Abstract
We conducted a retrospective analysis of 221 subjects with 256 suspected gastrointestinal lesions from 2007 to 2015 to explore the detecting efficiency of dual-time-point fluorine-18 fludeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) and pathology examination. The abdominal delayed PET/CT was performed within 45 min of the conventional scan. The change in maximum standardized uptake value (ΔSUVmax) and morphological features of the suspected lesions between the conventional and dual-time-point PET/CT were compared. The sensitivity, specificity, positive predictive value, and negative predictive value (NPV) of conventional PET/CT were 81.6% (84/103), 56.2% (86/153), 55.6% (84/151), and 81.9% (86/105), respectively. Those of dual-time-point PET/CT were 94.1% (97/103), 78.4% (120/153), 74.6% (97/130), and 95.2% (120/126), respectively. There was a significant difference between the conventional and dual-time-point PET/CT (P < 0.005). The SUVearly and the %ΔSUVmax could not present more information in differential diagnoses, but the rate of tumors with increased SUVdelay accounted for 79.6% (82/103) and more than that of nonneoplastic lesions (15.5%, 29/187) (x 2 = 115.5, P < 0.01). Therefore, the dual-time-point 18F-FDG PET/CT had a higher sensitivity and NPV than the conventional PET/CT to detect gastrointestinal tumors. The constant morphology and increased SUVdelay help to detect the tumors and adding delayed imaging on the locality will be an effective method when we accidentally find a suspected gastrointestinal tumor on the conventional PET/CT images.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
18F-FDG PET/CT had a superior advantage in detecting gastrointestinal tumors over other conventional imaging examinations, including gastrointestinal imaging (GI), computed tomography (CT), and magnetic resonance imaging (MRI) [1, 2]. Although 18F-FDG PET/CT imaging was sensitive to the detection of hypermetabolic gastrointestinal tumors, the factors affecting tumor detection were substantial, such as gastrointestinal physiologic uptake of FDG, gastric emptying and contraction, gastrointestinal peristalsis, breathing exercises, and the gastrointestinal contents, which were often considered as suspected lesions [1, 3]. Many scholars have conducted various studies in order to reduce the adverse effects of those factors and increase the detecting efficiency of gastrointestinal tumors with 18F-FDG PET/CT, and the dual-time-point 18F-FDG PET/CT was one of them [3,4,5,6,7]. The dual-time-point PET scanning was used very early on to differentially diagnose benign and malignant lesions of many organs [8,9,10]; in particular, PET/CT has played an important role. Studies, such as Miyake’s study, showed that this technique was useful for differentiating physiologic uptake from pathological uptake [11]; almost all of the studies were focused on the ΔSUVmax rather than the morphological change [3, 11, 12]. We paid attention to both the morphological change and the ΔSUVmax to explore the detecting efficiency of gastrointestinal tumors with dual-time-point PET/CT imaging. In this study, we retrospectively analyzed 221 subjects with 256 gastrointestinal suspected lesions that had dual-time-point 18F-FDG PET/CT imaging from 2007 to 2015 to assess the clinical value of the dual-time-point imaging.
2 Experimental
2.1 Subjects
We retrospectively collected 221 subjects who had both PET/CT imaging and pathological data (79 women and 142 men, aged 59.1 ± 12.9 years old) from 2007 to 2015. There were 256 suspected gastrointestinal lesions found in their baseline (conventional) PET/CT imaging, including 40 suspected gastric lesions, 61 suspected small intestinal lesions, and 155 suspected colorectal lesions, and the delayed imaging was subsequently carried out on the same sections where the suspected lesions were located (within 2 h).
The suspected lesions were defined as gastric bowel wall thickening, mass, or nodule in the CT images, and/or an increased focal radioactive area in the PET images. All of the subjects accidentally found the suspected gastrointestinal lesions on their PET/CT images for other purposes or their conventional PET/CT imaging for gastrointestinal lesions did not clearly show the tumors. The subjects who showed a clear and definite gastrointestinal mass or wall thickening in the baseline imaging were excluded from this study for their determined diagnosis as tumors.
2.2 PET/CT procedures
All of the subjects underwent dual-time-point imaging on a PET/CT scanner (Discovery STE, GE, USA) after an intravenous injection of 18F-FDG (Shanghai Ansheng Kexing Pharmaceutical Co., Ltd., radioactive and chemical purity ≥95%). The images were analyzed and post-processed on the workstation (Xeleris 6.0 and AW 4.3, GE, USA).
