passive layer of Cr2O3 in the human body environment.26 However, reports are also available on high amount of Ni and Cr being released at implantation site, causing toxic effects or allergic responses.27 Titanium (Ti) and its alloys are found to be promising for bone replacement implants. Ti possesses low density (4.5 g/cm3), good elastic modulus, significant corrosion resistance, biocompatibility and non-toxicity in human body environment.28 Ti and its alloys are also found to make good physical connections with the host bone28 and thus, have been used widely in total hip replacements and craniofacial implants.26 However, there are some common problems of metals and their alloys, such as, the stress shielding effect. This arises due to the mismatch in the elastic modulus of metal implants and that of natural bone. Stress shielding occurs when implant takes more portions of load and adjacent bone tissues possess comparatively less load, which ultimately leads to the loss in density of bone. This phenomenon is known as stress shielding caused by commercially available metallic implants, having elastic modulus higher than the natural human bones. Further, corrosion leads to wear debris or metal ions, which induce inflammatory and allergic reactions. One promising strategy to achieve suitable elastic modulus is to prepare porous metallic implants. But the use of these porous structures is limited to the tissue engineering applications due to their poor mechanical attributes.
Beyond these commercially available biomaterials, there is a need for the development of a biomaterial system which is biodegradable in body fluids and having elastic modulus similar to human bones. Metals, such as, magnesium (Mg), zinc (Zn) and iron (Fe) are degradable in the body fluids and show better biocompatibility. Additionally, Mg is having elastic modulus (~ 41–45 GPa) very similar to human bone (10–20 GPa).29 Degradation kinetics and accumulation of inflammatory iron hydroxide particles in many tissues have been the major limitations with the iron (Fe) metals.30 Slow degradation of Zn in the body fluid (complete degradation may require several years) is the main issue with the Zn metals for temporary orthopaedic application.30, 31 Magnesium can be alloyed with many different materials, such as, zinc, calcium, and aluminium. These alloys can be strengthened by uniform dispersion, solid solution and precipitation hardening.31 Furthermore, magnesium composites are now introduced in the fields of orthopaedic implants.
1.3 Biodegradable Magnesium as a Viable Solution and Challenges
The clinical application of biodegradable Mg-based materials is a tangible vision in temporary orthopaedic implants. Currently applied permanent metallic implants, for temporary applications as fracture fixing accessories, have several negative aspects, such as, inflammatory osteolysis due to the toxic release of metallic ions and interference in the radiological studies makes their uses limited.32 So, the non-toxicity of degraded particles is the primary concern for biodegradable implants. Interestingly, Mg2+ ions are the fourth most available cation in human body. In a healthy 70 kg human body, ~ 25–35 g (~ 1 mol) of Mg is stored.33 More than half of total physiological magnesium is present in human bone.33 Approximately 35–40% of total Mg is found in the soft tissues, followed by the blood serum. In addition to this, Mg element also takes part in more than 300 enzymatic and adenosine triphosphatase (ATP) reactions in the human body.33
Further, Mg-based materials possess the density of 1.74–2 g/cm3 which is quite comparable to the natural human bone (1.8–2.1 g/cm3).29 Additionally, elastic modulus of Mg-based materials is also quite comparable to natural bone (cortical bone 10–27 GPa, Mg 40–45 GPa).34 This similarity in the elastic modulus can address the issue of stress shielding, which is associated with the currently available metallic orthopaedic implants.
The high solubility rate of Mg in physiological environment is a major limitation in orthopaedic application.35 The electrochemical reaction involves formation of magnesium hydroxide [Mg(OH)2] layers and liberation of hydrogen (H2) gas. Mg(OH)2 acts as a temporary protective layer. But, the exposure of these hydroxide layers to chloride (Cl−) environment further enhance the degradation rate as Mg(OH)2 layer converts into MgCl2. Presence of high concentration of Cl− in the in-vivo condition leads to bulk degradation in the body environment.36
This high corrosion rate of Mg in in-vivo environment can have a toll on the mechanical integrity of the composites, even after short time exposure in physiological condition. Mg and its composites are attractive for fracture fixing accessories, in particular as bone screws and plates. To have enough mechanical strength of the Mg-based composite during in-vivo application, implants should have better degradation kinetics to match with the healing rate of the damaged bone tissues. Figure 1 shows the schematic representation of the desirable degradation kinetics of orthopaedic implants in line with the mechanical strength, till the total healing of the damaged bone tissue.
It has been observed that initially the degradation rates of Mg-based materials are very fast in the physiological solution, but it reduces with the time. Conversion of Mg(OH)2 protective layer in MgCl2 layers degrades materials severely and the mechanical integrity of the implants gets affected.37 Measures have been taken for slowing down the degradation rate of Mg, which includes alloying of metallic elements, use of ceramic materials as reinforcement (e.g. HA) and surface treatment. There are several limitations associated with the alloying of Mg metals, such as, the toxicity of alloying element (e.g. Al, Zr and rare earth metals) and less solubility of alloying element (e.g. Ca < 1.34%).4, 29 Additionally, low melting point (~ 650 °C) of Mg metal restricts fabrication of high corrosion-resistant ceramic coating on the surfaces. So, the development of a composite with inert and biocompatible ceramic phases as reinforcement could be the better option to tune the solubility of implant and bone regeneration.
1.4 Development of Mg-Based Composites
The importance of Mg was first recognized efficiently in 1907 by a surgeon named Albin Lambotte, who used Mg nails to fix the 2-months old fracture in 17-years old youth to treat severe pseudarthrosis in lower part of leg. Thus, magnesium degraded in 8 days and hydrogen gas was produced under the skin.38 Earl D. McBride also tried using Mg alloy (Mg: 95.7%, Al: 4%, Mn: 0.3%) plates and screws in the year 1938.39 The effervescence of the hydrogen gas during the corrosion reaction was the major issue reported in this study. The continued use of Mg was abandoned at that point because of the lack of mechanical properties, high degradation rate and high rate of hydrogen gas evolution at the implantation site.
The effort for overcoming the undesirable shortcoming of freestanding Mg implants has led to exploration of Mg-based composites for orthopaedic application. Several studies have explored the potential of Mg-based composite system using different bioceramics (e.g. HA, TCP, BG) as the reinforcement to improve mechanical properties, corrosion resistance and biocompatibility.40,41,42 Alumina (Al2O3) is one of reinforcement materials for Mg-based composites. It is bioinert in nature. It has attractive properties to be used for bone implants, such as, high wear and corrosion resistance. It is thermodynamically stable in nature. One of the in-vivo studies in white Japanese rabbit, performed using alumina as a reinforcement material, depicted weak tissue reaction.43 In addition to that, zirconia, calcium phosphate, bioglass, and carbon are other classes of reinforcement materials. Out of all the given reinforcements, zirconia is an emerging one, especially highlighted for total hip replacement application. However, small traces of radioactive elements were found with zirconia, which are quite harmful to living tissues.44 Bioactive glasses are another category of reinforcement used nowadays. They are mostly used in orthopaedic and dental prosthesis. Calcium phosphate ceramics (CPC) are widely known biomaterials for more than 20 years. The commonly used CPC are hydroxyapatite (HA) and beta tricalcium phosphate.
HA is a natural bioceramics material, found in the mineral part of natural human bones. It has the chemical formula of calcium apatite (Ca5 (PO4)3(OH) (Ca/P ratio of 1.67), also known for low degradation rate in physiological condition.45 Additionally, HA shows significant bioactivity and biocompatibility. In a nutshell, HA has a similar chemical and structural characteristic to the mineral part of natural bone.46 The application of monolithic HA is limited due to its insignificant load-bearing capacity. However, it serves as an ideal reinforcement in Mg-based metal matrix composites for orthopaedic applications. Figure 2 shows the summarized data on total number of publication based on HA reinforcement in Mg, in chronological order. Based on the given data, importance of HA in Mg-based composite can be clearly understood. A significant increase in the number of publications in the year 2016–2018 can be seen, which reveals the importance of Mg–HA composites in contemporary research. Thus, a comprehensive review on the effect of HA in Mg material will give a clear idea of advancement in the orthopaedics field. In addition to that, this review will produce a clear picture on the present status of findings. Not only this, it will also help in realizing the untouched areas and thus, leading the research community towards the proper direction for future research.

