Abstract
The aim of the study was to investigate the possible existence of a bifurcation point in sleep duration, which could differentiate children with behavioral problems from those without. We conducted a survey of children’s sleep and health between June and July 2012. A total of 383 children aged 4–6 years were studied (193 boys, 190 girls; average age 4.7 years; 223 and 160 children attended kindergarten and childcare centers, respectively), based on their parents’ reports using the Children’s ChronoType Questionnaire and the Strength and Difficulties Questionnaire. The dependent variable was the dichotomized behavior of total behavioral problems; the cut-off value was ≥13 points. The independent variable was sleep duration. The bifurcation point of sleep duration was the median value: 9.5 h for sleep period, 10.0 h for time in bed (TIB), and 10.5 h for the sum of TIB and naptime (24 h TIB). Binomial multiple logistic regression analyses were performed separately for sleep period, TIB, and 24 h TIB, which were controlled for chronotype, sex, age, and childcare programs; those corresponded to Models 1, 2, and 3, respectively. The results show that there was no significant association between total behavioral problems and sleep duration. However, using morning-type as a reference, adjusted odds ratios (95 % confidence intervals) for neither-type and evening-type were 2.06 (1.12–3.76) and 3.72 (1.60–8.66) in Model 1, 2.09 (1.14–3.82) and 3.89 (1.71–8.88) in Model 2, and 1.89 (1.03–3.50) and 3.61 (1.55–8.40) in Model 3.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep plays an important role in brain development and contributes to children’s health and well-being. In particular, children’s sleep duration is of great concern to parents. For example, some of parents’ most frequently asked questions to health professionals include whether their child is getting sufficient sleep, and how many hours of sleep are minimally required to achieve good health and development. However, according to a recent review on children’s sleep needs, there is no “magic number” or a specific hour-based sleep recommendation predicted upon the best available evidence [1].
The aim of this study was to investigate the possible existence of a bifurcation point in sleep duration, which could differentiate children with behavioral problems from those without. Chronotype, which indicates individual differences in diurnal preference, may affect the ability to determine sleep duration and sleep need [2]. Therefore, we included chronotype as a consideration, when examining the association between children’s sleep duration and their behavioral problems.
Materials and methods
Subjects and data collection
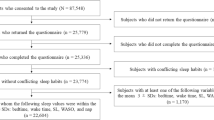
A total of 383 children aged 4–6 years were studied (193 boys, 190 girls; average age 4.7 years; 223 and 160 children attended kindergarten and childcare centers, respectively). We used parent-reported anonymous questionnaires on children’s sleep and health. The questionnaires were provided to the parents by teachers at kindergartens and childcare centers, located in Wako city in the metropolitan area of Tokyo, between June and July 2012. Details of the study protocol and procedures have been described previously [3]. This study was approved by the Institutional Review Board of the National Institute of Public Health, Japan.
Measures
Sleep durations and chronotype
Sleep durations were measured with the sleep–wake parameters in the Children’s ChronoType Questionnaire (CCTQ) [4], for weekdays and weekends. Sleep durations were defined as follows: the difference between sleep onset time and wake-up time for sleep period, the difference between bedtime and get-up time for time in bed (TIB), and the sum of TIB and naptime for 24 h TIB. The sleep durations on weekdays were used for the analyses in this study.
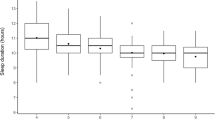
Based on our previous study [3], sleep–wake timings and sleep durations were not normally distributed; therefore, the medians [interquartile ranges (IQRs)] were presented. Sleep onset time and wake-up time (h:min) were 21:20 (1:04) and 7:00 (0:45), and bedtime and get-up time were 21:00 (1:00) and 7:00 (0:45), respectively [3]. Sleep period, TIB, and 24 h TIB were 9.58 (1.17), 10.00 (1.08), and 10.50 (1.00) h, respectively [3].
