Abstract
To evaluate specific features of sleep pattern and neurocognitive performance in OSA obese adolescents to correlate sleep macrostructural parameters and phasic events (K-complexes, KCs; and sleep spindles, SSs) with cognitive functioning in these individuals. Polysomnography was recorded from 25 male apneic obese patients (15–17 years), 20 age- and sex-matched non-apneic obese and 15 lean adolescents. KCs and SSs were identified during stage 2 non-rapid eye movement sleep (N2) and characteristics were evaluated. Furthermore, all participants underwent cognitive performance assessment using a battery of neurocognitive tests. Participant’s data, macro- and microstructural sleep variables and cognitive measures were compared. Finding data were analyzed using descriptive and regression analyses. Differences were reliable at p < 0.05. Compared to both controls, the OSA obese group had significantly reduced sleep onset latency (p = 0.061), slow-wave sleep (SWS) and rapid eye movement (REM) sleep (p < 0.01 for both), but increased N1–N2 stage duration (p < 0.01), the appearance of KCs during apnea and after apnea episodes (DE-KCs and AE-KCs, respectively), reduced spontaneous KCs (SN-KCs) number and periodicity, and lowered amplitude of apnea evoked KCs. SSs activity was an atypical increased in the OSA group. SWS, REM sleep, minimal SaO2, DE-KCs, AE-KCs, and SSs, as well as SN-KCs number, were predictors of cognitive functioning (attention, memory, thinking, speech) changes in OSA adolescents. Together, the above results provide some evidence for impairment in sleep homeostatic mechanisms, when OSA and obesity are comorbid, and provide novel insights into the relationship between sleep microstructure disruption and waking cognitive functioning in these adolescents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization (WHO) announced obesity is non-communicative pandemic, which affects more than 650 million adults and 340 million children and adolescents worldwide [1]. Obesity is associated with much serious comorbidity [2, 3], one of which is obstructive sleep apnea (OSA), affecting at least 2% of adolescents [4]. Resent a 10-year follow-up study showed that incidence of adolescent/adult OSA at follow-up was 22%. Wherein, male sex and obesity were associated with incident OSA [5]. OSA may be compounded by adverse cognitive impairments [6]. A relationship between OSA and cognitive deficits was first identified in the 1980s [7]. Later, it was reported that about 60% of adult OSA obese patients had at least one cognitive impairment [8]. However, the potential neurocognitive effects of OSA yet are significantly less developed for the adolescence. Some authors concluded that OSA obese patients may have an impaired executive functions and an increased risk for poorer educational outcomes [9]. These findings are very important, as this period of life is crucial for the development of frontal brain lobe functioning, but little systematic research has been done to characterize the nature of defective cognition and it underlying mechanisms.
OSA is characterized by the periodic collapse of the upper airway during sleep, leading to reduction or cessation of airflow, intermittent nocturnal hypoxia, cortical hyperarousal, and, as a result, sleep fragmentation and alteration of sleep homeostasis [10]. Studies assessing polysomnography (PSG) in apneic obese samples have mixed results. If sleep architecture were well described in adults, children and adolescents [11, 12], changes of sleep microstructure parameters (sleep spindles, SSs, and K-complexes, KCs) in these patients were documented among adult or children samples [13, 14]. However, in our previous study, preliminary evaluating SSs activity in overweight adolescents, we obtained controversial results [15]. Some authors showed correlations between sleep electroencephalography (EEG) parameters and neurocognitive performance in obese OSA patients and concluded that low non-rapid eye movement stage 2 (N2) sigma spectral powers and SS index, and similar findings could serve as a biomarker of risk for cognitive dysfunction in patients with OSA [13, 16, 17]. However, no studies have assessed such associations in OSA obese adolescents. So, the purpose of our research was to evaluate specific features of sleep pattern and neurocognitive performance in OSA obese adolescents to correlate sleep macrostructural parameters and phasic events (KCs and SSs) with waking cognitive functioning in these individuals. We hypothesized that OSA obese adolescents, having altered sleep homeostasis, would exhibit more cognitive abnormalities on neurocognitive measures with more numbers of significant interactions than would obese and lean controls.
