Abstract
Aromatherapy with essential oils is one of the most popular complementary medical tools for improving sleep quality. However, only a few reports have objectively measured the effects of essential oils on sleep. Here, we used objective and subjective measures to analyze the effects of the essential oils of lavender (Lavandula angustifolia) and sweet orange (Citrus sinensis) on the sleep quality of healthy university students. The participants were monitored for 15 consecutive nights as they inhaled lavender oil and sweet orange oil, in a crossover design. Their sleep was monitored objectively by actigraphy, and total sleep time (TST), sleep efficiency, sleep latency, and wake after sleep onset (WASO) were analyzed. Their sleep was analyzed subjectively using Oguri–Shirakawa–Azumi (OSA) sleep inventory scores. Inhalation of an essential oil improved sleep measures only in participant whose sleep quality was poor in the control condition. Lavender seemed more effective than sweet orange in objective measures, especially in improving sleep latency. In the subjective sleep analysis, the essential oils improved sleep maintenance, dreaming, and sleep length in subjects who had poor sleep quality. Sweet orange seemed more effective than lavender in the subjective sleep measures. The difference between the two oils suggests that expectancy bias had little effect on the hypnotic effect of lavender on objective sleep. Although no obvious effect was observed in good sleepers, the inhalation of lavender oil could be effective for helping poor sleepers improve objective sleep quality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep disturbance is common in developed countries, including Japan. A systematic review found that approximately 20% of Japanese adults had chronic symptomatic insomnia [1]. Another study analyzed the sleep status of a Japanese population using the Pittsburgh Sleep Quality Index (PSQI), and estimated that 26.4% of males and 31.1% of females had sleep problems [2]. People with insomnia feel dissatisfied with their sleep and impaired in their physical and social activities during the day. Furthermore, recent epidemiological and physiological studies revealed associations between sleep disturbance and various physical and psychological disorders, such as cardiovascular diseases, diabetes, mood disorders, and cognitive disorders [3,4,5,6,7]. Sleep disturbance is thought to be a risk factor for these chronic diseases and to have substantial adverse impacts on public health.
Aromatherapy is one of the most popular complementary therapies [8, 9]. Since many aroma oils are thought to provide a relaxing and sedative effect, they are frequently applied to reduce anxiety and to alleviate sleep disturbance [8,9,10,11]. A recent systematic review yielded 15 quantitative studies that examined the hypnotic effects of inhaled essential oils in human [10]. Most of these studies reported positive effects of essential oils on sleep, and lavender was the most frequently tested essential oil. Aromatherapy with lavender or other essential oils seemed effective for sleep disturbance. However, most of these studies assessed sleep quality by subjective indices such as PSQI, Profiles of Mood States (POMS), and visual analog scales. As pointed out by Howard and Hughes, the effects of the aromas were easily influenced by expectancy bias [12]. Although several studies analyzed sleep objectively with polysomnography (PSG) or actigraphy [10, 11, 13,14,15], further studies using objective measures are necessary to analyze the hypnotic effects of essential oils.
Sleep analysis with actigraphy is easy to conduct, and sleep estimation by actigraphy shows strong agreements and correlations with PSG, the gold standard of sleep examination [16, 17]. In 1995, Sadeh et al. [16] reviewed the empirical data on the validity of actigraphy and concluded that “actigraphy may be a useful, cost-effective method for assessing specific sleep disorders”. This conclusion was approved by the American Sleep Disorders Association, and provides the background for the standards for the practice of sleep medicine. Nowadays, actigraphy is recognized as a useful and validated tool for objective sleep analysis, and is widely used for sleep analysis in sleep research and in clinical [16,17,18,19,20].
In this study, we analyzed the effects of essential oils on subjective and objective sleep quality simultaneously in a crossover design. Young, healthy university students inhaled the scents of lavender oil and sweet orange oil during sleep, and their subjective and objective sleep data were analyzed using the Oguri–Shirakawa–Azumi Sleep Inventory scale for middle-aged and older adults (OSA-MA) and wrist actigraphy. Sweet orange was reported to have anxiolytic and sedative effects [21, 22]. Although both lavender and sweet orange have been thought to be effective for sleep, their components are quite different. The differences in their effects on sleep were analyzed and discussed.
