Abstract
Sleep problems are commonly associated with chronic pain. It is not known whether pain is more related to a particular type of sleep problem or to more composite measures of sleep disturbance. The aim of the study was to investigate cross-sectionally the association between three commonly used sleep problem scales and musculoskeletal pain, when controlling for age, lifestyle and work factors. A total of 1032 nurses answered the Epworth Sleepiness Scale, Bergen Insomnia Scale, Pittsburg Sleep Quality Index and questionnaires regarding work, personality and lifestyle factors. Data collection started in October 2014 and ended in November 2015. Data were analyzed with hierarchical multiple regressions. Musculoskeletal pain was associated with Epworth Sleepiness Scale and Bergen Insomnia Scale, with Bergen Insomnia Scale showing the strongest association. Post hoc analyses of the most frequently reported pain locations, back pain headache and neck pain, confirmed that Bergen Insomnia Scale showed the strongest association. Insomnia seems to be more strongly associated with musculoskeletal pain than subjective sleepiness, thus the measures used to explore this association should be carefully selected when studying the relation between disturbed sleep and pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
Shift workers often report sleep problems, such as insomnia, poor sleep quality and sleepiness [1, 2]. Among Norwegian nurses, around 70% are shift workers. Nurses also constitute a large, important risk group for musculoskeletal pain [3]. Musculoskeletal problems are associated with high health care cost and daily life restrictions [4] and sickness absence [5]. It is well documented that several sleep problems are associated with increased pain sensitivity and increased risk of developing pain [6, 7]. A comprehensive literature review by Menefee and colleagues [8], suggested that daytime sleepiness and insomnia are sleep measures commonly associated with chronic pain.
Disturbed sleep may result in daytime sleepiness. Daytime sleepiness refers to a person’s sleep propensity in their everyday life [9]. Changani and colleagues [10] found that sleepy individuals presented with a lower pain threshold than non-sleepy individuals. Sleepiness has also been associated with musculoskeletal pain in longitudinal [11] and cross sectional studies [12] and with abdominal pain with no identified medical cause [13].
Insomnia refers to difficulties falling or staying asleep. Insomnia may be classified by several criteria, of which the Diagnostic and Statistical Manual for Mental Disorders criteria is the most used for research and implemented in various questionnaires (DSM-5) [14]. Increased risk for musculoskeletal pain or headache has been associated with insomnia in longitudinal [15, 16] and cross-sectional studies [17]. In a large population study of 10,412 persons, having insomnia was associated with lower pain tolerance [18]. Furthermore, Dzierzewski and colleagues [19] found that older adults suffering from insomnia tended to report more pain after a night of reduced total sleep time, which is a feature of insomnia.
A widely used sleep measure is the Pittsburg Sleep Quality Index (PSQI), which is a global sleep disturbance measure, including aspects such as subjective sleep quality, duration, and efficiency [20]. Higher scores in PSQI were associated with higher pain intensity during back-pain patient rehabilitation [21].
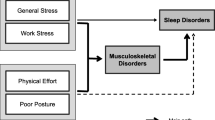
Despite extensive research on the association between sleep disturbances and pain, it is unclear whether pain is more related to a particular type of sleep problem (e.g. sleepiness or insomnia) or to more composite/unspecific measures of sleep disturbance. A range of personal and work-related risk factors for musculoskeletal pain were considered. Personal factors included age [22], lifestyle (e.g. smoking [23]; physical fitness [24]) and morningness/eveningness (i.e. being more awake and active in the morning/during evening) [25]. Work-related factors included psychological and social exposures (e.g. job demands, role conflict, empowering leadership) [26,27,28], extended work hours [29] and influence over schedule [30]. Physical workplace factors included working in a standing position, lifting heavy or unexpected loads [31].
