Abstract
Purpose
This is a prospective observational study from November 2020 to 2022 over 104 cases with an objective (a) to determine the incidence along with the clinicopathologic characteristics, (b) to find risk factors associated and its management (c) to evaluate the outcome of GTD after follow-up.
Methods
After detailed clinical and laboratory investigation, all cases of molar pregnancy were subjected for suction and evacuation followed by histopathological study and serum β-hCG. During its follow up visit, detailed history for signs and patterns of serum β-hCG was noted, categorized as high risk or low risk GTN and treated accordingly.
Results
The incidence was found to be 4.6/1000 pregnancies. A maximum of 66 cases (63.4%) were of O+ve, mostly presenting with amenorrhea. 84 cases (80.8%) were hydatidiform mole and 20 cases (19.2%) were of pGTT with 80 cases (76.9%) complete mole, 04 cases (3.8%) partial mole, 15 cases (14.4%) invasive mole and 5 cases (4.8%) choriocarcinoma. Suction & evacuation was done in all 86 cases (82.6%) of hydatidiform mole, hysterectomy in 12 cases (11.5%) and chemotherapy in 45 cases (43.2%) of GTN among which 40 cases (88.9%) completed follow up of 6 months with remission and only 5 cases (11.1%) developed resistant. FIGO scoring system showed 20 cases (44.4%) of low risk, 16 cases (35.5%) of medium risk and 9 cases (20%) of high risk.
Conclusion
Routine ultrasonography, appropriate diagnosis, treatment and follow up leads to near 100% cure. A multi-centered study and proper counseling is essential to determine the true incidence and overall outcome of molar pregnancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational trophoblastic disease (GTD) includes a series of disorders characterized by an abnormal proliferation of trophoblastic tissue with varying tendency to spontaneous remission, local invasion and metastasis [1]. It includes complete & partial hydatidiform mole, invasive mole, choriocarcinoma, placental site trophoblastic tumor (PSTT), epithelioid trophoblastic tumor (ETT) and atypical placental site nodule. Hydatidiform moles have been commonly found in adolescents and elderly women having prior history or family history of molar pregnancy. It is also commonly associated with vitamin deficiencies and in women who smoke regularly. There has been widespread variation in the incidence of molar pregnancy across the world. These discrepancies are mainly due to calculation of incidence in various hospital-based data or population-based data on basis of per number of pregnancies, number of live births or number of deliveries. The incidence is highest in Indonesia [2]. In past two decades owing to widespread use of routine first-trimester ultrasound, early detection and management of molar pregnancy is possible [3]. The classical triad of molar pregnancy still continues to be amenorrhea, irregular bleeding PV and passage of grape like vesicles. The basic management of GTD continues to be suction evacuation and regular follow up with serum β-hCG to detect persistent gestational trophoblastic disease (pGTD). Clinical findings of appropriate uterine involution, ovarian cyst regression and cessation of bleeding per vagina and reassuring signs of pGTD should be treated with appropriate chemotherapy as per the risk scoring. Proper reporting and follow up can prevent mortality associated with malignant transformation [4].
Materials and Methods
The current study is a prospective observational study conducted in the Department of O & G, MKCG Medical College and Hospital, Berhampur; Odisha from November 2020 to 2022 over 104 cases with an objective (a) to determine the incidence of molar pregnancies along with its clinic-pathological characteristics, (b) to find out risk factors associated with GTD and its management (c) to evaluate the outcome of GTD cases after a follow-up of 6 months. Cases were selected according to inclusion and exclusion criteria as follows: Inclusion criteria: all the cases diagnosed as GTD either histologically or sonographically which included complete mole, partial mole, invasive mole, choriocarcinoma, PSTT and ETT. Exclusion criteria: (a) all other intrauterine pregnancies, (b) unwillingness to give consent for the study. After detailed clinical and laboratory investigation, cases were classified as per FIGO classification as molar pregnancy and GTN (gestational trophoblastic neoplasia). All cases of molar pregnancy (complete and partial) were subjected for suction and evacuations followed by histopathological study (HP study) and regular follow up at an interval of 15 days with serum β-hCG up to 6 months. During follow up visit, detailed history for signs of GTN and pattern of serum β-hCG was noted and further categorized as high risk or low risk GTN and treated accordingly. Descriptive statistics were used to summarize and analyze the continuous and categorical variables using SPSS version 21 of Microsoft XL.
