Abstract
Many military personnel experience mental health problems, but do not seek professional treatment for their symptoms. The present study examined how support for seeking treatment from family members and friends, unit members, and leaders relate to soldiers’ treatment attitudes and decisions. Active-duty soldiers (N = 1725) completed assessments of perceived social support for treatment-seeking, attitudes toward treatment-seeking, mental health symptoms, and treatment-seeking behaviors. Family and friends were rated as most supportive of seeking treatment and support from all sources was related to a more positive attitude toward treatment seeking. For those who were experiencing a current problem (N = 718), support from all sources was indirectly related to treatment-seeking behaviors through overall attitude toward treatment. Of those who had sought treatment, family and friends were rated as most influential to that decision, and an instrumentally supportive behavior was rated as the most influential out of several supportive leader behaviors. These results demonstrate that support may be an important facilitator of treatment; however, the source of support and specific behaviors may be important considerations in optimally supporting soldiers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Employees in high stress jobs are subject to intense demands, which make them vulnerable to experiencing mental health problems. In the context of military personnel, studies of service members post-9/11 report that approximately 30% of soldiers experience a mental health problem such as Post-Traumatic Stress Disorder (PTSD), depression, or anxiety (Britt et al. 2011, 2016; Hoge et al. 2006). The majority of soldiers experiencing a problem do not seek help from a mental health professional (Britt et al. 2011, 2016; Hoge et al. 2004), which is concerning given the impact untreated symptoms may have on soldier wellbeing and duty performance.
Many factors impact an individual’s decision to seek mental health treatment. These factors include personal attitudes about seeking help (Britt et al. 2016; Kim et al. 2011), characteristics of the problem (e.g, experienced impairment; Britt et al. 2011; Fikretoglu et al. 2008), and practical constraints (e.g., time off work; transportation, Britt et al. 2008; Hoge et al. 2004). Important others are social influences that could have a positive impact on a soldier’s decision to seek help (i.e., social support; Zinzow et al. 2013) or negative influences by directly or indirectly discouraging treatment (i.e., stigma; Britt et al. 2008).
Ajzen’s (1985) theory of planned behavior captures how many of these factors influence behavior, proposing that an individual’s personal attitudes, perceived social norms, and perceived control together influence intentions to engage in a behavior, and subsequently the behavior itself. Thus, if a soldier has positive views of treatment seeking, believes important others would support treatment, and feels in control of the decision, he or she would be likely to get treatment (Britt et al. 2011). The stages of change model (Prochaska and DiClemente 1983) can be used as a framework to elaborate on the complexities of a treatment decision (Britt et al. 2016), where changing behavior involves recognizing a problem, contemplating change, preparing to engage in change-related behavior, actively working on the problem, and maintaining progress (Prochaska and DiClemente 1983; Prochaska et al. 1992). Social support has long been recognized as a resource for coping with stressful circumstances (Cohen and Wills 1985), and helping relationships in particular have been noted as important throughout the process of behavior change (Prochaska et al. 1992). Soldiers may rely on several important relationships as a resource throughout the treatment process, including friends and family, unit members,Footnote 1 and their leadership, due to the hierarchical nature of the military. In this study, we focus on the influence of these important others through a fine-grained analysis of social support related to treatment seeking.
Social support has been associated with soldiers’ adjustment following deployment and experience of symptoms (e.g., Fink et al. 2013; Sripada et al. 2015; Zang et al. 2017). A few studies have also compared perceived support of those in treatment to those not in treatment (Fink et al. 2013; Harpaz-Roten et al. 2014) or the influence of perceived norms associated with treatment seeking on treatment seeking intentions and behaviors (Britt et al. 2011). Fewer studies have considered how perceived support for treatment seeking can be associated with treatment-seeking behaviors (Britt et al. 2016; Zinzow et al. 2013, 2015).
Those existing studies examining social support and treatment seeking focused on soldiers who recognized a current problem (Britt et al. 2016) and those who had experienced sexual assault (Zinzow et al. 2015). As the potential benefits of social support were not the primary topic of investigation in these studies, but rather a broad strokes identification of major barriers and facilitators, the researchers combined perceived social support from several sources as an overall index of support in relation to treatment seeking. Using the combined measure Zinzow et al. 2015, but not Britt et al. 2016, found some evidence that social support could distinguish soldiers who sought treatment from those who did not. Beyond these studies, interviews with soldiers who had sought treatment for a mental health concern find social support to be a top facilitator of treatment seeking (Zinzow et al. 2013).
Given some of the discrepancies in the qualitative and quantitative findings and among different subsets of military populations, we sought to take a more detailed look at the complexities of social support as a facilitator of treatment seeking. The present study considered how three sources of support (family members, unit members, and leaders) could uniquely relate to treatment-seeking attitudes and behaviors. We explored these relationships for soldiers in various stages, in terms of their potential need for treatment. In a general sample of soldiers, we examined which sources of support are perceived as the most encouraging of help-seeking and whether the perception of support is related to a soldier’s attitude toward seeking treatment if they were to experience a problem. We then examined relationships with treatment seeking behaviors among soldiers experiencing a current mental health problem. Finally, we focused on a sub-sample of soldiers who had sought treatment and provided retrospective ratings of the extent to which supportive others influenced their treatment decision. In using the detailed approach, we hoped to determine whether it is necessary to distinguish the source of support in order to understand optimal forms of support to encourage soldiers to seek treatment when needed. Equipping important others to demonstrate social support and encouragement to an individual soldier could be an extremely actionable intervention strategy. Therefore, the research questions are important empirically, as well as practically in supporting the receipt of needed mental health treatment among military personnel and other high-risk occupations.
Social Support as a Resource
Social support can be broadly defined as providing assistance to others or exchanging resources to enhance the wellbeing of the recipient (Shumaker and Brownell 1984). The construct of social support has taken on a wide variety of operational definitions in the organizational and mental health literature, ranging from a simple assessment of whether or not a supportive resource is available to extensive assessments of supportive behaviors (e.g., Sherbourne and Stewart 1991). Theoretical perspectives and empirical evidence suggest that social support can directly reduce experienced stress, as well as buffer the negative impact of stressors on health-related outcomes (Cohen and Wills 1985). Although social support is generally regarded as a multidimensional construct, we first talk about the empirical and theoretical benefits of social support at a broad level and will later distinguish the source of support and function of different supportive behaviors.
As previously introduced, the theory of planned behavior (Ajzen 1985) and stages of change model (Prochaska and DiClemente 1983) capture the broader role of social support in behavior change (i.e., help-seeking) processes, noting that the support of important others may be a key ingredient in initiating and maintaining a change. A deeper look into the stress literature offers a better understanding of the value of support as a resource. In particular, the Conservation of Resources theory (COR; Hobfoll 1989) can be used to understand why social support may aid a soldier experiencing a mental health concern. COR theory broadly posits that individuals need resources to cope with demands, particularly resources that fit the nature of the demand (Hobfoll and Lilly 1993). Thus, individuals strive to protect, retain, and build resources, which include objects, conditions, personal characteristics, or other energies or states that are valued by an individual or that help them to obtain valued states or objects. Strain is experienced when an individual either experiences a loss of desirable resources or perceives that resources are threatened.
COR theory has been appropriately applied to a number of high stress circumstances, such as traumatic experiences or natural disasters in which resource loss is associated with poor adjustment (e.g., Bonanno et al. 2007; Freedy et al. 1994; Ironson et al. 1997). Resources may be of prime importance during and following high stress situations, as research has noted resource gains to be exceptionally important in times of high resource loss (Hobfoll 2001). Interpersonal resources, including social support, are considered a major resource category (Hobfoll and Lilly 1993) and have been found to help individuals to be more resilient following exposure to trauma or negative life events that inherently involve high resource loss (Bonanno et al. 2007; Holahan and Moos 1990).
