Abstract
Purpose
Rotator cuff (RC) tears affect many individuals around the globe. Ambiguity of rotator cuff repair surgical outcomes is currently a limitation that is associated with fat accumulation and atrophy in the rotator cuff muscles. To improve the efficacy of rotator cuff repairs, a deeper understanding of the root causes is required. Traditionally, the term “fat infiltration” has been used to described fatty changes in muscle after rotator cuff tears. This paper introduces the concept of fat expansion as a more appropriate description for the appearance of fatty rotator cuff tear pathological changes. Furthermore, the contribution of fibroadipogenic progenitor (FAP) cells to pathological changes associated with rotator cuff injuries is presented to characterize the molecular basis of impairment. Lastly, the field of regenerative engineering is discussed as a promising solution to the pathological changes associated with rotator cuff tears.
Methods
The connection between fatty infiltration, fat expansion, fat accumulation, fibroadipogenic cells, and regenerative engineering in the context of rotator cuff tears was explored using the databases PubMed and Google Scholar.
Results
Numerous articles have supported the role of muscle resident fibroadipogenic cells as a contributor to rotator cuff tear pathological changes. In addition, regenerative engineering solutions prove to improve the pathological changes associated with rotator cuff tears.
Conclusion
The term fat expansion is more appropriate to describe fat accumulation associated with rotator cuff tears, and the employment of regenerative engineering treatment strategies improve the pathological changes associated with rotator cuff tears.
Lay Summary
Fat accumulation after rotator cuff tears has been associated with post-operative complications. Infiltration or entering of adipocytes from the external muscle environment has historically been the reported cause of the rapid increase in fat and muscle atrophy observed after rotor cuff tears. This review will dismiss the use of the term fat infiltration and acknowledge the implications of muscle resident stem cells, known as fibroadipogenic (FAP) cells, to rotator cuff tear pathological changes. Additionally, regenerative engineering, a field which seeks to regenerate various tissues using biomaterial-based scaffolds and stem cells, will be discussed as a potential solution for pathological changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rotator cuff tears (RCT), also referred to as rotator cuff ruptures or rotator cuff tendon tears, represent prevalent orthopedic injuries associated with substantial discomfort and functional impairment in patients [1]. The primary therapeutic intervention for rotator cuff tendon tears is rotator cuff repair surgery [2]. Therapeutic outcomes are currently limited by the rate of retear after surgery (which can range from 13–94%) [3]. Fat accumulation within the muscle and muscle atrophy have been correlated with high retear rates after surgical repair of the rotator cuff [9]. As a result, clinicians and researchers across several disciplines have dedicated an extensive effort to clarify the etiological agents of adipogenic and atrophic changes associated with rotator cuff muscle injuries [4, 5].
The current understanding in the field posits that the entry of cells originating from outside the muscle contributes to the proliferation of fat cells or adipocytes within the muscle after rotator cuff tears, hence the term “fat infiltration.” This concept was first introduced by Goutallier et al. based on their initial observation of fat accumulation in patients with chronic RCTs [6, 7]. Subsequent histological studies in patients with RCTs have provided further support for the concept of fat infiltration as the presence of increased fat cells in the affected rotator cuff muscles post-RCTs has been observed [8]. Additionally, animal studies investigating RCT pathology have also confirmed the increase in fat content in the muscle following tendon resection of rotator cuff muscles [9, 10]. However, these studies have not definitively identified whether the accumulation of fat cells following RCTs is indeed attributed to cells that infiltrate into the muscle from locations external to the muscle. An example of locations external to the muscle includes the epimuscular fat deposit, which is a sheath of fat that encapsulates the muscle, or the subcutaneous fat deposits, which are located underneath the skin [11]. So, while Goutallier et al.’s initial observations led to the understanding of fat accumulation after RCTs, the concept of fat infiltration introduced by them has not been supported by sufficient evidence and has consequently led to a misinformed understanding of the etiological agents responsible for RCT related fatty changes.
More recently, a population of precursor cells residing in the interstitial space of muscle, known as “fibroadipogenic progenitor cells” (FAPs), has emerged as the main if not only contributor to fat accumulation and other pathological changes associated with rotator cuff tears (Fig. 2) [12]. FAPs have been observed to differentiate into both adipocytes and fibroblasts—which form the fibrotic tissue observed following rotator cuff tears [12]. This newfound understanding of the pathological contributors to rotator cuff tears suggests that the term “fat expansion” is more appropriate to describe the fatty changes observed in these tears. Therefore, in this review, we will introduce the term “fat expansion” as a new and more appropriate term to describe the fatty changes associated with rotator cuff tears, disabusing the field of the concept of “fat infiltration.” Further, the current knowledge on FAPs will be covered to give insight for therapeutic efforts.