Results
In the present study, total 22,480 deliveries enrolled from November 2020 to 2022 and 104 cases of GTD were diagnosed, treated and followed up for a period of 6 months. Incidence of molar pregnancies was found to be 4.6/1000 (2.85 in 1000 deliveries). Maximum of 83 cases (79.8%) were in age group of > 20–30 years with a mean age of 25.19 + 6.38 years. Maximum number of 56 cases (53.8%) presented in the first trimester (≤ 12 weeks), 46 cases (44.2%) between 13 and 20 weeks and only 2 cases (1.9%) presented after 20 weeks of gestation with a mean gestational age of 13.33 + 4.76 weeks. Only one case had no history of amenorrhea. Among all cases, maximum of 66 cases (63.4%) were of O+ve, 18 cases (17.3%) were of A+ve, 14 cases (13.4%) were of B+ve and 02 cases (1.9%) were of AB+ve. Only 2 cases (1.9%) of Rh-negative blood groups were noted. Out of all cases admitted with history of amenorrhea, 86 cases (82.6%) had bleeding per vaginum, 28 cases (26.9%) had pain abdomen, 8 cases (7.6%) had passage of grape like vesicles and 3 cases (2.8%) had hyperemesis as chief complain. Hyperthyroidism, pre-eclampsia and dry cough was seen in one case (0.9%) each (Fig. 1).
Among all cases at the time of first presentation, 84 cases (80.8%) were of hydatidiform mole and 20 cases (19.2%) were of pGTT. Among the 84 cases of hydatidiform mole, 80 cases (76.9%) belonged to complete mole and 04 cases (3.8%) belonged to partial mole while pGTT includes 15 cases (14.4%) of invasive mole and 5 cases (4.8%) of choriocarcinoma. During course of treatment 27 cases (32.1%) of molar pregnancy underwent GTN. After investigation, all the 80 cases (76.9%) of complete mole diagnosed on USG were confirmed on HP report. But only 4 cases (3.8%) of partial mole were diagnosed on USG whereas 6 cases (5.7%) of partial mole were diagnosed on HP study. Out of 15 cases (14.4%) of Invasive mole diagnosed on USG, 10 cases (9.6%) were confirmed on HP study. Among choriocarcinoma, 05 cases (4.8%) were diagnosed on USG whereas 08 cases (7.6%) were confirmed on HP report (Fig. 2).
On evaluation of antecedent pregnancy, among the 45 cases (43.2%) of GTN it was seen that 20 cases of (44.4%) complete mole, 07 cases (6.7%) of invasive mole and 05 cases (4.8%) of choriocarcinoma follows term pregnancy whereas 07 cases (6.7%) of complete mole, 02 cases (1.9%) of invasive mole and 3 cases (2.8%) of choriocarcinoma follows non molar abortion. Only 1 case (0.9%) of invasive mole developed after molar abortion. It was also seen that interval between GTN and antecedent pregnancy were as follows: < 6 months in 80 cases (76.9%) of hydatidiform mole, 10 cases (9.6%) of invasive mole and 05 cases (4.8%) of choriocarcinoma and > 6 months in 6 cases (5.7%) of hydatidiform mole and 3 cases (2.8%) of choriocarcinoma.
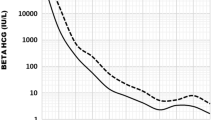
Out of 80 cases of complete mole, 64 cases (61.5%) had snow storm appearance in USG, 12 cases (11.5%) had bilateral cystic ovaries and 4 cases (3.8%) had unilateral cystic ovaries. Mass lesion in uterus was found in 03 cases (2.8%) of choriocarcinoma, metastatic lung lesion on chest X-ray was seen in 13 cases (12.5%). Invasion in myometrium was found in 16 cases (15.3%) of invasive mole and choriocarcinoma. Only 1 case (0.9%) each of focal lesion in the liver on CT abdomen and lesion in the brain matter was suggestive of liver and brain metastasis. Majority of cases, 68 cases (65.3%) had pre-evacuation β-hCG level of 1000–10,000 IU/mL, 5 cases (4.8%) had level of 10,000–100,000 IU/ml and 31 cases (29.8%) had level of > 100,000 IU/mL. The pre evacuation β-hCG levels were higher in complete mole as compared to partial mole which was statistically significant. (P value is 0.006). Maximum of 72 cases (69.2%) had Hb between 8 and 12 gm%, 20 cases (19.2%) had Hb < 8 gm% requiring blood transfusion while 12 cases (11.5%) had Hb > 12 gm%. Suction and evacuation was done in all cases (82.6%) of hydatidiform mole. Hysterectomy was done in 12 cases (11.5%) while chemotherapy was given in 45 cases (43.2%) of GTN which included 27 cases (25.9%) of post molar GTN, 10 cases (9.6%) of invasive mole and 8 cases (7.6%) of choriocarcinoma. Among all cases of hydatidiform mole, 27 cases (25.9%) had raised or plateau in serum β-hCG level which was further followed up by chemotherapy. Among the cases subjected for chemotherapy, 40 cases (88.9%) completed follow up of 6 months and had spontaneous remission and only 5 cases (11.1%) had developed resistant and treated subsequently. All cases of GTN were classified according to anatomical and FIGO scoring system and planned for either single agent or combination agent chemotherapy along with or without hysterectomy (Tables 1, 2).