In the case of military personnel, high demands (from both work and non-work stressors) can be associated with high resource loss, a reduced ability to gain resources, and the experience of mental health symptoms (Hobfoll et al. 2012). Symptoms of a mental health problem could further be experienced as resource loss if participation in daily life is affected, and if symptoms limit the continued acquisition of other resources (e.g., enjoyment of time with important others, ability to work, feelings of confidence/esteem). Seeking treatment from a mental health provider can be a clear resource to fit the demand of experienced mental health symptoms. Social support may be an important facilitating resource to encourage an individual to seek treatment and support this decision, relieving concerns about threat of loss in relationships (i.e., if a soldier perceives others would treat them differently as a result of seeking treatment). Social support could further help individuals to accumulate other resources such as boosting esteem or acquiring practical resources (e.g., transportation to appointments; time off work for appointments) that could facilitate treatment seeking.
Although COR theory would suggest a primary benefit of social support resources, it is important to note that research has yielded inconsistencies regarding the direct and moderating effects of social support on health-related outcomes (Van der Doef and Maes 1999). In fact, some have found that support is associated with negative health outcomes, such as supervisor attempts to provide help being associated with emotional exhaustion and physical health symptoms (Beehr et al. 2010) or co-worker support being associated with higher stress and exhaustion (Ray and Miller 1994). These studies highlight the complexities of providing appropriate support. A notable factor to be considered is the match between provided support and needs of the recipient (Beehr et al. 2003; Beehr et al. 2010). Further, supportive behaviors could be unhelpful if they draw unnecessary attention to the stressor, undermine an individual’s perceived competence, or are generally unwanted (Beehr et al. 2010).
Inconsistencies in the social support literature may also be attributed to the operationalization of support, where studies have used measures that vary widely (Heitzmann and Kaplan 1988). Cutrona (1990) argued that research techniques using aggregate support scores may obscure the true nature of relationships between more precise components of support. Thus, Cutrona recommended the matching approach, where the support assessed should be matched to the type of stressful event being experienced. Prior research has demonstrated the value of domain-specific measures of support, such as family supportive supervisor behaviors and family supportive organization perceptions explaining more variance in work-family related stress compared to more general measures of support (Kossek et al. 2011) as well as domain-specific measures of military leader support behaviors predicting a number of outcomes above and beyond general leadership measures (Adler et al. 2014; Gunia et al. 2015; Jennings et al. 2017). In the present study, we examined social support for mental health treatment seeking in order to capture a supportive resource that would fit the stressful circumstance of experiencing a mental health problem. Specifying the target supportive behavior (i.e., being supportive of seeking treatment) is particularly important so that the difference in others serving as a gateway to professional treatment rather than an informal alternative to treatment (Gottlieb 1976) can be better clarified.
In considering the role of support in the treatment process, studies have found that support in general and unit cohesion can be associated with reduced PTSD symptoms for soldiers undergoing treatment (Zang et al. 2017); however, the presence of close relationships has also been associated with increased discomfort with seeking treatment (e.g., comparing marital status in Ouimette et al. 2011). Britt and colleagues (Britt et al. 2011) found that positive perceived social norms regarding treatment were related to higher intentions to seek treatment for a mental health problem among military personnel.
As previously mentioned, the relationship between social support and actual treatment seeking has been somewhat mixed. Qualitative data report social support as a primary facilitator of treatment seeking for soldiers who had previously sought treatment for a mental health problem (Zinzow et al. 2013). Using quantitative measures, Zinzow et al. (2015) reported a significant relationship between social support and treatment seeking behaviors among military members who had been victims of sexual assault, with social support being measured by a combined assessment of perceived support for treatment seeking from friends and family, unit members, and leaders. Using the same social support measure, Britt and colleagues (Britt et al. 2016) found a non-significant relationship with treatment-seeking behaviors among a sample of soldiers who recognized a current problem. Although the three groups of individuals assessed in prior measures of support (i.e., family and friends, unit members, leaders) all serve as important forms of support, each may offer unique influences that are overlooked by averaging the three ratings.
Source of Support for Treatment Seeking
The source of support may indeed be meaningful to consider when studying the effects of social support. As noted in the COR framework, resources are likely to be most effective when they fit the nature of the demand (Hobfoll and Lilly 1993). A meta-analytic study found that source moderates, though somewhat weakly, relationships between social support and strain (Viswesvaran et al. 1999). Several more recent studies provide examples of these effects. Akerboom and Maes (2006) found that increases in supervisor support, but not co-worker support, corresponded with decreases in psychological distress. Halbesleben (2006) demonstrated in a meta-analytic study that different sources of support may protect employees from different dimensions of burnout. Specifically, work sources of social support were more highly related to the exhaustion dimension of burnout and non-work sources of support were more strongly related to depersonalization and personal accomplishment. Finally, Beehr and colleagues (Beehr et al. 2003) found that source congruence (i.e., if supervisor is the source of stress and the source of support) may be helpful in buffering the effects of social support on the relationship between various stressors and negative psychological outcomes. Many of these researchers attribute the difference in effects based on source to the closeness or control the source has over experienced demands and/or the resources at the disposal of the individual providing support. In sum, the effectiveness of support may depend on the role of the provider, as each provider has a unique relationship with the recipient and different resources at their disposal.
Although a number of studies with military populations have examined different sources of support, none to our knowledge have specifically compared the influence of different support sources on attitudes toward treatment seeking and treatment seeking behaviors. Our study seeks to determine unique influences of three support sources (family and friends, unit members, and leaders) from an overall facilitators of treatment measure used by Britt et al. (2016). Examining each source separately may highlight nuances in perceived support from each relationship. A soldier’s friends and family may be particularly influential because of the social closeness of such relationships (Gottlieb 1976). Having close family relationships has been related to decreased suicidal behaviors in soldiers (Jakupcak et al. 2010); however, close relationships may also elicit concerns with negative evaluations and stigma (Ouimette et al. 2011).
In the present study, we expected perceived support from family and friends to relate to a more positive attitude toward treatment seeking and to soldiers actually seeking treatment when experiencing a problem. We focused on emotional social support, assessed as the soldier perceiving that a family member or friend would encourage them to seek treatment if they needed it. Though emotional support may be expressed in a number of ways, encouragement is one way that care could be shown, aligning with definitions of emotional support (Barrera 1986; House 1981). In viewing stress as a state of depleted resources, aligning with COR theory, emotional support from family and friends would provide an important resource, particularly if a source of resource loss is that a soldier is concerned about negative evaluations from others. The availability of support would likely prevent resource loss associated with negative evaluations of self-worth that could come along with perceived stigma. Further, we expected that soldiers would rate perceived support from family and friends for seeking treatment as the highest of the three sources, as these are the individuals who are likely in closest relationship with the soldier and may have the greatest awareness of resource loss experienced as a result of symptoms. Thus, these individuals, being potentially more aware of a need for treatment, would be likely to support seeking treatment if a soldier were experiencing a mental health concern.
The hierarchical structure of the military and the emphasis on close unit bonds highlight the importance of emotional support from the unit and leader as well. Leaders inhabit an important role where they may influence the stressors soldiers experience, can make changes to the work environment that affect subordinate health and performance (Britt et al. 2004), and may shape the overall climate of the unit toward treatment-seeking (Britt and McFadden 2012). The unit itself is a prominent source of support, given the substantial emphasis on unit cohesion and trusting bonds within military teams (Coll et al. 2011). High unit cohesion has been associated with lower perceived stress and fewer experienced mental health symptoms (Sripada et al. 2015; Zang et al. 2017). Both unit cohesion and leader support have been associated with fewer mental health symptoms and lower stigma perceptions (Britt et al. 2012; Jones et al. 2012; Wright et al. 2009). As social support can be associated with fewer symptoms and stigma perceptions, support for treatment seeking from unit members and leaders should also be positively related to treatment-seeking attitudes and behaviors.
In the same way as support from family members, we expected that emotional support from unit members and leaders may be an important resource for soldiers experiencing the actual or threat of resource loss associated with mental health symptoms. Although we expected that family and friends may have the greatest awareness of a soldiers experienced symptoms, and thus be perceived as most likely to support treatment, unit members and leaders still occupy an important position to support a soldier given the closeness of military units and shared experiences. We expected that each of the three support sources would be significant predictors, accounting for unique variance in attitudes toward treatment seeking, given the different roles each source occupies in relation to the soldier. Given the rationale provided on the closeness of family and friends, we expected the strength of the relationship between support and attitude to be largest for family and friends, with unit and leadership being similar in magnitude. In sum, we hypothesized the following:
-
Hypothesis 1: Family and friends will be rated as most supportive of seeking treatment in comparison to unit members and leaders.