The aim of this cross-sectional study was to determine which of the three sleep problem scales (measuring daytime sleepiness, insomnia, global sleep disturbance) was most strongly associated with musculoskeletal pain among nurses, when assessed simultaneously, after controlling for age, lifestyle and work factors. The primary outcome measure was a global musculoskeletal index including all body regions. As secondary outcome measures, three regions commonly reported in literature (headache, neck pain and back pain) were analysed as separate outcome variables. A better understanding of which sleep problem is associated with pain could potentially influence nursing working policies and shift plans, to lower sickness absence and life restrictions influencing their job performance.
Participants
A random sample of shiftworking nurses working in public hospitals in Norway was recruited for the current study. In total, 1032 nurses participated in the study (male = 10.3%, female = 89.7%). Mean age was 41.61 years (SD = 11.20, range 22–65 years). The inclusion criteria were working as a nurse, working in more than 50% position, having a rotating shift schedule including morning, evening and night shifts, being 18 years old or older, not being pregnant, not breast feeding, and not on sick leave for more than 2 weeks during the last 6 months. Correcting for the inclusion criteria, the number of eligible nurses receiving the invitation was estimated to be approximately 5400. Of these, 4001 asked for a login key and were thus interested in participating. The data presented in the current study is from the 1032 subjects completing the questionnaire. The sample size was in accordance with criteria given by Field (2009).
Data collection
Data collection started in October 2014 and ended in November 2015. An invitation was sent by mail (n = 2000) or email (n = 20 500) to randomly selected members of the Norwegian Nurses Organisation. The invitation had the title ‘Shiftwork and health complaints study’, and participants were told to respond only if they fulfilled the inclusion criteria. Ethical approval was obtained from the Norwegian Regional Committee for Medical Research Ethics (approval number 2012/199).
Sleep measures
Daytime sleepiness was measured with the Epworth Sleepiness Scale (ESS) [9]. ESS consists of eight questions measuring average daytime sleep propensity. Items are scored on a 0 (no chance of dozing) to 3 (high chance of dozing) Likert type scale. Higher scores indicate higher daytime sleepiness. ESS is considered to have good test–retest reliability and internal consistency [32].
Insomnia was measured with the Bergen Insomnia Scale (BIS) [33]. BIS consists of 6 items assessing difficulty to initiate and maintain sleep, and nonrestorative sleep over a period of at least 1 month which disrupts the person’s everyday life, according to the DSM-IV-TR [34]. Responders reported the number of days per week. Higher total sum scores indicate more insomnia symptoms. The scale has good psychometric properties [33].
A composite measure of sleep disturbance was obtained with the Pittsburg Sleep Quality Index (PSQI) [20]. The PSQI consists of 19 items comprising seven factors: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. Items are scored either in terms of actual hourly responses, or on Likert type scale responses. The seven factors constitute an overall sleep quality score, which is used as a measure of global sleep disturbance in the current article.
All sleep variables were treated as continuous, without any cut-off points.
Musculoskeletal pain
Musculoskeletal pain was measured with the symptoms questionnaire by Steingrımsdottir, Vøllestad, Røe and Knardahl [35]. The questionnaire contains 30 questions measuring intensity and duration of various health complaints during the last month prior to responding.
For the current study, a musculoskeletal complaint severity index (MSI) was calculated. MSI was based on 11 questions measuring the intensity and duration of headache, neck pain, pain in left/right shoulder, pain in left/right forearm, pain in left/right wrist/hand, back pain, chest pain and pain in legs (e.g. ‘Symptoms and complaints last month regarding headache’). Complaint intensity was rated on a scale ranging from 0 (not bothered by pain) to 3 (very bothered by pain). Complaint duration was ranging from 1 (1–10 days) to 3 (21–31 days). A complaint severity score was then calculated for each complaint type by multiplying the intensity score by its duration (score range 0–9). The complaint severity index (MSI) was calculated as the mean severity score across the musculoskeletal regions, and was treated as a continuous variable in the analysis.
To describe the prevalence of localized pain, each one of the 11 pain regions measured in the current study was treated as a dichotomous variable (complaint intensity scores of 1 or more were indicating the presence of pain, while a score of 0 was indicating the absence of pain). The most prevalent of these pain regions were analyzed as separate outcome variables, based on the complaint severity scores described above.