The precise underlying cause of muscle atrophy in relation to rotator cuff tears remains elusive. However, an interesting finding has emerged from biopsies of patients with chronic rotator cuff tears that demonstrated the co-localization of fatty tissue with exclusively fibrotic tissue [13]. Furthermore, in additional biopsy samples, there has been close spatial association between fatty tissue, apoptosis—cell death—and additionally myophagocytosis, which refers to the cellular engulfment of muscle tissue [13]. These observations have been used collectively to suggest that the expansion of fatty tissue after rotator cuff tears may replace the space filled by muscle tissue that have undergone atrophic processes [13]. Nonetheless, the precise molecular mechanism leading to the atrophy of muscle tissue in this context remains unknown. However, recent in vitro studies have shed light on this matter by demonstrating that adipocytes derived from fibroadipogenic progenitor cells (FAPs) in human patients exhibit insulin resistance [14]. Insulin-resistant adipocytes have been linked to lipotoxicity, which refers to the excessive accumulation of lipids in non-adipose tissues, such as skeletal muscle [15, 16]. Lipotoxic conditions have been associated with muscle cell death, resulting in muscle atrophy in myopathic diseases [17]. While further in vivo investigation is imperative, the observed insulin resistance characteristic in “defective” adipocytes derived from FAPs offers a potential molecular basis for the muscle atrophy observed in RCT patients.
In recent years, the pioneering field of regenerative engineering, founded by Dr. Cato T. Laurencin, has developed promising approaches to overcome the current limitations in treatment options for patients with rotator cuff tendon tears (Fig. 1) [18]. Regenerative engineering utilizes a systematic, converging platform comprising stem cell science, advanced material science, physics, and developmental biology to permit and enhance tissue regeneration [18]. Material-based approaches using novel biomaterial-based matrices have proven to reduce adipogenic, atrophic, and even fibrotic changes associated with rotator cuff tears [3, 19]. Therefore, the field of regenerative engineering has the potential to transform rotator cuff tear treatment options by targeting pathological changes associated with poor surgical outcomes. In this review, we comprehensively discuss the concept of “fat expansion” as a more appropriate description for the appearance of fatty rotator cuff tear pathological changes over the existing “fatty infiltration” concept. Further, the connection between fatty infiltration, fat expansion, and fat accumulation will be discussed. Additionally, the field of regenerative engineering will be explored as a promising solution to the pathological changes associated with rotator cuff tears.
Schematic of rotator cuff tear implicated concepts. Fat accumulation, fibrosis, and muscle atrophy are observed after rotator cuff tears. Fibroadipogenic progenitor cells (FAP) and lipotoxicity are cellular and molecular agents, respectively, that are implicated in the pathophysiology of rotator cuff tears. Regenerative engineering is a field that aims to innovate approaches to treating rotator cuff tears using novel biomaterial combinations that are used to generate matrices and scaffolds using fabrication methods such as electrospinning and 3D printing
Reevaluating the Term “Fat Infiltration” in the Context of RCTs
In the medical field, “infiltration” refers to the phenomenon where certain cell types invade regions outside their usual locations, resulting in an abnormal accumulation of these cells. Hematopoietic stem cells provide a notable example as they are released from the bone marrow into the bloodstream, where they mature into lymphocytes—a specific type of white blood cell in the immune system [20]. In the context of cancer, these lymphocytes infiltrate cancerous tumors, leading to their accumulation within the tumor tissue [21, 22]. Various techniques, such as in vivo and in vitro cell labeling methods, have been employed to track the migration and penetration of lymphocytes into cancerous tissues [22]. However, the concept of “fat infiltration,” which describes the pathological accumulation of fatty tissue after RCTs, lacks conclusive evidence to demonstrate that cells indeed penetrate the muscle following rotator cuff tendon tears and contribute to fatty tissue accumulation. Thus, this section aims to highlight the limitations in the supporting evidence for the concept of fat infiltration in the context of rotator cuff tears by demonstrating the inadequacy of the techniques used to support this concept.