All of the subjects fasted for at least 6 h, and their blood glucose levels were <8.3 mmol/l. Then, they were intravenously administrated 18F-FDG (4.44–5.55 MBq/kg), followed by resting for approximately 60 min before the PET/CT examination. During the resting period, they drank 500–750 ml of water and urinated, and they were asked to drink another 250 ml of water immediately before scanning. Subjects were asked to be in the supine position with their arms naturally on the side of their bodies and eupnea during the PET and CT acquisitions. Whole-body PET data were obtained in three-dimensional (3-D) mode, which used CT data for attenuation correction with the scan range from the upper thigh to the skull vertex (a total of 6–8 sections, acquired 2 min/section). CT acquisition was performed with the tube voltage of 140 kV, the tube current of 160 mA, the collimation of 16 × 1.25 mm, and the pitch of 1.375. The CT images were reconstructed with the slice thickness of 3.75 mm.
Delayed imaging followed two modes: (A) For suspected gastric lesions, subjects continued to fast and wait for 45 min (about 2 h since intravenous injection), and then they drank 250–500 ml of water just before the delayed-phase upper abdominal imaging; and (B) for suspected intestinal lesions, subjects waited for about 45 min and were allowed to eat or drink or defecate freely before the delayed-phase abdominal local PET/CT scan. Their arms were raised above their heads during the delayed scans.
2.3 Image analysis
These subjects and their suspected lesions were chosen by the resident, and the diagnosis based on the PET/CT imaging was made by two nuclear medicine doctors with 8 years of experience with coming to a consensus about abdominal PET/CTs. The image reading procedure follows:
First, the doctors read the baseline PET/CT images and distinguished them as positive or negative for gastrointestinal tumors, including cancer, adenoma, lymphoma, or other tumors. The criteria of suspected gastrointestinal tumors in the baseline PET/CT imaging were: (1) single or multiple nodular or massive high-radioactive regions in the PET images; or (2) local gastric or intestinal wall thickening or dense lumen, but they were not sure if they were peristalsis artifacts, feces, or lesions on the CT images. This step was in accordance with conventional PET/CT imaging.
Second, the doctors read the baseline and delayed PET/CT images and distinguished them as positive or negative. The observation of the delayed PET/CT images was mainly for the morphologic change and SUVmax relative to the baseline suspected signs. The positive PET signs referred to the constant high-radioactive areas on the focal images, with unchanged or increased SUVmax. The negative PET signs referred to the high-radioactive areas that were distorted or disappeared with decreased SUVmax. The positive CT signs referred to unchanged gastrointestinal wall thickening or dense lumen without the image artifacts. The negative CT signs referred to the suspected signs obviously deformed and shifted, or findings without wall thickening or dense lumen.
The suspected baseline lesions with one or both of the positive PET and CT signs were classified as the positive group of conventional or dual-time-point PET/CT, respectively. The others were classified as the negative group.
All of the aforementioned image readings were compared to the pathological results. The pathological results were retrieved based on endoscopic biopsies in the month after the dual-time-point PET/CT imaging.
2.4 Statistics
The McNemar test, Kappa test, and Chi-square test were used to evaluate the efficiency of detecting gastrointestinal tumors with the conventional and the dual-time-point PET/CT imaging. Using the pathological results as the reference, the diagnostic accuracy of the image reading was calculated, including sensitivity, specificity, PPV, and NPV. Student’s t test (for %ΔSUV) and Chi-square test (for rate of increased SUVdelay) were used to determine the statistical significance between the tumors and nonneoplastic lesions, and between the cancer and adenoma. %ΔSUV = (SUVdelay − SUVearly)/SUVearly * 100%.
The statistical analysis was performed using SPSS19.0 (IBM, USA). P < 0.05 was considered to be statistically significant.
3 Results
3.1 Pathology comparison
There were 256 suspected gastrointestinal lesions in 221 subjects that were pathologically diagnosed, and 103 (40.2%) suspected lesions were confirmed as tumors, while the others (59.8%) were confirmed as inflammation or normal. The data for the pathological diagnoses are listed in Table 1.
The determination of the tumors and the nonneoplastic lesions based on the diagnostic criteria of Sect. 2.3 between the dual-time-point and conventional PET/CT is shown in Table 2.
