Abstract
Healthcare workers’ mental health has been a topic of growing interest. However, despite the significant prevalence of mental health disorders in this population, there are many barriers to care. The recent development of e-Health might present solutions to these challenges, allowing the prevention and early detection of mental health disorders. This paper aims to provide an overview of the existing research on e-Health applications focused on healthcare workers’ mental health. A scoping review was conducted based on PRISMA-ScR guidelines. A total of 6 databases (PubMed, Science Direct, Web of Science, Scopus, IEEE Explore, ACM Digital Library) were searched from inception to December 2022 without limits on the dates and types of publications. Studies were included in the review if they had incorporated e-Health in any application to healthcare workers’ mental health and had been published in English, Portuguese, or Spanish. In addition, publication-related information, mental health disorders studied, population profession, method of recruitment, and type of e-Health intervention or usage were extracted from each study. A total of 7 articles were included in this review. Two types of studies were found. The first type of study was strictly observational, while the other involved interventions utilizing e-Health to promote mental health improvement. There is a small number of studies pointing to a gap in the literature on this topic, with a necessity of further studies, considering studies design that mitigates the heterogeneities observed in this review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Healthcare workers’ mental health disorders are more prevalent than the general population, with higher rates of depression, anxiety, burnout, and substance misuse disorders (Lai et al., 2020; Ripp et al., 2020), (Bhugra et al., 2019). Moreover, in situations of high stress, such as in the recent pandemic, there are studies pointing to an early manifestation of psychological distress among this population (Lai et al., 2020). This situation is especially troublesome when taken into account the low rates of search for mental healthcare in this population (Givens & Tjia, 2002) and the potential positive impact of early interventions (Greenberg et al., 2020), (Iversen et al., 2008). This is potentialized by the low rates of self-care behaviors among these professionals.
With this in mind, it is paramount to search for initiatives toward early detection and to design effective interventions for the improvement of the care of the mental health of healthcare workers. The initiatives must be easy to access and potentially be available 24/7. e-Health apps are one of the tools that can be utilized with these objectives in mind, and they are becoming increasingly used to assess mental health disorders, granting ease of access and usage (Piers et al., 2023; Stentzel et al., 2023; Thabrew et al., 2018), and with interesting applications on vulnerable populations, reducing exclusion with a broader provision of information and opportunity for self-management of care(Pierce et al., 2023; Wilson et al., 2021).
There is also an increasing number of studies that are focused on vulnerable populations’ mental healthcare utilizing e-Health initiatives (Chen et al., 2021; Currie et al., 2022; Fiol-DeRoque et al., 2021; Golden et al., 2021; Goodday et al., 2021; Taylor et al., 2022; Thabrew et al., 2018; Trottier et al., 2022; Ungar et al., 2022; Wood et al., 2017; Xie et al., 2020); however, there is a lack of studies with large populations and consistent findings on the impact of the interventions (Andrades-González et al., 2021; Coumoundouros et al., 2022; Firth et al., 2017; Kerst et al., 2020; Piers et al., 2023; Souza do Nascimento et al., 2023; Stratton et al., 2017; Xie et al., 2022). Although there are studies focused on e-Health initiatives’ impact on healthcare workers’ mental health (Bégin et al., 2022; Drissi et al., 2021; Robins-Browne et al., 2022), there has not been a systematic approach to investigate healthcare workers’ mental health disorders and the usage of e-Health apps. The results are limited due to the population size and diverse methodologies.
To assess and review, through a systematic approach, the authors defined a protocol and conducted a scoping review of the literature. We aimed to identify what research was done in this area and the gaps in this area of knowledge.
Materials and Methods
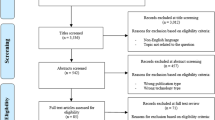
A scoping review was conducted to identify what research was done in the field of healthcare workers’ mental health disorders involving the usage of e-Health. Our protocol was drafted using the Preferred Reporting Items for Systematic Reviews and Meta-analysis Protocols (PRISMA-P), which was revised by the research team.