Chronotype was measured with a 10-item morningness (M)/eveningness (E) scale in the CCTQ (CCTQ-M/E). The assignment of scores for items 1, 2, 8, and 9 in the CCTQ-M/E is reversed. The total score of the CCTQ-M/E, ranging from 10 to 48, was divided into three different measures of chronotypes: ≤23 points for morning-type (M-type), 24–32 points for neither-type (N-type), and ≥33 points for evening-type (E-type). Based on the previous study [3], sleep onset times were 20:50 (1:01), 21:30 (0:53), and 22:00 (0:56), and wake-up times were 6:30 (0:40), 7:00 (0:40), and 7:00 (0:40) for M-, N-, and E-types, respectively. Bedtimes were 20:30 (1:00), 21:00 (0:45), and 21:30 (1:00), and get-up times were 6:35 (0:40), 7:01 (0:34), and 7:05 (0:40) for M-, N-, and E-types, respectively [3]. Sleep periods were 9.83 (1.09), 9.50 (1.17), and 9.00 (1.11) h, TIBs were 10.17 (1.08), 10.00 (1.25), and 9.75 (1.17) h, and 24 h TIBs were 10.50 (0.83), 10.50 (1.00), and 11.00 (1.21) h for M-, N-, and E-types, respectively [3].
The CCTQ and its Japanese version have been previously reported to be psychometrically reliable and valid [4–6].
Behavioral problems
Behavioral problems were measured with the Strengths and Difficulties Questionnaire (SDQ) [7]. The SDQ comprises five subscales with five items each: emotional symptoms, conduct problems, hyperactivity/inattention, peer problems, and prosocial behavior. In the subscales for emotional symptoms, conduct problems, hyperactivity/inattention, and peer problems, in which 5 positively worded items are reversed, each subscale score ranges from 0 to 10. In addition, the scores of the subscales, except for prosocial behaviors, can be summed to generate a total difficulties score for total behavioral problems, which ranges from 0 to 40. Therefore, higher scores for the subscales, except for the subscale of prosocial behavior, represent more behavioral problems. The cut-off values for borderline and abnormal behaviors were determined using the reference values derived from a representative sample of Japanese children [8]. The SDQ and its Japanese version have been shown to have good psychometric properties [8–10].
Statistical analyses
Sleep durations were not normally distributed; therefore, they were presented as half-hour intervals ranging from 7 to 14 h for weekdays and weekends (Fig. 1). The medians (IQRs) of sleep durations were calculated. A series of binomial logistic regression analyses were performed to examine whether sleep duration was associated with behavioral problems. The dependent variable was the dichotomized behavior of total behavioral problems as measured with the SDQ; the cut-off value was ≥13 points. The independent variables were the sleep period, TIB, and 24 h TIB on weekdays. The bifurcation point of sleep duration was assumed to be the median value; therefore, the corresponding short and long sleep durations were set at <9.5 and ≥9.5 h for the sleep period, <10.0 and ≥10.0 h for the TIB, and <10.5 and ≥10.5 h for the 24 h TIB, respectively [3]. Binomial multiple logistic regression analyses were performed separately for each sleep duration, the sleep period, the TIB, and the 24 h TIB, which were controlled for chronotype (M-type vs. N-, and E-types), sex (girls vs. boys), age (5–6-year-olds vs. 4-year-olds), and childcare programs (kindergarten vs. childcare centers); those corresponded to Models 1, 2, and 3, respectively. Both unadjusted and adjusted odds ratios (ORs) with 95 % confidence intervals (CIs) were calculated. Computations were based on the pairwise deletion of missing data. The statistical significance level was set at p < 0.05 (two-tailed). All analyses were performed using IBM SPSS Statistics for Windows, Version 20.0.
Distributions of sleep duration [sleep period (a), time in bed (TIB) (b), and TIB and naptime (24 h TIB) (c)], using the Children’s ChronoType Questionnaire (CCTQ), in preschool children aged 4–6 years attending kindergarten or childcare centers (N = 383). Black and white bars represent the number of children grouped by the categories of sleep duration at half-hour intervals from 7.0 to 14.0 h on weekdays and weekends, respectively
Results
No significant association was found between total behavioral problems and sleep period, TIB or 24 h TIB. However, total behavioral problems were significantly associated with chronotype; using M-type as a reference, adjusted ORs for N-type and E-type were 2.06 and 3.72 in Model 1, 2.09 and 3.89 in Model 2, and 1.89 and 3.61 in Model 3 (Table 1).