The McNemar test: x 2 = 5.06 and P < 0.05, and the Kappa test: K = 0.3811, V(K) = 64.9561 × 10−3, U = 1.4953, and P > 0.05, which meant the two methods were inconsistent.
The diagnostic accuracy is shown in Table 3 using pathologic results as the reference.
For conventional PET/CT, the sensitivity, specificity, PPV, and NPV were 81.6% (84/103), 56.2% (86/153), 55.6% (84/151), and 81.9% (86/105); and for dual-time-point PET/CT, the results were 94.1% (97/103), 78.4% (120/153), 74.6% (97/130), and 95.2% (120/126), respectively. The Chi-square test of the accuracy from the 2 groups of images with positive lesions was x 2 = 10.9857 and P < 0.005, which meant that the difference of the diagnoses were statistically significant and the diagnosis from the dual-time-point PET/CT imaging had the higher accuracy and NPV.
3.2 SUV comparison
As shown in Table 4 and 5, the SUVbaseline of tumors was higher than that of the nonneoplastic lesions and the increased SUVdelay of tumors was higher than that of nonneoplastic lesions. But the %ΔSUVmax did not show a significant difference between the tumors and the nonneoplastic lesions with an increased SUVdelay. While SUVearly, the rate and the %ΔSUVmax did not show a statistical difference between the malignant tumor (MT) and the benign tumor groups.
4 Discussion
18F-FDG PET/CT is sensitive to the detection of gastrointestinal tumors, and we often incidentally find gastrointestinal tumors or suspected lesions in our daily work; however, the physiological FDG uptake, peristalsis, and contents of the gastrointestinal tract easily produce artifacts that may confuse or cover up lesions and decrease the efficiency of detecting tumors. The gastrointestinal physiological FDG uptake commonly manifests the sheet, strip, or multiple segmental high-radioactive areas on PET images and has no gastrointestinal wall thickening and mass on CT images. If there was a local lump-like high-radioactive area on PET images that was suspected to be focal gastrointestinal wall thickening, lumps, nodules, luminal stenosis, and serosal infiltration, it would be diagnosed as a tumor or a suspected lesion (Figs. 1, 2, 3). As for conventional PET/CT imaging, these suspected lesions were often judged on the basis of the conventional imaging signs and by a doctor’s experience to a great extent.
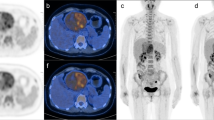
A 53-year-old woman with abdominal discomfort for 5 months. The purpose of PET/CT imaging was to screen for tumors. The early PET/CT imaging revealed a nodular high-radioactive area (SUVearly = 7.8) in the colonic hepatic flexure and the corresponding colon with seemingly irregular wall thickening having the interference of feces on CT images (a, b). The delayed PET/CT imaging displaying clearly the shape and SUVmax of lesion unchanged (SUVdelay = 7.8) (c, d). Both of the conventional and dual-time-point PET/CT conclusions were positive and finally confirmed as colonic carcinoma by colonoscopy biopsy and pathology
A 42-year-old woman with abdominal discomfort and irregular menstruation about 4 months. The early PET/CT images demonstrating the high FDG uptake and the suspected thickening of ileocecus (SUVmax = 5.2) (a, b). The delayed images showing the ileocecal cavity had expanded, the colonal wall was soft without thickening, and the area of high FDG uptake was fusing with the liquid of ileocecal cavity (SUVmax = 5.1) (c, d). The conventional PET/CT diagnosed as positive and the dual-time-point PET/CT diagnosed as negative. The colonoscopy suggested no tumor there
A 62-year-old man with edema of lower limbs about 2 months, and CA125, CA199, and CEA above normal. The early PET/CT showing a focal high FDG uptake and the local disorder small intestinal structure in the left upper abdominal (a). The early MIP displaying the nodular increased FDG uptake (arrow in b) lies in the left upper abdominal and ileocecal. The delayed imaging revealing the increased FDG uptake disappeared (c, d). The conventional PET/CT diagnosed as positive in the jejunum and negative in the ileocecus, while the dual-time-point PET/CT diagnosed as negative in both the jejunum and the ileocecus. There was confirmed as no lesion in jejunum and ileocecus by small intestinal and colonal endoscopy
In order to reduce the interference of the physiological gastrointestinal FDG uptake and gastrointestinal wall artifacts to improve the detecting efficiency, scholars carried out some explorations; for example, using positive contrast agent (1–2% meglumine diatrizoate solution) or negative contrast agent (2.5% mannitol diluent), or even a retention enema to induce gastrointestinal cavity expansion [4, 5]; using drugs to reduce gastrointestinal peristalsis [6]; and using a foaming agent to dilate the stomach and colon [7] were somewhat effective, but they were not easily done and were not appropriate for every patient, especially the old and infirm.