For the purposes of this study, we considered e-Health/m-Health interventions or assessments that did not involve human mediation. We aimed to determine what kind of mental health disorders were investigated, the types of interventions made, and their outcomes, systematically mapping the research done in this area and identifying any existing gaps in knowledge.
Information Sources
A total of 6 databases (PubMed, Science Direct, Web of Science, Scopus, IEEE Explore, and ACM Digital Library) were assessed. The search terms had to be included in either the title or abstract.
Search Strategy
In the search term, premises 1–3 were connected by an AND; alternatives in wording and spelling were connected within each premise by an OR.
-
1.
Mental Health OR Depression OR Anxiety OR Burnout OR Stress
-
2.
Healthcare worker* OR Healthcare professional* OR Health care worker* OR Health care professional*
-
3.
App OR e-Health OR m-Health OR eHealth OR mHealth
No supplementation of the database search would be done by referencing tracking or further searches. Duplicated papers that were found on the searches were excluded.
Selection of Sources of Evidence
The final protocol was made with the participation of all members. MT searched for what types of evidence were available on this topic. All participants worked on the selection of the articles per the keywords selected and were divided into pairs (LT and EH, AS and MT, and FS and HT). Three reviewers (FS, HT, and MT) evaluated the titles, three reviewers (LT, EH, and AS) evaluated abstracts, and all participants assessed the full text of all publications found in our search. All reviewers screened the same publications, discussed their results, and amended the screening process. Any disagreements on study selection or data extraction were resolved through consensus and discussion with other reviewers.
Eligibility Criteria
-
1.
The study utilized e-Health or m-Health tools to evaluate or make interventions related to mental health disorders in healthcare workers.
-
2.
If the population included non-healthcare workers, it would only be included if there were separate data for the healthcare workers’ population.
-
3.
The study was published in English, Portuguese, or Spanish.
Data Charting Process
EH developed the initial draft of the data charting process, and all participants contributed to the final version of the data charting. A form was made with all the relevant information to the study and was updated during the data collection phase after discussions of the findings. In addition, EH and LT reviewers independently charted the data and discussed the results.
Publication-related information, mental health disorders studied, population profession, method of recruitment, and type of e-Health intervention or usage were extracted from each study.
Results
Selected Studies
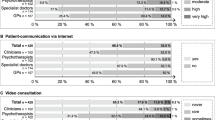
A total of eight studies were included by the end of our selection (Fig. 1).
Study Characteristics
The populations included in the studies were heterogeneous. There was a female predominance in all the studies, and there was not a homogenous distribution of the healthcare workers’ professions in the included studies. The results were also heterogeneous, with four being strictly observational, investigating the prevalence of mental health disorders and psychological distress, and four with proposed interventions.
Study Outcomes
For the included studies, we identified six types of mental health disorders and psychological distress investigated: anxiety, stress, depression, burnout, post-traumatic stress disorder, and substance abuse.
e-Health and Anxiety (Table 1)
The studies utilized three scales to investigate anxiety (DASS-21, GAD-2, and GAD-7).
The number of participants was heterogeneous, varying between 21 and 1803. The largest study (Chen et al., 2021) only included nurses and focused on different areas in China. In contrast, the one with the fewest participants (n = 21) focused on healthcare workers, not limited to nurses, in a single hospital in Canada. There was a substantial preponderance of female participants in the studies that provided gender data (Chen et al., 2021; Currie et al., 2022; Fiol-DeRoque et al., 2021; Taylor et al., 2022; Trottier et al., 2022).