Covariates (lifestyle factors and personality traits)
Physical exercise was measured with one item ‘How many times per week do you exercise to an extent that your breath becomes shortened and/or are sweating’. Answers were ranging from 1 (never) to 6 (more than four times per week). Smoking and use of oral tobacco were measured with one item each, answered in a 0 (no)/1 (yes) format. Alcohol consumption frequency was measured with one item, answered on a 1 (never) to 5 (four times per week or more) format. Circardian rhythms were measured with 7 items from the Horne-Østberg Morningness–Eveningess Questionnaire [36], which were then combined into one. Lower scores in that scale indicate morningness, while higher scores indicate eveningness.
Work factors
Extended work hours were measured with the items ‘How many overtime hours have you worked the last 4 weeks’ and ‘What is the percentage/extent/size of your full-time position’ (which in Norway describes the number of contracted hours worked). Influence over the work schedule was measured with one item (‘How much influence do you personally have regarding your working schedule’), and answers were ranging from 1 (None) to 5 (Very much). Napping frequency during nightshift was measured with one item (‘How often do you have the opportunity to take a nap during your nightshift’), with answers ranging from 1 (Very rarely) to 5 (Very often/always’). Number of night shifts worked was measured with one item (‘Approximately how many nights have you worked the last 12 months?’). Having a second (night) job was measured with two items which were entered separately in the analyses (‘Do you have other paid work?’, ‘If yes, does it include nightwork?’, answered in a yes/no format).
The psychological and social work factors quantitative job demands, role conflict, control of decisions and of work pacing, empowering leadership and organizational climate were measured with the General Nordic Questionnaire for Psychosocial and Social Factors at Work (QPSNordic) [37]. QPSNordic subscales were answered in a frequency of occurrence scale.
Physical demands of the work environment were measured with 12 items which were entered as separate factors in the analyses. These were the items, with the specific questions in parenthesis: ‘Lift objects in uncomfortable positions’ (Do you have to lift in uncomfortable positions?), ‘Work in a standing position’ (Are you working in a standing position?), ‘Working in a sitting position’ (How long are you working in a sitting position on a regular working day?), ‘Working in forward leaned position’ (Are you working in forward-leaned positions without support from hands or arms?), ‘Work with the back twisted’ (Are you working with your back twisted?), ‘Lift loads of 20 kg or more daily’ (Do you daily lift something weighting more than 20 kg, and if so, how many times per day?), ‘Lift unexpected heavy loads daily’ (Do your work tasks include being exposed to sudden unexpected heavy loads?), ‘Pull or push objects weighting more than 50 kg’ (To what degree do your working tasks include pushing or pulling persons or heavy objects weighing more than 50 kg?), ‘Consider the work environment as physically strenuous’ (How physically strenuous do you usually experience your working situation?), ‘Manually move patients in bed’ (How many times per day, evening, night shift do you manually move a patient in bed?), ‘Lift or support patients between the bed and the chair and lift’ (How many times per day, evening, night shift do you lift or support patients between the bed and the chair?), ‘Carry or push heavy objects’ (How many times per day, evening, night shift do you lift, carry or push heavy objects?). Higher scores indicate a more physically strenuous work environment.
