Abstract
Purpose
To report a predictable minimally invasive treatment approach for a gummy smile patient by using laser-assisted guided gingivectomy and lip repositioning.
Background
Excessive gingival display is one of the most common esthetic concerns that might affect the patient’s psychology and social life, especially in young age. For a long time, orthognathic surgery was recommended in spite of its high morbidity. Lip repositioning was the treatment of choice for many patients as it was effective for the reduction of gingival display, a safe and less invasive procedure. Although, due to the multifactorial origin of gummy smile, combined treatment protocols are usually required. Besides, the patients demand reduced pain following procedures as well as predictable outcomes.
Case report
A 20-year-old male patient was requesting a treatment for his gummy smile. Upon examination, 7-mm gingival display was reported with a multifactorial origin. A 3D-printed computerized gingivectomy guide was fabricated based on the smile design for the patient by using the cone beam computed tomography, extraoral and intraoral photographs. A 940-nm diode laser in a continuous wave mode and with a power of 1.5 W was used for the gingivectomy and lip repositioning. The procedure was performed under local anesthesia with no bleeding or post-operative complications reported.
Conclusion
The combined treatment approach by using computer-guided gingivectomy and lip repositioning by using 940 diode laser was effective to provide predictable outcomes for treatment of gummy smile with minimal bleeding, uneventful healing, and minimal postoperative pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Smile esthetics is directly related to facial attractiveness. Any developmental or acquired condition that negatively affects the smile results in patient dissatisfaction [1]. One of the most prevalent esthetic issues among patients is excessive gingival display (EGD), sometimes known as a “gummy smile” which is defined as more than 3–4 mm of the gingiva visible during smiling [2]. Excessive gingival display occurs in 10.5 to 29% of young adults, with a higher incidence in females [3]. The etiology of excessive gingival display is multifactorial. It might be skeletal such as vertical maxillary excess (VME) and maxillary protrusion; gingival as in gingival enlargement and altered passive eruption (APE); and muscular, such as hypermobile upper lip (HUL) and short lip length or a combination of 2 or more of these causes [2, 4].
Treatment modalities for excessive gingival display include orthodontic treatment, orthognathic surgery, esthetic crown lengthening, lip repositioning, and non-surgical procedures such as botulinum toxin A (Botox) injections, fat transplantation, and injection of hyaluronic acid (HA) fillers into the upper lip [4]. For maximum esthetic results, dental professionals must establish a correct diagnosis and an interdisciplinary treatment plan according to the underlying etiologic factors of the patient’s gummy smile [4].
Lip repositioning procedure was reported to be an effective treatment modality for patients with gummy smiles with a hypermobile lip etiology or mild vertical maxillary excess [1, 2, 5]. It was first described as part of medical plastic surgery in the 1970s [6]. The procedure includes the removal of a strip of intraoral mucosa from the labial vestibule. The outline of this mucosal strip is the mucogingival junction coronally, a line parallel to it apically and to the labial commissures during smiling laterally then suturing of the apical incision line coronally to the mucogingival junction incision [7]. Lip repositioning is a conservative surgical technique that provides a less invasive and safer approach than orthognathic surgery for the treatment of gummy smiles. Lip repositioning surgery results in the reduction of gummy smile through decreasing the vestibular depth, restriction of the muscle pull during smiling, and increasing the lip fullness [8].
Another procedure that is frequently performed in clinical practice to correct the appearance of a gummy smile is gingivectomy. Scalpels, burs, electrocautery, and other traditional surgical techniques for performing gingivectomy have shown significant drawbacks. Therefore, many studies concluded that using different types of lasers was preferred to the conventional surgical tools for performing gingivectomy procedures as it is less invasive, has more controllable cutting with no or minimal bleeding, uneventful healing, and more predictable results in comparison to the conventional surgical tool [9,10,11].