Four studies investigated anxiety levels after an intervention. The first one involved DBT and mindfulness techniques (Fiol-DeRoque et al., 2021) and showed no difference in anxiety levels compared to a control population that received an app with general recommendations about mental healthcare. One involved an app-based Yoga of Immortals intervention (Currie et al., 2022), which showed a significant decrease in anxiety levels compared to the control population, who received a general well-being orientation. Another (Taylor et al., 2022) compared digital mindfulness-based self-help intervention with a control group that utilized the NHS digital platform for work-related stress, Moodzone, showing a positive impact of the intervention. The last one (Trottier et al., 2022) utilized an online guided transdiagnostic intervention including cognitive-behavioral interventions targeted to healthcare workers during the COVID-19 pandemic, showing significant impact after the intervention and at the 1-month follow-up.
e-Health and Stress (Table 2)
The studies utilized two scales to investigate stress (DASS-21 and IES-R). Three studies were observational, and one pointed to high-stress levels in the participants (Chen et al., 2021) and non-critical-care ward nurses compared to critical-care ward nurses (Xie et al., 2020) However, only one of these studies had stress prevalence (Chen et al., 2021), while the other three only focused on the median score of the scales. Two studies proposed investigating stress after an intervention, one using an app with DBT and mindfulness techniques (Fiol-DeRoque et al., 2021), showing no significant difference between the intervention and control group, and another utilizing digital mindfulness-based self-help intervention (Taylor et al., 2022), showing significant differences, with decreased mean scores on the intervention group.
e-Health and Depression (Table 3)
Six studies investigated depression, utilizing three scales (DASS-21, PHQ-9, and a modified version of PHQ-9). In the modified version of PHQ-9, the authors suppressed the suicidality question. Most of the studies recruited participants from one different country each (Chen et al., 2021; Fiol-DeRoque et al., 2021; Golden et al., 2021; Taylor et al., 2022; Trottier et al., 2022). The five studies that presented gender information had a notable difference in gender distribution, with a predominantly female enrolled population (83.3–97.7%) (Chen et al., 2021; Currie et al., 2022; Fiol-DeRoque et al., 2021; Taylor et al., 2022; Trottier et al., 2022). Four studies investigated depression after an intervention, one using an app with DBT and mindfulness techniques (Fiol-DeRoque et al., 2021), showing no significant difference between the groups. However, all the other studies showed decreased levels of depression after the intervention.
The study that utilized app-based Yoga of Immortals intervention (Currie et al., 2022) and the one that utilized digital mindfulness self-help intervention showed decreased levels of depression in the intervention group compared to the control.
The clinical trial study that did not utilize a control group (Trottier et al., 2022) also showed decreased levels of depression after the intervention and at the 1-month follow-up.
e-Health and Burnout (Table 4)
Only two studies evaluated burnout symptoms, utilizing two different methods, the Maslach Burnout Inventory Human Services Survey and the ProQOL Burnout subscale. One study was a clinical trial (Fiol-DeRoque et al., 2021), proposing an intervention using an app with DBT and mindfulness techniques, showing no significant difference after the intervention. The other was a cross-sectional study, and the comparison between burnout prevalence in these studies pointed to a considerable disparity (61.8%–37.2% (Fiol-DeRoque et al., 2021), (Wood et al., 2017)).
e-Health and Post-Traumatic Stress Disorder (Table 5)
Only one study evaluated post-traumatic stress disorder. The scale utilized by this study was the Post-Traumatic Disorder Checklist (PCL-5), with a population recruited from Ontario, Canada. The sample size was small (n = 21), predominantly female (95.2%), and had a hospital work setting (76.2%). This study suggested an important prevalence of PTSD (95.2%) (Trottier et al., 2022).
e-Health and Substance Use and Abuse (Table 6)
Only one study evaluated substance use and abuse, and it was limited to investigating alcohol misuse, utilizing the AUDIT-C scale, with a population exclusively recruited from a single hospital in the USA, with data suggesting a significant rate of alcohol misuse (49.7%) (Golden et al., 2021).
Discussion
This scoping review identified eight studies that examined the correlation between e-Health and healthcare workers’ mental health disorders. Among the studies that included a control group and a follow-up, only two reported a positive impact on the intervention group (Currie et al., 2022; Taylor et al., 2022).
The studies focused mostly on anxiety and depression (5; 62.5%), followed by stress (4; 50%). Other outcomes measured were burnout (2; 25%), post-traumatic stress disorder, and substance use and abuse (1; 12.5%). The studies included different countries and heterogeneous population characteristics and in the size of the samples investigated.