Data analyses
The population prevalence was calculated for each of the 11 musculoskeletal complaints (regions). Before analyzing the data, a missing data frequency analysis was performed on the covariates and covariates variables with 5% or more of missing data were excluded from the analyses. Multiple regression analysis was performed to assess the associations between musculoskeletal pain and daytime sleepiness, insomnia and global sleep disturbance, after controlling for age, lifestyle and work factors. For each outcome measure, these analyses were performed in the following manner: First, a stepwise backward regression was performed with the covariates and the three sleep measures. Only the covariates and sleep variables which had associations with chance probability p < 0.1 with the outcome variable were retained for the final analyses. Next, hierarchical multiple regressions were performed, in which the significant covariates were entered at step 1. The sleep measures that survived the stepwise procedure were then entered one at a time in each of the steps that followed. Standardized beta values (β) were used to determine which of the three sleep measures (i.e. daytime sleepiness, insomnia, global sleep disturbance) had the strongest associations with each outcome variable, higher β indicating stronger association [38]. The analyses did not violate the assumptions of normality, linearity and homoscedasity, which was inspected visually through histograms, P–P plots and residuals plots, respectively. Intercorrelations between the three sleep measures can be found in Table 3. Even though the correlation between PSQI and BIS was relatively high (r = 0.718), multicollinearity between all variables was within the acceptable range (tolerance > 0.1) and average VIF was not substantially greater than 1 [38]. In the final analyses, variables with a significance level of p < .01 were considered as significant. All analyses were performed with SPSS version 23.
Results
Among our sample of nurses, 17.3% reported daytime sleepiness (a score of 11 or more in ESS indicated the presence of daytime sleepiness), 49.8% had insomnia (a score of 3 days/week or more in one or more of the first 4 questions and a score of 3 days/week or more in one or more of the questions 5 and 6 of BIS indicated insomnia), and 47.6% experienced sleep disturbance (a score of 6 or more in PSQI indicated global sleep disturbance).
Prevalence of pain regions
The most commonly reported types of pain were back pain (62.3%), headache (60.8%), and neck pain (51.8%) (Fig. 1).
Association between sleep and musculoskeletal pain index
ESS and BIS were significantly associated with musculoskeletal pain, and according to the standardized beta values (β) in Table 1, the association of BIS with musculoskeletal pain seemed to be stronger than that of ESS. PSQI was not significantly associated with musculoskeletal pain in the backward regression, hence it was not included in the final analysis (Table 1). Age, working in a forward leaned position, and having work tasks that include being exposed to sudden unexpected loads were also associated with musculoskeletal pain (Table 1).
Associations between sleep and headache, back pain and neck pain
BIS was associated with headache, back pain and neck pain complaint severity. ESS was associated with headache and neck pain complaint severity (Table 2). According to the standardized beta values in Table 2, the association of BIS with all three pain types was somewhat greater than that of ESS. PSQI was not significantly associated with localised pain in the backward regressions, hence it is not presented in Table 2. Age, working in a standing or forward leaned position, and lifting objects in uncomfortable positions or lifting unexpected loads were also associated with these three pain types (Table 2). Intercorrelations between the three sleep measures can be found in Table 3.
Discussion
The main findings of the present cross-sectional study were that insomnia measured by BIS was more strongly associated with musculoskeletal pain than sleepiness measured by ESS. This was shown both for the global musculoskeletal index, and for headache, back pain and neck pain. PSQI total score was not associated with any of the pain complaints.
In line with previous research, ESS was associated with musculoskeletal pain, headache and neck pain [39]. In addition, BIS was significantly associated with musculoskeletal pain in the present sample, in accordance with other studies. Chung and Tso [40] found that insomnia was associated with musculoskeletal pain symptoms amongst individuals suffering from depression, and attributed that finding to the distressing cognitions that accompany insomnia. Other studies have also found associations between insomnia and chronic pain [41,42,43], neck strain (whiplash), chest pain and headache [15].
PSQI total score was not associated with musculoskeletal pain in the current study. Alsaadi and coworkers [21] found that higher scores in the PSQI were associated with higher pain intensity amongst patients with acute low back pain. This discrepancy of findings can be explained by the fact that the current study controlled for two more sleep factors (i.e. daytime sleepiness and insomnia) and other covariates that could confound the relationship. It seems that the effects of PSQI total on musculoskeletal pain are no longer significant when measured simultaneously with other sleep measures. As noted above, based on VIF and tolerance values, we did not consider multicollinearity to be an issue. However, this possibility cannot be excluded completely and may have contributed to the lack of association between PSQI total and pain complaints.