Limitations of Supporting Evidence for Fat Infiltration in Muscles Affected by RCTs: Insufficiencies Undermining the Concept
In 1995, Goutallier et al., the pioneer of the concept of fat infiltration in the context of rotator cuff tendon tears, described the observation of abnormal fatty tissue accumulation in patients with rotator cuff tear injuries using computed tomography (CT) scans. CT scans have been used widely since their observation supports the notion of fat infiltration following rotator cuff tendon tears [23, 24]. Additionally, MRI scans have also been used to support the concept of fat infiltration [25]. For example, Longo et al. in 2023 employed MR imaging to assess the extent of fat infiltration in patients with varying degrees of rotator cuff tear injuries [8]. Additionally, Junjie et al. illustrated the utility of MRI in developing predictive measures for overall fat accumulation, or “fat infiltration” as they termed it, in the muscle post rotator cuff tear injuries [26]. However, it is important to note that the CT and MRI scans used to support the notion of fat infiltration merely identify the presence of fatty tissue in the rotator cuff muscle of patients with rotator cuff tears without providing insights into the origin, migration, and penetration of these fat cells into the muscle.
Additionally, histological evaluations in animal models of rotator cuff tears have been used to provide support for the concept of fat infiltration. These evaluations demonstrate an increased accumulation of fatty tissue in the muscle of the rotator cuff following tendon resection. For instance, a study involving a mouse model of rotator cuff tendon tear revealed heightened fat accumulation in the muscle post-tendon resection, which was verified through the quantification of intramuscular fat (IMF) using standard histological markers like Oil Red O and trichrome staining [26]. Similarly, Vargas-Vila et al. employed the rabbit model for rotator cuff tears, using Oil Red O to histologically outline the architectural evolution and histological shifts as fatty tissue accumulated following supraspinatus tendon resection [27]. However, such histological assessments mainly provide a before-and-after representation of fat accumulation without providing any information of the origin or migration of the cells contributing to accumulation of fatty tissue after rotator cuff tendon tear. Thus, the concept of “fat infiltration” in RCTs warrants further examination, as much of the available evidence fails to establish a definitive understanding of the origin, migration, and penetration of cells that contribute to fatty tissue accumulation within the muscle tissue. Until there is substantiated evidence confirming the notion of fat infiltration of the muscle after rotator cuff tendon tear, it is essential to disabuse the field of the term fat infiltration in the context of rotator cuff tears. Further confirmation using appropriate techniques for determining the origin, migration, and penetration of the cells into the muscle following rotator cuff tendon tears is necessary to support the concept of fat infiltration.
Fibroadipogenic Progenitor Cells: Unveiling the Role in Fat Expansion Pathogenesis Associated with Rotator Cuff Tendon Tears
As previously mentioned, insufficient evidence exists to support the prevalent concept of “fat infiltration” in the context of rotator cuff tendon tears, highlighting the need for a more appropriate terminology to describe the observed pathological fatty changes. A more fitting term, “fat expansion,” which can also be referred to as adipose tissue expansion, emerges as a suitable alternative, as it describes the increased number and/or size of adipocytes, that results in adipose tissue growth within a specific fat deposit [16]. In the context of rotator cuff tendon tears, the overall augmentation of the intramuscular fat deposit (IMFD), localized within the musculature, has garnered substantial support in the scientific and clinical literature, therefore supporting the conception of the term fat expansion [27, 28]. Additionally, the term fat expansion accurately captures the involvement of specific cell types—whose involvement is excluded with the term fat infiltration—in the pathological fatty changes associated with rotator cuff tears. Specifically, fibroadipogenic progenitor cells (FAPs), residing within the muscle, have recently been identified as the main contributor to the fatty changes associated with rotator cuff tears demonstrating their importance in fat expansion [12].
In the next section, we will delve into the exploration of fibroadipogenic progenitor cells and their intricate role in the pathogenesis of fat expansion associated with rotator cuff tendon tears. By understanding these cells, we aim to enhance our knowledge of rotator cuff tear pathology and pave the way for therapeutic strategies.