Out of 86 cases that underwent suction and evacuation, 40 cases (46.5%) developed complications which included 12 cases (13.9%) of hemorrhage requiring blood transfusion, 27 cases (31.3%) of persistent GTN requiring chemotherapy and one case (1.1%) of incomplete evacuation. Out of 45 cases of GTN, 36 cases (80%) were in stage-I, 03 cases (6.7%) were in stage-II with sub-urethral nodule in one of the case, 05 cases (11.1%) were in stage-III involving lungs and 1 case (2.2%) was in stage-IV with liver and brain metastasis. These were further classified as WHO modified FIGO scoring with 20 cases (44.4%) as low risk (< 4), 16 cases (35.5%) as medium risk and 9 cases (20%) as high risk (> 8) category (Table 2).
Out of 8 cases (17.7%) of choriocarcinoma, 03 cases (6.6%) were at low risk and received MTX + FA whereas 05 cases (11.1%) were at high risk who received EMA–CO regimen. Out of 10 cases (22.2%) of invasive mole, 05 cases (11.1%) were at low risk and received MTX + FA whereas 5 cases (11.1%) were at high risk received EMA–CO regimen. Among the 27 cases (25.9%) of post molar GTN, only 1 case (2.2%) was at high risk who received EMA–CO while the rest were at low risk being treated with MTX + FA. Among the 20 low risk cases, 18 cases (40%) achieved remission and 2 cases (4.4%) of GTN developed resistance. Among the two resistant cases, one case underwent hysterectomy along with EMA–CO regimen and achieved remission while another achieved remission with EMA–CO regimen only. Only 01 case (2.2%) of GTN in the moderate risk group underwent hysterectomy along with EMA–CO regimen & achieved remission and rest 15 cases had remission with EMA–CO regimen. Out of 9 cases (8.6%) of high risk score who received EMACO regimen, 07 cases (6.7%) developed remission and 02 cases (1.9%) developed resistance. The 2 high risk cases that develop resistance had undergone hysterectomy along with chemotherapy by EMA–CO regimen (Table 3).
The lost to follow up counted to 4 cases (3.8%) in this study. Out of all, maximum of 33 cases (31.7%) achieved remission within 4–8 weeks whereas 10 cases (9.6%) had negative β-hCG within 4 weeks and 10 cases (9.6%) attained remission by 12 weeks of follow up. Outstanding 27 cases were found to be GTN. Among the cases subjected for chemotherapy, 23 cases (22.1%) developed complications which included 19 cases (42.2%) of anemia, 8 cases (17.7%) of intractable bleeding, 6 cases (13.3%) of shortness of breath, 21 cases (46.6%) with HDCU admission, 12 cases (26.6%) underwent emergency laparotomy, 2 cases (4.4%) with ICU admission and only 1 case had (2.2%) myelo-suppression following EMA–CO therapy (Fig. 2). Only 1 case (2.2%) of choriocarcinoma died within 2 days of admission which was admitted at a very late stage with features of neurological defects and multi-organ failure suggestive of liver and brain metastasis.