The results of the present study suggest that, for the present population of nurses, sleep complaints influence musculoskeletal pain in a differential way. Insomnia symptoms showed a strong association with musculoskeletal pain in general and an even stronger association when the three most prevalent pains were analyzed separately. Subjective sleepiness had a somewhat weaker association with pain than insomnia, while PSQI total did not show an association with pain. These findings are in line with previous research, according to which pain thresholds decrease following sleep restriction [44]. Hence, it is not indifferent which sleep problems are asked for when investigating the relationship between sleep complaints and pain, as well as when treating pain [45].
In accordance with previous research also other factors, apart from sleep measures, were associated with pain amongst our sample, such as physical job demands [46] and age [22]. Some of the covariates (e.g. role conflict) were significant in the first steps of the analyses, however, when sleep measures were entered, these covariates did not continue to be significant. This indicates that, when investigating other occupational exposures on musculoskeletal pain, sleep problems should be taken into account as a potential mediator.
The current findings could possibly contribute when developing occupational health guidelines for the assessment and treatment of pain incidences. Roehrs and Roth [47] and Smith and Haythornthwaite [48] argued that the relationship between sleep and pain is bidirectional, potentially forming a vicious cycle. Addressing the specific sleep problem that an individual may have could possibly put an end to that potential circular trajectory and set the grounds for pain recovery [45] Future studies should focus on the effects that the improvement of specific sleep problems (i.e. daytime sleepiness, insomnia) may have on specific types of pain.
Limitations
The cross-sectional nature of the current study does not allow for any conclusions of direction of effects to be drawn. Our sample mainly consisted of nurses working on rotating shifts. Since rotating shift workers may have difficulties estimating their ‘average sleep’, data obtained with the PSQI could be debatable. This possible drawback was intended to be accounted for in the analyses by asking the number of nights worked during the past year. However, this could not be entered as a control variable in the analyses, since it did not survive the missing-data analyses. Selection bias could have also influenced the current findings, since the prevalence of pain complaints in our sample was quite high. e.g., the prevalence of back pain in the present sample was 62.3%, whereas the prevalence of back pain in nurses in general has been reported to be 45–47% for nurses working shift or night [49]. The relatively high prevalence indicates that nurses who agreed to participate were experiencing some kind of pain and, therefore, were more motivated to participate than nurses not experiencing pain. Thus, it is possible that the relationship between sleep and pain observed in the current study may not be the same for a population with lower prevalence of pain. Moreover, the mean age of our nurses working on rotating shifts was 41.6 years, and this may have contributed to the high prevalence of reported pain. Although the response rate for the current study was restricted, the socio-economic status of the present study can be considered homogeneous and the age range covers the full spectrum of occupational life.
Conclusion
In the current restricted population of shiftworking nurses, which showed a relatively high prevalence of pain complaints, insomnia was more strongly associated with musculoskeletal pain than subjective sleepiness. While PSQI had no association with musculoskeletal pain in this sample, this finding should not be generalized outside the current population. Designing shift plans that minimize insomnia symptoms may be a fruitful approach when trying to address musculoskeletal pain amongst nurses.
References
Akerstedt T, Nordin M, Alfredsson L, Westerholm P, Kecklund G. Sleep and sleepiness: impact of entering or leaving shiftwork–a prospective study. Chronobiol Int 2010;27:987–96.
Takahashi M, Iwakiri K, Sotoyama M, et al. Work schedule differences in sleep problems of nursing home caregivers. Appl Ergon. 2008;39:597–604.
Lorusso A, Bruno S. L’abbate N A review of low back pain and musculoskeletal disorders among Italian nursing personnel. Ind Health 2007;45:637–44.
Picavet H, Schouten J. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC 3-study. Pain. 2003;102:167–78.
Andersen LL, Clausen T, Mortensen OS, Burr H. Holtermann A A prospective cohort study on musculoskeletal risk factors for long-term sickness absence among healthcare workers in eldercare. Int Arch Occup Environ Health. 2012;85:615–22.