Subjects and methods
Subject selection
Study participants were recruited from patients referred to the Children’s Hospital in the period from January to December 2019. All adolescents were male, between 15 and 17 years of age, with no craniofacial anomalies and neuromuscular diseases, no treatment by adenotonsillectomy or continuous positive airway pressure (CPAP) therapy. Obese participants should have body mass index Z-score (zBMI) > 2 for age and sex, and normal weight (NW) individuals should have zBMI ≥ −2 to + 1 for age and sex [18]. So, the study sample included 60 participants: of these, 45 had obesity (mean age 16.2 ± 0.4 years), and 15 NW adolescents were lean controls (mean age 16.0 ± 0.5 years). Assignment of obese participants to subgroups was based on PSG results: 25 patients were included in the OSA obese group and 20 non-OSA patients were age-matched obese controls.
The study was conducted in accordance with the Declaration of Helsinki (World Medical Association, 2013), and the study protocol was approved by the Local Committee on Biomedical Ethics. Written informed consent was obtained from all recruited adolescents.
Measurements and procedures
Standing height and body weight were measured once when adolescents were included in the study. BMI was calculated as weight in kilograms over height in meters squared (kg/m2). BMI was further analyzed as zBMI using the AnthroPlus calculator based on the WHO (2007) [18].
Sleep was recorded overnight using the GRASS-TELEFACTOR Twin PSG (Comet) with As the amplifier 40 with an integrated module for sleep SPM-1 (USA). Standard PSG included EEG from F3, F4, Fz, Cz, C3, C4, O1, and O2 scalp, electrooculography (EOG) from the outer upper corner of each orbit, electrocardiography (ECG) from left and right the 2-nd intercostal spaces, electromyography (EMG) from the chin, airflow measurement from the nose and the mouth, snore assessment from the body site at the sternocleidomastoid muscle front edge, respiratory movements and blood oxygen saturation (SpO2) monitoring with chest and abdomen bands, and finger sensor, accordingly, EMG from left and right tibialis anterior muscles. EEG electrode disposition were referenced to M1 and M2 as F3-M2, F4-M1, C3-M2, C4-M1, O1-M2, and O2-M1. Cz was the reference and Fz was the ground. Night was stage scored according to the American Academy of Sleep Medicine (AASM) scoring rules [19]. Sleep macrostructure parameters were determined, including total sleep time (TST), sleep onset latency (SOL), wake after sleep onset (WASO), sleep efficiency (SE), non-rapid eye movement sleep stages 1 and 2 (N1-N2), slow-wave sleep (SWS) and rapid eye movement sleep (REM) stages. Cortical arousals were expressed as a total number of events per hour of sleep (arousal index, AI). Obstructive apneas were defined as at least a 90%, and hypopneas at least 30% reduction of the airflow signal amplitude. Obstructive apneas and hypopneas were expressed as the number of events per hour of sleep (apnea/hypopnea index, AHI). OSA was identified if apnea/hypopnea index (AHI) ≥ 2 number/hour [20].
KCs were visually identified at F4-M1 in N2 stage as 75 μV waves at least 0.5 s in duration. Number (total number of KCs in N2 stage); mean density (number of KCs per minute of N2 stage); mean duration (average duration of KCs in msec.); amplitude peak-to-peak (μV) and mean inter-KCs time interval were calculated. In OSA adolescents, all recorded KCs were divided into three categories [21]: (1) KCs occurring during the apneic episode (DE-KCs); (2) KCs occurring after apneic episode (AE-KCs); and (3) KCs occurring without an apneic episode and drop in SpO2 (spontaneous KCs, SN-KCs). In both obese and lean controls SN-KCs only were detected and analyzed.
To identify SSs, C4 channel was spatially filtered to display frequencies between 11 and 16 Hz [13]. SSs were detected in all epochs of N2 stage on recording night as a narrow conical shape waves at least 0.5 s in length. Number (total number of SSs in N2 stage); density (number of SSs per minute of N2 stage); maximum amplitude (μV); mean duration (average duration of SSs in second) and mean frequency (mean SSs frequency in Hz) were calculated. Power spectrum was automatically scored for consecutive 20 s. epochs with Spectral Analysis option of GRASS-TELEFACTOR Twin PSG (hanning window, averages of five 4 s. epochs; frequency resolution 0.25 Hz).
