Abstract
Introduction
Isolated Splenic metastasis from ovarian cancer rarely occurs with only very few cases recorded in the literature. It can occur as a synchronous metastasis or as late as 20 years post-primary debulking surgery.
Case Report
A 62-year-old woman with carcinoma ovary stage IIIC was treated with primary debulking surgery in 2009, followed by six cycles of chemotherapy. In 2013, she was found to have an elevated serum CA-125 level during her regular follow-up. Imaging with CT scan abdomen showed a hyperdense lesion in splenic parenchyma of 2.1 × 2.4 cm. She underwent laparoscopic splenectomy. Histopathological examination revealed adenocarcinoma localised to the spleen, consistent with metastasis carcinoma ovary. Post-splenectomy, her CA-125 level returned to normal. Over the last 6 years, she is on regular follow-up and remains disease-free.
Conclusion
Isolated, solitary splenic metastasis from epithelial ovarian cancer is very rare. It occurred after a DFI of 4 years and was successfully treated and is remaining disease-free without any chemotherapy for the last 7 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The spleen is the largest lymphoid tissue in the body, but it is not a common site of metastasis in patients with ovarian cancer [1]. Malignancies that frequently metastasise to spleen arise from colon, breast, lung, melanoma, ovarian and uterine cancers. According to the clinicopathologic studies in populations with carcinoma, splenic metastases from non-hematologic malignancies are very rare, with an incidence rate of about 0.6–1.1% [2]. Splenic metastasis generally occurs as part of multi-visceral metastatic disease [3]. They can present simultaneously or after as long as 20 years of post-primary debulking surgery [4]. They may present with painful splenomegaly or fully asymptomatic and detected only during routine follow-up. Here we report a 62-year-old lady with isolated, solitary splenic metastasis occurring after a DFI of 4-years and was successfully treated and is remaining disease-free without any chemotherapy for the last 7 years.
Case Report
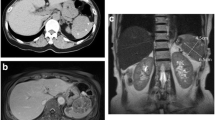
A 62-year-old female, presented with complaints of abdominal distension of 1-week duration. CT scan abdomen done on 24 October 2009 showed a complex solid and cystic mass of 7.3 × 9.5 cm arising from both the adnexa and extending into the pouch of Douglas. Deposits were noted on the superior surface of the bladder and omentum with ascites. Her Ca-125 was 3400 U/ml. Clinically and radiologically, she was diagnosed with ovarian cancer stage IIIC, and she underwent primary debulking surgery (total abdominal hysterectomy, bilateral salpingo-oophorectomy, omentectomy and appendicectomy) on 31 October 2009. This was followed by six cycles of chemotherapy. In 2013, while on routine follow-up her CA 125 was found to be high − 1772.0 U/ml and CEA was found to be 2.18 ng/ml. Imaging with CT scan abdomen showed a hyperdense lesion in the splenic parenchyma of 2.1 × 2.4 cm (Figs. 1, 2). There was no disease elsewhere. No evidence of septation or calcification was seen. She underwent laparoscopic splenectomy. Grossly there was no disease in the abdomen. So peritoneal washings were not taken for cytologic examination. Spleen was extracted intact through a small lower abdominal midline incision. On gross examination of specimen, spleen size was 12.5 × 7.5 × 3 cm, the surface was normal, cut section showed a well-circumscribed, granular, friable grey-brown lesion measuring 2.9 × 2.3 × 2.5 cm. Rest of the spleen appeared unremarkable. Histopathology revealed metastatic moderately differentiated adenocarcinoma. Previous slides were reviewed, and it was found to be consistent with metastasis from adenocarcinoma ovary. After splenectomy, her CA-125 level returned to normal. At 1-month follow-up CA 125 level was 6.41 U/ml. As she was not willing, and that was the only site of disease, no further chemotherapy was administered. Over the last 7 years, she is on regular follow-up and remains disease-free.
Discussion
Splenic metastases, defined as parenchymal lesion from non-hematologic malignancies, are very rare, with an incidence rate of about 0.6–1.1% [2]. Solid tumours that commonly metastasise to spleen originate from colon, breast, lung, melanoma, and gynaecologic cancers. Isolated Splenic metastases from ovarian carcinomas are very rare [4, 5]. Splenic metastases usually take place in the context of multi-visceral disseminated disease. However, due to the improvement of imaging techniques and the increasing number of long-term survivors with cancer, the number of cases of isolated splenic metastasis has been increased [5].
Several theories were proposed to explain the rarity of splenic metastases (1) the underdeveloped lymphoid system of the spleen, especially the lack of afferent lymphatic vessels, prevents the spleen from receiving metastatic tumour cells; (2) splenic artery branching from the celiac trunk is in a sharp angle, this makes it difficult or the tumor cells to enter the spleen (3) the growth of micrometastatic foci may be hindered by the microenvironment of the spleen (4) rhythmic contractions of the spleen results in continuous blood flow and prevents tumour cells from settling in the spleen.