Discussion
There is wide geographical variation in the incidence of GTD. The incidence of GTD in the present study is 4.6 per 1000 pregnancies which is consistent with rates found in previous hospital-based studies in Eastern Nepal (4.17 per 1000 live births), Kathmandu (3.94 per 1000 deliveries) [5]. A majority of 83 cases (79.8%) were in ≥ 20–30 years of age group with mean age of 25.19 + 6.38 years. Similar study conducted by Kumar et al. [6] showed that majority of their cases (66%) was in the age group of 20–25 years with mean age 24.6 ± 4.4 years. Again Dinesh Kumar et al. also reported highest incidence in age group of 20–30 years [7]. WHO prognostic scoring system earlier for GTD had included ABO blood group as one of the prognostic factor. If female and male partner are with blood group either O or A, A or O respectively it carries better prognosis when compared with female having blood group B or AB. Here high incidence of GTD in patients with blood group O positive (63.4%) followed by blood group ‘A’ (17.3%) and the least was noted in blood group ‘AB’ thereby resulting in good outcome, comparable to Jethwani et al. and Chandran et al. [8, 9]. Majority of cases (53.7%) were presented in the first trimester which is not concurrent to Ocheke et al. (44%) and Fatima et al. (31.6%) [10, 11]. The mean gestational age during diagnosis was 13.33 ± 4.76 weeks in current study, comparable to Nirmala et al. [12] (11 ± 3 weeks). All cases except one, i.e., 99% cases is presented with history of amenorrhea, 82.6% cases with vaginal bleeding is concurrent to Koirala et al. (86.3%) and Fatima et al. (94.2%) [5, 11]. Complete mole was found in 76.9% cases, i.e., majority of GTD were of molar pregnancy which is similar to Fatima et al. Invasive mole accounts for 9.6% of cases of GTD, i.e., second most common entity which is not similar to Kumar et al. [6] who found partial mole as the second most common instead of invasive mole. The serum β-hCG is the most sensitive and specific for diagnosis and follows up of GTN. An increasing level of total β-hCG is diagnostic of invasive disease and choriocarcinoma that helps to determine treatment response and recurrence of tumor. A majority of cases (65.3%) had pre-evacuation β-hCG values between 1000 and 10,000 IU/mL and only 5 cases (4.8%) had their β-hCG between 10,000 and 100,000 IU/ml, not concurrent to Lakra et al. [13] (18.4% cases) having serum β-hCG level > 100,000 IU/ml. Suction and evacuation was the primary management in 82.6% cases of GTD. Hysterectomy was performed in 12 cases (11.5%) and chemotherapy was given in 45 cases (43.2%) which is similar to Agrawal et al. [14] (87.5%). The current study revealed 44.4% cases of low risk and 20% cases of high risk women among GTN cases which is not concurrent to Chandran JR et.al (high risk:93.6% and low risk: 6.4%) [8]. Among 45 cases of GTN, 36 cases (80%) were in stage I, 03 cases (6.6%) in stage II and 05 cases (11.1%) was in stage III and 1 case (2.2%) in stage IV with liver and brain metastasis. Among 20 low risk cases, 18 cases (40%) achieved remission and 2 cases (4.4%) of GTN developed resistance (one case underwent hysterectomy along with EMA–CO and achieved remission and the other case received only EMA–CO thus achieving remission). Only 01 case (2.2%) of moderate risk underwent hysterectomy along with EMA–CO & achieved remission and other 15 cases achieved remission with EMA–CO regimen. About 9 cases (8.6%) of high risk score who received EMACO, 07 cases (6.7%) achieved remission and 02 cases (1.9%) of choriocarcinoma developed resistance and further treated with hysterectomy along with EMA–CO which is similar to Hussain et al. [15] showing 96.29% complete remission by 1st line treatment modality. Complications usually associated with GTN include anemia, haemorrhage, and HDCU admission in current study which can be due to patients coming at a very late stage where the disease is aggressive. Anaemia (42.2%) is the most common complication followed by shortness of breath (13.3%), emergency exploratory laparotomy (26.6%), intractable bleeding (17.7%), and HDCU/ICU support (46.6%) which is similar to Agarwal et.al and Wang et al. [14, 16]. One case of myelo-suppression following EMA–CO therapy and was treated subsequently with 3 doses of Filgrastim.
Conclusion
Asian women are at increased risk of having molar pregnancies. The prevalence of gestational trophoblastic disease was higher than the published reports from non-Asian population which is consistent with earlier epidemiological studies from Asian population. Routine use of ultrasonography leads to diagnosis of molar pregnancy in the first rather than late second trimester. Appropriate diagnosis, treatment and follow up leads to near 100% cure. Majority of cases are cured by simple surgical intervention. Follow up of the patients remains a challenging task. Uncomplicated molar pregnancy should have shorter duration of follow up not exceeding 6 months after attaining an undetectable level of serum beta hCG. Longer follow up protocol do not pose additional benefit but rather increases financial and emotional burdens on to the women and also health providers both of which attribute to poor compliance. Proper counseling is essential to have a proper follow up. A multi-centered study is essential in India to determine the true incidence and overall outcome of molar pregnancy that will help in the understanding of the burden of the disease. There is a need to establish a centralized disease specific registry to ensure unbiased and non-selected data because of paucity of epidemiological studies from India.