All participants completed neurocognitive tests including tasks from the Schulte tables [22], pictogram test [23], ten-word retrieval test, associated thinking test [24] and object classification test [25] to assess a voluntary attention (Vol_A), a verbal memory (Verb_M), a visual memory (Vis_M), an associative thinking (Ass_T) and a semantic speech (Sem_S), accordingly. The tests were performed in a separate visit from PSG during the morning between 8 and 9 am in a quiet and tranquil environment with a trained psychologist.
Statistical tests were performed using Statistica v10.0 (StatSoft, USA). Descriptive statistics were used to analyze participant’s demographic, polysomnographic characteristics and neurocognitive data. Numbers, N; percentages, %; mean, M, and standard deviation, SD were presented. The comparison between participant’s data, sleep parameters (macrostructure, SSs and KCs), as well as neurocognitive measures was performed by means of the Mann–Whitney U test for independent data sets. Lineal regression correlation analysis was performed to identify the relationship between neurocognitive test’s scores, estimating Verb_M, Vis_M, Vol_A, Ass_T and Sem_S, and various sleep macrostructure and microstructure characteristics in OSA and non-OSA obese patients. Among the variables showing statistically significant correlations, multiple stepwise linear regression analysis was performed to further clarify the relationship between above mention neurocognitive variables and sleep parameters in OSA adolescents only. Differences were considered statistically significant at p-value (adjusted p-value − adj.p) < 0.05.
Results
Sample characteristics and sleep data
The results of comparisons between groups on age, BMI and PSG (macrostructural) variables are shown in Table 1. No group differences were apparent on mean age. Wherein, as expected, zBMI differed significantly for in lean adolescents compared to both obese groups (adj.p = 0.0003) but did not differ between the OSA group and obese controls (p = 0.75). All PSG parameters in the non-OSA obese and lean individuals were not significantly different. However, the analysis indicated that compared to both controls, the OSA group had higher AHI (adj.p = 0.0006), lower minimal SaO2 (adj.p = 0.0003), higher AI (adj.p = 0.0003), shorter SOL (adj.p = 0.061), more time in N1-N2 stages (adj.p < 0.01), but less time in both SWS (adj.p < 0.01) and REM sleep (adj.p < 0.01).
Microstructural sleep variables
Participant’s KCs characteristics are presented in Table 2. It should be noted that, among OSA participants, there were on average 468 DE-KCs, 499 AE-KCs and 220 SN-KCs. While in the both controls were detected SN-KCs only. Intergroup analysis was shown that OSA obese adolescents had a significantly higher number of KCs (adj.p < 0.001) and KCs density (adj.p = 0.0003), as well as lower amplitude, smaller KCs duration and time interval between KCs than both controls (adj.p < 0.01, adj.p < 0.006 and adj.p < 0.001, respectively). Furthermore, we compared across DE-KCs, AE-KCs, and SN-KCs in OSA obese adolescents. As shown in Table 3, the highest values of the mean density, but the smallest values of mean duration, amplitude, and inter-KCs time interval were found in DE-KCs. AE-KCs showed the middle values of above-mentioned variables. In comparing DE-KCs and SN-KCs, as well as AE-KCs and SN-KCs, all characteristics showed highly significant differences.
Table 4 shows the SSs analysis for all study groups. OSA patients had a significant higher SSs number (adj.p < 0.001) and density (adj.p < 0.01), but smaller amplitude (adj.p < 0.01) and frequency (p = 0.034) than both controls. There was no significant change in SSs duration between the three groups (p = 0.462). No group differences were apparent on SSs characteristics for non-OSA obese adolescents and their lean peers.
Figure 1 shows examples of KCs and SSs detection in an OSA obese patient, in an obese control patient and in a lean control adolescent.
Examples of visual KCs and SS detection in an obese patient with OSA (top tracing), in an obese control patient (middle tracing), and a lean control adolescent (bottom tracing), 20-s epoch. In OSA patient, KCs accompanying different events contributed to the definition of DE-KC, AE-KC, and SN-KC. The ovals marked on F4-M1 of top tracing illustrate KCs produced in different situations. The boxes marked on C4-M1 illustrate SSs produced. The box labeled on AIRFLOW channel indicates respiratory event (obstructive apnea episode). OSA: obstructive sleep apnea; KCs: K-complexes; DE-KCs: K-complexes during apneic episodes; AE-KC: K-complexes after apneic episodes; SN-KCs: spontaneous K-complexes; SSs: sleep spindles; N2 : non-rapid yes movement stage 2
Neurocognitive measures
Figure 2 presents the comparative results of neurocognitive tests for the study sample. The OSA obese group had significantly poorer attention, associative thinking and semantic speech activity compared to obese (p < 0.0005, p < 0.001 and p = 0.008, respectively) and lean controls (p < 0.0001, p < 0.0005 and p = 0.002, respectively). Similarly, OSA obese adolescents had significantly worse visual and verbal memories compared to non-OSA obese (p = 0.004 and p < 0.001) and lean peers (p < 0.001 and p < 0.0005). No differences were found between obese and lean controls.