Methods
Participants
The participants consisted of 12 healthy university students aged 18–24 years (8 females, 4 males). They were recruited by an announcement posted on bulletin boards at the Chiba campus of Josai International University, and volunteered to participate in the study. The participants were required to be healthy, and those who were in subjectively poor physical and/or mental condition, under medication, or diagnosed as allergic to the components used in the study were excluded. All participants fulfilled the entry criteria. Although the smoking was not included in the entry criteria, there was no smoker in the participants. Before the experiment began, an outline of the study was explained to them, and they signed their informed consent.
Materials
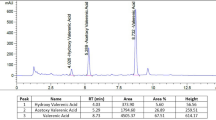
The essential oils of lavender (Lavandula angustifolia) and sweet orange (Citrus sinensis) were obtained from Pranarom (Ghislenghien, Belgium).
Sleep recording by actigraphy
Objective sleep was recorded using ActiSleepMonitor (ASM; Actigraph, Pensacola, FL, USA), and the following sleep measures were analyzed. Sleep latency: duration from the time of going to bed to the time of falling asleep (sleep onset time); wake after sleep onset (WASO): total amount of time that is scored as awake after sleep onset; total sleep time (TST): total amount of time that is scored as sleep. Sleep latency and WASO are subtracted from total time in bed; sleep efficiency: ratio of TST to total time in bed. The ASM recorded the movement score in 1 min epochs, and the collected data were analyzed by the official data analysis software for ASM, ActiLife6 (Actigraph, Pensacola, FL, USA) that uses the standard sleep scoring algorithms developed and validated by Cole and colleagues [23]. The time of going to bed at night and the time of getting up in the morning were determined by the sleep diary and the data in ASM. ActiLife6 scored individual epochs as either sleep or non-sleep, and determined the time of falling asleep and the value of sleep measures with the Cole–Kripke sleep scoring algorithm [23].
Self-evaluation of sleep by questionnaire
Subjective sleep was measured by OSA-MA [24]. Although this questionnaire was developed to measure subjective sleep in middle-aged and older adults, the OSA-MA is applicable to young adults and has been widely used for sleep analysis in various age groups [25, 26]. OSA-MA consists of 16 items scored on a four-point scale; these items are divided into five factors: (1) sleepiness on rising, (2) initiation and maintenance of sleep, (3) frequent dreaming, (4) refreshment, and (5) sleep length. A higher score means a better sleep quality. The mean ± SD of 670 Japanese (aged 26–75) were reported as follows [24]: (1) 21.0 ± 7.5, (2) 21.1 ± 6.8, (3) 23.3 ± 7.4, (4) 20.8 ± 7.6, (5) 21.4 ± 7.2.
Procedure
The total procedure took 15 consecutive days and was divided into three 5-day sessions. In the first session, the participants inhaled the first essential oil (lavender or sweet orange) every night during sleep. The second session was a control period, during which the participants took their usual sleep without any intervention. In the third session, the participants inhaled the second essential oil every night during sleep. Those who used lavender in the first session used sweet orange in the third session, and vice versa; the order for each participant was randomly assigned by the experimenter.
The participants were instructed to maintain their usual lifestyle and sleep habits in their own home during the procedure. They were instructed to write a sleep diary in which they recorded the time of going to bed at night, the time of getting up in the morning, the time of meals, and unusual events that could affect sleep quality such as vigorous exercise, alcohol and caffeine intake at night, medication, and different sleep habits. These data were used to analyze the ASM data and to confirm whether they maintained their usual lifestyle and sleep habits.
The participants were instructed to wear the ASM on the wrist of their nondominant hand during sleep every night for the 15-day study period. They were also instructed to fill out the OSA-MA after they woke up on the last morning of each session.
In the first and third sessions, each participant was instructed to drip two drops of the assigned essential oil onto a tissue paper and to place the paper by their pillow. Since the participants could easily identify the contents by the smell, they were not blinded. The participants were instructed to use the oil every night during the 5-day session.
In the analysis of sleep measures, aggregation of the data in multiple nights is routinely done because single-night measures can be easily disordered by accidental factors [27]. Some previous studies reported that 3–5, or more nights were necessary to obtain reliable aggregated measures, and the mean value might ensure reproducible individual sleep characteristics [19, 27]. We obtained objective data from each participant for each day of a session. To minimize accidental inter-day fluctuation of sleep measures, we used the mean value of each measure during the 5-day session as each participant’s value in that session. Some participants sometimes forgot to put on the ASM, and the data were missed. If data were successfully obtained from four or more nights of a session, we used the data for analysis. If data for fewer than four nights were obtained, all of that participant’s data in the session were excluded from analysis. As a result, we excluded the data of two participants (subjects 03 and 11 in Fig. 1) in the sweet orange session.