Source: http://Scopus.com
Chronological record of number of publications on HA reinforced Mg-based composites
So, in the present review article, studies related to the effect of HA in Mg-based materials have been summarized in terms of the different fabrication techniques available to synthesize the given composites; keeping the limitations of these material systems in mind. Comprehensive analysis of degradation and biocompatibility behaviour of these composites in the physiological environment has been given main priority. In addition to that, article includes a comparative discussion on the in-vivo biodegradation and biocompatibility performance of Mg–HA-based composite systems. Finally, this article presents a snapshot of current state of Mg–HA composite, with an understanding of the challenges and development.
Several comprehensive studies have reported the effect of different reinforcement in Mg-based composite system in terms of the mechanical behaviour and corrosion resistance. Based on the excellent outcomes of HA reinforcement in Mg-based composites, the detailed study of these composite systems, in terms of in-vitro degradation behaviour in different physiological environment, as well as, the in-vivo performance need to be summarized thoroughly to provide a clear picture of these materials system for temporary orthopaedic application. As per the authors’ knowledge, none of the review articles have summarized the detailed degradation behaviour of HA-reinforced Mg-based composite in several different physiological solutions. In addition to that, most important property, biocompatibility, needs to be addressed in detail for these composite systems. In this review article, the progress on the development of HA-reinforced Mg-based composites, with particular focus on the degradation behaviour in different physiological solution and bioactivity performance in in-vitro and in-vivo conditions, have been addressed in a comprehensive manner.
2 Fabrication of Mg–HA-Based Composite
Homogeneous distribution of HA in Mg-based matrix, along with the better densification, are the main points taken care during the mixing and consolidation of powders, to control the porosity. Figure 3 represents different categories of synthesizing techniques used to fabricate Mg–HA-based composites. Desired temporary orthopaedic application properties, like, suitable degradability in physiological environment, significant mechanical property and better structural integrity of composite, can be achieved by tuning the dispersion of HA reinforcement and porosity. Following are the sub sections giving a clear picture on efficacy of each technique in consolidation of Mg–HA-based composite.
2.1 Powder Processing Route
Powder processing route is the most widely used technique for the fabrication of Mg–HA composites. Conventional powder processing consolidation technique has mainly been applied for synthesizing Mg–HA-based composite with variety of modifications to optimize the temperature and exposure time.
2.1.1 Conventional Sintering
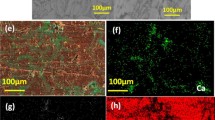
Sintering is the process of making dense object from the green compacts by applying heat below their melting point. Bonding of the particles takes place by the process of diffusion, leading to densification of the structure. The consolidation of Mg–HA-based composite by conventional sintering is always carried out after green compaction of the powders.29, 40, 48–50 Uniaxial compaction has been generally used to make green compacts. Isostatic pressing has also been tried in cases, for making green compacts out of the composite powders29, 51 using ball milling technique to mix the Mg/HA (10, 20, 30 wt%) powders using agate balls, followed by the combination of cold pressing and hot extrusion to achieve the composite structure. Morphology, mechanical behaviour, in-vitro assessment and biocompatibility of Mg/HA composites were performed after the fabrication of Mg–HA composites. It was observed that, with increase in content of HA (> 10 wt%), the extent of uniform distribution of hydroxyapatite decreased. The tensile yield strength increased, but ultimate tensile strength and elongation decreased with HA reinforcement. Moreover, the corrosion resistance of Mg/HA composites decreased with an increase of HA content beyond 10 wt%.51 Mg–10HA composites showed good biocompatibility and did not induce any toxicity in L929 cells.51 In a study by Khalajabadi’s et al. a three-step process, involving milling–pressing–sintering technology, was used to prepare Mg/HA/TiO2 composites and its properties were compared with Mg/HA nano-composites. In comparison to Mg/HA composite, the corrosion resistance of Mg/HA/TiO2 composites improved and its biocompatibility was also retained significantly. However, the presence of TiO2 in the Mg–HA composite system hinders its full degradability in the body fluid. In addition to this, researchers have even tried the concept of two-stage sintering in conventional approach to achieve better compaction.29 The major issue with conventional sintering is that of long duration and low heating rate. The chances of oxidation during heating are more in conventional sintering, which becomes crucial in case of magnesium-based materials. Various ranges of temperatures, starting from 350 to 600 °C, with a dwell time of 2– h, have been adopted for Mg–HA-based composite.29, 40, 48, 52, 53 Due to the higher melting point of HA (~ 1100 °C), it does not allow the particles to form bonding at Mg–HA interfaces. Low heating rate of conventional sintering route also creates the limitations in achieving high density. The present authors have used the conventional sintering approach to compact the Mg–HA.29 Figure 4 shows the scanning electron microscopy image of the individual powders and Fig. 4d shows the uniform dispersion of 5 wt% HA powder in Mg–3 wt% Zn powder. Sintering of the green compacts was performed in two stages, with a cycle of 450 °C for 8 h, followed by 550 °C for 4 h. Relative density of 91–96% was obtained for Mg–3Zn and Mg–3Zn/HA composites. This study has shown that the incorporation of 5 wt% HA to Mg–3Zn matrix composite via conventional sintering route has enhanced the corrosion resistance and compressive yield strength by ~ 42 and 23%, respectively.29 To evaluate the potentials of these composites for bioactivity behaviour, protein adhesion study was also performed on Mg–3Zn and Mg–3Zn/5HA composites.54 Addition of 5 wt% HA has enhanced the protein adhesion by ~ 40% as compared to without HA composite.55 Recently, magnesium with 6.5 wt% Zn, along with a range of HA content (0, 5, 10 wt%), synthesized through powder processing route via conventional sintering, suggested that Mg with 10 wt% HA exhibited highest corrosion rate.55 Similarly, other studies on Mg–HA-based composites developed through powder processing route using conventional sintering technique, show the limitation of usage of maximum composition of HA for better density and significant corrosion and bioactivity behaviour.29, 55 These findings suggest that conventional sintering route have limitations for incorporating maximum composition of HA in Mg matrix. The conventional sintering was mostly carried out in inert atmosphere, i.e. argon gas and vacuum. Although, there is no study available as per the knowledge of authors, which can summarize the advantages and disadvantages of different sintering atmospheres on Mg–HA-based composites.
Powder FESEM images of a HA, b Mg, c Zn, d 5 wt% HA mixed with Mg–3Zn, e elemental analysis of 5 wt% HA added Mg–3Zn powder29.
2.1.2 Spark Plasma Sintering
Spark plasma sintering (SPS) is another method of sintering used for the consolidation of Mg–HA-based composites.40, 56–60 The benefits of using spark plasma sintering for Mg–HA-based composite system are (1) fine grain morphology; (2) high relative density; (3) comparatively less time required for sintering; (4) lower temperature and (5) application of high pressure. Spark plasma sintering is a very promising technology for the fabrication of ceramic and nanostructured materials since it retains fine grain morphology after sintering.40, 61 It is more helpful in case of ceramic materials, as fine grain could also increase the mechanical properties, such as, hardness, compressive strength and fracture toughness.40 The conventional sintering route requires higher temperature and longer holding time, which ultimately causes grain growth severely. On the other hand, SPS involves pressure and fast heating rate simultaneously. The outcome through SPS route is comparatively better density at very low temperature. Because of shorter duration in SPS, the microstructure is retained, leading to improvement in mechanical characteristics of the material (Sidhu 2018).40, 61 Spark plasma sintering of Mg–HA has operating temperatures within range of 350–500 °C,58, 61 pressure of 30–80 MPa in vacuum or argon atmosphere.58 The systematic studies have shown minimum range of 475–585 °C as the optimum spark plasma-sintered temperature for Mg–HA composite system.58
Ratna Sunil et al.34, 35, 40 synthesized Mg–HA-based composites using SPS method. Addition of 10 wt% HA in Mg matrix reduced the corrosion rate significantly. It was observed that, after the addition of 10 wt% HA, Ecorr, of Mg–10HA, composite shifted towards the positive with increase in corrosion resistance by ~ 15%.