FAP Cell Identification
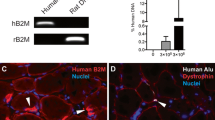
Fibroadipogenic progenitor cells (FAPs) are a distinct cell population extensively investigated in animal and adult tissues. Uezumi et al. initially characterized FAPs by employing fluorescence-activated cell sorting after enzymatic digestion of murine skeletal muscle [29]. FAPs were found to be positive for platelet-derived growth factor alpha (PDGFRα) but negative for the satellite cell marker (SM/C-2.6), endothelial cell marker (CD31), also referred to as (PECAM-1), and hematopoietic stem cell marker (CD45) [29]. In a separate study, Joe et al. used a different fluorescence-activated cell sorting method to isolate FAPs from murine skeletal muscle [30]. They described FAPs as cells lacking CD45, CD31, and alpha-7-integrin, but expressing stem cell antigen-1 (SCA-1) and the stem cell-surface antigen (CD34) [30]. Additionally, subpopulations within the FAP cell pool have been described to express the cell surface marker PDGFRβ [31]. These findings collectively indicate that FAPs represent a distinctive population of muscle progenitor cells characterized by distinct surface marker expression profiles (Fig. 2).
Muscle resident progenitor cell location and rotator cuff tear symptomology. (A) Fibro-adipogenic progenitor (FAP) cell location and satellite cell location in rotator cuff muscle. FAP cells reside in the extracellular space between muscle cells or myofibers (green). These cells have both adipogenic and fibrotic potential. Satellite cells (red) have myogenic potential and are important in the regeneration of skeletal muscle. (B) Fat accumulation, fibrosis, and muscle atrophy after rotator cuff injury. Characteristic of rotator cuff injuries is the accumulation of fat cells within muscle (yellow) as well as increased fibrotic cells (pink) between muscle fibers. FAP cells (seen in A) contribute to fibrosis and fat accumulation. Decreased myocyte diameter or muscle atrophy is a hallmark symptom of chronic rotator cuff tears
Adipogenic Fates of FAPs
Adipogenic differentiation of fibroadipogenic progenitor cells (FAPs) can give rise to various adipocyte phenotypes, including white, beige, and brown adipocytes (Fig. 3) [32]. Each phenotype exhibits distinct morphological and biological characteristics. White adipocytes, for example, are characterized by large unilocular lipid vacuoles, whereas beige/brown adipocytes display multilocular lipid vacuoles [32]. Brown/beige adipocytes are further distinguished by dense mitochondrial packing and high expression levels of the mitochondrial marker uncoupling protein-1 (UP-1) [32]. The precise mechanism governing the adipogenic fate of FAP cells following rotator cuff tears remains poorly understood. However, it has been suggested that the transcription factor Odd-skipped related 1 (OSR-1), known for its role in musculoskeletal development, might be involved in modulating the adipogenic fate of FAP cells [33]. Increased expression of OSR-1 has been observed in FAPs following muscle injury compared to non-injury conditions [33]. Moreover, in a mouse model, FAPs with high OSR-1 expression (referred to as OSR-1 positive FAP cells) were found to colocalize with perilipin, a known white adipocyte marker, after muscle injury, suggesting that OSR-1 may promote FAP adipogenic differentiation toward a white adipocyte trajectory [33].
Differentiation potentials of fibroadipogenic progenitor (FAP) cells. Fibroadipogenic progenitor cells are a distinct group of progenitor cells found within the interstitial space between muscle fibers. FAPs may differentiate into fibroblast (red), white adipocytes (tan), beige adipocytes (brown), and brown adipocytes (dark brown) in response to muscle injury
FAPs’ Role in Rotator Cuff Tear Fat Expansion
After rotator cuff tendon tears, fibroadipogenic progenitor cells (FAPs) have emerged as the primary contributor to intramuscular fat expansion. In a mouse model of rotator cuff tendon tear, it was observed that 96% of PDGFRα-labeled FAPs co-localized with the late-stage adipogenic marker adiponectin after tendon resection [34]. Additionally, 83% of PDGFRα-labeled FAPs were found to colocalize with PPARγ [34]. This suggests that PDGFRα-labeled FAPs play a significant role in adipogenesis following tendon injury. It was also reported that the proliferation of PDGFRα + FAPs precedes adipogenesis and the appearance of adipogenic transcription factors, indicating a relationship between the expansion of PDGFRα + FAPs and adipogenesis after injury. Moreover, inhibition of PDGFR signaling has been shown to reduce intramuscular fat expansion in a murine rotator cuff tear model [35]. Additionally, the promotion of FAP apoptosis using a TGF-β small molecule inhibitor resulted in a significant reduction in intramuscular fat in a mouse rotator cuff injury model [36]. These studies provide support for the claim that FAPs are the main if not only contributors to rotator cuff tear fat expansion. Notably, FAPs within the rotator cuff demonstrated the highest proliferative and adipogenic potential compared to FAPs from other muscle groups, highlighting the significance of the FAP population within this anatomical location [37]. Collectively, these studies provide compelling evidence of the profound impact of FAPs on fat expansion following rotator cuff tendon tears.