-
Hypothesis 2a: Support from family and friends, unit members, and leaders will be significantly related to a more positive overall attitude treatment seeking, with each predictor accounting for unique variance in attitude.
-
Hypothesis 2b: Support from family and friends will have a stronger relationship with overall attitude, compared to support from the unit and leader.
The first two hypotheses were examined among a general sample of soldiers. Perceptions regarding treatment seeking barriers may change once a soldier is actually experiencing a problem, presumably because the barriers feel more real (Hoge et al. 2004) and actual resource loss may be experienced in the face of symptoms and other experienced stressors (Hobfoll et al. 2012). We addressed this potential difference in perceptions by considering whether mean differences in ratings of support for treatment differ based on whether or not a soldier is experiencing a current problem. In the same way that barriers may become more apparent when one experiences a problem, the perceived availability or absence of supportive resources may also become more salient.
-
Hypothesis 3: The differences in mean ratings of support from the three sources will depend on whether or not a soldier has a current problem.
Our fourth hypothesis concerned only those experiencing a current problem, as indicated by self-reporting a problem or screening positive on symptom measures of PTSD, depression, or an alcohol problem. We extend the logic that emotional support from important others should affect a soldier’s willingness to engage in treatment if they were to experience a problem, as well as their actual treatment seeking behaviors when symptoms are present. Again, we expected that support from family and friends would result in the strongest association with treatment seeking.
-
Hypothesis 4a: Support from family and friends, unit members, and leaders will be significantly related to a higher likelihood of having sought treatment.
-
Hypothesis 4b: Support from family and friends will have a stronger relationship with overall attitude, compared to support from the unit and leader.
Beyond the overall relationships between support and treatment seeking, we sought to connect the relationships among support, attitudes toward treatment, and treatment-seeking behavior. We sought to determine whether emotional support from important others could be conceptualized as a resource that directly encourages soldiers to seek treatment or whether it may have an indirect effect through positively influencing a soldier’s attitude toward treatment. Although the theory of planned behavior discusses social norms as a contributing factor, alongside personal attitudes, to intentions to engage in a given behavior, other research has found that personal attitudes can mediate the relationship between social influences (social stigma, social norms, social support) and intentions to seek treatment (Vogel et al. 2005). This indirect relationship likely extends to treatment-seeking behaviors and may be important in demonstrating that although it is ultimately the decision of the individual to seek treatment, support from others could impact the overall attitude, a personal resource that would facilitate the acquisition of treatment.
-
Hypothesis 5: The relationship between the three sources of support and treatment seeking will be mediated by a soldier’s overall attitude toward seeking treatment.
Supportive Leader Behaviors
We have noted the importance of family and friends and unit members. The role of a leader can also be critical in helping employees cope with difficult circumstances and avoid negative outcomes, where leaders can serve as a buffer in stressful situations (Bliese and Castro 2000; Bliese and Halverson 2002). Up to this point, we have focused our study hypotheses on emotionally supportive behaviors; however, different types of supportive behaviors could be used to encourage treatment seeking. Early research distinguished types of supportive behaviors, including: emotional support that demonstrates care for an individual, instrumental support that meets a tangible need, informational support that provides information to help solve a problem, and appraisal support that provides information relevant to an individual’s self-evaluations (Barrera 1986; House 1981).
As previously noted, research on leader support has also highlighted the value of using domain-specific assessments of support from leaders (Adler et al. 2014; Gunia et al. 2015; Hammer et al. 2009; Jennings et al. 2017; Kossek et al. 2011). These measures, such as Family Supportive Supervisor Behaviors (FSSB; Hammer et al. 2009), demonstrate the value of differentiating different types of supportive behaviors relevant to a given target (i.e., supporting work-family balance). In the present study, we examined leader behaviors which influenced soldiers’ decisions to seek treatment. These assessments of leader support were contextualized to the domain of treatment seeking and were classified by the authors as emotional, instrumental, and informational in nature.
Supportive behaviors were examined retrospectively, where soldiers who had sought treatment rated how influential three leader behaviors were to their decision to seek treatment. The assessment also included single items addressing emotional support from family and fellow unit members. We acknowledge that detailed assessments of different supportive behaviors from friends and unit members would be valuable; however, in the present research additional items assessing targeted support focused on leaders because several of the typical types of support map onto leadership competencies (e.g., supporting soldiers, creating a positive work environment; Department of the Army 2006). We proposed that, of the leader support behaviors, instrumental support would be rated as most influential. Access to practical needs (e.g., time off work) are likely an important resource to engaging in treatment and maintaining progress. Such resources are often under the control of the leader. Thus, leaders would be in a valuable position to offer instrumental support that can facilitate treatment for those in an active stage of behavior change, such as by altering demands of the job that can create practical barriers to care.
-
Hypothesis 6: Among soldiers who report having sought treatment for a mental health problem, instrumental support from leaders will be rated as more influential to the soldier’s decision to seek treatment than emotional and informational support.
Method
Participants
U.S. Army soldiers (N = 1911) were surveyed on their base, and 90% (N = 1725) provided consent for their responses to be used for research purposes (Britt et al. 2016). Only these responses with consent given were used in analyses. The full sample was used for examining Hypotheses 1–3. The majority of the sample identified as male (90.1%). The most commonly reported ethnicity was white (63%), followed by African American (18%), Hispanic (10%), and Asian/Pacific Islander (4%) or other (5%). Most soldiers were between the ages of 20 and 24 (46%) or 25 and 29 (27%), with fewer soldiers aged 18 to 19 (5%), 30 to 39 (18%), or over 40 (4%). Average military tenure was 5 years (SD = 5.6) and most soldiers were junior enlisted (69% E1-E4) or non-commissioned officers (21% E5-E6). Fewer soldiers were E7-E9 (3%) or officer ranks (O1-O9; WO1-WO5; 7%).Footnote 2
For Hypothesis 4 and 5, the focal sample was soldiers who either reported experiencing a current problem or who met screening criteria for PTSD, depression, or an alcohol problem (N = 718). The subsample of those with a mental health problem was demographically similar to the total sample: male (89.7%), white (65.6%), age 20 to 24 (45.4%) or 25 to 29 (27.3%), average military tenure 5.4 years (SD = 5.6), and junior enlisted (70%). For Hypothesis 6, only those who had sought treatment were included (N = 318), as these individuals indicated the sources of support that most influenced them to seek treatment.
The dataset has been used in prior research by Britt et al. (2016) and Zinzow et al. (2015). Britt et al. (2016) examined an overall measure of social support as a predictor of treatment seeking only among those individuals who recognized their problem. Zinzow et al. (2015) used an overall measure of social support only among victims of sexual assault. The present study offers novel contributions by examining individual sources of support, the mediating role of overall attitude towards treatment, and how influential individual sources were in getting treatment.
Procedure
A survey designed to understand soldier perceptions and utilization of mental health services was administered to soldiers nine months following the Brigade’s combat deployment. The survey assessment took place over five consecutive days, consisting of 29 total sessions with a maximum of 140 soldiers in each session. Soldiers arrived to a classroom facility on the base with their unit at times arranged with unit leadership to complete the survey.
Measures
Sources of Support for Treatment Seeking
was assessed with three items (Britt et al. 2016), which were examined independently. Past research has established that single item measures can demonstrate comparable validity to that of multiple item measures (Bergkvist and Rossiter 2007). The items were: “Friends and family would encourage me to go get mental health treatment if I needed it”, “My leaders would encourage me to go get treatment if I needed it”, and “My fellow unit members would encourage me to go get treatment if I needed it”. Responses ranged from strongly disagree (1) to strongly agree (5).