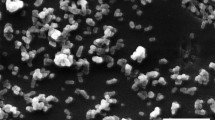
Prakash et al. reported synthesis of Mg–HA-based composite using SPS method.60, 61 Sintering temperature of 350 °C was used to consolidate the mixed powders, which is quite low when compared to other studies. It has been observed that addition of 10 wt% HA in Mg-based composite has reduced the corrosion resistance drastically by ~ 52%. Low sintering temperature of this composite system might be reason for deteriorating the corrosion properties. Muhammad et al.58 have reported the effective range of temperature during spark-plasma sintering of magnesium-based composites to be 475–585 °C. They have claimed that tensile strength of composites has increased with the sintering temperature, due the better consolidation. Although, there was no sign of hardness change with the temperature for SPS-sintered Mg–HA composite. In another effort59 to synthesize Mg–HA composite through SPS, a temperature of 475 °C and pressure of 40 MPa was used in vacuum atmosphere. Mg and HA powders were first ball-milled for 2 h for mixing of the powders. After sintering through SPS, the consolidated specimens were treated through plasma electrolytic oxidation (PEO) to further improve the corrosion resistance. Figure 5a–d shows the optical micrographs of sintered magnesium/hydroxyapatite composites. The morphology of sintered Mg/10 HA (Fig. 6c) is revealing minor chunks (agglomeration) of HA particles (black in colour) randomly dispersed in composite. But, severe clustering is observed in Mg/15HA composite system (Fig. 6d). Agglomeration of HA reinforcement limits the content of HA in Mg matrix (e.g. 15 wt% in this case).62
Optical micrographs of the compacts a pure Mg, b Mg/5HA, c Mg/10HA d Mg/15HA62.
Compressive stress–strain behaviour of Mg–3Zn/HA composites fabricated via powder processing route using conventional sintering29.
Simultaneous application of pressure and temperature in SPS technology allows incorporation of higher content of HA, as compared to conventional sintering. Thus, spark-plasma sintering could be the promising technique for consolidation of Mg–HA-based composite system.
2.2 Casting
Casting is another conventional approach to synthesize the composite materials system. Mg/PLGA scaffolds were synthesized using solvent casting technique followed by the salt leaching.63 Compressive strength of the porous structure increased by ~ 180% with the addition of 40 wt% Mg powder. In another study,64 Mg–3Zn–Ca/β-tricalcium phosphate (β-TCP) bioabsorbable material was fabricated by melt shearing along with high-pressure die casting (HPDC) technique. The dispersion of β-tricalcium phosphate particles in magnesium matrix was achieved through high shear unit. Improvement was seen in hardness. But elongation and yield strength could not match the mechanical integrity. Another research compared the degradation rate of HA/Mg–Zn–Ca and TCP/Mg–Zn–Ca, synthesized by shear mixing casting method.65 Though, the rate of dissolution of β-tricalcium phosphate in physiological solution is slightly higher than HA. But, TCP/Mg–Zn–Ca composite studies have shown quite better degradation resistance as compared to HA/Mg–Zn–Ca composite.64 The degradation rates of β-tricalcium phosphate reinforced composites were lower than HA-reinforced Mg matrix composites.64 Further, another Mg–HA composite was synthesized by melting, followed by hot extrusion, with different composition of HA (5, 10, and 15 wt% HA).17, 45 The results showed increment in compressive strength of composite, with the increase in percentage of HA. But, tensile strength of these composites showed decrement with the HA composition, due to the brittle nature of HA.17, 45 Ye et al.66 have also designed Mg–Zn–Zr–nHA composite, prepared by melting and hot extrusion. Addition of 1 wt% nano HA powder (nHA) in Mg–3Zn–0.8Zr matrix improved immersion corrosion resistance by ~ 72% after 20 days of immersion. Sun et al.67 have also synthesized Mg–3Zn–0.5Zr/xHA (x = 0, 0.5, 1 and 1.5 wt%) composites through melting and mechanical stirring, followed by hot extrusion. They have reported ~ 10% improvement in mechanical properties for Mg–3Zn–0.5Zr/1.5 HA composite with addition of HA. However, Mg–3Zn–0.5Zr/1 HA composite showed ~ 60% lower degradation rate, after 12 days of immersion.
2.3 Microwave-assisted processing
The microwave science has also been used as rapid processing technique for the fabrication of magnesium-based composite. Chemical reactions between the powder particles are initiated using radiation technique. The electromagnetic waves (wavelength of 1 mm to 1 m), with corresponding high frequency (300 MHz to 300 GHz) electric fields, are used produce the radiations. On the application electromagnetic waves, polarization of the bound charges happens within the material. By maintaining the energy balance without a temperature gradient provides uniform heating. Thus, the synthesis process takes lesser time as compared to conventional sintering route.68, 69 The earlier studies on microwave technology focused only on the monolithic materials. Until now, there is only study on Mg–HA-based composite, fabricated through microwave-assisted sintering.70
The researcher70 mentioned the advantages of sintering route in terms of densification, fast heating rate and balancing of energy, thus saving the time required for the whole process. Additionally, use of 15 wt% HA in Mg showed ~ 66% higher microhardness and ~ 44% increases in flexural strength as compared to Mg. Addition of 10 wt% HA into Mg leads to 67.5 and 42.8% increment in the compressive strength and modulus, respectively.
2.4 Friction Stirring Process
Friction stir processing (FSP) has also been used to synthesize Mg–HA-based composites in several studies.34, 35, 40, 71, 72 This solid state processing technology works on the concept of friction stir welding. In this technique, the tool in the form of cylinder consists of small pin, which is penetrated in to sample surfaces. Further, it is plunged along the surface, which induces heavy plastic flow during the process followed by the dynamic recrystallization in the area of FSP zone. This recrystallization gives fine gain microstructure. The stirring action of friction stir processing can be used to fuse the ceramic powders (HA) into the Mg matrix. Report is also available on significant reduction of grain size (~ 93%) as a result of FSP.34, 35, 40 Another report through FSP showed 52% increase in corrosion resistance of Mg–5 wt% HA composite. Reduction in the grain size of Mg–5 wt% HA composite helped in the more apatite formation due to the increase in the grain boundary area per unit volume. However, uniform dispersion of HA throughout the composite, as well as, the fabrication of bulk composite structure cannot be achieved through FSP technique. In addition to that, wear debris of FSP tool contaminate the base metals during the process of fabrication.73
2.5 Other Fabrication Techniques
High-frequency induction heat sintering (HFIHS) method has also been explored for synthesizing Mg–HA-based composites.74, 75 The study reported, HFIHS as a promising sintering technique for the consolidation of metals and ceramics. This rapid sintering involves a coil (known as work coil), which is wrapped around a work piece of nanostructured ceramic or metal. A very high-frequency, high-power A.C. current flows around workpiece. The workpiece becomes red hot first and afterwards it is molten. This technique is quite similar to hot pressing (carried out in graphite die). But the sintering is accomplished through high-frequency electricity. The current generated in the coil is highly intense, which changes the magnetic field rapidly within the space of work coil. Thus, the workpiece gets heated, which is placed within magnetic field. Khalil et al.75 showed the effect of HFIHS sintering conditions on morphology and mechanical behaviour of Mg–HA composites. The relative density (RD) of Mg: 5 wt% HA composite system was obtained ~ 99.7%, at temperature of 550 °C. Another report74 on Mg–HA composite by same group showed the excellent performance against degradation in simulated body fluid (SBF) for Mg/5 wt% HA.
3 Tunability of Mechanical Properties
HA is found to be the ideal reinforcement for Mg matrix, while tuning the mechanical behaviour of Mg-based composites. In general, being ceramic in nature, addition of HA in Mg materials enhances the hardness and compressive strength of composites. However, tensile property deteriorates after the addition of HA. Nevertheless, comprehensive strength is more important for the material system to be used in orthopaedic applications.