Lautenbacher S, Kundermann B, Krieg J-C. Sleep deprivation and pain perception. Sleep Med Rev. 2006;10:357–69.
Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain. 2013;14:1539–52.
Menefee LA, Cohen MJ, Anderson WR, Doghramji K, Frank ED, Lee H. Sleep disturbance and nonmalignant chronic pain: a comprehensive review of the literature. Pain Med. 2000;1:156–72.
Johns. MW A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–45.
Chhangani BS, Roehrs TA, Harris EJ, et al. Pain sensitivity in sleepy pain-free normals. Sleep. 2009;32:1011–17.
Harrison L, Wilson S. Munafò MR exploring the associations between sleep problems and chronic musculoskeletal pain in adolescents: a prospective cohort study. Pain Res Manag. 2014;19:e139–e45.
Roehrs TA, Harris E, Randall S, Roth T. Pain sensitivity and recovery from mild chronic sleep loss. Sleep. 2012;35:1667–72.
Huntley ED, Campo JV, Dahl RE, Lewin DS. Sleep characteristics of youth with functional abdominal pain and a healthy comparison group. J Pediatr Psychol. 2007;32:938–49.
Association AP. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Publishing.; 2013.
Sivertsen B, Lallukka T, Salo P, et al. Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. J Sleep Res. 2014;23:124 – 32.
Ødegård SS, Sand T, Engstrøm M, Stovner LJ, Zwart JA, Hagen K. The long-term effect of insomnia on primary headaches: a prospective population-based cohort study (HUNT-2 and HUNT-3). Headache: J Head Face Pain. 2011;51:570–80.
Zhang J, Lam S-P, Li S, et al. Insomnia, sleep quality, pain, and somatic symptoms: sex differences and shared genetic components. Pain. 2012;153:666–73.
Sivertsen B, Lallukka T, Petrie KJ, Steingrímsdóttir ÓA, Stubhaug A, Nielsen CS. Sleep and pain sensitivity in adults. Pain. 2015;156:1433–39.
Dzierzewski JM, Williams JM, Roditi D, et al. Daily variations in objective nighttime sleep and subjective morning pain in older adults with insomnia: evidence of covariation over time. J Am Geriatr Soc. 2010;58:925–30.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Alsaadi SM, McAuley JH, Hush JM, et al. Poor sleep quality is strongly associated with subsequent pain intensity in patients with acute low back pain. Arthritis Rheumatol. 2014;66:1388–94.
Ihlebæk C, Eriksen HR, Ursin H. Prevalence of subjective health complaints (SHC) in Norway. Scandinavian J Public Health. 2002;30:20–9.
Andersson H, Ejlertsson G, Leden I. Widespread musculoskeletal chronic pain associated with smoking. An epidemiological study in a general rural population. Scand J Rehabil Med. 1998;30:185–91.
Krismer M, Van Tulder M. Low back pain (non-specific). Best Pract Res Clin Rheumatol. 2007;21:77–91.
Merikanto I, Lahti T, Seitsalo S, et al. Behavioral trait of morningness-eveningness in association with articular and spinal diseases in a population. PloS One. 2014;9:e114635.
Ariëns GA, Bongers PM, Hoogendoorn WE, Houtman IL, van der Wal G, van. Mechelen W High quantitative job demands and low coworker support as risk factors for neck pain: results of a prospective cohort study. Spine (Phila Pa 1976). 2001;26:1896–901.
Christensen JO, Knardahl S. Work and neck pain: a prospective study of psychological, social, and mechanical risk factors. Pain. 2010;151:162–73.
Vleeshouwers J, Knardahl S, Christensen JO. Effects of psychological and social work factors on self-reported sleep disturbance and difficulties initiating sleep. Sleep. 2015;39:833.
Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J, Lang G. Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. Am J Ind Med. 2006;49:964–71.
Elfering A, Grebner S, Semmer NK, Gerber H. Time control, catecholamines and back pain among young nurses. Scand J Work Environ Health 2002:386–93.