For the analysis of subjective sleep, one participant (subject 10 in Fig. 3) forgot to complete the questionnaire for the sweet orange session, and the data thus are missing.
Statistical analysis
Data are expressed as means ± SD. Data obtained from the measurement with ASM and OSA-MA were analyzed with repeated-measures ANOVA. The significance level was set at 0.05.
All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics [28].
Results
Objective sleep
Objective sleep was measured for 5 days in each session (no aroma, lavender, and sweet orange). Table 1 shows the results of each day in each session. Although the values fluctuate during 5-day session, the fluctuation seems random, and we could not find any trend such as monotonic increase/decrease according to time and high/low value in the specific day (e.g., specifically high in day 1). “No aroma” session also showed no specific trend. Since the day 1 of the “No aroma” session was the next day of the day 5 of the first essential oil session, the carryover effect of the essential oil inhalation might be concerned in the first day of “No aroma” session. As described above, however, data in Table 1 does not indicate any specific influence on the first day of “No aroma” session. We considered that the carryover effect had little effect on sleep measures in this study. We used the data in “No aroma” session as control in the following analysis.
The individual results of the analysis are shown in Fig. 1. One-way repeated-measures ANOVA could not detect any statistically significant difference between treatments (TST: F 2,18 = 1.0907, p = 0.3572, η p 2 = 0.1081; sleep efficiency: F 2,18 = 0.9161, p = 0.418, η p 2 = 0.0931; sleep latency: F 2,18 = 2.2958, p = 0.1294, η p 2 = 0.2032; WASO: F 2,18 = 0.6705, p = 0.5238, η p 2 = 0.0693). Although there was no statistically significant difference, the effect sizes suggested small to moderate effects of aroma treatment on sleep quality. As shown in Fig. 1, some participants showed large improvements by the aroma treatment. The effect of treatment on sleep might depend on the sleep quality of the participants during the control (no aroma) session. We tried to analyze with stratification.
Participants were divided into three groups according to their sleep measures obtained in the control condition: good sleepers, medial sleepers, and poor sleepers. The “good” and “poor” groups consisted of the participants who scored in the top and bottom thirds in the sleep measures, respectively. The main effects of sleep status (good, medial, and poor sleepers) and aroma treatment (no aroma, lavender, and sweet orange), as well as the interaction effect, were analyzed with two-way repeated-measures ANOVA. The results are shown in Fig. 2, and the results of the statistical analysis are summarized in Table 2.
The ANOVA revealed that the interaction between sleep status and aroma treatment was significant only in sleep latency. In other measures, the main effect of sleep status was detected in sleep efficiency and WASO. There were no statistically significant differences among the groups in TST. The effect sizes suggested small to moderate effect of aroma treatment and moderate interaction effect in all measures. The effect size of the interaction effect in sleep latency seemed large, although the η p 2 value did not meet the suggested size by Ferguson [29]. The sleep latency of poor sleepers was shorter in the lavender condition than in either the control or sweet orange condition. Figure 2 and Table 2 indicate that lavender shortened sleep latency only for people in the poor sleep quality group.
Subjective sleep
The individual results of the analysis are shown in Fig. 3. The means ± SD of all participants for each factor in the control condition were 16.2 ± 8.0 (sleepiness), 15.8 ± 5.6 (sleep maintenance), 19.0 ± 8.4 (dreaming), 18.8 ± 6.1 (refreshment), and 17.7 ± 6.1 (sleep length). Compared with the standard value of a Japanese population reported by Yamamoto et al. [24], the participants in the present study showed lower values in all measures, suggesting that as a population, their sleep quality was slightly poorer.
One-way repeated-measures ANOVA could not detect any statistically significant difference between treatments (sleepiness: F 2,20 = 1.983, p = 0.1638, η p 2 = 0.1654; maintenance: F 2,20 = 0.5629, p = 0.5783, η p 2 = 0.0532; dreaming: F 2,20 = 1.5182, p = 0.2433, η p 2 = 0.1318; refreshment: F 2,20 = 0.163, p = 0.8507, η p 2 = 0.0161; length: F 2,20 = 3.3189, p = 0.0569, η p 2 = 0.2492). The effect sizes suggested moderate effect of aroma treatment in sleep length, and small effects in sleepiness, sleep maintenance, and dreaming.