Xu et al.76 have synthesized Mg–HA composite via conventional sintering route. They have reported ~ 8% improvement in the compressive strength after the addition of 5 wt% HA in Mg matrix. In another study on Mg–HA composite, fabricated through melting and extrusion process, decrease in the tensile strength by ~ 27% with 15 wt% HA addition is recorded.17, 45 Elongation also decreased with the addition of 15 wt% HA, which shows the brittle nature of the composite. Strengthening of Mg–HA composite depends on many factors, such as (1) load transfer from matrix to reinforcement; (2) type of processing technique used for fabrication and (3) type of reinforcement used.
Figure 6 shows the representative stress–strain curve of Mg–3Zn/HA composites, fabricated through powder-processing route via conventional sintering technique. Incorporation of 5 wt% HA is found to be effective in increase in the compressive yield strength of Mg–3Zn/HA composite by 23%, as compared to Mg–3Zn.29 Higher compressive strength of HA (~ 700 MPa) can positively influence the mechanical property of composites.
In addition to that, compressive strength of Mg also depends on the homogeneous distribution of HA inside the matrix. Agglomeration of HA nano particles in the composites is the main cause of poor mechanical properties with higher HA content.
Figure 7 presents the comprehensive plot of ultimate compressive strength, obtained after addition of different compositions of HA in Mg-based matrix in different studies.42, 45, 46, 62, 78
It can be clearly seen from Fig. 6 that the addition of HA in Mg-based matrix generally enhances the compressive strength of composites up to a certain composition due to the brittle nature HA ceramic. However, the content of HA is limited due to starting of their agglomeration at higher content, which makes composite comparatively weaker. However, strength of theses composites also depends on the presence of other elements as well.
Addition of HA in Mg-based matrix also tunes the hardness of Mg–HA composites system. Addition of harder phases (i.e. ceramic) in Mg materials generally enhances the hardness of the composite system significantly. In addition to that, processing route of fabrication also contributes to altering the hardness of composites. Researchers have used Vicker’s hardness technique and instrumentation indentation measurement29, 60, 61 to quantify hardness of Mg–HA composite. Jaiswal et.al showed ~ 41% improvement in hardness for 5 wt% HA-reinforced Mg (Fig. 8).29 Similar trend was observed by other studies as well60, 61 HA has hardness value of 5.8 GPa,79 which is significantly higher than Mg (0.44 GPa).80 This is one of the reasons for high hardness of composite material. The increment in hardness values can also be attributed to the cumulative effect of work hardening, due to presence of the dissimilar particles in the composite. On other hand, a study conducted by Ratna Sunil et al.34, 35, 40 on Mg–HA (0, 8, 10 and 15 wt%) composite, fabricated through spark plasma sintering, has reported decrement in microhardness by 18% after the addition of 8 wt% of HA in Mg matrix (Fig. 9a, b). It might be due to the agglomeration of HA nanoparticles during SPS. However, an inconsistency in the hardness trend was observed with the HA composition. Addition of 10 wt% HA in same Mg matrix further increased the nanohardness of the composites. Addition of more HA in Mg matrix might produce higher strain hardening, which may be the reason for the further increment in the nano hardness. Although, continuous drops in the young’s modulus values was observed with the increment of HA composition in Mg matrix (Fig. 9c, d). However, no explanation is provided for this apparently unexpected behaviour.
Hardness variation of composites as a function of HA content29.
The HA addition to Mg enhances the hardness impressively due to (1) strengthening of matrix and (2) strain hardening. Clustering of HA in Mg matrix inhibits the improvement of hardness. Similar to compressive strength, the hardness also depends on the processing parameters of consolidation route.
4 Mg–HA-Based Composites
4.1 Biodegradation of Mg–HA-Based Composites
Recently, Mg-based biodegradable implants have made much progress in the development of smart materials for orthopaedic application. Although, the extensive use of Mg-based orthopaedic implants is still restricted mainly due to their high corrosion rate in physiological environment. In addition to that, integrity of mechanical properties during degradation also inhibits the extensive application of these metallic materials. The degradation of Mg metal in aqueous solution can be presented by the following equations. Equation (1) represents the partial primary anodic reaction and Eq. (2) expresses the reduction of protons at cathode site.
Figure 10 represents the schematic diagram for basic corrosion mechanism of Mg metal. Formation of hydrogen gas during the degradation of Mg-based implants is another undesirable consequence of the reaction. High concentration of Cl- ions, present in the physiological environment, accelerates rapid formation of subcutaneous hydrogen bubbles. Major effect of hydrogen gas accumulation can be seen in the first week of the implantation, which approximately vanished after 2–3 weeks of implantation.81 Song et al. postulated that the human body has the tendency to tolerate the hydrogen gas evolution rate of 0.01 ml/cm2/day, which generally does not create any trouble.82 Hydrogen gas release can be directly tuned by improving corrosion resistance of Mg-based materials. In addition to that, pH of the physiological solution, different ions present in the body, protein and its adsorption also affect the rate of degradation of Mg metals. Surrounding tissues, present in vicinity of implants, also take part in the corrosion process. It has been reported that the corrosion resistance of Mg metal can be improved by forming the composite material system. A composite with inert and biocompatible reinforcement phase could be a better option to tailor the degradation behaviour of Mg materials. Inert nature of ceramic materials in physiological environment authenticates them as better reinforcement for Mg-based system. Furthermore, Mg–HA-based composite system forms continuous precipitation of the bone-like apatite because of homoepitaxial nature of HA. Apparently, as time span increases when Mg–HA composite is exposed to simulated body fluid, the process of dissolution of apatite layer starts. Moreover, formation and dissolution of apatite layers lead to mass gain and mass loss of Mg–HA-based composite. Thus, reaction kinetics (Eqs. 1, 23, 4, 5, 6 and 7) explain the mechanism behind the Mg–HA degradation in simulated body fluid. Consequently, substantial in-vitro biodegradation experiments have been carried out to simulate the real in-vivo degradation behaviour of Mg-based biodegradable metallic implants.
The formation of the new apatite layer was described with the following equations55:
The dissolution reaction of apatite can be described by Eqs. (6) and (7) as follows97:
4.1.1 Evaluation of the Corrosion of Mg-Based Biomaterials
High complexity of corrosion process in physiological solutions, due to the presence of aggressive environment, like, higher amount of salts, sugar, proteins, inhibits the wide interest of many research groups to explore the potential of Mg metal for orthopaedic application. Physiological environment is so important because this environment has a considerable influence on degradation behaviour of various materials. Selection of a more relevant physiological solution is of utmost important to evaluate corrosion rate of Mg-based implants, as it should offer the closest approximation for in-vivo conditions. To develop the smart material for orthopaedic application, and to evaluate their proper bio corrosion properties, several methods are available to quantify the corrosion rate in physiological environment. Potentiodynamic polarization test, i.e. accelerated corrosion test, cyclic polarization and in-vitro immersion studies for longer duration (depending on the time required for respective bone healing) are popular experiments to measure the corrosion properties of Mg-based implants.
4.1.1.1 Electrochemical Study
Potentiodynamic polarization tests are carried out by several research groups to determine the corrosion resistance of the Mg–HA-based composite materials system.29, 62, 69 It is a convenient and simple technique to measure the corrosion resistance by testing the OCP (open circuit potential), polarization curve via three electrode system. Scanning rate of tests also plays an important role, because it balances the steady state approximation. Ultimate aim of adding the HA in Mg matrix is to improve the corrosion resistance of the system. Table 1 represents several studies of accelerated corrosion test performed on the Mg–HA-based composite system. Different kinds of physiological solutions used in the experiments are also mentioned in Table 1. It has been observed that addition of HA in Mg-based matrix has significantly improved the corrosion resistance of the materials. In addition to this, the fabrication process involved in the development of composite also affects the corrosion rate of the materials.