In our study, we only added delayed imaging to the subjects whose conventional PET/CT images were found to have the suspected gastrointestinal tumors. The dual-time-point PET/CT imaging provided favorable results to judge the suspected gastrointestinal lesions by focusing on both the morphological and the SUVmax changes. Gastrointestinal peristalsis always brought us image artifacts in the conventional PET/CT examinations, but it could be used to distinguish the gastrointestinal tumors from the nonneoplastic lesions based on the dual-time-point PET/CT imaging because the neoplasms retained their shape (Fig. 1), while the nonneoplastic lesions or artifacts were distorted or moved on the delayed CT images, and the synchronous changes appeared on the PET images with the SUVmax increased or decreased (Figs. 2, 3). Then, we analyzed the morphological changes of the gastrointestinal lesions to determine whether tumors existed. Conventional PET/CT imaging diagnosis was made by high-FDG-uptake lesions on the PET images and the mass effect on the CT images according to the doctor’s experience. However, the diagnosis on the dual-time-point PET/CT imaging was made on the basis of more objective morphological changes and ΔSUVmax, which should ensure a more steady and reliable diagnosis for the suspected gastrointestinal lesions. The different levels of accuracy of these suspected lesions with the conventional and the dual-time-point PET/CT, respectively, are shown in Tables 2 and 3. Compared to conventional PET/CT imaging, the sensitivity, specificity, PPV, and NPV of the dual-time-point PET/CT were 94.1% (97/103), 78.4% (120/153), 74.6% (97/130), and 95.2% (120/126), respectively, and they are also higher than the results of Weston’s study, which were determined from conventional PET/CT imaging [13]. With dual-time-point PET/CT imaging, almost all of the tumors were detected and the negative lesions would be determined to be mostly be normal or as a result of inflammation. In addition, there were a few tumors that were too small to display abnormal signs and they were lost by dual-time-point PET/CT [13, 14].
The SUVearly is a important index to reveal the tumors or other lesions, and the tumorous SUVearly was often higher than the nonneoplastic SUVearly, but the SUVearly cannot be applied mechanically to judge the tumors and nonneoplastic lesions because the numerical values were so overlapped (2.1–21.8 for tumors and 2.0–19.4 for nonneoplastic lesions) in spite of the statistical difference (P < 0.01) (Table 4). The %ΔSUVmax of the delayed PET/CT imaging was often used to differentiate the benign and malignant tumors by many scholars, and some studies considered that if the %ΔSUVmax increased to 10% or more than 30%, it would support malignant lesions and the decreased SUVmax would support the benign lesions [12, 15,16,17], but the intestinal physiological FDG uptake could also increase significantly from the early to the delayed phase [3]. In our study, the %ΔSUVmax of lesions with increased SUVdelay was 26.9% to 28.0% (Tables 4, 5). There was no statistical difference between the tumors and the nonneoplastic lesions (P = 0.412) as well as between the MTs and adenomas (P = 0.451). This meant that there were a lot of overlapping results and there was no level of difference among the MTs, the benign tumors, and the nonneoplastic lesions with increased SUVdelay, so there also was a limited value in judging the properties of the gastrointestinal lesions. However, the rate of tumors with increased SUVdelay (79.6%, 82/103) was significantly higher than that of the nonneoplastic lesions (15.5%, 29/187) (x 2 = 115.5, P < 0.01), which would help us to confirm the existence of gastrointestinal tumors and improve the detection rate, and also tell us which lesions with decreased SUVdelay would be mostly nonneoplastic lesions. With the rate of adenoma with increased SUVdelay (37/48, 77.7%) being similar to that of the MTs (81.8%, 45/55) (x 2 = 0.997, P > 0.50), it may mean there is a similar mechanism between the adenoma and the adenocarcinoma and it supports the high cancerated rate of intestinal adenoma.