Influences on Treatment Seeking
Assessed the behaviors and individuals that influenced soldiers who decided to seek treatment (Zinzow et al. 2015). Participants were asked to indicate the extent to which a series of factors influenced them to seek treatment with response options ranging from not at all (1) to very much (5). Three items reflected emotional support from the different sources: “My spouse/family encouraged me”, “A fellow soldier or friend encouraged me”, and “My leaders were supportive of seeking treatment”. In addition to the item assessing emotional support from leaders, two items reflected instrumental and informational supportive leader behaviors: “My leaders allowed me time off work to attend treatment” and “My leaders gave me information on where to go for treatment”.
Attitude Toward Treatment Seeking
Was assessed using one item: “Overall, what is your current attitude toward seeking treatment from a mental health professional were you to develop a problem?” (Britt et al. 2011). Response options were very negative (1) to very positive (7).
Treatment Seeking
Was assessed in four ways. Soldiers were considered to have sought treatment if they indicated that they had: 1) Sought treatment from any of nine sources that were provided within the past 12 months (e.g., military behavioral health clinics, civilian providers); 2) Received any of six provided treatments within the past 12 months (e.g., individual therapy or counseling, medication); 3) Attended mental health visits within the past 12 months (response options: 0, 1–2, 3–7, 8–12, or more than 12); or 4) started treatment but dropped out.
Current Problem
Soldiers were considered to be experiencing a current problem if they self-reported a current problem on a single item asking if they were currently experiencing a stress, emotional, alcohol, or family problem (response options yes or no) or screened positive on any symptom measures described below.
PTSD (α = .96) symptoms were assessed using the 17-item PTSD Checklist (Weathers et al. 1993). Soldiers were asked to indicate how bothered they had been by 17 symptoms in the past month (1 = not at all; 5 = extremely). A sample item was “Repeated, disturbing memories, thoughts, or images of the stressful experience”. Participants were considered as experiencing PTSD if they met DSM-IV criteria for PTSD and had a symptom severity score greater than 50 (National Center for PTSD 2012).
Depression (α = 91) symptoms were assessed using the nine-item Patient Health Questionnaire (PHQ; Kroenke et al. 2001). Participants indicated how often they had been bothered by each symptom in the past two weeks (1 = not at all; 4 = nearly every day). A sample item was “little interest or pleasure in doing things”. Participants also indicated how difficult the problems made it to do work, take care of things at home, or get along with others (1 = not difficult at all; 4 = extremely difficult). Participants were considered as having Major Depressive Disorder if they: 1) reported “little interest or pleasure in doing things” or “feeling down, depressed, or hopeless” at least more than half the days; 2) reported on five or more items that they experienced the symptom at least more than half of the days, and; 3) reported at least somewhat difficult on the difficulty item.
Alcohol Problem (rSB = .66). A problem with excessive alcohol use was assessed using the Two Item Conjoint Screen (TICS; Brown et al. 2001). Items were “Have you ever felt you wanted or needed to cut down on your drinking?” and “Have you ever used alcohol more than you meant to?” Participants were considered to have an alcohol problem if they responded yes to at least one of the items.
Demographics and Control Variables
Age, gender, race/ethnicity and education were included as control variables in analyses to account for any basic differences in treatment seeking based on demographics, as demographic variables can be related to perceptions/availability of support, help-seeking attitudes, and help-seeking behaviors (e.g., Galdas et al. 2005; Hall and Tucker 1985; Mckinlay 1973; Steele et al. 2007). In analyses involving those experiencing a problem, we also controlled for functional impairment, as the degree of impairment caused by symptoms has been related to treatment seeking behaviors (Britt et al. 2011; Fikretoglu et al. 2008). Functional impairment (α = .91) was measured using three items adapted from Sheehan et al. (1996). Participants were asked how much stress or emotional problems had “limited your ability to do your primary military job”, “disrupted your social life”, and “disrupted your family life/home responsibilities” over the past four weeks (1 = not at all; 5 = extremely).
Results
Analyses were conducted using SPSS v.25. Means, standard deviations, and correlations for variables used in analyses for the full sample are presented in Table 1; correlations for those with a current problem are reported in Table 2. Initial correlations provided support for the proposed relationships, where each source of support was correlated with overall attitude toward treatment; however, only support from family members and friends was correlated with treatment seeking for those who were experiencing a problem.
Mean Differences in Support Ratings
To examine Hypothesis 1 and 3, a 3 × 2 mixed ANOVA was conducted to determine whether there were differences in the repeated measures of source of support and differences between subjects who were experiencing a problem verses those who were not. There was a significant difference in mean ratings of the three sources of support for treatment seeking, F(1.70, 2911.27) = 365.04, p < .01, \( {\upeta}_{\mathrm{p}}^2 \) = .18. Results of the Greenhouse-Geisser test are reported because Mauchly’s test of Sphericity was violated. Post-hoc comparisons indicated that ratings of support for treatment from family and friends (M = 4.05, SD = .93) were higher than support from one’s leader (M = 3.50, SD = 1.05; p < .01) and unit (M = 3.42, SD = .98; p < .01), supporting Hypothesis 1. Leader support was also rated higher than unit support (p < .01).
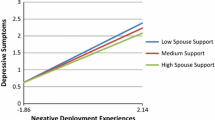
There was an interaction between support ratings and whether a soldier was experiencing a current problem, F (1.70, 2911.27) = 14.91, p < .001, \( {\upeta}_{\mathrm{p}}^2 \) = .01. Soldiers experiencing a problem tended to rate support for treatment from all sources as lower than those not experiencing a problem. Differences were more pronounced in the ratings of perceived support from leaders and unit members (Fig. 1).
Support and Attitude Toward Treatment
A series of linear regressions were conducted relating each source of support for treatment seeking to overall attitude toward treatment seeking (Hypothesis 2). Each source was first entered into a separate model with demographic control variables (age, gender, race/ethnicity, and education). Demographics were entered in Step 1 and the specific source of support was entered in Step 2 to determine the variance explained beyond the control variables. All significant support predictors were entered into a final model, including the control variables. In addition, a relative weights analysis using the web-based software developed by Tonidandel and LeBreton (2015) was conducted to determine whether the magnitude of the effects of each source of support were significantly different from one another.
In the initial regression analyses, examining each source of support separately, social support for treatment seeking from family members was positively related to the soldier’s overall attitude toward seeking treatment (B = .29, SE = .04, p < .01, 95% CI: .21, .37, ΔR2 = .03). The same relationships were true for leader support (B = .25, SE = .04, p < .01, 95% CI: .18, .31, ΔR2 = .03) and unit support being positively related to overall attitude (B = .34, SE = .04, p < .01, 95% CI: .26, .41, ΔR2 = .05).
When all variables were entered into a single regression (Table 3), support from family and friends and unit members remained significant predictors of attitude toward treatment seeking; leader support was not significantly related to attitude when accounting for the other two sources of support. These results suggest that support for treatment from family and unit members explain unique variance in a soldier’s overall attitude toward seeking treatment, providing partial support for Hypothesis 2a. A relative weights analysis revealed that unit support accounted for the largest portion of the variance explained in the model. Table 3 provides the relative weights for the different predictors and the portion of the explained variance accounted for by each predictor (RS-RW %). When comparing the strength of the relative weights, the contribution by unit support was not significantly higher when compared to family support (95% CI = −.03, .008); however, the relative weight for the unit was significantly higher than support from the leader (95% CI = .0007, .03). Thus, these results did not support Hypothesis 2b. Rather, our results demonstrated that the unit and family may be similarly influential sources of support in relation to a soldier’s overall attitude.
Support and Treatment-Seeking Behaviors
The effect of each source of support on treatment-seeking behaviors for soldiers experiencing a current problem was examined in a series of logistic regressions (Hypothesis 4). Age, ethnicity, education, and functional impairment were included as control variables. Note gender was excluded as a control variable because there were a number of cases who did not report gender. Because the sample size was already limited when focusing on those with a problem and given the weak and non-significant correlations between gender and treatment seeking, we saw this as an appropriate measure to preserve statistical power.
Logistic regressions were conducted for each source of support separately. Only family support (OR = 1.16, 95% CI: .98, 1.37, p = .09) and leader support (OR = 1.15, 95% CI: .99, 1.33, p = .07), but not unit support, approached significance as predictors of treatment seeking. Thus, Hypothesis 4a was not supported. Given the lack of support for Hypothesis 4a, Hypothesis 4b was not tested with a relative weights comparison.