4.1.1.2 Immersion Test
Immersion test in physiological solution (e.g. SBF, PBS etc.) at body temperature (~ 37 °C) is a standard method to assess the corrosion properties of biodegradable Mg–HA-based composites. ISO 10993—15 (Biological evaluation of medical devices-Part 15: Identification and quantification of degradation products from metals and alloys), and ASTM G31-7 (standard protocol for immersion test of metallic materials) are testing standards to perform the immersion studies in physiological solutions.82 According to the ISO 10993-15, immersion test vials should be tightly closed during the experiments to avoid the evaporation and stored in a constant temperature (37 °C) environment. There are many important factors, like, the ratio of solution volume-to-sample surface area (V/A), time duration of immersion study, the flow rate of the solution in case of dynamic immersion studies and several methods to evaluate degradation rate affect the final degradation behaviour of materials.
To avoid any severe change in the degradation behaviour of samples, due to the exhaustion of corrosive constituents or corrosion products accumulation during immersion testing, ASTM G31-72 recommends the standard solution volume is of 20 mL/cm2 and 40 mL/cm2 to perform test. Researchers have studied the effect of V/A ratio on materials’ degradation rate by varying the ratio from 0.67 mL/cm2 to 6.7 mL/cm2. It has been seen that, low ratio of V/A led to a high pH of the solution, which influence the corrosion rate. However, in case of high ratio of V/A, such as 6.7, the effect was negligible. In addition to that, the selection of the physiological solution and the V/A ratio, based on the required bio environment, is a very important parameter to predict the degradation behaviour of these composites in service condition. It was suggested that a high V/A ratio, such as 6.7, and a low V/A ratio, such as 0.67, should be selected to simulate the V/A ratio should be considered in terms their clinically relevance.
In general, based on the state of physiological solution, immersion test can be classified into two types: static immersion and dynamic immersion. In the case of static immersion test, the samples are dipped in the immobile physiological solution, while in the case of dynamic immersion test, the solution is in the flowing condition. It has been observed that several available studies on immersion testing have adopted static immersion method to evaluate the degradation behaviour of metallic materials.29, 34, 35, 40, 52, 54, 55 But, at the same time, some outcomes show that in-vitro degradation data cannot predict the in-vivo degradation behaviour.93 Therefore, several dynamic equipment have been invented for better simulation of the in-vivo environment. It has been recommended that future immersion experiments for blood contacting implants should use more physiologically accurate test systems by mimicking the real body fluids. One of the dynamic immersion studies on degradation behaviour of pure Mg in 0.6% NaCl solution under multiple rotation speed (1, 120, 1440 r/min) has reported that the flowing of physiological solution during immersion tests accelerates the degradation rate by reducing the deposition of apatite layers on the surfaces.82 So, the flow rate of the physiological solution should be managed properly during dynamic immersion tests, depending on the physiological condition of the implanted part of the body. Table 2 shows the comprehensive study of Mg–HA composites in in-vitro degradation in different physiological solution. Effect of various compositions of HA reinforcement in Mg-based composites can be clearly seen through the Table 2.
4.1.1.3 Mg2+ Ions Release
To evaluate the concentration of Mg2+ ions’ release from the retrieved immersion solution, atomic absorption spectroscopy (AAS) or inductively coupled plasma-mass spectroscopy (ICP-MS) tests have been performed. In one of the study, addition of 5 wt% HA in Mg–3Zn matrix has significantly improved corrosion resistance. Due to the increased corrosion resistance, the release of Mg2+ ion is comparatively lower.29
It is interesting to know that orthopaedic implants operate in the protein containing physiological solution. Human blood plasma contains three different types of dissolved proteins, namely, albumin, globulins and fibrinogen. Following implantation, protein adsorption is the first in the series of events to follow at the material–tissue interface.95 Thus, the use of SBF as a physiological solution for immersion studies would not properly mimic real picture of the degradation behaviour of Mg–HA-based composites. To mimic the real physiological environment for Mg–HA-based composites, the authors group has developed a modified physiological solution, which is a mixture of fetal bovine serum (FBS) and SBF in a specific composition based on the composition of real body fluids. It has been observed that, Mg-based composite showed ~ 67% better corrosion resistance in modified solution as compared to SBF.52, 54 So, the degradation behaviour of Mg–HA-based implants will mainly depend on the type of solution used for immersion studies.
4.2 Degradation Rate with Respect to Mechanical Properties
The previous studies of in vitro experiments have revealed the potential capacity of Mg/HA composites for biodegradable metallic orthopedic implants (Satish 2018).34, 35, 40, 94 Generally, these implants fail in load-bearing application due to loss of its mechanical integrity. Moreover, when Mg–HA composites are synthesized in the forms of plates, screws and pins, it becomes important that these bone-fixation devices have enough strength until the healing of bone tissues and regain their mechanical integrity. Addition of HA in Mg matrix has the possibility to tailor the degradation behaviour and enhance the bioactivity of composites. However, the issues related to the evolution of mechanical behaviour of such composites, during degradation, have not been addressed yet. To evaluate the potential of Mg–HA composites in orthopaedic accessories, it is important to understand the mechanical integrity subjected to in vitro immersion in simulated body condition. This assessment provides insight on the length of period the implants are going to withstand the stress and if that is enough for complete healing and tissue formation.
Until now, only our group has reported the mechanical integrity of Mg–HA composite during in-vitro exposure in simulated body fluid.52, 54 Reports showed Mg–3Zn and Mg–3Zn–5HA composites have retained ~ 34 and 66% of ultimate compressive strength after 3 days of immersion. Figure 11 reveals the stress–strain plot of Mg–3Zn/HA composites after the immersion in SBF for different periods. The focus of this study was to have an insight of mechanical integrity of such material in service condition (SBF). Addition of 5 wt% HA in Mg–3Zn matrix enhanced the degradation resistance, which in turn maintained the mechanical integrity of composites even after immersion.
4.3 Biocompatibility
There is a possibility of local pH change in the vicinity of Mg–HA implant environment, due to the alkaline nature of the degraded product. Several times, in case of drastic change, the local shooting of pH severely damages the cell proliferation, differentiation and viability on the interface of orthopaedic implants and consequently induces chronic tissue inflammatory reactions and blood clots.96 To develop ideal Mg–HA composites for orthopaedic implants, biocompatibility is a critical property to be evaluated thoroughly. Incorporation of HA in the Mg-based matrix is a better strategy to improve the biocompatibity of implants for orthopaedic application. Due to the exceptionally high biocompatibility of HA, the Mg–HA-based composite can offer better biocompatibility at the time of bone healing, than Mg itself. To develop significantly biocompatible material system, Witte et al. synthesized a metal matrix composite by adding 20 wt% of HA in AZ91D matrix. To check the biocompatibility of AZ91D-20HA composite, cytocompatibility tests were performed. MTT assay data have shown that macrophages, osteoblasts and human bone-derived cells adhere, proliferate and survive on the synthesized AZ91D-20HA composites in a cell culture system.83 The incorporation of HA into the AZ91D matrix increased the corrosion resistance, slowed down the pH-increase and improved the cell viability for HBDC, MG63, and RAW 264.7.83 However, AZ91D-20HA composite cannot be accepted in orthopaedic applications, considering the risk of long-term toxicity due to the release of Al ions during degradation. Presence of high content of Al ions in the human body can cause the Alzheimer’s disease.29 In another study, Ye et al. synthesized Mg–Zn–Zr/nHA composite and performed in-vitro cell experiments. The growth of osteoblasts on the composite surface was evaluated after incubation for 1, 3, 5 and 7 days.66, 84 The cell density of osteoblasts was found greater on Mg–Zn–Zr/nHA composites, as compared to Mg–Zn–Zr composite for all designated incubation times. It can be concluded that the osteoblasts, cultured with Mg–Zn–Zr/nHA composite, have a much higher activity rate than Mg–Zn–Zr composite.66, 84 Figure 12 reveals the cell density of osteoblasts cultured on the both composites for various time periods. In another study, cytotoxicity tests were performed to evaluate the biocompatibility of Mg/HA (10, 20, 30 wt%) composite, synthesized by powder processing route.48, 51 Cytotoxicity data indicated that extraction medium of Mg–10HA composite does not induce any toxicity to L-929 cells, while extraction medium from Mg–20HA and Mg–30HA composites reduced cell viability significantly (Fig. 13).48, 51 A comparatively high degradation rate of Mg–20HA and Mg–30HA composites, as compared to Mg–10HA, causes higher change in the pH value of extraction medium. So, the cell viability of these composites is comparatively less.