Since its introduction, CAD-CAM technology has aided numerous surgical operations by providing more accurate, predictable results that satisfy both medical professionals and patients. By utilizing the patient’s pictures and clinical and radiographic data, smile design software enables virtual visualization of the patient’s most esthetically pleasing, harmonious smile. Besides, using a 3D-printed gingivectomy guide was reported to be effective for accurate transfer of the approved smile design with minimal errors and easier and shorter procedure for the surgeon. As far as we know, there is a lack of the reported data about combining using laser and CAD/CAM technique for treatment of gummy smile in the same case. Therefore, the aim of this case report was to describe a laser-assisted combination treatment of lip repositioning and guided gingivectomy to decrease gummy smile [12, 13].
Clinical report
A 20-year-old male patient presented seeking treatment for his gummy smile. After history taking, there were no reported systemic diseases or medications that might cause gingival enlargement. For proper diagnosis of the patient’s gummy smile etiology, a series of extraoral and intraoral photographs in addition to a CBCT radiograph were taken for the patient in addition to the clinical examination. The patient’s upper lip was of a normal length (22 mm measured from the base of the nose to the lower border of the upper lip (mid-lip) at rest) excluding short lips. The patient was diagnosed with excessive gingival display (7 mm) that had a combined origin (Fig. 1). The patient had a hypermobile upper lip in addition to a mild vertical maxillary excess and mild gingival enlargement with no altered passive eruption. After the discussion of different treatment options with the patient, a combined treatment of laser-assisted guided gingivectomy and conservative lip repositioning was approved for treatment.
For guided gingivectomy, the patient’s full-face photos were exported to exocad software (exocad GmbH, Darmstadt, Germany). Considering the cemento-enamel junction position and the bone level from the CBCT, the proper smile design was chosen, and the gingivectomy surgical guide was designed accordingly (Fig. 2). The gingivectomy guide design was exported as a STL file and 3D-printed (Creality HALOT-SKY 3D Printer, China) (Fig. 2). One week before surgery, the patient’s teeth were scaled and polished, and the patient was instructed to follow a meticulous oral hygiene routine. At the surgery day and after administration of local anesthesia (4% articaine with 1:100,000 epinephrine), the gingivectomy guide was fixed in place (Fig. 3). Gingivectomy was performed by using diode laser 940 nm in a continuous wave mode and 1.5 W power by using an initiated E4 tip (Epic X, BIOLASE). After gingivectomy (Fig. 3), the outline of the mucosal band to be removed was marked by using the same diode laser but with lower power, 1 W in a continuous wave mode. The first incision line was parallel and 1 mm from the mucogingival line; the second incision was 12 mm apical to the first line and parallel to it. The incisions extended laterally and connected at the second premolar area. Then, mucosal band within the marked lines was removed in a partial thickness by using the same parameters used in gingivectomy (Fig. 4). The apical incision line was then approximated coronally and sutured at the muco-gingival line level by using continuous sutures (5–0 silk) with caution to maintain the position of the midline. The patient was prescribed ibuprofen 600 mg 3 times daily and 0.12% chlorhexidine mouth rinse without vigorous movements 3 times per day. He was instructed to apply ice packs at 20-min intervals for the first 24 h and to eat a soft diet during the first postoperative week. Besides, the patient was instructed to avoid any excessive movements of the lip during smiling and talking. The wound was checked 48 h postoperatively, and oral hygiene instructions were repeated. The sutures were removed 10 days postoperatively.
Results
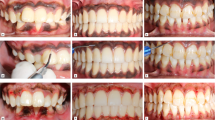
The procedure was relatively fast (20 min) with minimal bleeding and high patient satisfaction. On the day of surgery and the following day, the patient experienced minimal edema of the upper lip. In the second visit, 48 h after the procedure, the edema was resolved although the patient had minimal discomfort while eating and smiling which continued during the healing period while sutures were in place (Fig. 5). After removal of sutures, there was no pain. Complete healing was noted after 3 weeks with minimal gingival display (1 mm average gingival display) although the patient was still experiencing some tension at the surgery site while smiling (Fig. 6). The patient was followed up for 6 months; a scar line was observed upon upper lip retraction at surgery site, with average gingival display of 2.5 mm (4.5-mm reduction) from the original gum display and about 35% relapse from the original gum display of 7 mm (Fig. 7).