Solitary splenic metastasis is considered to occur through the hematogenous route. Majority of isolated, solitary splenic metastasis are completely asymptomatic and are diagnosed incidentally. Only a few patients with splenic metastasis become symptomatic because of the presence of spontaneous rupture of the spleen [6, 7]. Some patients harbouring splenic metastases may complain of fatigue, weight loss, fever, abdominal pain, splenomegaly, anaemia, or thrombocytopenia [8]. In our patient, the raised CA125 level gave a clue regarding the relapse, and further investigations showed splenic metastasis. Generally, during the oncologic follow-up, when an isolated splenic lesion is found, a metastatic origin should be suspected. The overall prognosis looks good for patients with solitary splenic metastasis of ovarian cancer treated by splenectomy, followed by chemotherapy. Serum CA-125 is a useful biomarker for follow-up of these patients [9]. Splenectomy decreases chances of the tumour spreading to distal areas from the spleen and enhances long-term survival. Survival after splenectomy in patients with isolated splenic metastasis from ovarian carcinoma varies from 0.5 to 7 years [9, 10]. There is increasing evidence that laparoscopic splenectomy is a safe alternative to open resection in the treatment of isolated splenic metastasis [11,12,13,14]. With splenectomy alone, our patient is remaining disease-free even after 7 years.
Conclusion
Metastasis to the spleen from solid tumours is rare. Due to more vigilant patient follow-up and advancements in imaging modalities, the reported cases of splenic metastasis are increasing. These patients require prolonged follow-up with serial imaging to detect recurrence because delayed recurrence can occur, and the patients may be asymptomatic. Recent reports suggest that laparoscopic splenectomy is a safe alternative to open resection in cases of isolated splenic metastasis. Our patient is remaining disease-free, almost 7-years, and is in good performance status.
References
Pisanu A, Ravarino A, Nieddu R, et al. Synchronous isolated splenic metastasis from colon carcinoma and concomitant splenic abscess: a case report and review of the literature. World J Gastroenterol. 2007;13:5516–20.
Lam KY, Tang V. Metastatic tumours to the spleen: a 25-year clinicopathologic study. Arch Pathol Lab Med. 2000;124:526–30.
Karni D, Kopelman D. Hatoum OA solitary splenic metastasis of ovarian carcinoma: a case report. J Med Case Rep. 2014;8(1):154.
Izuishi K, Sano T, Usuki H, Okano K, Masaki T, Kushida Y, et al. Isolated splenic metastasis of ovarian cancer 20 years after operation: a case report and literature review. Tumori. 2010;96(5):784–6.
Resta G, Vedana L, Marino S, Scagliarini L, Bandi M, Anania G. Isolated splenic metastasis of ovaric cancer. Case report and literature review. G Chir. 2014;35(7–8):181–4.
Berge T. Splenic metastases. Frequencies and patterns. Acta Pathol Microbiol Scand A. 1974;82(4):499–506.
Salani R, Axtell A, Gerardi M, Holschneider C, Bristow RE. Limited utility of conventional criteria for predicting unresectable disease in patients with advanced-stage epithelial ovarian cancer. Gynecol Oncol. 2008;108(2):271–5.
Belinkie SA, Narayanan NC, Russell JC, Becker DR. Splenic abscess associated with Streptococcus bovis septicemia and neoplastic lesions of the colon. Dis Colon Rectum. 1983;26(12):823–4.
Furuya M. Ovarian cancer stroma pathophysiology and the roles in cancer development. Cancer. 2012;4(3):701–24.
Lv M, Li Y, Luo C, Liu P, Yang J. Splenic metastasis of ovarian clear cell adenocarcinoma: a case report and review of the literature. Exp Ther Med. 2014;7(4):982–6.
Gallotta V, Nero C, Lodoli C, Chiantera V, Pacelli V, Fagotti A, et al. Laparoscopic splenectomy for secondary cytoreduction in ovarian cancer patients with localized spleen recurrence: feasibility and technique. J Minim Invasive Gynecol. 2016;23(3):425–8.
Yasuda K, Yoshimura T, Kitade H, Yanagida H, Hosaka N. Laparoscopic splenectomy for solitary splenic metastasis in a patient with ovarian cancer with a long disease-free interval: a case report. J Med Case Rep. 2018;12(1):132. https://doi.org/10.1186/s13256-018-1673-4.
Paterniti TA, Ahmad S, Holloway RW. Robotic-assisted laparoscopic splenectomy for recurrent ovarian cancer. Int J Gynecol Cancer. 2020. https://doi.org/10.1136/ijgc-2020-001384.
Acosta-Torres S, Fader AN. Laparoscopic splenectomy for secondary cytoreduction of ovarian cancer in a woman with localized splenic recurrence. Gynecol Oncol. 2020;156(3):744–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, S.S., Nazarudeen, F., Rajanbabu, A. et al. Isolated Splenic Metastasis from Ovarian Carcinoma. Indian J Gynecol Oncolog 18, 98 (2020). https://doi.org/10.1007/s40944-020-00446-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-020-00446-z