Ratna Sunil et al. have performed MTT assay to evaluate the rat skeleton muscle (L6) cell viability on HA-reinforced AZ91 metal matrix composite, fabricated via friction stir processing (Ratna Sunil et al. 34, 35, 40). The results indicated no toxicity for all the composites. However, cell adhesion was comparatively higher for composites having HA as reinforcement.34, 35, 40 Figure 14 presents the SEM micrographs of the L6 cells on the composites incubated for 24 h, having standard polystyrene tissue culture plate as control substrate.
Jaiswal et al.29 have synthesized Mg–3Zn/HA composite, having various contents of HA (0, 2, 5, 10 wt%) and performed biocompatibility tests in terms of cell adhesion and cell viability. Mg–3Zn/5HA composites have shown better cell-adhesion properties due to the homogeneous distribution of HA inside the Mg–3Zn matrix. Figure 15 presents the fluorescence images of the cell adhered on the various composites.
Fluorescence images of hFOB cells adhered on different composites a control, b Mg–3Zn, c Mg–3Zn–5HA and d Mg–3Zn–10HA surfaces29.
Higher number of cells were attached with the composites having HA as nano filler. These studies prove that the addition of HA as a reinforcement helps in the enhancement of biocompatibility.
5 Concluding Remarks
There is significant promise for Mg–HA composites in the field of orthopaedic fracture fixing accessories. Tailoring the degradation rate, along with retention of mechanical integrity of Mg–HA composites, has been a great challenge. However, the use of Mg–HA-based composite for temporary orthopaedic field is limited due to the constraints in controlling the degradation rate of Mg–HA-based composites. HA presence on the Mg–HA composites’ surfaces accelerates the epitaxial precipitation of apatite layers as compared to pure Mg on exposed surfaces of targeted composites under body environment. These apatite layers shield the exposed surfaces from degradation and retain the mechanical integrity. Two main factors are crucial for the success of Mg-based composites. First one involves the standardized protocols to be followed for both biodegradation and biocompatibility experiments. This will allow the comparison of materials between the groups of experiments. This will further help in generating a vast volume of comparable data to give a thorough and comprehensive understanding of the subject. Second, further development in this orthopaedic field required clinical investigation of these material systems developed, which is still lacking. Achieving these two will secure the future of Mg–HA-based composites as orthopaedic fracture-fixing accessories.
6 Future Perspectives
The review of literature shows the demand of the research in Mg–HA system for orthopaedic applications. The effect of HA as reinforcement to strengthen the Mg matrix and controlling the degradation rate along with the biocompatibility has been the focused; though optimized wt% of HA still remains debatable. Several powder-processing routes have been used for consolidation of Mg–HA composites, out of which SPS was found to be the most promising one. HA reinforcement is effective in improving the compressive strength, hardness, elastic modulus, and degradation behaviour of the Mg–HA composite. Uniform dispersion of HA in Mg matrix is crucial for degradation rate and mechanical strengthening of the Mg–HA composite system. Mostly, studies have shown the positive influence of HA reinforcement on the Mg–HA composite. Biocompatibility and in-vitro assessment of Mg–HA composite have been reported in number of studies. But the in-vivo aspect of composite is rarely investigated. Critical observations are mentioned in point-wise manner below, which can assist in future development and successful use of Mg–HA composite system for clinical trials in orthopaedics.
-
Knowledge of Mg–HA interface is vital in determining the mechanical behaviour of composite system. But, there is insufficient information available on Mg–HA interface. Therefore, more research is required in this area to understand the concept of the interface and bond strength between magnesium and HA, as a function of different consolidation and processing techniques. Such knowledge would recommend the best techniques for processing of composite and better understanding about tailoring the mechanical property and degradation rate.
-
In-vitro assessment of Mg–HA composite for ideal orthopaedic implant needs better representative body fluids for immersion study as our body fluids contain organic, proteins and many other elements. In addition to that, exposure of right area of implants to medium depends on the exact anatomical location of implantation. Better mimicking of body environment is prerequisite for developing ideal Mg–HA-based implants. However, present studies do not really focus in this aspect.
-
Biocompatibility studies, which were performed on Mg–HA composite surface by incubating bone cells, prove the biocompatible nature of Mg–HA composite in terms of cell viability, cell proliferation and cell differentiation. But only one study was carried out on protein adsorption characteristics of Mg–HA composites. Thorough investigation of protein profile is needed on Mg–HA surface for the further confirmation of biocompatibility of Mg–HA composites and understanding of cell interaction with them, before going for clinical trials.
-
These studies on Mg–HA composite system have made a great progress in materials innovation and preclinical tests. The bottleneck is their translation from research to clinical application. Besides the optimized composition of HA in Mg and processing route to control the degradation rate, a constructive clinical investigation of these material systems is mandatory to translate these materials to industry.
This knowledge gap will be a roadmap for future research, which will determine the potential of Mg–HA composite for orthopaedic application.
References
Hill G et al (2010) Benefits and associated risks of using allograft, autograft and synthetic bone fusion material for patients and service providers—a systematic review. JBI Libr Syst Rev 8:1–13
Moussy F et al (2010) Biomaterials for the developing world. J. Biomed. Mater. Res. A 94:1001–1003
Stumpf CP et al (2013) Biomaterials in dental ceramics, topics in mining, metallurgy and materials engineering. Springer, Berlin, pp 9–13
Zheng YF, Gu XN, Witte F et al (2014) Biodegradable metals. Mater Sci Eng, R 77:1–34
Katti S, Lakshmi IR, Laurecin CT et al (2002) Toxicity biodegradation and elimination of polyanhydrides. Adv Drug Deliv Rev 54:933–961
Vert M, Maudtui J, Li S et al (1994) Biodegradation of PLA/PGA polymers: increasing complexity. Biomaterials 15:1209–1213
Cai X, Tong H, Hu J et al (2009) Preparation and characterization of homogeneous chitosan–polylactic acid/hydroxyapatite nanocomposite for bone tissue engineering and evaluation of its mechanical properties. Acta Biomater 5:2693–2703
EdiTanase C et al (2014) PLA/chitosan/keratin composites for biomedical applications. Mater Sci Eng, C 40:242–247
Park SY et al (2010) Electrospun silk fibroin scaffolds with macropores for bone regeneration: an in vitro and in vivo study. Tissue Eng Part A 16:1271–1279
Mieszawska AJ et al (2011) Clay enriched silk biomaterials for bone formation. Acta Biomater 7:3036–3041
Wang Y et al (2008) In vivo degradation of three-dimensional silk fibroin scaffolds. Biomaterials 9(3):415–428