Insulin Resistance in FAP-Derived White Fat Cells: Implications for Rotator Cuff Muscle Atrophy
The metabolic phenomenon of lipotoxicity, which encompasses the inappropriate buildup of lipids within non-adipose tissues, has emerged as a pivotal contributor to cellular dysfunction and subsequent cell death. This process’s role in the pathology underlying rotator cuff tears has been increasingly illuminated through a range of animal model studies, underscoring its potential significance in understanding, and addressing this medical issue. Flück et al. reported alterations in gene expression as well as lipidome—the number of lipid species in a cell—changes related to fat accumulation in a sheep RCT model [38, 39]. The study revealed that rotator cuff tears was connected with the upregulation of 227 lipid species within the defected muscle and elevated levels of the adipocyte differentiation marker Peroxisome Proliferator Activated Receptor 2γ (PPAR2γ) [39]. Of the 227 lipid species upregulated, triglyceride levels were the highest [39]. Increasing triglyceride content within the skeletal muscle after rotator cuff injury may be caused by a specific muscle resident progenitor cell population referred to as fibroadipogenic progenitor cells (FAPs).
FAPs that differentiate into white adipocytes have been reported to be insulin insensitive or insulin resistant by Arrighi et al. [14]. Sensitivity to insulin in adipocytes is significant to adipocyte lipid vacuole expansion, as well as adipocyte lipid vacuole reduction [40]. Adipocyte lipid vacuole reduction is caused by lipolysis, the breakdown of triglycerides into adipocytes, resulting in decreased adipocyte lipid volume. Conversely, adipocyte expansion results in an increase in adipocyte lipid volume via triglyceride uptake [40]. In insulin-resistant adipocytes, lipolysis is suppressed by insulin [40]. However, the suppressive effects of insulin are negligible in insulin-resistant adipocytes resulting in the accumulation of lipids in skeletal muscle—which may induce lipotoxic effects such as muscle atrophy (Fig. 4) [40]. “The cell biology of fat expansion” by Rutkowki et al. contains a thorough explanation of the mechanistic pathways that may be affected due to insulin insensitivity that results in the deposition of lipids in non-adipose tissues such as skeletal muscle [40]. Furthermore, the work of Fluck et al. and Arrighi et al. suggests that the increase in triglyceride content within skeletal muscle observed after rotator cuff tears may be attributed to metabolic alterations in insulin-resistant adipocytes derived from FAP cells.
Overview of insulin-sensitive adipocyte impact on lipotoxicity. (A) Non-lipotoxic conditions: Adipocytes that are insulin sensitive typically undergo normal lipolysis or breakdown of triglycerides into free fatty acids (FFA), resulting in normal lipid distribution in skeletal muscle. (B) Lipotoxic conditions: Adipocytes that are insulin resistant may undergo irregular lipolysis that increases the FFA levels in muscle environment. This may result in the accumulation of lipid in skeletal muscle that results in muscle atrophy
Muscle atrophy associated with rotator cuff tears correlates with lipid accumulation within skeletal muscle, but the exact mechanism that links the two phenomena in the setting of rotator cuff tears has not yet been elucidated. However, previous research on mechanisms of lipid buildup in animal models of myopathic illness may provide insight for future investigation. For example, Tamilarasan et al. demonstrated that upregulating lipoprotein lipase (LPL), the enzyme implicated in the uptake of lipids into skeletal muscle, resulted in lipid accumulation, muscle atrophy, and impaired muscle regeneration—all of which are associated with rotator cuff tear injuries—in a transgenic mouse model [41]. This suggests that changes in the expression of LPL in skeletal muscle may contribute to the atrophic effects seen in skeletal muscle myopathies like rotator cuff tear injuries. However, to validate the effect of LPL upregulation in the setting of rotator cuff tears, the LPL levels should be further evaluated in in vivo models of rotator cuff tears.