Hypothesis 5 proposed an indirect relationship between sources of support and treatment seeking behaviors through overall attitude toward treatment. Although we did not find evidence of direct effects between support and treatment seeking, it is possible and still meaningful to find an indirect relationship in the absence of a direct effect (Zhao et al. 2010). Because each source of support was related to overall attitude and attitude was correlated with treatment-seeking (r = .25), three tests were done to determine if there could be an indirect effect of support on treatment seeking through overall attitude using Hayes (2012) SPSS PROCESS script. Age, education, and functional impairment were included as control variables. Again, gender was omitted as a control variable to conserve statistical power.
Results suggested a significant indirect effect, with bootstrap confidence intervals (using 5000 iterations) not including zero, for family support (Bootstrap CI: .04, .17), leader support (Bootstrap CI: .03, .14), and unit support (Bootstrap CI: .05, .17) related to treatment seeking through overall attitude. Thus, there was evidence for Hypothesis 5 that support from each source could have an indirect effect on treatment-seeking behavior through overall attitude. Figure 2 provides a summary of the indirect paths for each of the three models.
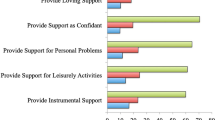
Retrospective Supportive Ratings
The final analyses focused on differences in the retrospective ratings of supportive behaviors that influenced a soldier’s decision to seek treatment. Providing additional support for Hypothesis 1, a repeated measures ANOVA comparing the ratings of influences to seeking treatment revealed that the ratings of family members encouraging soldiers to go to treatment were highest (M = 2.52, SD = 1.35) compared to support from leaders (M = 1.72, SD = 1.32) or a fellow soldier/friend (M = 1.81, SD = 1.35). The mean differences were significant, F (1.96, 699.77) = 64.59, p < .001, \( {\upeta}_{\mathrm{p}}^2 \) = .15. Post-hoc comparisons revealed that ratings of family were significantly higher than ratings of leaders and fellow soldiers (which were not significantly different from one another). Again, values for the Greenhouse-Geisser test are reported.
In regard to supportive leader behaviors, a repeated measure ANOVA revealed a significant difference in reports of instrumental (M = 1.95, SD = 1.27), informational (M = 1.44, SD = 1.33), and emotional (M = 1.74, SD = 1.32) support behaviors, F (1.77, 640.63) = 37.53, p < .01, \( {\upeta}_{\mathrm{p}}^2 \) = .09. Each type of support was significantly different from the others, with instrumental support as the highest rated form of support that influenced the soldier to seek treatment (p < .01), supporting Hypothesis 6.
Discussion
The results of the present study demonstrate that social support for treatment seeking may be influential to soldiers’ attitudes toward seeking treatment, as well indirectly related to actual treatment decisions. Family and friends were rated as the most supportive of seeking treatment, both in general ratings from soldiers and retrospective ratings from those who sought treatment. The findings support previous research, which theorizes that those closest to an individual will have the strongest influence on whether or not an individual decides to seek treatment (Gottlieb 1976). Family and friends are likely influential because they can provide a critical resource of support when a soldier anticipates or experiences stress associated with a mental health concern. Such interpersonal resources are likely an ideal match to the demands (Cutrona 1990; Hobfoll and Lilly 1993) experienced by a soldier with a mental health concern, given resource loss that may be associated with symptoms or threat of loss if there is concern about a mental health concern affecting relationships with others. As an interesting consideration, we also found that perceptions of support may be different for those experiencing a problem. Extending the findings of Hoge et al. (2004), where soldiers perceived more stigma and barriers to treatment when experiencing a problem, soldiers experiencing a problem may feel less supported. The lower ratings of support could be a function of the soldiers’ symptoms themselves, or could indicate that that soldiers do not feel their supportive resources are sufficient when they actually experience a problem and threat of or actual resource loss.
Although close family members may exert a strong influence by supporting soldiers, organizational agents may still influence a soldier’s attitude. Unit members remained a unique predictor of a soldier’s attitude toward treatment, with a relative weight similar to family support, but significantly larger than leader support. The strong relationship with a soldier’s attitude could be concerning, given perceived support for seeking treatment from one’s unit was rated as lowest in mean comparisons. Such findings support the need for increased intervention at the unit level to create a unit climate that is supportive of treatment seeking (Britt et al. 2018). For instance, in the training by Britt et al. (2018) soldiers were encouraged to proactively talk about barriers to mental health treatment and how the unit can facilitate treatment for soldiers who could benefit from professional help.
Our findings in regard to leader and unit support add to past research on positive leadership and unit cohesiveness in the military (Britt et al. 2012; Wright et al. 2009) by showing that support for treatment from these individuals is related to soldiers’ attitudes toward treatment seeking. In addition, we found that instrumental support may be the most influential form of support for leaders to provide. Soldiers may first seek emotional support from those closest to them (e.g., family members and potentially unit members), but adjustments to work demands may be important forms of support from leaders. Further, these may be the most relevant sources of support at the stage of being actively involved in treatment and maintaining progress compared to more emotional support that may be needed for recognizing a problem and initiating treatment.
The results of this study hold several theoretical and practical implications. First, the present study contributes existing research by showing that social support is related to soldier’s attitudes toward treatment seeking (Britt et al. 2011) and indirectly to treatment-seeking behaviors. In line with research that recommends matching a measure of support to a particular need (Cutrona 1990), we provide evidence that targeted support assessments may be valuable in providing conceptual clarity for understanding support as a facilitator of treatment. Some researchers have noted that individuals may cope with problems through informal support sources rather than utilizing professional services (Gottlieb 1976). Using targeted assessments of support for seeking professional treatment clarifies the nature of support provided. Future research studies could use more extensive assessments of informal support (as an alternative to treatment) to further understand the nuances of support from important others.
Our study also provided evidence that researchers should not immediately turn to oversimplified measures of social support averaging across sources because support from different individuals shown through different behaviors may have unique relationships with outcomes. Of practical significance, friends and family members were generally rated as most supportive and influential to a soldier’s treatment decisions, yet unit support was still strongly and uniquely related to attitudes toward treatment. The importance of family may encourage the organization to emphasize family involvement and provide educational resources for family members of soldiers. It may be particularly helpful to offer resources to educate family members on how to provide the most appropriate support to encourage service members to seek treatment. These trainings could focus on offering support that matches the need of the soldier (e.g., trying to direct a soldier to professional help rather than serving as a substitute) or recognition of symptom severity that may warrant treatment.
Because of the relationships with attitude and indirect effects on treatment seeking, unit members and leaders should also be considered important and unique support sources. In past research, positive behaviors from the leader and unit have been associated with lower perceptions of stigma and barriers (Wright et al. 2009). The present study further demonstrates the value of positive unit members and leadership, not only to reduce barriers, but also in facilitating treatment by offering support.
The lower ratings of support from the unit in the present study highlight the need for unit-level interventions. These results should encourage the military as a whole to emphasize the importance of supporting fellow unit members in seeking treatment, potentially through support training such as that developed by Britt et al. (2018). Using this training format soldiers can be taught to recognize the effect that unit members can have on fellow soldiers’ decisions to seek treatment. As one example, Britt et al. (2018) highlighted how the unit can create heightened concerns that others will perceive a soldier as trying to get out of work if they attend treatment, which could be a major barrier to treatment seeking. Britt et al. (2018) found evidence that such a training focusing on reducing stigma and developing a positive unit climate could increase supportive behaviors toward fellow unit members. Beyond changes to the climate, unit members may also be in a critical position to be trained to recognize symptoms in fellow soldiers, given close unit bonds and shared experiences. In particular, studies suggest that peer support through sharing similar experiences of symptoms, and thus normalizing mental health concerns to some degree, shows beneficial effects that can encourage treatment seeking (Murphy et al. 2014; Ben-Zeev et al. 2012).
