Abstract
Turner mosaic with Y chromosome material has increased risk for germ cell tumor. A high index of suspicion is important while evaluating an adolescent female with dysgerminoma and amenorrhea. Karyotyping plays a major role in girls with suspected gonadal dysgenesis as detection of Y chromosome necessitates a prophylactic gonadectomy. Here, we report a 21-year-old woman with short stature, normal secondary sexual characteristics and primary amenorrhea who had torsion right ovarian cyst at 13 years of age and underwent excision of gangrenous right ovary. HPR was dysgerminoma ovary. Initial karyotyping done was normal but later in view of disease recurrence and amenorrhea with elevated FSH, repeat karyotyping done which revealed Turner mosaic with Y chromosome. She underwent right adnexal mass excision with prophylactic left gonadectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gonadoblastoma and dysgerminoma are the most common gonadal neoplasm that develops in dysgenetic gonads [1]. Gonadal dysgenesis is a genetic condition due to errors in cell division or alterations in genetic material, leading to complete or partial loss of gonadal development. Turner syndrome is a common type of chromosomal aneuploidy and it occurs in 1:2500 female live births [2]. 50 to 60% of patients with Turner syndrome will have 45X, karyotype and the rest will have partial X chromosome or mosaicism [3]. Abnormal Y chromosome is seen in 4–38% of Turner syndrome as reported in various studies [4]. In Y chromosome patients, the risk of gonadoblastoma is 22–43% [4] and 50% will progress into invasive dysgerminoma [5]. So prophylactic gonadectomy is usually offered in patients with Turner syndrome with Y chromosome. A high index of suspicion is necessary to identify Turner mosaic in girls with dysgerminoma and gonadal dysgenesis as a minority can have normal secondary sexual characteristics. Here, we report a patient with Turner mosaic with dysgerminoma, normal secondary sexual characteristics and without streak gonads.
Case Report
A 21-year-old unmarried woman presented to our center with lower abdominal pain in April 2019. In 2011, at 13 years of age, she had acute abdominal pain and was diagnosed to have torsion of right ovarian cyst. She underwent emergency laparotomy noted to have gangrenous right ovary and underwent right salpingo-oophorectomy at another center. Histopathology of the specimen revealed it to be a dysgerminoma of the ovary with torsion. She was evaluated for primary amenorrhea on follow-up. In view of short stature, karyotyping was done and it revealed her genotype to be 46,XX. She was given oral contraceptive pills at another center and had occasional withdrawal bleeding per vagina.
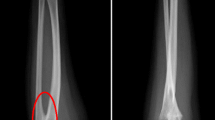
In view of her abdominal pain, CECT abdomen and pelvis were done and it showed a 7 × 6.5 cm heterogeneous lesion in the pelvis with the left ovary not being separately visualized and with doubtful fat plane with small bowel. LDH was 540 U/L and other tumor markers AFP and β-HCG were within normal limits. As per the multidisciplinary tumor board discussion, she was planned for surgery. She underwent laparotomy, and intraoperatively, there was 8 × 8 cm right adnexal mass infiltrating caecum and multiple small bowel loops. In view of extensive bowel resection required for clearance of the tumor and based on previous right oophorectomy pathology dysgerminoma with elevated LDH, it was decided for chemotherapy and re-assessment. She received BEP (bleomycin, etoposide, platinum) chemotherapy for four cycles. Re-assessment CECT abdomen and pelvis showed a residual heterogenous right ovarian cystic lesion 3 × 2 cm (Fig. 1). Post-chemotherapy LDH was 246U/L.
She had a normal female secondary sexual development, but in view of her short stature, amenorrhea, FSH was done and it was 120 IU/L. Karyotyping was repeated which revealed Turner mosaic with Y chromosome (Fig. 2).
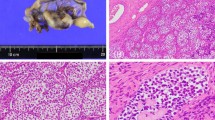
Patient and family were counseled for bilateral gonadectomy as the karyotyping showed mosaic Turner with Y chromosome. She underwent excision of right adnexal mass and left salpingo-oophorectomy and omentectomy as a part of interval debulking surgery. Intraoperatively, left ovary appeared normal. Histopathology report was gonadoblastoma in both ovaries with features of post-chemotherapy changes in right adnexal mass. She is on follow-up and her recent tumor markers and ultrasound abdomen are normal.
Discussion
In our patient, classical phenotype of Turner syndrome was absent except for the short stature. As she had dysgerminoma at 13 years of age with stunted growth and primary amenorrhea, there was a suspicion of dysgenetic gonads though the imaging showed normal left ovary. She had elevated FSH, and second karyotyping revealed the presence of Y chromosome. The possible explanation for first karyotype being normal could be undetected mosaicism as only 20 to 30 peripheral blood lymphocytes are analyzed for karyotype determination [6]. This repeat karyotyping helped us to counsel the patient and family for prophylactic gonadectomy on the left side as the left ovary was normal but final histopathology revealed gonadoblastoma in both ovaries.
Turner syndrome is caused by absent or abnormal X chromosome, and it is one of the most common chromosomal abnormalities and seen in one in 2500 female live births [5]. Pure 45X is the most common karyotype seen in 50% of individuals with Turner syndrome. Classical phenotype includes short stature, webbed neck, skeletal deformities, hearing deficit, cardiac and renal anomalies, gonadal dysgenesis (streak gonads) with impaired sexual development [7]. The remaining 50% are mosaic cases carrying normal and abnormal cell lines together with Y chromosome fragments detected in 10–11% of cases [8]. Few studies have quoted the presence of Y chromosome in Turner syndrome up to 40% [9]. Most of the classical Turner with 45X karyotype are detected at birth, while Turner mosaic diagnosis can be delayed and detected at adolescence while evaluating for stunted growth, delayed puberty and few patients can attain menarche and will have secondary amenorrhea or menstrual irregularities or infertility [7].