Discussion
This study showed that whilst sleep period, TIB, and 24 h TIB are not associated with total behavioral problems in children aged 4–6 years, chronotype does have an impact on children’s behavior. That is, a specific cut-off value of sleep duration that could differentiate children with behavioral problems from those without was not identified. N- and E-types were significantly associated with total behavioral problems.
These results are in contrast with those reported in previous studies conducted on children under 6 years of age, which suggested an association between short sleep duration and hyperactivity/impulsivity, attention problems, internalizing behavioral problems, and total psychiatric symptoms [11, 12]. However, none of these studies took into account chronotype or circadian rhythmicity in examining the aforementioned associations.
The findings obtained in our study are, however, in line with those of other studies; Komada et al. [13] reported that attention and aggressive behavioral problems were not associated with sleep duration, but rather with bedtime irregularity in 4–5-year-old Japanese nursery school children. In Komada’s study, parent-reported sleep duration was divided into short and long sleep groups by the median value (9.3 h), and behavioral problems were assessed using the Children’s Behavioral Check List (CBCL). van der Heijden et al. [14] studied school-aged children and reported that eveningness was related to the increase in total behavioral problems and attention problems; however, sleep duration hardly affected the behavioral problems. In their study, sleep duration was measured using a sleep diary. Chronotype and behavioral problems were assessed using the CCTQ and the CBCL, respectively.
According to Bax, it is rare for a child under 5 years of age, unless he or she has been forcibly kept up and kept awake, to suffer from a shortage of sleep [15]. In the present study, the median (IQR) of 24 h TIB was 10.50 (1.00) h both for weekdays and weekends, although nocturnal sleep durations were shorter on weekdays than weekends [3]. In fact, nocturnal sleep durations lengthened from weekdays to weekends without change in sleep latency [10.2 (10.2)] min: from 9.58 (1.17) to 9.83 (1.17) h for sleep period, and from 10.00 (1.08) to 10.25 (1.17) h for TIB [3]. Taking these findings together, it suggests that daytime napping compensates for an accumulated weekday sleep shortage in preschool children aged 4–6 years. As such, daytime napping as compensation for lesser total sleep duration may provide an explanation for the absence of a significant association between sleep duration and behavioral problems among these preschool children. However, the benefits and adverse effects of a daytime nap are controversial. For example, Fukuda and Asaoka [16] suggest that the delayed bedtime of nursery school children caused by a daytime nap may give rise to such problems as unwillingness to go to school and poor morning moods during their elementary school days.
Matsuoka et al. conducted a school-based study to compare sleep/wake patterns and sleep problems between children aged 6–12 years with and without developmental disorders. The former were more likely than the latter to have sleep problems including parasomnias and disordered breathing; however, there was no significant difference in sleep start time, sleep end time, and sleep duration between the two groups [17]. These findings suggest that children with developmental disorders have delayed development of sleep architecture, or a combination of abnormal neuromuscular control and anatomical upper airway narrowing, whereas they show no difference in the regulation of sleep–wake timing and sleep duration compared to children without developmental disorders. Further research on younger children to examine whether a significant difference in sleep/wake patterns exists between developmentally delayed and developmentally normal children will provide us with insight into developmental sleep–wake control mechanisms.
This study had a few limitations. First, the participants, who all lived in a certain area, were not necessarily representative of preschool children attending kindergarten or childcare centers across the whole of Japan. Second, the sample size was small. Therefore, the present study did not analyze a relationship between sleep duration and each subscale of behavioral problems—emotional symptoms, conduct problems, hyperactivity/inattention, peer problems, and prosocial behavioral problems—because the reliable value of OR with a 95 % CI for each behavioral problem was not obtained. Therefore, the study did not consider more than two categories of sleep durations. Third, the cross-sectional design used in this study could not establish a cause-effect relationship.