Trinkoff AM, Geiger-Brown JM, Caruso CC, Lipscomb JA, Johantgen M, Nelson AL, Sattler BA, Selby VL. Personal safety for nurses. In: Hughes RG, editor. Personal safety for nurses. Agency for Healthcare Research and Quality, Rockville 2008. pp. 1–36.
Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376–81.
Pallesen S, Bjorvatn B, Nordhus IH, Sivertsen B, Hjørnevik M, Morin CM A new scale for measuring insomnia: the Bergen Insomnia Scale. Percept Mot Skills. 2008;107:691–706.
Association AP. Diagnostic and statistical manual of mental disorders. 4th ed. text rev.). Washington, DC: American psychiatric association; 2000.
Steingrimsdottir OA, Vollestad NK, Roe C, Knardahl S. Variation in reporting of pain and other subjective health complaints in a working population and limitations of single sample measurements. Pain. 2004;110:130–9.
Horne JA. Ostberg O A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1975;4:97–110.
Dallner M. Validation of the General Nordic Questionnaire (QPSNordic) for psychological and social factors at work. Nordic Council of Ministers [Nordiska ministerrådet], 2000.
Field A. Discovering statistics using SPSS. Sage publications, California, 2009.
Roizenblatt S, Souza AL, Palombini L, Godoy LM, Tufik S. Bittencourt LRA Musculoskeletal pain as a marker of health quality. Findings from the epidemiological sleep study among the adult population of sao paulo city. PloS One. 2015;10:e0142726.
Chung KF. Tso KC Relationship between insomnia and pain in major depressive disorder: a sleep diary and actigraphy study. Sleep Med. 2010;11:752–8.
Taylor DJ, Mallory LJ, Lichstein KL, Durrence H, Riedel BW. Bush AJ Comorbidity of chronic insomnia with medical problems. SLEEP-NEW YORK THEN WESTCHESTER-. 2007;30:213.
Smith MT, Klick B, Kozachik S, et al. Sleep onset insomnia symptoms during hospitalization for major burn injury predict chronic pain. Pain. 2008;138:497–506.
Wilson KG, Eriksson MY, Joyce L, Mikail SF. Emery PC Major depression and insomnia in chronic pain. Clin J Pain. 2002;18:77–83.
Faraut B, Léger D, Medkour T, et al. Napping reverses increased pain sensitivity due to sleep restriction. PloS One. 2015;10:e0117425.
Tang NK, Lereya ST, Boulton H, Miller MA, Wolke D, Cappuccio FP. Nonpharmacological treatments of insomnia for long-term painful conditions: a systematic review and meta-analysis of patient-reported outcomes in randomized controlled trials. Sleep. 2015;38:1751.
Manchikanti L. Epidemiology of low back pain. Pain Physician 2000;3:167–92.
Roehrs T, Roth T. Sleep and pain: interaction of two vital functions In: Sleep and pain: interaction of two vital functions. City: Copyright© 2005 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA., 2005:106–16.
Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. 2004;8:119–32.
Aagestad C, Tynes T, Sterud T, Johannessen HA, Gravseth HM, Løvseth EK. JH Alfonso, S Aasnæss Faktabok om arbeidsmiljø og helse [Facts on work environment and health]. National Institute of Occupational Health, Norway (STAMI). 2015.
Acknowledgements
We kindly acknowledge Heidi Ødegaard Notø, Tonje Gjulem and Daniel Pitz Jacobsen for assisting with data collection and processing. Funding received from: National Institute of Occupational Health, Norway. The work was performed at the National Institute of Occupational Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have seen and approved the manuscript. All authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Katsifaraki, M., Nilsen, K.B., Wærsted, M. et al. The association of sleepiness, insomnia, sleep disturbance and pain: a study amongst shiftworking nurses. Sleep Biol. Rhythms 16, 133–140 (2018). https://doi.org/10.1007/s41105-017-0135-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-017-0135-5