Discussion
The present report describes a combined treatment approach for the reduction of excessive gingival display by using laser-assisted lip repositioning and guided gingivectomy. The patient was diagnosed with excessive gingival display of 7 mm that is due to hypermobile lip, mild vertical maxillary excess, and slight gingival enlargement.
This is in agreement with Andijani et al. [3] as they reported hypermobile upper lip as the most prevalent cause (either solitary or combined with altered passive eruption) among patients seeking treatment for a gummy smile. They also considered 8 mm as the cutoff for hypermobile lip diagnosis [3].
Lip repositioning was used in this study as it was reported to be an effective less invasive treatment for excessive gingival display caused by hypermobile lip and mild vertical maxillary excess with an average reduction of 2.87 mm in the gingival display after 3 months from the procedure [1]. This is consistent with the present study’s outcome as a significant reduction in excessive gingival display was reported 3 weeks after the procedure. The average gingival display was 2.5 mm which is considered within the accepted range of normal smile gingival display [2].
Primary closure of the wound was applied to avoid possible infections, prolonged healing, irritation of the wound, and high contraction that might occur if the wound was left for secondary intention healing [14].
In the current report, guided gingivectomy was combined with lip repositioning. It was decided to use guided gingivectomy as it is more accurate, requires no measurements during the procedure, and provides more predictable results [12]. Besides, to avoid violation of the biological width, the measurements of the clinical crowns, along with the radiographic crown and bone level from the CBCT, were incorporated during the gingivectomy guide designing.
Diode laser was used for both the gingivectomy and lip repositioning as it is highly absorbed by hemoglobin and melanin which allows for easier manipulation of soft tissue. In addition, diode laser was reported to promote coagulation and prevents bleeding by sealing the blood vessels with minimal pain sensation during the procedures. This provides better visualization and spontaneous assessment of the operative area [9, 15, 16]. Despite the advantages of using a diode laser in oral mucosa surgeries, it has been reported to have delayed healing patterns in comparison to using conventional surgical scalpels [17].
A 35% of the original gum display relapse was recorded in our case after 6 months of follow-up, which is higher than the 25% documented relapse in Dos Santos et al.’s [1] systematic review study, despite the fact that all of the studies included in their evaluation had less pre-operative gingival display (4.31–6.36) than the current research (7 mm).
This increase in the relapse ratio in the current case is suggested to be owing to the multiple interrelated origins of the excessive gingival display. Injections of the botulinum toxin might have helped to achieve more stable results and reduce relapse, in our opinion, as excessive muscle pull is one of the major reasons of relapse. Other causes of relapse have been reported in the literature, such as removing a mucosal strap with insufficient width, performing the procedure in patients with minimal attached gingiva, and not following the postoperative instructions; however, they are not applicable in this case [5]. Furthermore, using the photobiomodulation therapy during the healing process might have helped for achieving better results, as using low-level laser therapy (LLLT) in periodontal surgeries has been reported to result in pain relief, inflammation reduction, significant wound healing promotion, increased gingival fibroblast proliferation, epithelialization enhancement, and increased collagen formation [14, 18]. This suggests that combining more treatment approaches with lip repositioning for more predictable and stable outcomes is recommended, which is in agreement with Dos Santos et al.’s recommendations [1].