Lineal regression correlations between sleep parameters and neurocognitive variables
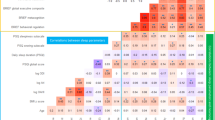
Lineal regression correlation analysis was performed to assess correlations of Verb_M, Vis_M, Vol_A, Ass_T and Sem_S assessment scores with sleep macrostructure (TST, SE, SOL, N1-N2, SWS, and REM sleep) and microstructure (KCs and SSs variables) in obese adolescents with and without OSA. The results are shown in Table 5.
As shown from the table, among the neurocognitive parameters, Verb_M and Vis_M were significantly positively correlated with SWS (r = 0.254, p = 0.003 and r = 0.247, p = 0.004, respectively) and REM (r = 0.265, p = 0.001 and r = 0.198, p = 0.034, respectively), but negatively correlated with N1-N2 (r = − 0.216, p = 0.012 and r = − 0.213, p = 0.002, respectively) in apneic obese patients. Verb_M was significantly positively correlated with REM only (r = 0.177, p = 0.046) in non-apneic obese patients. Vol_A also showed statistically significant correlation with such macrostructural sleep parameters as SWS and REM (r = 0.198, p = 0.023 and r = 0.371, p < 0.001, respectively) in OSA obese adolescents only. Sem_S demonstrating significant positive correlation with SWS (r = 0.175, p = 0.049) and REM (r = 0.177, p = 0.047) in apneic patient only.
Verb_M was significantly correlated with the number of all KCs, duration and an average time interval (r = − 0.461, p < 0.001; r = 0.361, p = 0.006; and r = 0.302, p = 0.002, respectively) in OSA obese patients. It should be noted that, slightly significant positive correlations were found between KCs number and an average time interval (r = 0.198, p = 0.021; and r = 0.215, p = 0.011, respectively) and Verb_M in the non-OSA obese group. Vol_A was significantly negatively correlated with the number of KCs and mean density, and positively correlated with an average time interval of KCs (r = − 0.399, p < 0.001; r = − 0.276, p = 0.003; and r = 0.281, p = 0.002; respectively) in OSA participants only. There was no association between Vol_A and amplitude peak-to peak and duration of KCs. However, no significant correlations were found between KCs variables and semantic speech activity parameters, neither in OSA adolescents, nor in obese controls (all p > 0.05 throughout).
Spindle activity measures, such as the number and the maximum amplitude in N2 sleep stage were significantly correlated with Verb_M and Vol_A in OSA adolescents (r = −0.293, p = 0.001 and r = 0.312, p = 0.004: r = -0.482, p < 0.001 and r = 0.466, p = 0.005; respectively), as well as Vol_A was negatively correlated with SSs density (r = −0.291, p = 0.002) and Ass_T was negatively correlated with number of SSs (r = − 0.271, p = 0.004). In obese controls there were also significant correlations, however in a lower magnitude and only with the number of SSs and the maximum amplitude in N2 sleep stage (r = −0.231, p = 0.012 and r = 0.171, p = 0.032, respectively). No significant correlations were found between SSs duration and frequency and these cognitive measures, neither in OSA subjects nor in obese controls (all p > 0.05 throughout).
Further, correlations between AHI, nadir SaO2, DE-KCs, AE-KCs, and SN-KCs and indexes of aforementioned cognitive domains was also carried out in the OSA group only (Table 6).
Verb_M was significantly correlated with AHI and nadir of SaO2 as well as DE-KCs density, DE-KCs duration and inter-DE-KCs time interval (r = − 0.201, p = 0.031; r = −0.338, p < 0.001; r = 0.312, p = 0.002), AE-KCs density (r = − 0.389, p < 0.001), SN-KCs density and inter-SN-KCs time interval (r = 0.281, p = 0.002; and r = 0.278, p = 0.003, respectively). It should be noted that, slightly significant correlations were found between AHI, DE-KCs density and inter-DE-KCs time interval (r = − 0.191, p = 0.041; r = −0.176, p = 0.047; r = 0.185, p = 0.031). However there was strong enough correlation between Vis_M and nadir of SaO2 (r = 0.269, p = 0.008) in apneic patients, as well as Sem_S and this OSA-related parameter (r = 0.227, p = 0.002).