Bhattacharjee P et al (2017) Silk scaffolds in bone tissue engineering An overview. Acta Biomater 63:1–17
Terasaka S, Iwasaki Y, Uchida T et al (2006) Fibrin glue and polyglycolic acid non woven fabric as a biocompatible dural substitute. Neurosurgery 58:134–139
Witte F, Hort N, Kainer KU et al (2008) Degradable biomaterials based on magnesium corrosion. Curr Opin Solid State Mater Sci 12:63–72
Sáenz A, Rivera-Muñoz EW, Castaño VM et al (1991) Ceramic biomaterials: an introductory overview. J Mater Educ 21:297–306
Khanra AK, Jung HC, Hong KS, Shin KS et al (2010) Microstructure and mechanical properties of Mg–HAP composites. Bull Mater Sci 33:43–47
Hee Kim Y, Jyoti MA, Youn M Ho, Sun Youn H, Seok Seo H et al (2010) In vitro and in vivo evaluation of a macro porous β-TCP granule-shaped bone substitute fabricated by the fibrous monolithic process. Biomed Mater 5:359–366
Gu YW, Loha NH, Tor SB, Cheang P et al (2002) Spark plasma sintering of hydroxyapatite powders. Biomaterials 23:37–43
White AA et al (2007) Hydroxyapatite–carbon nanotube composites for biomedical applications: a review. Int J Appl Ceram Technol 4:1–13
Yu LG, Khor KA, Cheang P et al (2003) Effect of spark plasma sintering on the microstructure and in vitro behavior of plasma sprayed HA coatings. Biomaterials 24:2695–2705
Hench LL et al (2002) Third-generation biomedical materials. Science 295:1014–1017
Xu W et al (2018) Accelerated corrosion of 316L stainless steel in simulated body fluids in the presence of H2O2 and albumin. Mater Sci Eng C 92:11–19
Sivakumar M, Dhanadurai KS, Thulasiraman V et al (1995) Failures in stainless steel orthopaedic implant devices: a survey. J Mater Sci Lett 14:351–354
Gonzalez-Carrasco JL et al (2009) Metals as bone repair materials. In: Planell JA, Best SM, Lacroix D, Merolli A (eds) Bone repair biomaterials. Woodhead Publishing, pp 154–193
Chen Q et al (2015) Metallic implant biomaterials. Mater Sci Eng R 87:1–57
Stohs SJ et al (1995) Oxidative mechanisms in the toxicity of metal ions. Free Radical Biol Med 18:321–336
Manam NS, Harun, Shri DNA et al (2017) Study of corrosion in biocompatible metals for implants: a review. J Alloys Compound 701:698–715
Jaiswal S, Manoj Kumara R, Roy P, Lahiri D et al (2018) Mechanical, corrosion and biocompatibility behaviour of Mg–3Zn–HA biodegradable composites for orthopaedic fixture accessories. J Mech Behav Biomed Mater 78:442–454
Rahim MI et al (2018) Advances and challenges of biodegradable implant materials with a focus on magnesium-alloys and bacterial infections. Metals 8:532
Pierson D et al (2012) A simplified in vivo approach for evaluating the bioabsorbable behaviour of candidate stent materials. J Biomed Mater Res B 100B:58–67
Staiger MP, Pietak AM, Dias G et al (2006) Magnesium and its alloys as orthopedic biomaterials: a review. Biomaterials 27:1728–1736
Waizy H, Reifenrath J, Windhagen H et al (2013) Biodegradable magnesium implants for orthopedic applications. J Mater Sci 48:39–50
Ratna Sunil B, Sampath Kumar TS, Nandakumar V et al (2014) Nano-hydroxyapatite reinforced AZ31 magnesium alloy by friction stir processing: a solid state processing for biodegradable metal matrix composites. J Mater Sci Mater Med 25:975–988
Ratna Sunil B, Sampath Kumar TS, Nandakumar V et al (2014) Friction stir processing of magnesium–nanohydroxyapatite composites with controlled in vitro degradation behavior. Mater Sci Eng C 39:315–324
Witte F, Fischer J, Crostack HA, Kaese, Beckmann F, Windhagen H et al (2006) In vitro and in vivo corrosion measurements of magnesium alloys. Biomaterials 27(7):1013–1018
Wang J, Xu W, Liu L Qin et al (2016) Biodegradable magnesium (Mg) implantation does not impose related metabolic disorders in rats with chronic renal failure. Sci Rep 6:26341
Lambotte L (1932) Utilisation of magnesium comme materiel perdu dans l’osteosynthèse. Bull Mem Soc Nat Chir 28:1325–1334
McBride ED (1938) Absorbable metal in bone surgery. J Am Med 111:2464–2467
Ratna Sunil B, Sampath Kumar TS et al (2014) Processing and mechanical behavior of lamellar structured degradable magnesium–hydroxyapatite implants. J Mech Behav Biomed Mater 40:178–189
Ahmadkhaniha D, Fedel M, Sohi A, Deflorian F et al (2016) Corrosion behavior of magnesium and magnesium–hydroxyapatite composite fabricated by friction stir processing in dulbecco’s phosphate buffered saline. Corros Sci 104:319–329
Wang X, Dong LH, Li XL, Ma XL, Zheng YF et al (2013) Microstructure, mechanical property and corrosion behavior of interpenetrating (HA+β-TCP)/MgCa composite fabricated by suction casting. Mater Sci Eng, C 33:4266–4273
Sawada K, Ika KF, Zasshi D et al (1998) 107(2):237–250
Kawatani H, Fukumoto K, Zairyo S et al (1994) 12(3):119–126
Khanra AK, Jung HC, Shin KS et al (2010) Comparative property study on extruded Mg–HAP and ZM61–HAP composites. Mater Sci Eng, A 527:6283–6288
Chen B, Yin KY, Lu TF, Sun BY, Zheng JX et al (2016) AZ91 magnesium alloy/porous hydroxyapatite composite for potential application in bone repair. J Mater Sci Technol 32:858–864
Haghshenas M et al (2017) Mechanical characteristics of biodegradable magnesium matrix composites: a review. J Magn Alloys 5(2):189–201
Gu X, Zhou W, Zheng Y, Xi Y, Chai D et al (2010) Microstructure, mechanical property, bio-corrosion and cytotoxicity evaluations of Mg/HA composites. Mater Sci Eng, C 30:827–832
Zhao J, Yu Z, Chen L et al (2011) Biodegradable behaviors of Mg–6%Zn–5% Hydroxyapatite biomaterial. Adv Mater Res 239–242:1287–1291
Sun J, Chen M, Cao G, Wei J et al (2013) The effect of nano-hydroxyapatite on the microstructure and properties of Mg–3Zn–0.5Zr alloy. J Compo Mater 48:825–834
Gu X, Zhou W, Zheng Y, Xi Y, Chai D et al (2010) Microstructure, mechanical property, bio-corrosion and cytotoxicity evaluations of Mg/HA composites. Mater Sci Eng C 30:827–832
Dubey A et al (2019) Mechanical integrity of biodegradable Mg–HA composite during in-vitro exposure. J Mater Eng Perform 8(2):800–809
Liu DB et al (2010) Fabrication and corrosion behavior of HA/Mg–Zn biocomposites. Front Mater Sci Chin 4:139–144
Dubey A, Jaiswal S, Roy P, Lahiri D et al (2019) Protein adsorption and biodegradation behaviour of Mg–3Zn/HA for biomedical application. Nanomater Energy 8:1–10
Salleh EM, Zuhailawati H, Noor M, Othman NK et al (2018) In vitro biodegradation and mechanical properties of Mg–Zn alloy and Mg–Zn–Hydroxyapatite composite produced by mechanical alloying for potential application in bone repair. Metall Mater Trans A 49:5888–5903
Guo P, Cui Z, Cheng L, WenxianWang W, Xu B et al (2016) Preparation of Mg/Nano-HA composites by spark plasma sintering method and evaluation of different milling time effects on their microhardness, corrosion resistance, and biocompatibility. Adv Eng Materals 19(1):1600294
Kim KR, Ahn JW, Han JH, Roh JS, Kim WJ, Kim HS et al (2014) Corrosion behavior of magnesium powder fabricated by high-energy ball milling and spark plasma sintering. Metall Mater Int 20(6):1095–1101
Azrina WN, Muhammada W, Mutohd Y, YukioMiyashitad Y et al (2011) Microstructure and mechanical properties of magnesium composites prepared by spark plasma sintering technology. J Alloy Compd 509:6021–6029
Viswanathan R, Rameshbabu N, Sreekanth D, Venkateswarlu K, Rani S, Muthupandi V et al (2013) Plasma electrolytic oxidation and characterization of spark plasma sintered magnesium/hydroxyapatite composites). Mater Sci Forum 765:827–831