Conclusion
The present report described an effective treatment protocol for excessive gingival display by combining laser-assisted guided gingivectomy and lip positioning. This approach provided a predictable, quick, and less painful technique for gummy smile treatment with satisfactory results for the patient.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Dos Santos-Pereira SA, Cicareli ÁJ, Idalgo FA, Nunes AG, Kassis EN, Castanha Henriques JF, Bellini-Pereira SA (2021) Effectiveness of lip repositioning surgeries in the treatment of excessive gingival display: a systematic review and meta-analysis. J Esthetic Restor Dent : Official Public Am Acad Esthetic Dentistry [et al] 33(3):446–457
Mendoza-Geng A, Gonzales-Medina K, Meza-Mauricio J, Muniz F, Vergara-Buenaventura A (2022) Clinical efficacy of lip repositioning technique and its modifications for the treatment of gummy smile: systematic review and meta-analysis. Clin Oral Investig 26(6):4243–4261
Andijani RI, Tatakis DN (2019) Hypermobile upper lip is highly prevalent among patients seeking treatment for gummy smile. J Periodontol 90(3):256–262
Polo M (2022) Gummy smile treatment: a 40-year journey. AJO-DO Clinical Companion 2(2):125–135
Dym H, Pierre R 2nd (2020) Diagnosis and treatment approaches to a “gummy smile.” Dent Clin North Am 64(2):341–349
Kostianovsky AS, Rubinstein AM (1976) The “unpleasant” smile. Aesthetic Plast Surg 1(1):161–166
Andijani RI, Paramitha V, Guo X, Deguchi T, Tatakis DN (2021) Lip repositioning surgery for gummy smile: 6-month clinical and radiographic lip dimensional changes. Clin Oral Invest 25(10):5907–5915
Faus-Matoses V, Faus-Matoses I, Jorques-Zafrilla A, Faus-Llácer VJ (2018) Lip repositioning technique A simple surgical procedure to improve the smile harmony. J Clin Exp Dent 10(4):e408–e412
Kazakova RT, Tomov GT, Kissov CK, Vlahova AP, Zlatev SC, Bachurska SY (2018) Histological gingival assessment after conventional and laser gingivectomy. Folia Med 60(4):610–616
Capodiferro S, Kazakova R (2022) Laser-assisted gingivectomy to treat gummy smile. Dent Clin North Am 66(3):399–417
Khamis M, Abdelrehim A (2019) Interdisciplinary management of a patient with a gummy smile. J Oral Maxillofacial Radiol 7(2):38–43
Liu X, Yu J, Zhou J, Tan J (2018) A digitally guided dual technique for both gingival and bone resection during crown lengthening surgery. J Prosthet Dent 119(3):345–349
Arias DM, Trushkowsky RD, Brea LM, David SB (2015) Treatment of the patient with gummy smile in conjunction with digital smile approach. Dent Clin North Am 59(3):703–716
Ebrahimi P, Hadilou M, Naserneysari F, Dolatabadi A, Tarzemany R, Vahed N, Nikniaz L, Fekrazad R, Gholami L (2021) Effect of photobiomodulation in secondary intention gingival wound healing-a systematic review and meta-analysis. BMC Oral Health 21(1):258
Mossaad AM, Abdelrahman MA, Kotb AM, Alolayan AB, Elsayed SA (2021) Gummy smile management using diode laser gingivectomy versus botulinum toxin injection - a prospective study. Annals of maxillofacial surgery 11(1):70–74
Abdelhafez RS, Rawabdeh RN, Alhabashneh RA (2022) The use of diode laser in esthetic crown lengthening: a randomized controlled clinical trial. Lasers Med Sci 37(5):2449–2455
Kim HR, Son K, Son YT, Kim YG, Lee KB, Lee SC, Suh JY, Lee JM (2022) A comparative immunohistochemical study of wound healing after dental diode laser treatment in the rat oral mucosa. Bioengineering (Basel, Switzerland) 9(9):466
Yildiz MS, Gunpinar S (2019) Free gingival graft adjunct with low-level laser therapy: a randomized placebo-controlled parallel group study. Clin Oral Invest 23(4):1845–1854
Acknowledgements
The authors would like to thank Egypt Smart Labs for the valuable assistance with the fabrication of the gingivectomy guide.
Author information
Authors and Affiliations
Contributions
Amal Ashry and Mohamed M. Khamis conceived the idea and planned for the case. Amal Ashry carried out the procedure under the supervision of Mohamed M. Khamis, Ahmed M. Abdelhamid, and Lucette G Segaan. All the authors led the writing and approved the final form of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from the participant included in the study.
Consent for publication
Informed consent was obtained from the participant for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ashry, A., Khamis, M.M., Abdelhamid, A.M. et al. Lip repositioning and guided gingivectomy combined treatment for excessive gingival display by using 940-nm diode laser: a case report. Laser Dent Sci 7, 25–31 (2023). https://doi.org/10.1007/s41547-023-00174-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41547-023-00174-5