All of DE-KCs variables demonstrating significant correlations with Vol_A (r = − 0.321, p < 0.001 for density; r = 0.267, p = 0.007 for duration; r = 0.260, p = 0.006 for amplitude peak-to peak; and r = 0.285, p = 0.002 for inter-KCs time interval), as well as the AE-KCs density and an average time interval (r = − 0.302, p = 0.002; and r = 0.279, p = 0.003, respectively). No significant correlation was found between SN-KCs characteristics and Vol_A.
There is significant negatively correlation between Ass_T and DE-KCs density, as well as its positively correlation with SN-KCs density (r = − 0.251, p = 0.006 and r = 0.273, p = 0.003, respectively) in OSA obese adolescents. No significant correlation was found between above-mentioned KCs variables and Sem_s.
These results suggest critical associations between SWS, REM sleep, AHI, SaO2 and sleep microstructural variables and neurocognitive parameters in OSA obese patients.
Multiple regression analysis results with sleep parameters as predictors of neurocognitive characteristic’s changes
Macro- and microstructural sleep parameters showing significant correlations with the neurocognitive measures in OSA obese adolescents were entered as possible predictors in regression models. Results from multiple regression analysis indicated that SWS, REM sleep, nadir of SaO2, DE-KCs density, AE-KCs density and the number of SSs best predicted Verb_M scores, whereas Vis_M was predicted by SWS, REM sleep, nadir of SaO2, DE-KCs density and the number of SSs. With respect to other neurocognitive parameters, Vol_A was predicted by SWS, the number of KCs, DE-KCs density and the number of SSs. Ass_T was best predicted by the number of SSs, and Sem_S by nadir of SaO2 (see Table 7).
Discussion
The present study is one of the few to suggest a relationship between neurocognitive functions and macro-and microstructural sleep variables in obese adolescents with and without OSA by using polysomnography. Several sleep parameters were significantly correlated with cognitive measures utilized in this study, and regression models demonstrated that SWS, REM sleep, nadir of SaO2, DE-KCs density, AE-KCs density, and the number of SSs are predictive of cognitive characteristic’s changes in OSA obese patients.
It is known that OSA is characterized by multiple interruptions of airflow between periods of EEG arousals that leading to sleep disruption in apneic patients. The current study did find evidence of greater arousal generation reported in previous studies [17, 26]. Reduced SWS, found in the OSA group, reflects disruption to a specific brain mechanism, that is the homeostatic control of non-REM sleep, following weight gain, the immune regulatory dysfunction, growth retardation and others health problems [27]. This is understandable since the brain regions, including thalamocortical area, underlying the generation of slow waves in non-REM sleep [28] are vulnerable to the diffuse hypoxic brain damage typical of OSA. It is well documented that sleep is essential for learning and memory performance [29] and decreasing REM sleep, obtained in our study, as well as SWS, non-surprisingly, may contribute to cognitive impairment in OSA patients. Indeed, in the current study, SWS and REM sleep significantly predicted memories, attention and speech scores in OSA obese adolescents. Disruption of these sleep phases and their significant reduction in adult OSA patient’s cohort have been suggested in previous research, but this problem among adolescents remains insufficiently studied and widely discussed [30]. SWS is important for declarative memory consolidation, a process in which the prefrontal brain cortex plays an important role, as well as REM sleep mainly reflect deficient of attention. Indeed, the percentage of SWS and REM sleep predicted the Verb_M, Vis_M and Vol_A scores in the OSA obese patient group in our study, that confirm the hypothesis of a close connection between sleep and memory consolidation/attention in this group of adolescents.
It is known, that hypoxia, accompanying OSA, may affect the structure and function of the brain, leading to the long-term alter synaptic plasticity, and contribute to cognitive impairment [31]. Hypoxia-induced oxidative injury in the brain may lead to associated cognitive dysfunction, which confirmed in our OSA patients.