Our scoping review has some limitations. Despite the potential limitation caused by the search structure, we maintained this decision, so the systematics of this scoping review were maintained. There is also a lack of expert consensus on this topic and of reviews with the usage of e-Health apps on this population. The low number of studies, the heterogeneity of both study populations, and the type of psychological distress and mental disorders investigated impair our analysis. There is also the possibility that e-Health initiatives are made with this population, but few studies have been published with this scope in mind, given its particularity. Another potential limitation of this scoping review is a bias of the original publications, given a known difficulty within this population to seek help and participate in these studies.
Conclusions
From this scoping review of the literature, given the search parameters that we previously decided to utilize, we derive the following conclusions:
-
1.
There is a lack of evidence correlating e-Health tools and healthcare workers’ mental health disorders. Therefore, further studies are necessary to thoroughly assess the impact of e-Health initiatives on healthcare workers’ mental health disorders.
-
2.
The evidence found in the literature points to a need for further studies, considering studies design that mitigates the heterogeneity observed in this review.
-
3.
Clinical trials can help further understand e-Health interventions’ impact on this population.
References
Andrades-González, I., Romero-Franco, N., & Molina-Mula, J. (2021). e-Health as a tool to improve the quality of life of informal caregivers dealing with stroke patients: Systematic review with meta-analysis. Journal of Nursing Scholarship : An Official Publication of Sigma Theta Tau International Honor Society of Nursing, 53(6), 790–802. https://doi.org/10.1111/JNU.12699
Bégin, C., Berthod, J., Martinez, L. Z., & Truchon, M. (2022). Use of mobile apps and online programs of mindfulness and self-compassion training in workers: A scoping review. Journal of Technology in Behavioral Science, 7(4), 477–515. https://doi.org/10.1007/S41347-022-00267-1
Bhugra, D., Sauerteig, S. O., Bland, D., Lloyd-Kendall, A., Wijesuriya, J., Singh, G., Kochhar, A., Molodynski, A., & Ventriglio, A. (2019). A descriptive study of mental health and wellbeing of doctors and medical students in the UK. International Review of Psychiatry, 31(7–8), 563–568. https://doi.org/10.1080/09540261.2019.1648621
Chen, X., Arber, A., Gao, J., Zhang, L., Ji, M., Wang, D., Wu, J., & Du, J. (2021). The mental health status among nurses from low-risk areas under normalized COVID-19 pandemic prevention and control in China: A cross-sectional study. International Journal of Mental Health Nursing, 30(4), 975–987. https://doi.org/10.1111/INM.12852
Coumoundouros, C., Mårtensson, E., Ferraris, G., Zuidberg, J. M., von Essen, L., Sanderman, R., & Woodford, J. (2022). Implementation of e-mental health interventions for informal caregivers of adults with chronic diseases: Mixed methods systematic review with a qualitative comparative analysis and thematic synthesis. JMIR Mental Health, 9(11). https://doi.org/10.2196/41891
Currie, K., Gupta, B. V., Shivanand, I., Desai, A., Bhatt, S., Tunuguntla, H. S., & Verma, S. (2022). Reductions in anxiety, depression and insomnia in health care workers using a non-pharmaceutical intervention. Frontiers in Psychiatry, 13. https://doi.org/10.3389/FPSYT.2022.983165
Drissi, N., Ouhbi, S., Marques, G., De La Torre Díez, I., Ghogho, M., & Janati Idrissi, M. A. (2021). A systematic literature review on e-mental health solutions to assist health care workers during COVID-19. Telemedicine Journal and E-Health : THe Official Journal of the American Telemedicine Association, 27(6), 594–602. https://doi.org/10.1089/TMJ.2020.0287
Fiol-DeRoque, M. A., Serrano-Ripoll, M. J., Jiménez, R., Zamanillo-Campos, R., Yáñez-Juan, A. M., Bennasar-Veny, M., Leiva, A., Gervilla, E., García-Buades, M. E., García-Toro, M., Alonso-Coello, P., Pastor-Moreno, G., Ruiz-Pérez, I., Sitges, C., García-Campayo, J., Llobera-Cánaves, J., & Ricci-Cabello, I. (2021). A mobile phone-based intervention to reduce mental health problems in health care workers during the COVID-19 pandemic (PsyCovidApp): Randomized controlled trial. JMIR MHealth and UHealth, 9(5). https://doi.org/10.2196/27039
Firth, J., Torous, J., Nicholas, J., Carney, R., Rosenbaum, S., & Sarris, J. (2017). Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. Journal of Affective Disorders, 218, 15–22. https://doi.org/10.1016/J.JAD.2017.04.046
Givens, J. L., & Tjia, J. (2002). Depressed medical students’ use of mental health services and barriers to use. 918–921.