Although emotional support from leaders was generally less related to a soldier’s attitude compared to family and friends and unit members, our study highlights that leaders may be exceptionally valuable in their ability to provide instrumental support. Leaders could receive further training on how to be an instrumental and informational resource to soldiers who may benefit from seeking mental health treatment. Making sure it is readily known to soldiers that leaders can help accommodate practical treatment needs could be an important facilitator for soldiers who are concerned with seeking treatment because of interference with their work schedule, or even how seeking treatment may be perceived by their leadership. Studies have suggested that military leaders do view caring for the behavioral health of their soldiers as an aspect of their leadership role (Mallick et al. 2016). Therefore, such training on tools for providing optimal support would likely be welcomed by leaders who share with this view of their role.
It is worth highlighting that these findings may practically apply to other high stress occupations, such as firefighters, police officers, and other first responders. Many of these occupations can be characterized by potential for traumatic exposure, working in close units, and emphasize norms that emphasize resilience. With such parallels, it is likely that these occupations could also benefit from both interventions with family members to recognize symptoms and support those who may experience a problem, as well as working to create a supportive climate among unit members and leadership.
Limitations and Future Directions
Limitations of the present study highlight potential areas for future research. First, the study utilized cross-sectional and self-report data. Although self-report data is an optimal way to capture perceptions of support and personal attitudes, concerns about confidentiality or social desirability may impact participant responses. Further, using a single self-report survey during a single measurement occasion presents some concerns that common method variance could inflate the observed relationships (Podsakoff et al. 2003). We do, however, note that our self-report items did ask participants to provide responses to a variety of measures, some that were perceptual in nature, some that were behavioral (i.e., past treatment seeking visits). The scales also had different response formats, where some were agreement scales and others assessed the presence or absence of various behaviors. In order to reduce concerns about social desirability and common method variance, future studies could attempt to gather more objective measures of treatment visits or multi-source data for assessing support. In addition, longitudinal research could better capture the process that may unfold between perceived and provided support and treatment decisions. For instance, we found that perceptions of support may be lower among soldiers experiencing a problem. It would be interesting to consider how these perceptions change over time as the potential for treatment becomes more real to both the recipient and provider of support.
Second, the assessments of social support were based on one-item measures. Past research has established that single item measures can demonstrate comparable validity to that of multiple item measures (Bergkvist and Rossiter 2007; Matthews et al. 2010). Further, the support items were targeted specifically for treatment seeking, and should have adequately captured the support of interest. Still, future studies should also assess social support using larger inventories of possible supportive behaviors that may facilitate treatment seeking, particularly assessing different supportive behaviors from the three different sources. Our study results differentiating types of support provided by leaders suggest that this may be a worthwhile future direction to distinguish a variety of targeted supportive behaviors provided by unit members and family, in addition to leaders. Researchers could also utilize more general measures of support in conjunction with measures of support specifically for treatment seeking to better understand whether general support functions more strongly as a facilitator to treatment seeking or more as an informal source of treatment for the problem.
Related to this second limitation in our measurement of support, we did rely on retrospective ratings of leader support in particular. The analyses involving those who had previously sought treatment represent an important contribution in asking soldiers to consider what supportive others affected their decision to seek treatment. We cannot, however, eliminate the possibility that a soldiers ratings could be influenced by changes in symptoms. Just as our findings suggest that those experiencing a current problem may rate available support as lower than those not experiencing a current problem, a soldier may rate supportive individuals more positively following treatment, when symptoms have subsided. Detailed assessments of support throughout the treatment process are needed to better clarify the potential for these complex relationships.
There are several other areas where future research could extend the findings of the present study. We found evidence for an indirect effect of support on treatment seeking through overall attitude toward treatment seeking, which aligns with prior work that has considered personal attitudes and beliefs as mediators (Vogel et al. 2005). Further research should seek a better understanding of mediating and moderating mechanisms that may impact treatment-seeking decisions. In particular, it is important for future studies to examine these potential mediating mechanisms using a longitudinal design to better understand how the effect of support on attitudes and treatment seeking may unfold over time. Studies should also consider any unintended consequences of social support (Beehr et al. 2010) that could occur in the process of considering treatment. These options for unintended outcomes should be considered in order to provide optimal support, as well as training in providing support to those close to soldiers. Finally, in addition to further studies with military personnel, researchers should seek to replicate and apply the results of this study to other high stress occupations, such as police officers and other first responders. We anticipate that our findings would translate well into these occupational groups, but further research is needed to clarify the support needs of these populations.
Conclusion
Many soldiers experience mental health problems as a result of occupational conditions; however, many who may benefit from professional treatment do not seek help. The present study found that support for treatment seeking from friends and family, unit members, and leaders was directly related to attitudes toward seeking treatment and indirectly to decisions to seek treatment through attitude. Continued research and application of the present findings should seek to enhance social support provided to soldiers to encourage them to get needed treatment to improve their quality of life and military service.
Notes
The term unit members is used as a general term in this paper. In the specific context of the Army (the population studied in the present study), this could refer to either a service member’s squad (the smallest unit in the Army, typically 6 to 10 members) or potentially their platoon (3 or 4 squads). Because the nature of the work itself could affect what “unit” means to a given soldier, we opt for this more generic term rather than the more specific terms. Still, it is expected that most service members would interpret the term unit as the smallest group with which they regularly work.
Officers are military personnel who have a minimum of a bachelor’s degree and who went through formal officer leadership training. Non-commissioned officers are enlisted soldiers who have attained the minimum rank of Sergeant and participated in non-commissioned officer leadership training. Junior enlisted soldiers are those enlisted personnel with the rank of Private, Private First Class, or Specialist.
References
Adler, A. B., Saboe, K. N., Anderson, J., Sipos, M. L., & Thomas, J. L. (2014). Behavioral health leadership: new directions in occupational mental health. Current Psychiatry Reports, 16(10), 1–7. https://doi.org/10.1007/s11920-014-0484-6.
Ajzen, I. (1985). From intentions to action: A theory of planned behavior. In J. Kuhl & J. Beckman (Eds.), Action control: From cognition to behavior (pp. 11–39). Heidelberg: Springer.
Akerboom, S., & Maes, S. (2006). Beyond demand and control: the contribution of organizational risk factors in assessing the psychological well-being of health care employees. Work and Stress, 20(1), 21–26. https://doi.org/10.1080/02678370600690915.
Barrera, M. (1986). Distinctions between social support concepts, measures, and models. American Journal of Community Psychology, 14(4), 413–445. https://doi.org/10.1007/BF00922627.
Beehr, T. A., Farmer, S. J., Glazer, S., Gudanowski, D. M., & Nair, V. N. (2003). The enigma of social support and occupational stress: Source congruence and gender role effects. Journal of Occupational Health Psychology, 8(3), 220–231. https://doi.org/10.1037/1076-8998.8.3.220.
Beehr, T. A., Bowling, N. A., & Bennett, M. M. (2010). Occupational stress and failures of social support: when helping hurts. Journal of Occupational Health Psychology, 15(1), 45–59. https://doi.org/10.1037/a0018234.
Ben-Zeev, D., Corrigan, P. W., Britt, T. W., & Langford, L. (2012). Stigma of mental illness and service use in the military. Journal of Mental Health, 21(3), 264–273. https://doi.org/10.3109/09638237.2011.621468.
Bergkvist, L., & Rossiter, J. R. (2007). The predictive validity of multiple-item versus single-item measures of the same constructs. Journal of Marketing Research, 44(2), 175–184. https://doi.org/10.1509/jmkr.44.2.175.
Bliese, P., & Castro, C. (2000). Role clarity, work overload and organizational support: multilevel evidence of the importance of support. Work and Stress, 14, 65–73. https://doi.org/10.1080/026783700417230.
Bliese, P., & Halverson, R. (2002). Using random group resampling in multilevel research: an example of the buffering effects of leadership climate. The Leadership Quarterly, 13(1), 53–68. https://doi.org/10.1016/S1048-9843(01)00104-7.
Bonanno, G. A., Galea, S., Bucciarelli, A., & Vlahov, D. (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75(5), 671–682. https://doi.org/10.1037/0022-006X.75.5.671.
Britt, T. & McFadden, A. (2012). Understanding mental health treatment-seeking in high stress occupations. In J. Houdmont, S. Leka, & R. Sinclair (Eds.) Contemporary Occupational Health Psychology: Global Perspectives on Research and Practice, 2, 57–73.