The data were stratified according to good, medial, and poor sleepers, the same as in the objective sleep analysis, and the results are shown in Fig. 4 and Table 3. Good sleepers showed higher values and poor sleepers showed lower values than the standard of a Japanese population reported by Yamamoto et al. [24] in all measures. The ANOVA revealed that the interaction between sleep status and aroma treatment was significant in sleep maintenance, dreaming, and sleep length. In other measures, the main effect of sleep status was detected in sleepiness and refreshment. The effect sizes suggested small to moderate effects of aroma treatment in sleepiness, sleep maintenance, dreaming, and sleep length. The interaction effect in these measures also showed moderate to large effect sizes. Among the poorer sleepers, sleep length seemed longer in the sweet orange condition than in the control or lavender condition. These results indicate that aroma treatment is effective for improving sleep maintenance, dreaming, and sleep length only for poor sleepers. Sweet orange seemed more effective than lavender for improving subjective sleep, especially in sleep length.
Discussion
This study investigated the effects of two essential oils, lavender and sweet orange, on objective and subjective sleep. Although neither lavender nor sweet orange improved sleep among good sleepers, both showed alleviative effects for poor sleepers in several sleep measures. Moderate to large effect sizes of the interaction effects between sleep status and aroma treatment suggested that the effect of essential oils were quite different between good sleepers and poor sleepers. In particular, lavender shortened the objective sleep latency of poor sleepers, and sweet orange lengthened the subjective sleep length of poor sleepers. Since good sleepers slept well without aroma treatment, sleep-improving effects of aroma oils could not be detected with actigraphy or the self-checked questionnaire. The present results suggest that the inhalation of essential oils during sleep is effective for alleviating mild sleep complaints.
There was an inconsistency between the results of objective and subjective sleep measures. Lavender seemed more effective for objective sleep, whereas sweet orange seemed more effective for subjective sleep. We suspect that this might be the result of individual preferences for the smell of one essential oil over the other. Some participants found the smell of sweet orange oil pleasant, but the smell of lavender essential oil not pleasant. This difference in preference could psychologically affect the self-estimation of subjective sleep.
In studies of aroma treatment thus far, participants could recognize easily which aroma oil they were inhaling. Since participants expect some positive effects of aroma treatments, it is difficult to eliminate expectancy bias [12]. We used two aroma oils in this study, and found a difference between them. Lavender greatly improved the objective sleep latency of poor sleepers, while sweet orange did not. On the other hand, sweet orange showed larger effects than lavender on subjective sleep measures. Since subjective estimations were more likely to be affected by psychological factors, the effect of sweet orange on subjective sleep may have been confounded by expectancy bias. We considered, however, that the difference between the two oils in objective sleep latency suggested that lavender had an actual effect. Since sweet orange did not show any effect on objective sleep latency, expectancy bias had little effect on object sleep latency. The effect of lavender was not due to expectancy bias. Lavender could exert alleviative effects on sleep by acting physiologically rather than psychologically.
Nagai and colleagues [30] reported the effects of olfactory stimulation with grapefruit and lavender oils on autonomic nerves. Inhalation of grapefruit essential oil activates sympathetic nerves and elicits physiological changes such as the elevation of blood pressure [31, 32]. Inhalation of lavender essential oil activates parasympathetic nerves and elicits physiological changes such as the reduction of blood pressure [33, 34]. Limonene and linalool, the main components of grapefruit and lavender oils, respectively, showed the same effects as grapefruit and lavender. Since the main component of sweet orange oil is limonene [22], sweet orange might show the same effect as grapefruit.
The effects of linalool and limonene on autonomic nerves might contribute to the results of the present study. The activation of parasympathetic nerves by linalool could enhance the sleep-inducing effect of lavender. The activation of sympathetic nerves by limonene could not induce such sleep-inducing effect in sweet orange treatment. These effects might contribute to the positive and negative effects of lavender and sweet orange, respectively, on objective sleep latency.