In conclusion, the present study reveals that there is substantial individual variation in the amount of sleep among preschool children aged 4–6 years attending kindergarten or childcare centers. It suggests that their behavioral problems are not significantly associated with sleep duration, but rather associated with their chronotype, if the child’s actual sleep duration meets his or her biological sleep need. Further research is warranted to explore optimal sleep, in terms of its amount, timing, regularity, and circadian preference, for improving developmental behavioral function in young children.
References
Matricciani L, Blunden S, Rigney G, Williams MT, Olds TS. Children’s sleep needs: is there sufficient evidence to recommend optimal sleep for children? Sleep. 2013;36:527–34.
Roepke SE, Duffy JF. Differential impact of chronotype on weekday and weekend sleep timing and duration. Nat Sci Sleep. 2010;2010:213–20.
Doi Y, Ishihara K, Uchiyama M. Sleep/wake patterns and circadian typology in preschool children based on standardized parental self-reports. Chronobiol Int. 2014;31:328–36.
Werner H, Lebourgeois MK, Geiger A, Jenni OG. Assessment of chronotype in four- to eleven-year-old children: reliability and validity of the Children’s Chronotype Questionnaire (CCTQ). Chronobiol Int. 2009;26:992–1014.
Doi Y, Ishihara K, Uchiyama M, Takimoto H. Development of the Japanese version of Children’s ChronoType Questionnaire. Jpn J Sleep Med. 2013;7:486–93 (in Japanese).
Ishihara K, Doi Y, Uchiyama M. The reliability and validity of the Japanese version of the Children’s ChronoType Questionnaire (CCTQ) in preschool children. Chronobiol Int. 2014;31:947–53.
Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry. 1997;38:581–6.
Matsuishi T, Nagano M, Araki Y, et al. Scale properties of the Japanese version of the Strengths and Difficulties Questionnaire (SDQ): a study of infant and school children in community samples. Brain Dev. 2008;30:410–5.
Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40:1337–45.
Doi Y, Ishihara K, Uchiyama M. Reliability of the Strengths and Difficulties Questionnaire in Japanese preschool children aged 4–6 years. J Epidemiol. 2014;24:514–8.
Paavonen EJ, Porkka-Heiskanen T, Lahikainen AR. Sleep quality, duration and behavioral symptoms among 5-6-year-old children. Eur Child Adolesc Psychiatry. 2009;18:747–54.
Touchette E, Petit D, Seguin JR, Boivin M, Tremblay RE, Montplaisir JY. Associations between sleep duration patterns and behavioral/cognitive functioning at school entry. Sleep. 2007;30:1213–9.
Komada Y, Abe T, Okajima I, et al. Short sleep duration and irregular bedtime are associated with increased behavioral problems among Japanese preschool-age children. Tohoku J Exp Med. 2011;224:127–36.
van der Heijden KB, de Sonneville LM, Swaab H. Association of eveningness with problem behavior in children: a mediating role of impaired sleep. Chronobiol Int. 2013;30:919–29.
Bax MC. Sleep disturbance in the young child. Br Med J. 1980;280:1177–9.
Fukuda K, Asaoka S. Delayed bedtime of nursery school children, caused by the obligatory nap, lasts during the elementary school period. Sleep Biol Rhythms. 2004;2:129–34.
Matsuoka M, Nagamitsu S, Iwasaki M, et al. High incidence of sleep problems in children with developmental disorders: results of a questionnaire survey in a Japanese elementary school. Brain Dev. 2014;36:35–44.
Acknowledgments
This work was supported by JSPS KAKENHI Grant Number 23390181 and partly by a Research Grant from the Japan Society for Promoting Science and Technology Agency (22591301, 2011–2012). The authors thank all the parents, kindergartens, and childcare centers that participated in this study. The authors also thank Midori Kajitani for her assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Doi, Y., Ishihara, K. & Uchiyama, M. Sleep duration in relation to behavioral problems among Japanese preschool children. Sleep Biol. Rhythms 14, 107–111 (2016). https://doi.org/10.1007/s41105-015-0028-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-015-0028-4