Britt, T. W., Davison, J., Bliese, P. D., & Castro, C. A. (2004). How leaders can influence the impact that stressors have on soldiers. Military Medicine, 169(7), 541–545. https://doi.org/10.7205/MILMED.169.7.541.
Britt, T. W., Greene-Shortridge, T. M., Brink, S., Nguyen, Q. B., Rath, J., Cox, A. L., Hoge, C. W., & Castro, C. A. (2008). Perceived stigma and barriers to care for psychological treatment: Implications for reactions to stressors in different contexts. Journal of Social and Clinical Psychology, 27(4), 317–335. https://doi.org/10.1521/jscp.2008.27.4.317.
Britt, T. W., Bennett, E. A., Crabtree, M., Haugh, C., Oliver, K., McFadden, A., & Pury, C. S. (2011). The theory of planned behavior and reserve component veteran treatment seeking. Military Psychology, 23(1), 82–96. https://doi.org/10.1080/08995605.2011.534417.
Britt, T. W., Wright, K. M., & Moore, D. (2012). Leadership as a predictor of stigma and practical barriers toward receiving mental health treatment: a multilevel approach. Psychological Services, 9(1), 26–37. https://doi.org/10.1037/a0026412.
Britt, T. W., Jennings, K. S., Cheung, J., Zinzow, H., Pury, C., Raymond, M. A., & Mcfadden, A. (2016). Determinants of mental health treatment seeking among soldiers who recognize their problem: implications for high-risk occupations. Work and Stress, 30(4), 318–336. https://doi.org/10.1080/02678373.2016.1246490.
Britt, T.W., Black, K.J., Cheung, J. H., Zinzow, H. M., Pury, C. L. (2018). Unit training to increase support for military personnel with mental health problems. Work & Stress, Advance online publication. https://doi.org/10.1080/02678373.2018.1445671.
Brown, R. L., Leonard, T., Saunders, L. A., & Papasouliotis, O. (2001). A two-item conjoint screen for alcohol and other drug problems. The Journal of the American Board of Family Practice, 14(2), 95–106.
Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. https://doi.org/10.1037/0033-2909.98.2.310.
Coll, J. E., Weiss, E. L., & Yarvis, J. S. (2011). No one leaves unchanged: insights for civilian mental health care professionals into the military experience and culture. Social Work in Health Care, 50(7), 487–500. https://doi.org/10.1080/00981389.2010.528727.
Cutrona, C. E. (1990). Stress and social support—In search of optimal matching. Journal of Social and Clinical Psychology, 9(1), 3–14. https://doi.org/10.1521/jscp.1990.9.1.3.
Department of the Army. (2006). Army leadership: Competent, confident, and agile (FM6–22). Washington, D.C.: Department of the Army.
Fikretoglu, D., Guay, S., Pedlar, D., & Brunet, A. (2008). Twelve month use of mental health services in a nationally representative, active military sample. Medical Care, 46(2), 217–223. https://doi.org/10.1097/MLR.0b013e31815b979a.
Fink, D. S., Gallaway, M. S., & Millikan, A. M. (2013). Assessment of subthreshold and developing behavioral health concerns among US Army soldiers. Military Medicine, 178(11), 1188–1195. https://doi.org/10.7205/MILMED-D-13-00243.
Freedy, J. R., Saladin, M. E., Kilpatrick, D. G., Resnick, H. S., & Saunders, B. E. (1994). Understanding acute psychological distress following natural disaster. Journal of Traumatic Stress, 7(2), 257–273. https://doi.org/10.1002/jts.2490070207.
Galdas, P., Cheater, F., & Marshall, P. (2005). Men and health help-seeking behaviour: literature review. Journal of Advanced Nursing, 49(6), 616–623. https://doi.org/10.1111/j.1365-2648.2004.03331.x.
Gottlieb, B. H. (1976). Lay influences on the utilization and provision of health services: a review. Canadian Psychological Review, 17(2), 126–136. https://doi.org/10.1037/h0081829.
Gunia, B. C., Sipos, M. L., LoPresti, M., & Adler, A. B. (2015). Sleep leadership in high-risk occupations: an investigation of soldiers on peacekeeping and combat missions. Military Psychology, 27(4), 197–211. https://doi.org/10.1037/mil0000078.
Halbesleben, J. R. (2006). Sources of social support and burnout: a meta-analytic test of the conservation of resources model. Journal of Applied Psychology, 91(5), 1134. https://doi.org/10.1037/0021-9010.91.5.1134.
Hall, L., & Tucker, C. (1985). Relationships between ethnicity, conceptions of mental illness, and attitudes associated with seeking psychological help. Psychological Reports, 57(3), 907–916. https://doi.org/10.2466/pr0.1985.57.3.907.
Hammer, L., Kossek, E., Yragui, N., Bodner, T., & Hanson, G. (2009). Development and validation of a multidimensional measure of family supportive supervisor behaviors (FSSB). Journal of Management, 35(4), 837–856. https://doi.org/10.1177/0149206308328510.
Harpaz-Roten, I., Rosenheck, R. A., & Southwick, S. (2014). Determinants of prospective engagement in mental health treatment among symptomatic Iraq/Afghanistan veterans. The Journal of Nervous and Mental Disease, 202(2), 97–104. https://doi.org/10.1097/NMD.0000000000000078.
Hayes, A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper]. Retrieved from http://www.afhayes.com/public/process2012.pdf
Heitzmann, C. A., & Kaplan, R. M. (1988). Assessment of methods for measuring social support. Health Psychology, 7(1), 75–109. https://doi.org/10.1037/0278-6133.7.1.75.
Hobfoll, S. E. (1989). Conservation of resources: a new attempt at conceptualizing stress. American Psychologist, 44(3), 513–524. https://doi.org/10.1037/0003-066X.44.3.513.
Hobfoll, S. E. (2001). The influence of culture, community, and the nested-self in the stress process: advancing conservation of resources theory. Applied Psychology. An International Review, 50(3), 337–370. https://doi.org/10.1111/1464-0597.00062.
Hobfoll, S. E., & Lilly, R. S. (1993). Resource conservation as a strategy for community psychology. Journal of Community Psychology, 21(2), 128–148. https://doi.org/10.1002/1520-6629(199304)21.
Hobfoll, S. E., Vinokur, A. D., Pierce, P. F., & Lewandowski-Romps, L. (2012). The combined stress of family life, work, and war in air force men and women: a test of conservation of resources theory. International Journal of Stress Management, 19(3), 217–237. https://doi.org/10.1037/a0029247.
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351(1), 13–22. https://doi.org/10.1056/NEJMoa040603.
Hoge, C. W., Auchterlonie, J. L., & Milliken, C. S. (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association, 295(9), 1023–1032. https://doi.org/10.1001/jama.295.9.1023.
Holahan, C., & Moos, R. (1990). Life stressors, resistance factors, and improved psychological functioning: an extension of the stress resistance paradigm. Journal of Personality and Social Psychology, 58(5), 909–917. https://doi.org/10.1037/0022-3514.58.5.909.
House, J. S. (1981). Work stress and social support. Reading: Addison-Wesley Publishing Company.
Ironson, G., Wynings, C., Schneiderman, N., Baum, A., Rodriguez, M., Greenwood, D., et al. (1997). Posttraumatic stress symptoms, intrusive thoughts, loss, and immune function after Hurricane Andrew. Psychosomatic Medicine, 59(2), 128–141.
Jakupcak, M., Vannoy, S., Imel, Z., Cook, J. W., Fontana, A., Rosenheck, R., & McFall, M. (2010). Does PTSD moderate the relationship between social support and suicide risk in Iraq and Afghanistan war veterans seeking mental health treatment? Depression and Anxiety, 27(11), 1001–1005. https://doi.org/10.1002/da.20722.
Jennings, K., Adler, A., & Thomas, J. (2017). Characterizing the health and attitudes of rear detachment soldiers. Military Behavioral Health, 5(2), 189–201. https://doi.org/10.1080/21635781.2016.1272022.