Golden, E. A., Zweig, M., Danieletto, M., Landell, K., Nadkarni, G., Bottinger, E., Katz, L., Somarriba, R., Sharma, V., Katz, C. L., Marin, D. B., DePierro, J., & Charney, D. S. (2021). A resilience-building app to support the mental health of health care workers in the COVID-19 era: Design process, distribution, and evaluation. JMIR Formative Research, 5(5). https://doi.org/10.2196/26590
Goodday, S. M., Karlin, E., Alfarano, A., Brooks, A., Chapman, C., Desille, R., Karlin, D. R., Emami, H., Woods, N. F., Boch, A., Foschini, L., Wildman, M., Cormack, F., Taptiklis, N., Pratap, A., Ghassemi, M., Goldenberg, A., Nagaraj, S., Walsh, E., … Gerold, K. (2021). An alternative to the light touch digital health remote study: The stress and recovery in frontline COVID-19 health care workers study. JMIR Formative Research, 5(12). https://doi.org/10.2196/32165
Greenberg, N., Docherty, M., Gnanapragasam, S., & Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. In The BMJ (Vol. 368). BMJ Publishing Group. https://doi.org/10.1136/bmj.m1211
Iversen, A. C., Fear, N. T., Ehlers, A., Hacker Hughes, J., Hull, L., Earnshaw, M., Greenberg, N., Rona, R., Wessely, S., & Hotopf, M. (2008). Risk factors for post-traumatic stress disorder among UK Armed Forces personnel. Psychological Medicine, 38(4), 511–522. https://doi.org/10.1017/S0033291708002778
Kerst, A., Zielasek, J., & Gaebel, W. (2020). Smartphone applications for depression: A systematic literature review and a survey of health care professionals’ attitudes towards their use in clinical practice. European Archives of Psychiatry and Clinical Neuroscience, 270(2), 139–152. https://doi.org/10.1007/S00406-018-0974-3
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., Wu, J., Du, H., Chen, T., Li, R., Tan, H., Kang, L., Yao, L., Huang, M., Wang, H., Wang, G., Liu, Z., & Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976
Pierce, P., Whitten, M., & Hillman, S. (2023). The impact of digital healthcare on vulnerable pregnant women: A review of the use of the MyCare app in the maternity department at a central London tertiary unit. Frontiers in Digital Health, 5. https://doi.org/10.3389/FDGTH.2023.1155708
Piers, R., Williams, J. M., & Sharpe, H. (2023). Review: Can digital mental health interventions bridge the “digital divide” for socioeconomically and digitally marginalised youth? A systematic review. Child and Adolescent Mental Health, 28(1), 90–104. https://doi.org/10.1111/CAMH.12620
Ripp, J., Peccoralo, L., & Charney, D. (2020). Attending to the emotional well-being of the health care workforce in a New York City health system during the COVID-19 pandemic. Academic Medicine : Journal of the Association of American Medical Colleges. https://doi.org/10.1097/ACM.0000000000003414
Robins-Browne, K., Lewis, M., Burchill, L. J., Gilbert, C., Johnson, C., O’Donnell, M., Kotevski, A., Poonian, J., & Palmer, V. J. (2022). Interventions to support the mental health and well-being of front-line healthcare workers in hospitals during pandemics: An evidence review and synthesis. British Medical Journal Open, 12(11), e061317. https://doi.org/10.1136/BMJOPEN-2022-061317
Souza do Nascimento, V., Teotonio Rodrigues, A., Rotta, I., de Mendonça Lima, T., & Melo Aguiar, P. (2023). Evaluation of mobile applications focused on the care of patients with anxiety disorders: A systematic review in app stores in Brazil. International Journal of Medical Informatics, 175. https://doi.org/10.1016/J.IJMEDINF.2023.105087