In our study, we operated the dual-time-point PET/CT scan without special bowel preparation (except for the conventional fast and drinking water) and we detected the tumors up to 94.1% (97/103) and excluded about half of the suspected lesions (49.2%, 126/256) with the high NPV (95.2%). In our daily work, we believe that only the stomach cavity needs to be expanded and that the intestines may not need to be expanded for two reasons: first, because of the low morbidity of the small intestinal and the bad effect of filling the colonic lumen without cleaning, and second, the dual-time-point PET/CT could distinguish most of the gastrointestinal peristalsis artifacts and the impact of feces. Some scholars actually think that the intestinal preparation may have increased physiological FDG uptake and influenced the conventional effect [18, 19], and the use of meglumine diatrizoate or mannitol diluent may spur some elderly patients who are prone to diarrhea, and the situation may even appear in the process of scanning. Drinking water could expand the stomach adequately, hydrate the body, speed up the excretion of FDG, and reduce the radioactive background of the body, so the delay in imaging is a simple, convenient, and safe additional measures.
Even with the high sensitivity and NPV in our study, there were still six false negative lesions (4.8%, 6/126), including early flat gastric lymphoma, early gastric cancer, rectal cancer, and small colonic adenomatous polyps; of course the rate may gradually rise as there is a longer duration of follow-up. Because some of the lesions were so small and early stage or of some pathologic types (gastric signet ring cell carcinoma) and had low FDG uptake, it increased the difficulty in checking them out and caused them to be missed on the PET/CT images. Therefore, gastrointestinal endoscope checking may become an important supplemental method for suspected lesions on PET/CT images, and it could easily be used to obtain the biopsy pathology of positive lesions [20]. With the help of the endoscope, the duty of PET/CT in determining whether lesions exist or not is more important than distinguishing the pathological type.
Adding a delay to PET/CT imaging to observe the ΔSUV and morphological changes of the gastrointestinal suspected lesions means we pay low inputs of time and labor to simultaneously obtain high outputs of imaging diagnoses. We will help more patients get the appropriate examination and treatment in time with the high outputs, reduce the need for some other imaging scans, and save the false-positive crowd from unnecessary stress.
5 Conclusion
The dual-time-point 18F-FDG PET/CT imaging had a higher sensitivity and NPV than conventional PET/CT imaging in detecting gastrointestinal tumors. The constant morphology and increased SUVdelay were helpful in detecting tumors, while the SUVearly and %ΔSUVmax were of limited value in differentiating them for the overlapped SUVearly and the proximate %ΔSUVmax between the tumors and the nonneoplastic lesions. Dual-time-point 18F-FDG PET/CT imaging, as a kind of effective means of detecting gastrointestinal tumors, has the unique advantage of sensitivity, accuracy, convenience, safety, noninvasiveness, and comprehensive evaluation in detecting gastrointestinal tumors. It will be an advisable choice to add a delay to PET/CT imaging when we occasionally find a suspected gastrointestinal lesion on conventional PET/CT images.
References
J.H. Song, J.H. Zhao, X. Chen et al., Evaluation of the primary lesion detection in colorectal carcinoma with 18F-FDG PET-CT. Chin. J. Gastrointest. Surg. 12, 174–177 (2009). doi:10.3760/cma.j.issn.1671-0274.2009.02.027. (in Chinese)
J. Czernin, M. Allen-Auerbach, H.R. Schelbert, Improvements in cancer staging with PET/CT: literature-based evidence as of September 2006. J. Nucl. Med. 48(suppl 1), 78S–88S (2007)
A. Toriihara, K. Yoshida, I. Umehara et al., Normal variants of bowel FDG uptake in dual-time-point PET/CT imaging. Ann. Nucl. Med. 25, 173–178 (2011). doi:10.1007/s12149-010-0439-x