There are limitations in this study. Since the participants spent daily life in their usual environment and slept in their own home, the absolute control of participants’ activity and environment was impossible. The participants were instructed to keep usual lifestyle and sleep habits, and we confirmed by their sleep diaries and ASM data that there was no activity that disturbed the sleep at night. However, we could not exclude the possibility that the participants violated the protocol. Furthermore, there are other factors that could affect sleep but were not controlled in this study. Intra- and inter-individual difference in various factors such as physical and psychological stresses, unaware medical conditions, the amount and the balance of nutrition in their meal, the amount of activity in daytime, the amount of light exposure in daytime and at night, and menstrual cycle of female participants could mask the effect of essential oil inhalation. To control and exclude the effects of these factors, experiments in a sleep laboratory in which participants spend whole day in controlled condition with thorough monitoring might be effective.
We did not design a long washout period in this study. The data in Table 1 suggest that the carryover effect had little effect on sleep measures in the present experimental setting. Previous crossover studies that analyzed the effect of aroma treatment on sleep used various washout period [10, 11, 13, 14]. Some studies designed the experiments with a washout period for 2–7 days, whereas the other studies analyzed the effect with a washout period for 15–23 h. We consider that the essential oils might affect the brain activity transiently during exposure at night, and the effect would be washed out within a half day (from morning to night of the day). However, we could not exclude the possibility that the carryover effect of the first essential oil lasted for more than 5 days in the present study. In that case, the sleep quality of control session might be estimated better than it really is, and the effect of essential oils might be underestimated. The experiment with a long washout period may detect the alleviative effects of essential oils on sleep more efficiently.
In this study, we revealed that including a control condition in the stratification of sleep status is important for analyzing the hypnotic effects of essential oils because the effects were so mild that they were difficult to detect in good sleepers. Although this study was a small-scale open trial, we detected the alleviative effects of essential oils for people with poor sleep quality. In particular, lavender showed 58% (12 min) reduction in objective sleep latency in poor sleepers. The inhalation of lavender essential oil may be useful for alleviating objective sleep quality. Further study on a larger scale with objective sleep analysis in a controlled sleep laboratory would clarify more precisely the effects and the mechanisms of lavender and other essential oils on sleep quality.
References
Doi Y. Prevalence and health impacts of sleep disorders in Japan (in Japanese). J Natl Inst Public Health. 2012;61:3–10.
Doi Y, Minowa M, Uchiyama M, Okawa M. Subjective sleep quality and sleep problems in the general Japanese adult population. Psychiatry Clin Neurosci. 2001;55:213–5.
Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–92.
Beihl DA, Liese AD, Haffner SM. Sleep duration as a risk factor for incident type 2 diabetes in a multiethnic cohort. Ann Epidemiol. 2009;19:351–7.
Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64:443–9.
Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O’donnell J, Christensen D, Nicholson C, Iliff JJ, Takano T, Deane R, Nedergaard M. Sleep drives metabolite clearance from the adult brain. Science. 2013;342:373–7.
Tworoger SS, Lee S, Schernhammer ES, Grodstein F. The association of self-reported sleep duration, difficulty sleeping, and snoring with cognitive function in older women. Alzheimer Disease Assoc Disord. 2006; 20: 41 – 8.
Maddocks-Jennings W, Wilkinson JM. Aromatherapy practice in nursing: literature review. J Adv Nurs. 2004;48:93–103.
Cooke B, Ernst E. Aromatherapy: a systematic review. Br J Gen Pract. 2000;50:493.
Lillehei AS, Halcon LL. A systematic review of the effect of inhaled essential oils on sleep. J Altern Complement Med. 2014; 20: 441 – 51.
Fismer KL, Pilkington K. Lavender and sleep: a systematic review of the evidence. Eur J Integr Med. 2012;4:e436-e47.
Howard S, Hughes BM. Expectancies, not aroma, explain impact of lavender aromatherapy on psychophysiological indices of relaxation in young healthy women. Br J Health Psychol. 2008; 13: 603 – 17.
Raudenbush B, Koon J, Smith J, Zoladz P. Effects of odorant administration of objective and subjective measures of sleep quality, post-sleep mood and alertness, and cognitive performance. North Am J Psychol. 2003; 5: 181 – 92.
Goel N, Kim H, Lao RP. An olfactory stimulus modifies nighttime sleep in young men and women. Chronobiol Int. 2005;22:889–904.