Prakash C, Singh S, Mia M, Królczyk G, Khanna N et al (2018) Synthesis, characterization, corrosion resistance and in-vitro bioactivity behavior of biodegradable Mg–Zn–Mn–(Si–HA) composite for orthopaedic applications. Materials 111602
Prakash C, Sidhu S, Verma K, Sigh S et al (2018) Synthesis and characterization of Mg–Zn–Mn–HA composite by spark plasma sintering process for orthopedic applications. Vacuum 155:578–584
Campoa RD, Savoini B, Mongea MA, Garce´s G et al (2014) Mechanical properties and corrosion behavior of Mg–HAP composites. J Mech Behav Biomed Mater 39:238–246
Brown A, Zaky S, Sfeir C et al (2015) Porous magnesium/PLGA composite scaffolds for enhanced bone regeneration following tooth extraction. Acta Biomater 11:543–553
Liu Y, Liu D et al (2014) Corrosion properties of compositematerials HA (beta-TCP)/Mg–Zn–Ca. Rare Metal Mater Eng 43(1):205–209
Bansal S, Chauhan V, Juyal A, Raghuvanshi S et al (2009) Evaluation of hydroxyapatite and beta-tricalcium phosphate mixed with bone marrow aspirate as a bone graft substitute for posterolateral spinal fusion. Indian J Orthopaed 43:234–239
Ye X, Chen M et al (2010) In vitro corrosion resistance and cytocompatibility of nano-hydroxyapatite reinforced Mg–Zn–Zr composites. J Mater Sci Mater Med 21:1321–1328
Sun M, Chen G, Liu B, Wei J et al (2013) The effect of nano-hydroxyapatite on the microstructure and properties of Mg–3Zn–0.5Zr alloy. J Compos Mater 48:825–834
Champion E et al (2013) Sintering of calcium phosphate bioceramics. Acta Biomater 9:5855–5875
Kutty MG, Bhaduri SB, Yaghoubi A et al (2015) In situ measurement of shrinkage and temperature profile in microwave-and conventionally-sintered hydroxyapatite bioceramic. Mater Lett 161:375–378
Xiong G, Nie Y, Li J, Zhu Y, Li W et al (2016) Characterization of biomedical hydroxyapatite/magnesium composites prepared by powder metallurgy assisted with microwave sintering. Curr Appl Phys 16:830–836
Ma C, Chen L, Xu J, Frank E, Neil P, Duffie A, Zheng J, Li X et al (2013) Biodegradability and mechanical performance of hydroxyapatite reinforced magnesium matrix nanocomposites. Suppl Proc Vol 1 Mater Process Interfaces 120124
Ma C, Chen L, Xu J, Fehrenbacher A, Zheng J, Li X et al (2013) Effect of fabrication and processing technology on the biodegradability of magnesium nanocomposites. J Biomed Mater Res B Appl Biomater 101B
Li K, Zhao Y et al (2019) Research status and prospect of friction stir processing technology. Coatings 9:2–14
Khalil A, Sherif ME et al (2011) Corrosion passivation in simulated body fluid of magnesium/hydroxyapatite nanocomposites sintered by high frequency induction heating. Int J Electrochem Sci 6:6184–6199
Khalil A, Sherif ME et al (2012) Effect of high-frequency induction heat sintering conditions on the microstructure and mechanical properties of nanostructured magnesium/hydroxyapatite nanocomposites. Mater Des 36:58–68
Xu L, Pan F, Yang L, Zhang E, Yang K et al (2009) In vitro and in vivo evaluation of the surface bioactivity of a calcium phosphate coated magnesium alloy. Biomaterials 30:1512–1523
Chen B, Yin KY, Dong Q, Zheng JX, Lu C, Li ZC et al (2016) AZ91 magnesium alloy/porous hydroxyapatite composite for potential application in bone repair. J Mater Sci Technol 32:858–864
Kowalski K, Nowak M, Jurczyk M et al (2016) The effects of hydroxyapatite addition on the properties of the mechanically alloyed and sintered Mg–RE–Zr Alloy. 25:4469–4477
Pramanik S, Agarwal AK et al (2005) Development of high strength hydroxyapatite for hard tissue replacement. Trends Biomater Artif Organs 19:46–51
Saravanan RA, Surappa MK et al (2000) Fabrication and characterization of pure magnesium-30 vol% SiC particle composite. Mater Sci Eng A 276:108–116
Witte F, Kaese V, Switzer E, Lindenberg A, Wirth M, Windhagen H et al (2005) In vivo corrosion of magnesium alloys and the associated bone response. Biomaterials 26(17):3557–3563
Song G et al (2007) Control of biodegradation of biocompatible magnesium alloys. Corros Sci 49:1696–1701
Witte F, Feyerabend F, Fischer J, Blawert C, Dietzel W, Hort N et al (2007) Biodegradable magnesium–hydroxyapatite metal matrix composites. Biomaterials 28:2163–2174
Ye X, Chen M, Liu D et al (2010) In vitro corrosion resistance and cytocompatibility of nano-hydroxyapatite reinforced Mg–Zn–Zr composites. Journal of. Mater Sci Mater Med 21:1321–1328
Chiu C, Lu C, Ou KL et al (2017) Effect of hydroxyapatite on the mechanical properties and corrosion behavior of Mg–Zn–Y Alloy. Materials 10:855
Khalajabadia SZ, Abdul Kadira MR, Bakhsheshi HR, Farahany S et al (2014) Effect of mechanical alloying on the phase evolution, microstructure and bio-corrosion properties of a Mg/HA/TiO2/MgO nanocomposite. Ceram Int 40:16743–16759
Lia JX, Zhanga Y, Xie JX et al (2018) Effect of trace HA on microstructure, mechanical properties and corrosion behavior of Mg–2Zn–0.5Sr alloy. J Mater Sci Technol 34:299–310
Aboudzadeh N, Ali SM et al (2018) In vitro degradation and cytotoxicity of Mg − 5Zn − 0.3Ca/nHA biocomposites prepared by powder metallurgy. Trans Nonferrous Metall Soc China 28:1745–1754
Gill P et al (2012) Characterization and degradation behaviour of anodized magnesium-hydroxyapatite metal matrix composites. J Biomimetics Biomater Tissue Eng 16:55–69
Ma C, Chen L, Zheng J et al (2013) Effect of fabrication and processing technology on the biodegradability of magnesium nanocomposites. J Biomed Mater Res Part B 101:870–877
Nakka K, Chikkala N, Buradagunta S et al (2018) Developing composites of ZE41 Mg alloy-naturally derived hydroxyapatite by friction stir processing: investigating in vitro degradation behavior. Mater Technol 33:603–611
Ramya M, Pillai MM, Raj B, Ravi KR et al (2018) Hydroxyapatite particle (HAp) reinforced biodegradable Mg–Zn–Ca metallic glass composite for bio-implant applications. Biomed Phys Eng Express 4:25–39
Bohner M, Lemaitre J et al (2009) Can bioactivity be tested in vitro with SBF solution? Biomaterials 30:2175–2179
Zhao J, Yu MZ, Chen LJ et al (2011) Biodegradable behaviors of Mg–6%Zn–5% hydroxyapatite biomaterial. Adv Mater Res 239–242:1287–1291
Collier T, Jenney CR, Anderson JM et al (1997) Protein adsorption on chemically modified surfaces. Biomed Sci Instrum 33:178–183
Seal CK, Vince K, Hodgson MA et al (2009) Biodegradable surgical implants based on magnesium alloys- a review of current research. IOP Conf Ser Mater Sci Eng 4:06–011
Oliva J, Cama J, Cortina JL, Ayora C, De Pablo J et al (2012) Biogenic hydroxyapatite (Apatite II™) dissolution kinetics and metal removal from acid mine drainage. J Hazard Mater 213:7–18
Acknowledgements
The authors are thankful to Ms. Swati Haldar from Centre of Nanotechnology of Indian Institute of Technology Roorkee, for her help and support in understanding of biological studies. D.L. acknowledges funding from the Department of Science and Technology, India (SB/SO/HS/138/2013). The figures from other articles have been reproduced in this review with permission from the respective publishers and the appropriate citation is mentioned using reference numbers in figure captions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jaiswal, S., Dubey, A. & Lahiri, D. In Vitro Biodegradation and Biocompatibility of Mg–HA-Based Composites for Orthopaedic Applications: A Review. J Indian Inst Sci 99, 303–327 (2019). https://doi.org/10.1007/s41745-019-00124-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41745-019-00124-w