Dysgenetic gonads are the risk factor for developing germ cell tumors. The precursor lesion which develops in dysgenetic gonad is gonadoblastoma and 60% progress to invasive dysgerminoma and rarely to embryonic carcinoma, teratoma, yolk sac tumor and choriocarcinoma [10]. 90% of patients with gonadoblastoma have Y chromosome material in their genetic evaluation [11]. The risk of gonadoblastoma in presence of Y chromosome is 30% [12]. The presence of Y chromosome serves as a risk factor due to the presence of specific part of the Y chromosome that is known as the gonadoblastoma region of the Y chromosome (GBY) [13]. In Turner girls with 45X,46XY without signs of virilization, the tumor development is usually seen in post-pubertal ages [13]. The GBY locus is seen in the pericentromeric region, and the candidate gene within this region testis-specific protein on the Y chromosome (TSPY) has been studied extensively in the pathogenesis of gonadoblastoma [14].
The classical cytogenetic analysis is performed in thirty metaphases, which allows detection of 10% mosaicism and in Turner girls with less than 10% mosaicism can go undetected by this method [9]. FISH and PCR analyses can be used to detect low-level mosaicism [15]. The American College of Medical Genetics (ACMG) recommends karyotyping a minimum of 30 cells due to the high incidence of mosaicism in Turner syndrome, unless mosaicism is encountered within the first 20 cells. If there is a high index of clinical suspicion of Turner syndrome in a patient with a 46,XX karyotype, FISH study of a second tissue type is advised. In view of high risk of gonadoblastoma with occult Y chromosome mosaicism, the ACMG recommends 200 cell FISH analysis when 30-cell karyotype results in a nonmosaic 45,X karyotype [16].
Molecular testing for Y chromosome material should be recommended for all patients with Turner syndrome to detect individuals at high risk for gonadoblastoma. Prophylactic gonadectomy has been recently recommended for all girls with Turner mosaicism having Y chromosome [13].
Conclusion
A critical clinical analysis is needed while evaluating an adolescent female with dysgerminoma and any suspicious features of Turner or gonadal dysgenesis which further warrant molecular screening. Identification of Y chromosome in a Turner mosaic plays an important role as they have high risk for development of germ cell tumors and they need a prophylactic gonadectomy.
References
Piazza MJ. Germ cell tumors in Dysgenetic gonads. Clinics. 2019; Nov 4. https://doi.org/10.6061/clinics/2019/e408
Cui X. A basic understanding of turner syndrome: incidence, complications, diagnosis, and treatment. Intract Rare Dis Res. 2018;7(4):223–8. https://doi.org/10.5582/irdr.2017.01056.
Bianco B. Detection of hidden Y mosaicism in turner’s syndrome: importance in the prevention of gonadoblastoma. J Pediatr Endocrinol Metab. 2006;19(9):1113–8.
Kwon A. Risk of gonadoblastoma development in patients with turner syndrome with cryptic Y chromosome material. HORM CANC. 2017. https://doi.org/10.1007/s12672-017-0291-8.
Mancilla E. Y chromosome sequences in turner’s syndrome: association with virilization and gonadoblastoma. J Pediatr Endocrinol Metab. 2003;16(8):1157–63.
Yorifuji T. PCR-based detection of mosaicism in turner syndrome patients. Hum Genet. 1997;99:62–5.
Alwan IA. Turner syndrome genotype and phenotype and their effect on presenting features and timing of diagnosis. Int J Health Sci. 2014;8(2):195–202.
Doger E. Reproductive and obstetric outcomes in mosaic Turner’s Syndrome: a cross-sectional study and review of the literature. Reprod Biol Endocrinol. 2015;13:59.
Oliveira RMRD. Y chromosome in Turner syndrome: review of the literature. Sao Paulo Med J. 2009;127:6.
Kota SK. Dysgerminoma in a female with turner syndrome and Y chromosome material: a case-based review of literature. Indian J Endocrinol Metab. 2012;16(3):436–40.
Marqui ABTD. Prevalence of Y-chromosome sequences and gonadoblastoma in Turner syndrome. Rev Paul Pediatr. 2016;34(1):114–21.
Gravholt CH. Occurrence of gonadoblastoma in females with turner syndrome and Y chromosome material: a population study. J Clin Endocrinol Metab. 2000;85(9):3199–202.
Yüce Ö. Gonadoblastoma with dysgerminoma in a phenotypically turner-like girl with 45, X/46, XY karyotype. J Clin Res Pediatr Endocrinol. 2015;7(4):336–9.
Looijenga LHJ. Gonadal tumours and DSD. Best Pract Res Clin Endocrinol Metabol. 2010;24:291–310.
Rasouli M. Mosaic Turner syndrome presenting with a 46, XY karyotype. Case Rep Obstet Gynecol. 2019. https://doi.org/10.1155/2019/3719178
Wolff DJ. Laboratory guideline for turner syndrome. Genet Med. 2010;12(1):52–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abinaya, R.N., Rema, P., Suchetha, S. et al. Significance of Y Chromosome in a Turner Mosaic Girl with Dysgerminoma: Case Report with Literature Review. Indian J Gynecol Oncolog 19, 98 (2021). https://doi.org/10.1007/s40944-021-00563-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-021-00563-3