KCs and SSs are the most obvious and recognizable features of human sleep EEG. In addition to characterizing brainwaves unique to non-REM sleep which have phasic patterns, these are intimately related to sleep depth and homeostasis [32, 33]. It should be noted that, changes in these sleep EEG patterns were expected, but we got some results in contrast to previous studies. Participants with OSA had greater DE-KCs and AE-KCs than both controls, excluding SN-KCs, that similar with the results of Parekh’s et al. study [16]. Shorted time interval between the generation of DE-KCs and AE-KCs are reflecting the change in the periodicity of these EEG events [21]. It is known that KCs are playing a protective or inhibitory role [34]. In our study, the sleep inhibitory mechanism was disrupted in N2 stage in OSA obese adolescents, but not in both controls.
SSs have been implicated in multiple brain functions, including sleep quality, and sleep-dependent memory consolidation [32, 35]. In OSA individuals, SSs number decreased in non-REM sleep were typically observed [35], however, this value was increased in our OSA adolescents, as well as SSs density. OSA adolescents were expected to have significantly more frequent SSs, as well as shown in our previous study in overweight apneic patients [15]. However, this is contrasting with other studies of SSs features in OSA children [13]. These patterns can be explained increased arousal ability in response to an excessive respiratory stimuli in OSA patients, causes frequent for the appearance of SSs as a protective brain mechanism from arousing stimuli and thereby enhance sleep consolidation.
Given the specific features of sleep microstructure in OSA obese adolescents, we explored the relationship between altered sleep homeostasis and waking neurocognitive functioning. Correlation analyses indicated that higher KCs and SSs generation was correlated with worse cognitive functioning in the OSA group, that in contrast with the earlier pediatric study [13, 33]. However less number of SN-KCs in the OSA group positive correlated with memory performance. KCs number, density and inter-KCs time interval correlated with performances on a broad range of neurocognitive tests. Specifically, correlations of these variables in both DE-KCs and AE-KCs were negative, while in SN-KCs those were positive. Increased spindle activity was significantly correlated with all of the evaluated neurocognitive domains. Several cognitive measures, like Verb_M, Vis_M and Vol_A, in obese controls also have significant correlations, but a lower magnitude and with one of the SSs variables. These results suggest that altered sleep EEG pattern generation may represent an initial adaptation to periodic hypoxic events in OSA adolescents, already leading to neurocognitive impairment.
To conclude, previous research on sleep patterns and associations between sleep EEG phasic events, as indicators of sleep homeostasis, and neurocognitive performance in OSA patients has been limited to children or adults. The current study was conducted to investigate these relationships in adolescence characterized main physical, emotional, behavioral and social changes. Specifically, the OSA group had a significant higher DE-KCs and AE-KCs generation evoked periodic respiratory events, as well as SSs activity, providing some evidence of disruption to sleep homeostasis. In addition, fewer SN-KCs, with reduced periodicity and increased amplitude revealed disrupted sleep inhibitory and information processing mechanisms that are necessary for sleep consolidation. SSs also showed an atypical pattern for OSA patients that assumed availability of impairments in sleep regulatory and inhibitory mechanisms at the stage of initial adaptation to apneic events in adolescence. We showed that apneic patients with fewer SN-KCs generation, as well as greater spindle activity, had significantly pure cognitive performance, than non-apneic obese and lean controls. These data can improve understanding of sleep pattern changes if OSA is present and provide direction for future researches to manage sleep inhibitory and regulatory mechanisms in these individuals. Studying of the impact altered sleep homeostasis on waking cognitive functioning may help to direct novel strategies to neurocognitive improvements and prevention of early dementia disorders in young adults.
This work was performed with the use of the equipment of Collective research centre “Center for the development of progressive personalized technologies for health” SC FHHRP, Irkutsk.
References
Obesity and overweight. Report of a WHO. 2020. https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 15 Jun 2020
Kolesnikova L, Dzyatkovskaya E, Rychkova L, Polyakov V. New approaches to identifying children of psychosomatic disorders risk group. Proc Soc Behav Sci. 2015;214:882–9.
Kohut T, Robbins J, Panganiban J. Update on childhood/adolescent obesity and its sequela. Curr Opin Pediatr. 2019;31(5):645–53.