Jones, N., Seddon, R., Fear, N. T., McAllister, P., Wessely, S., & Greenberg, N. (2012). Leadership, cohesion, morale, and the mental health of UK armed forces in Afghanistan. Psychiatry: Interpersonal and Biological Processes, 75(1), 49–59. https://doi.org/10.1521/psyc.2012.75.1.49.
Kim, P. Y., Britt, T. W., Klocko, R. P., Riviere, L. A., & Adler, A. B. (2011). Stigma, negative attitudes about treatment, and utilization of mental health care among soldiers. Military Psychology, 23(1), 65–81. https://doi.org/10.1080/08995605.2011.534415.
Kossek, E., Pichler, S., Bodner, T., & Hammer, L. (2011). Workplace social support and work-family conflict: a meta-analysis clarifying the influence of general and work-family-specific supervisor and organizational support. Personnel Psychology, 64(2), 289–313. https://doi.org/10.1111/j.1744-6570.2011.01211.x.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The Phq9. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Mallick, L. M., Mitchell, M. M., Millikan-Bell, A., & Shayne Gallaway, M. (2016). Small unit leader perceptions of managing soldier behavioral health and associated factors. Military Psychology, 28(3), 147–161. https://doi.org/10.1037/mil0000101.
Matthews, R. A., Kath, L. M., & Barnes-Farrell, J. L. (2010). A short, valid, predictive measure of work–family conflict: item selection and scale validation. Journal of Occupational Health Psychology, 15(1), 75–99. https://doi.org/10.1037/a0017443.
Mckinlay, J. (1973). Social networks, lay consultation and help-seeking behavior. Social Forces, 51(3), 275–292. https://doi.org/10.1093/sf/51.3.275.
Murphy, D., Hunt, E., Luzon, O., & Greenberg, N. (2014). Exploring positive pathways tocare for members of the UK armed forces receiving treatment for PTSD: a qualitative study. European Journal of Psychotraumatology, 5, 21759. https://doi.org/10.3402/ejpt.v5.21759.
National Center for PTSD (2012). Using the PTSD Checklist (PCL). Retrieved from http://www.ptsd.va.gov/professional/pages/assessments/assessment-pdf/PCL-handout.pdf
Ouimette, P., Vogt, D., Wade, M., Tirone, V., Greenbaum, M. A., Kimerling, R., Laffaye, C., Fitt, J., & Rosen, C. (2011). Perceived barriers to care among veterans health administration patients with posttraumatic stress disorder. Psychological Services, 8(3), 212–223. https://doi.org/10.1037/a0024360.
Podsakoff, P. M., MacKenzie, S. B., Lee, J. Y., & Podsakoff, N. P. (2003). Common method biases in behavioral research: a critical review of the literature and recommended remedies. Journal of Applied Psychology, 88(5), 879. https://doi.org/10.1037/0021-9010.88.5.879.
Prochaska, J. O., & DiClemente, C. C. (1983). Stages and processes of self-change of smoking: toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51(3), 390–395. https://doi.org/10.1037//0022-006X.51.3.390.
Prochaska, J. O., DiClemente, C. C., & Norcross, J. C. (1992). In search of how people change: Applications to addictive behaviors. American Psychologist, 47(9), 1102–1114. https://doi.org/10.1037/0003-066X.47.9.1102.
Ray, E. B., & Miller, K. I. (1994). Social support, home/work stress, and burnout: Who can help? The Journal of Applied Behavioral Science, 30(3), 357–373. https://doi.org/10.1177/0021886394303007.
Sheehan, D. V., Harnett-Sheehan, K. K., & Raj, B. A. (1996). The measurement of disability. International Clinical Psychopharmacology, 11(3), 89–95.
Sherbourne, C. D., & Stewart, A. L. (1991). The MOS social support survey. Social Science & Medicine, 32(6), 705–714. https://doi.org/10.1016/0277-9536(91)90150-B.
Shumaker, S. A., & Brownell, A. (1984). Toward a theory of social support: closing conceptual gaps. Journal of Social Issues, 40(4), 11–36. https://doi.org/10.1111/j.1540-4560.1984.tb01105.x.
Sripada, R. K., Bohnert, A. S., Teo, A. R., Levine, D. S., Pfeiffer, P. N., Bowersox, N. W., et al. (2015). Social networks, mental health problems, and mental health service utilization in OEF/OIF National Guard veterans. Social Psychiatry and Psychiatric Epidemiology, 50(9), 1367–1378. https://doi.org/10.1007/s00127-015-1078-2.
Steele, L., Dewa, C., & Lee, K. (2007). Socioeconomic status and self-reported barriers to mental health service use. The Canadian Journal of Psychiatry, 52(3), 201–206. https://doi.org/10.1177/070674370705200312.
Tonidandel, S., & LeBreton, J. M. (2015). RWA web: a free, comprehensive, web-based, and user-friendly tool for relative weight analyses. Journal of Business and Psychology, 30(2), 207–216. https://doi.org/10.1007/s10869-014-9351-z.
Van der Doef, M., & Maes, S. (1999). The job demand-control (−support) model and psychological well-being: a review of 20 years of empirical research. Work and Stress, 13(2), 87–114. https://doi.org/10.1080/026783799296084.
Viswesvaran, C., Sanchez, J. I., & Fisher, J. (1999). The role of social support in the process of work stress: a meta-analysis. Journal of Vocational Behavior, 54(2), 314–334. https://doi.org/10.1006/jvbe.1998.1661.
Vogel, D. L., Wester, S. R., Wei, M., & Boysen, G. A. (2005). The role of outcome expectations and attitudes on decisions to seek professional help. Journal of Counseling Psychology, 52(4), 459. https://doi.org/10.1037/0022-0167.52.4.459.
Weathers, F. W., Litz, B. T., Herman, D. S., Huska, J. A., & Keane, T. M. (1993). The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. In annual meeting of the international society for traumatic stress studies, San Antonio, TX (Vol. 141, No. 7).
Wright, K. M., Cabrera, O. A., Bliese, P. D., Adler, A. B., Hoge, C. W., & Castro, C. A. (2009). Stigma and barriers to care in soldiers postcombat. Psychological Services, 6(2), 108–116. https://doi.org/10.1037/a0012620.
Zang, Y., Gallagher, T., McLean, C. P., Tannahill, H. S., Yarvis, J. S., & Foa, E. B. (2017). The impact of social support, unit cohesion, and trait resilience on PTSD in treatment-seeking military personnel with PTSD: the role of posttraumatic cognitions. Journal of Psychiatric Research, 86, 18–25. https://doi.org/10.1016/j.jpsychires.2016.11.005.
Zhao, X., Lynch, J. G., Jr., & Chen, Q. (2010). Reconsidering Baron and Kenny: myths and truths about mediation analysis. Journal of Consumer Research, 37, 197–206. https://doi.org/10.1086/651257.
Zinzow, H. M., Britt, T. W., Pury, C. L. S., Raymond, M. A., McFadden, A. C., & Burnette, C. M. (2013). Barriers and facilitators of mental health treatment seeking among active-duty army personnel. Military Psychology, 25(5), 514–535. https://doi.org/10.1037/mil0000015.
Zinzow, H. M., Britt, T. W., Pury, C. L., Jennings, K. S., Cheung, J. H., & Rayomd, M. A. (2015). Barriers and facilitators of mental health treatment-seeking in active duty soldiers with sexual assault histories. Journal of Traumatic Stress, 28(4), 289–297. https://doi.org/10.1002/jts.22026B.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Preparation of this manuscript was supported by Grant #W81XWH-11-2-0010 from the Department of Defense, administered by the U.S. Army Medical Research Acquisition Activity. The views expressed in this article are those of the authors and do not necessarily represent the official policy or position of the U.S. Army Medical Command or the Department of Defense. We would like to thank John Cryer, Fabio Delgado, and David Nege for serving as ombudsmen in the present study, and Mary Anne Raymond for her assistance in data collection.
Rights and permissions
About this article
Cite this article
Black, K.J., Britt, T.W., Zinzow, H.M. et al. The Role of Social Support in Treatment Seeking Among Soldiers. Occup Health Sci 3, 337–361 (2019). https://doi.org/10.1007/s41542-019-00044-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41542-019-00044-2