Stentzel, U., Grabe, H. J., Schmidt, S., Tomczyk, S., van den Berg, N., & Beyer, A. (2023). Mental health-related telemedicine interventions for pregnant women and new mothers: A systematic literature review. BMC Psychiatry, 23(1), 292. https://doi.org/10.1186/S12888-023-04790-0
Stratton, E., Lampit, A., Choi, I., Calvo, R. A., Harvey, S. B., & Glozier, N. (2017). Effectiveness of eHealth interventions for reducing mental health conditions in employees: A systematic review and meta-analysis. PloS One, 12(12). https://doi.org/10.1371/JOURNAL.PONE.0189904
Taylor, H., Cavanagh, K., Field, A. P., & Strauss, C. (2022). Health care workers’ need for headspace: Findings from a multisite definitive randomized controlled trial of an unguided digital mindfulness-based self-help app to reduce healthcare worker stress. JMIR MHealth and UHealth, 10(8). https://doi.org/10.2196/31744
Thabrew, H., Stasiak, K., Hetrick, S. E., Wong, S., Huss, J. H., & Merry, S. N. (2018). E‐Health interventions for anxiety and depression in children and adolescents with long‐term physical conditions. The Cochrane Database of Systematic Reviews, 2018(8). https://doi.org/10.1002/14651858.CD012489.PUB2
Trottier, K., Monson, C. M., Kaysen, D., Wagner, A. C., Liebman, R. E., & Abbey, S. E. (2022). Initial findings on RESTORE for healthcare workers: An Internet-delivered intervention for COVID-19-related mental health symptoms. Translational Psychiatry, 12(1). https://doi.org/10.1038/S41398-022-01965-3
Ungar, P., Schindler, A. K., Polujanski, S., & Rotthoff, T. (2022). Online programs to strengthen the mental health of medical students: A systematic review of the literature. Medical Education Online, 27(1). https://doi.org/10.1080/10872981.2022.2082909
Wilson, J., Heinsch, M., Betts, D., Booth, D., & Kay-Lambkin, F. (2021). Barriers and facilitators to the use of e-health by older adults: a scoping review. BMC Public Health, 21(1). https://doi.org/10.1186/S12889-021-11623-W
Wood, A. E., Prins, A., Bush, N. E., Hsia, J. F., Bourn, L. E., Earley, M. D., Walser, R. D., & Ruzek, J. (2017). Reduction of burnout in mental health care providers using the provider resilience mobile application. Community Mental Health Journal, 53(4), 452–459. https://doi.org/10.1007/S10597-016-0076-5
Xie, H., Cheng, X., Song, X., Wu, W., Chen, J., Xi, Z., & Shou, K. (2020). Investigation of the psychological disorders in the healthcare nurses during a coronavirus disease 2019 outbreak in China. Medicine, 99(34), e21662. https://doi.org/10.1097/MD.0000000000021662
Xie, Q., Torous, J., & Goldberg, S. B. (2022). E-mental health for people with personality disorders: A systematic review. Current Psychiatry Reports, 24(10), 541–552. https://doi.org/10.1007/S11920-022-01360-1
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by all authors as explained in the manuscript. The first draft of the manuscript was written by Lucas Tokeshi, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tokeshi, L., de Castro Humes, E., de Andrade, A.L. et al. Healthcare Workers Mental Health and e-Health: A Scoping Review. J. technol. behav. sci. 9, 542–551 (2024). https://doi.org/10.1007/s41347-023-00381-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41347-023-00381-8