Sanchez-Armengol A, Fuentes-Pradera MA, Capote-Gil F, García-Díaz E, Cano-Gómez S, Carmona-Bernal C, Castillo-Gómez J. Sleep related breathing disorders in adolescents aged 12 to 16 years: clinical and polygraphic findings. Chest. 2001;119:1393–400.
Chan KC, Au CT, Hui LL, Ng S-K, Wing YK, Li AM. How OSA evolves from childhood to young adulthood: natural history from a 10-year follow-up study. Chest. 2019;156(1):120–30.
Madaeva I, Berdina O, Polyakov V, Kolesnikov S. Obstructive sleep apnea and hypertension in adolescents: effect on neurobehavioral and cognitive functioning. Can Respir J. 2016;4:1–6.
Findley LJ, Barth JT, Powers DC, Wilhoit SC, Boyd DG, Suratt PM. Cognitive impairment in patients with obstructive sleep apnea and associated hypoxemia. Chest. 1986;90:686–90.
Pierobon A, Giardini A, Fanfulla F, Callegari S, Majani G. A multidimensional assessment of obese patients with obstructive sleep apnoea syndrome (OSAS): a study of psychological, neuropsychological and clinical relationships in a disabling multifaceted disease. Sleep Med. 2008;9:882–9.
Watach AJ, Radcliffe J, Xanthopoulos MS, Novick MB, Sawyer AM. Executive function impairments in adolescents with obesity and obstructive sleep apnea syndrome. Biol Res Nurs. 2019;21(4):377–83.
Dehlink E, Tan HL. Update on paediatric obstructive sleep apnoea. J Thorac. 2016;8(2):224–35.
Antczak J, Horn B, Richter A, Jernajczyk W, Bodenschatz R, Schmidtal EWW. The influence of obesity on sleep quality in male sleep apnea patients before and during therapy. J Physiol Pharmacol. 2008;59(Suppl 6):123–34.
Hayes JF, Balantekin KN, Altman M, Wilfley DE, Taylor CB, Williams J. Sleep patterns and quality are associated with severity of obesity and weight-related behaviors in adolescents with overweight and obesity. Child Obes. 2018;14(1):11–7.
Brockmann P, Damiani F, Pincheira E, Daiber F, Ruiz S, Aboitiz F, Ferri R, Bruni O. Sleep spindle activity in children with obstructive sleep apnea as a marker of neurocognitive performance: a pilot study. Eur J Paediatr Neurol. 2018;22(3):434–9.
Li W, Duan Y, Yan J, Gao H, Li X. Association between loss of sleep-specific waves and age, sleep efficiency, body mass index, and apnea-hypopnea index in human N3 sleep. Aging Dis. 2020;11(1):73–81.
Madaeva I, Berdina O, Rychkova L, Bugun O. Sleep spindle characteristics in overweight adolescents with obstructive sleep apnea syndrome. Sleep Biol Rhythm. 2017;15(3):251–7.
Parekh A, Mullins AE, Kam K, Varga AW, Rapoport DM, Ayappa I. Slow-wave activity surrounding stage N2 k-complexes and daytime function measured by psychomotor vigilance test in obstructive sleep apnea. Sleep. 2019;42(3):1–13.
Li N, Wang J, Wang D, Wang Q, Han F, Jyothi K, Chen R. Correlation of sleep microstructure with daytime sleepiness and cognitive function in young and middle-aged adults with obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2019;276(12):3525–32.
Obesity and overweight. Fact sheet. Growth reference 5–19 years. 2020. https://www.who.int/growthref/who2007_bmi_for_age/en/. Accessed 5 Jul 2020
Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, Vaughn BV. The AASM Manual for the scoring of sleep and associated events: rules, terminology and technical specifications, version 2.2. Darien: American Academy of Sleep Medicine; 2015
Kaditis AG, Alvarez MLA, Boudewyns A, Alexopoulos EI, Ersu R, Joosten K, Larramona H, Miano S, Narang I, Trang H, Tsaoussoglou M, Vandenbussche N, Villa MP, Waardenburg DV, Weber S, Verhulst S. Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J. 2016;47(1):69–94.
Sun L, Zang X, Huang S, Liang J, Luo Y. K-complex morphological features in male obstructive sleep apnea-hypopnea syndrome patients. Respir Physiol Neurobiol. 2018;248:10–6.