References
Smith HO. Gestational trophoblastic disease epidemiology and trends. Clin Obstet Gynecol. 2003;46:541–56. https://doi.org/10.1097/00003081-2000309000-00006.
Altieri A, Franceschi S, Ferlay J, La Vecchia C. Epidemiology and aetiology of gestational trophoblastic diseases. Lancet Oncol. 2003;4:670–8. https://doi.org/10.1016/s1470-2045(03)01245-2.
Lybol C, Thomas CMG, Bulten J, JaaM VD, Sweep FCGJ, Massuger LFAG. Increase in the incidence of gestational trophoblastic disease in The Netherlands. Gynecol Oncol. 2011;121(2):334–8.
Szulman AE, Surti U. The syndrome of hydatidiform mole. II. Morphologic evaluation of the complete and partial mole. Am J Obstet Gynecol. 1978;132:20–7. https://doi.org/10.1016/0002-9378(78)90792-5.
Koirala A, Khatiwada P, Giri A, Kandel P, Regmi M, Upreti D. The Demographics of molar pregnancies in BPKIHS. Kathmandu Univ Med J. 2011;9(4):298–300.
Kumar N, Saxena YK, Rathi AK, Chitra R, Kumar P. Host and risk factors for gestational trophoblastic disease: a hospital-based analysis from India. Med Sci Monit. 2003;9(10):CR442–7.
Sarma D, Chinthala M. Gestational trophoblastic disease: study on incidence and management at a tertiary centre. Indian J Basic Appl Med Res. 2017;7(1):317–24.
Jethwani L, Rekhachoudhury. Clinicoepidemiological Study of Molar pregnancies in a tertiary care centre: a prospective observational study. Int J Sci Res. 2017;6(7):2277–8179.
Chandran JR, Sumangala Devi D, Gorhatti SN. Epidemiology of gestational trophoblastic disease at a Tertiary Hospital in India over last 8 years. J South Asian Fed Obstet Gynecol. 2019;11(1):27–9.
Ocheke AN, Musa J, Uamai AO. Hydatidiform mole in Jos, Nigeria. Niger Med J J Niger Med Assoc. 2011;52(4):223–6.
Fatima M, Kasi PM, Baloch SN, Kassi M. Incidence, management, and outcome of molar pregnancies at a tertiary care hospital in Quetta, Pakistan. ISRN Obstet Gynecol. 2011;2011: 925316.
Nirmala CK, Nor Azlin MI, Harry SR, Lim PS, Shafiee MN, Nur Azurah AG, et al. Outcome of molar pregnancies in Malaysia: a tertiary centre experience. J Obstet Gynaecol J Inst Obstet Gynaecol. 2013;33(2):191–3.
Lakra P, Sangwan V, Siwach S. Outcome of gestational trophoblastic disease in a rural tertiary centre of Haryana, India. Int J Reprod Contracept Obstet Gynecol. 2017;6(1):271–5.
Agrawal N, Sagtani RA, Budhathoki SS, Pokhare HP. Clinicopathological profile of molar pregnancies in a tertiary care centre of Eastern Nepal: a retrospective review of medical records. Gynecol Oncol Res Pract. 2015;2:9–12.
Hussain SS, Raees M, Rahim R. Ten-year review of gestational trophoblastic disease at Lady Reading Hospital, Peshawar. Cureus. 2022;14(7):e26620. https://doi.org/10.7759/cureus.26620.
Wang Z, Han P, Zhu X, Ying J, Qian J. Role of emergency surgery for fatal complications of gestational trophoblastic neoplasia: a single-center experience. Cancer Manag Res. 2022;14:851–61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sahoo, S., Palo, I., Sahu, M. et al. Clinicopathological Study of Gestational Trophoblastic Disease (GTD) in a Tertiary Care Hospital. Indian J Gynecol Oncolog 21, 71 (2023). https://doi.org/10.1007/s40944-023-00745-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-023-00745-1