X.J. Cui, N. Fang, Y.L. Wang et al., The effect of cleaning and retention enema on the diagnosis of locally hypermetabolic lesions in colorectum using 18F-FDG PET/CT. Acta Academiae Medicinae Qingdao Universitatis 45, 49–51 (2009). doi:10.3969/j.issn.1672-4488.2009.01.018. (in Chinese)
P. Veit, C. Kühle, T. Beyer et al., Whole body positron emission tomography/computed tomography (PET/CT) tumour staging with integrated PET/CT colonography: technical feasibility and first experiences in patients with colorectal cancer. Gut 55, 68–73 (2006). doi:10.1136/gut.2005.064170
H.B. Wu, Z.H. Huang, Q.S. Wang et al., Several methods for eliminating physiological accumulation of 18F-FDG in the stomach and intestine. Chin. J. Nucl. Med. 22, 235–236 (2002). doi:10.3760/cma.j.issn.2095-2848.2002.04.017. (in Chinese)
L. Filippi, M. D’Arienzo, F. Scopinaro et al., Usefulness of dual-time point imaging after carbonated water for the fluorodeoxyglucose positron emission imaging of peritoneal carcinomatosis in colon cancer. Cancer Biother. Radiopharm. 28, 29–33 (2013). doi:10.1089/cbr.2012.1179
H. Zhuang, M. Pourdehnad, E.S. Lambright et al., Dual time point 18F-FDG PET imaging for differentiating malignant from inflammatory processes. J. Nucl. Med. 42, 1412–1417 (2001)
A. Matthies, M. Hickeson, A. Cuchiara et al., Dual time point 18F-FDG PET for the evaluation of pulmonary nodules. J. Nucl. Med. 43, 871–875 (2002)
R. Kumar, V.A. Loving, A. Chauhan et al., Potential of dual-time-point imaging to improve breast cancer diagnosis with (18)F-FDG PET. J. Nucl. Med. 46, 1819–1824 (2005)
K.K. Miyake, Y. Nakamoto, K. Togashi, Dual-time-point 18F-FDG PET/CT in patients with colorectal cancer: clinical value of early delayed scanning. Ann. Nucl. Med. 26, 492–500 (2012). doi:10.1007/s12149-012-0599-y
J. Cui, P. Zhao, Z. Ren et al., Evaluation of dual time point imaging 18F-FDG PET/CT in differentiating malignancy from benign gastric disease. Medicine 94, e1356 (2015). doi:10.1097/MD.0000000000001356
B.R. Weston, R.B. Lyer, W. Qiao et al., Ability of integrated positron emission and computed tomography to detect significant colonic pathology: the experience of a tertiary cancer center. Cancer 116, 1454–1461 (2010). doi:10.1002/cncr.24885
E. Shmidt, V. Nehra, V. Lowe et al., Clinical significance of incidental [18F]FDG uptake in the gastrointestinal tract on PET/CT imaging: a retrospective cohort study. BMC Gastroenterol. 16, 125 (2016). doi:10.1186/s12876-016-0545-x
A. Zade, N. Purandare, V. Rangarajan et al., Role of delayed imaging to differentiate intense physiological 18F FDG uptake from peritoneal deposits in patients presenting with intestinal obstruction. Clin. Nucl. Med. 37, 783–785 (2012). doi:10.1097/RLU.0b013e31824c5e7d
Y.E. Huang, Y.J. Huang, M. Ko et al., Dual-time-point 18F-FDG PET/CT in the diagnosis of solitary pulmonary lesions in a region with endemic granulomatous diseases. Ann. Nucl. Med. 30, 652–658 (2016). doi:10.1007/s12149-016-1109-4
D. Kadaria, D.S. Archie, I. SultanAli et al., Dual time point positron emission tomography/computed tomography scan in evaluation of intrathoracic lesions in an area endemic for histoplasmosis and with high prevalence of sarcoidosis. Am. J. Med. Sci. 346, 358–362 (2013). doi:10.1097/MAJ.0b013e31827b9b6d
D.G. Meng, X.G. Sun, G. Huang et al., Comparison of the effect of positive and negative oral contrast agents on delineation and 18F-FDG uptake of gastrointestinal tract. Chin. J. Nucl. Med. 30, 272–275 (2010). doi:10.3760/cma.j.issn.0253-9780.2010.04.014. (in Chinese)
J.D. Soyka, K. Strobel, P. Veit-Haibach et al., Influence of bowel preparation before 18F-FDG PET/CT on physiologic 18F-FDG activity in the intestine. J. Nucl. Med. 51, 507–510 (2010). doi:10.2967/jnumed.109.071001
S.B. Ahn, D.S. Han, J.H. Bae et al., The miss rate for colorectal adenoma determined by quality-adjusted, back-to-back colonoscopies. Gut Liver 6, 64–70 (2012). doi:10.5009/gnl.2012.6.1.64
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Song, JH., Zhao, JH., Xie, XQ. et al. Improving the detecting efficiency of suspected gastrointestinal tumors with dual-time-point 18F-FDG PET/CT. NUCL SCI TECH 28, 138 (2017). https://doi.org/10.1007/s41365-017-0294-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41365-017-0294-8