Kumpaitiene B, Svagzdiene M, Drigotiene I, Sirvinskas E, Sepetiene R, Zakelis R, Benetis R. Correlation among decreased regional cerebral oxygen saturation, blood levels of brain injury biomarkers, and cognitive disorder. J Int Med Res. 2018;46(9):3621–9.
Leontieva L, Rostova J, Tunick R, Golovko S, Harkulich J, Ploutz-Snyder R. Cross-cultural diagnostic applicability of the Pictogram Test. J Pers Assess. 2008;90(2):165–74.
Bertola L, Mota N, Copelli M, Rivero T, Diniz BS, Romano-Silva MA, Ribeiro S, Malloy-Diniz LF. Graph analysis of verbal fluency test discriminate between patients with Alzheimer’s disease, mild cognitive impairment and normal elderly controls. Front Aging Neurosci. 2014;6(185):1–10.
Nosarti C, Giouroukou E, Micali N, Rifkin L, Morris LG, Murray RM. Impaired executive functioning in young adults born very preterm. J Int Neuropsychol Soc. 2007;13(4):571–81.
Gurbani N, Verhulst SL, Tan C, Simakajornboon N. Sleep complaints and sleep architecture in children with idiopathic central sleep apnea. J Clin Sleep Med. 2017;13(6):777–83. https://doi.org/10.5664/jcsm.6614.
Assefa SZ, Diaz-Abad M, Wickwire EM, Scharf SM. The functions of sleep. AIMS Neurosci. 2015;2(3):155–71.
McGinty D, Szymusiak R. Neural control of sleep in mammals. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine, 5th ed. London: W.C. Elsevier; 2011. pp. 54–66
Abel T, Havekes R, Saletin JM, Walker MP. Sleep, plasticity and memory from molecules to wholebrain networks. Curr Biol. 2013;23(17):R774–88.
Krysta K, Bratek A, Zawada K, Stepańczak R. Cognitive deficits in adults with obstructive sleep apnea compared to children and adolescents. J Neural Transm (Vienna). 2017;124(Suppl 1):187–201. https://doi.org/10.1007/s00702-015-1501-6.
Gildeh N, Drakatos P, Higgins S, Rosenzweig I, Kent BD. Emerging co-morbidities of obstructive sleep apnea: cognition, kidney disease, and cancer. J Thorac Dis. 2016;8(9):E901–17. https://doi.org/10.21037/jtd.2016.09.23.
Carvalho DZ, Gerhardt GJ, Dellagustin G, de Santa-Helena EL, Lemke N, Segal AZ, Schönwald SV. Loss of sleep spindle frequency deceleration in obstructive sleep apnea. Clin Neurophysiol. 2014;125(2):306–12.
De Gennaro L, Gorgoni M, Reda F, Lauri G, Truglia I, Cordone S, Scarpelli S, Mangiaruga A, D’atri A, Lacidogna G, Ferrar M, Marra C, Rossini PM. The fall of sleep K-complex in Alzheimer disease. Sci Rep. 2017;3(7):39688.
Rodríguez-Labrada R, Galicia-Polo L, Canales-Ochoa N, Voss U, Tuin I, Peña-Acosta A, Estupiñán-Rodriguez A, Medrano-Montero J, Vázquez-Mojena Y, González-Zaldivar Y, Auburger G, Velázquez-Pérez L. Sleep spindles and K-complex activities are decreased in spinocerebellar ataxia type 2: relationship to memory and motor performances. Sleep Med. 2019;60:188–96.
Yetkin O, Aydogan D. Effect of CPAP on sleep spindles in patients with OSA. Respir Physiol Neurobiol. 2018;247:71–3.
Funding
No financial support.
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The requirements for authorship have been met. All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by OB, IM, SB, VP, OB and LR. The first draft of the manuscript was written by OB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Olga Berdina, Irina Madaeva, Svetlana Bolshakova, Vladimir Polyakov, Olga Bugun and Liubov Rychkova declare that they have no conflict of interest. Statements by each author are attached.
Research involving Human Participants and/or Animals
All procedures performed in this study involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments. This study has been approved by the Scientific Centre for Family Health and Human Reproduction Problems Committee on Biomedical Ethics.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Berdina, O., Madaeva, I., Bolshakova, S. et al. Alteration of sleep homeostasis and cognitive impairment in apneic obese adolescents. Sleep Biol. Rhythms 19, 285–295 (2021). https://doi.org/10.1007/s41105-021-00317-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-021-00317-w