Perl O, Arzi A, Sela L, Secundo L, Holtzman Y, Samnon P, Oksenberg A, Sobel N, Hairston IS. Odors enhance slow-wave activity in non-rapid eye movement sleep. J Neurophysiol. 2016; 115: 2294–302.
Sadeh A, Hauri PJ, Kripke DF, Lavie P. The role of actigraphy in the evaluation of sleep disorders. Sleep. 1995;18:288–302.
Jean-Louis G, Kripke DF, Cole RJ, Assmus JD, Langer RD. Sleep detection with an accelerometer actigraph: comparisons with polysomnography. Physiol Behav. 2001; 72:21–8.
Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003; 26: 342–92.
Littner M, Kushida CA, Anderson WM, Bailey D, Berry RB, Davila DG, Hirshkowitz M, Kapen S, Kramer M, loube D, Wise M, Johnson SF. Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: an update for 2002. Sleep. 2003; 26:337–41.
Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev. 2011; 15: 259–67.
Goes TC, Antunes FD, Alves PB, Teixeira-Silva F. Effect of sweet orange aroma on experimental anxiety in humans. J Altern Complement Med. 2012;18:798–804.
Guzmán-Gutiérrez SL, Navarrete A. pharmacological exploration of the sedative mechanism of hesperidin identified as the active principle of citrus sinensis flowers. Planta Med. 2009;75:295–301.
Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC. Automatic sleep/wake identification from wrist activity. Sleep. 1992;15:461–9.
Yamamoto Y, Tanaka H, Takase M, Yamazaki K, Azumi K, Shirakawa S. Standardization of revised version of OSA sleep inventory for middle age and aged (in Japanese). Brain Sci Mental Disord. 1999;10:401–9.
Hirokawa K, Nishimoto T, Taniguchi T. Effects of lavender aroma on sleep quality in healthy Japanese students. Percept Mot Skills. 2012; 114: 111–22.
Yamagishi R, Yokomaku A, Omoto F, Misao K, Takada K, Yoshimatsu S, Abe A, Hayashi M. Sleep-improving effects of the aromatic compound heliotropin. Sleep Biol Rhythms. 2010; 8: 254–60.
Acebo C, Sadeh A, Seifer R, Tzischinsky O, Wolfson AR, Hafer A, Carskadon MA. Estimating sleep patterns with activity monitoring in children and adolescents: how many nights are necessary for reliable measures? Sleep. 1999;22:95–103.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Ferguson C. An effect size primer: a guide for clinicians and researchers. Prof Psychol Res Pract. 2009;40:532–8.
Nagai K, Niijima A, Horii Y, Shen J, Tanida M. Olfactory stimulatory with grapefruit and lavender oils change autonomic nerve activity and physiological function. Auton Neurosci. 2014;185:29–35.
Shen J, Niijima A, Tanida M, Horii Y, Maeda K, Nagai K. Olfactory stimulation with scent of grapefruit oil affects autonomic nerves, lipolysis and appetite in rats. Neurosci Lett. 2005; 380: 289 – 94.
Tanida M, Niijima A, Shen J, Nakamura T, Nagai K. Olfactory stimulation with scent of essential oil of grapefruit affects autonomic neurotransmission and blood pressure. Brain Res. 2005;1058:44–55.
Shen J, Niijima A, Tanida M, Horii Y, Maeda K, Nagai K. Olfactory stimulation with scent of lavender oil affects autonomic nerves, lipolysis and appetite in rats. Neurosci Lett. 2005; 383: 188 – 93.
Tanida M, Niijima A, Shen J, Nakamura T, Nagai K. Olfactory stimulation with scent of lavender oil affects autonomic neurotransmission and blood pressure in rats. Neurosci Lett. 2006; 398: 155 – 60.
Acknowledgements
The authors thank the participants for taking part in this study. The authors also thank the assistance provided by H. Miyama, M. Kazato, and H. Maruyama.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and animal rights statement
This study involves human participants.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Research Ethics Committee (Josai International University) Permission Number: 32 (dated April 18, 2013).
Informed consent
Informed consent was obtained from all individual participants included in this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kawai, H., Tanaka, S., Nakamura, C. et al. Effects of essential oil inhalation on objective and subjective sleep quality in healthy university students. Sleep Biol. Rhythms 16, 37–44 (2018). https://doi.org/10.1007/s41105-017-0121-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-017-0121-y