Potential Therapeutic Strategies Targeting FAPs
Approaches targeting fibroadipogenic progenitor cells (FAPs) have shown promising results in pre-clinical animal studies. In a specific mouse model investigating rotator cuff tear injury, Davies et al. reported a significant reduction in FAP cell numbers following the inhibition of the TGF-β1 pathway using the small molecule inhibitor SB431542 [36]. This was associated with marked decreases in both fat expansion and fibrotic tissue formation, conditions commonly associated with FAP activity in rotator cuff injuries [36]. Furthermore, LY2090314, an intracellular transducer that plays a pivotal role in the regulation of adipogenesis, demonstrated a significant capacity to attenuate FAP-induced adipogenesis through the inhibition of glycogen synthase kinase 3 (GSK) [42]. This was empirically validated within a three-dimensional model meticulously crafted to emulate the intramuscular adipose tissue accumulations observed in vivo [42]. These results substantiate the promising therapeutic potential of such interventions, aiming to ameliorate the detrimental impacts attributed to FAP activity in the context of rotator cuff pathologies.
In another study, Liu et al. explored the epigenetic influences on FAPs, finding a substantial upregulation of histone deacetylase (HDAC) in FAPs post-rotator cuff tendon transection in mice [43]. Notably, administration of the HDAC inhibitor Trichostatin A led to a decrease in fat expansion and promoted the differentiation of FAPs into brown adipocytes, a cell type known to play a vital role in muscle regeneration following rotator cuff injuries [43].
Complementing these findings, other research initiatives have employed pharmacological agents to target FAPs after rotator cuff injuries [44]. Lio et al. demonstrated that administering parathyroid hormone (PTH) induced the formation of FAP-derived beige adipocytes and increased the expression of genes associated with adipose tissue browning [44]. This PTH-induced transformation of FAPs was shown to reduce fat expansion and mitigate muscle atrophy in a rat model of rotator cuff tear injury. Additionally, the administration of imatinib, an inhibitor of the platelet-derived growth factor, resulted in diminished fat expansion following tendon resection [35].
Collectively, these studies underscore the potential of therapeutic strategies aimed at modulating FAP activity, offering a promising avenue for the treatment of rotator cuff injuries and associated complications.
Exploring the Potential of FAPs in Stem Cell Therapies and Tissue Engineering for Rotator Cuff Injuries
Fibroadipogenic progenitor cells (FAPs) have emerged as a promising candidate in the realm of regenerative medicine for addressing rotator cuff tear injuries. In a noteworthy study conducted by Lee et al., beige FAP cells sourced from mice were investigated within the context of a murine model simulating a substantial rotator cuff tear injury [45, 46]. The study demonstrated the compelling capacity of these beige FAPs to ameliorate pathological hallmarks associated with this injury, notably attenuating fat expansion and mitigating fibrotic tissue formation [45, 46].
To holistically evaluate the efficacy of these interventions, in the same study, a comprehensive gait analysis was employed [45, 46]. Parameters encompassing stride length, stride duration, and stance were meticulously assessed. Notably, the application of beige FAP implantation resulted in improved gait analysis outcomes, signifying an enhancement in shoulder performance [45, 46]. These findings underscore the substantive potential of FAPs as a viable asset in the armamentarium of stem cell-based therapeutic strategies and tissue engineering approaches for the treatment of rotator cuff injuries. Therefore, continued exploration of the therapeutic modalities offered by FAPs presents a promising avenue for advancing regenerative engineering efforts for develop therapeutics approaches for rotator cuff injuries. Furthermore, the LY2090314, a transducer found to control adipogenesis, was demonstrated to reduce FAP adipogenesis by inhibiting glycogen synthase kinase 3 (GSK) in a 3-D model mimicking intramuscular fat deposits.
Future Directions in FAP Research
In recent years, there has been a burgeoning interest in unraveling the intricate regulatory pathways that govern the behavior of fibroadipogenic progenitor cells (FAPs). The primary objective of these scientific endeavors is to modulate these pathways with precision, with the end goal of enhancing muscle regeneration and attenuating the accrual of fibrotic and adipose tissues subsequent to rotator cuff injuries.
At present, it is unequivocally established that key pathways, notably the Wnt and TNF-alpha pathways, play a vital role in maintaining the homeostasis of FAP cells and directing their differentiation after muscle injury [31]. The introduction of sophisticated technologies, such as RNA sequencing, has enabled an in-depth, gene-level analysis, casting light on the nuanced alterations taking place within these pathways.
The application of RNA sequencing allows for the meticulous dissection of the genetic changes associated with the expansion of adipose tissue and the formation of fibrotic structures within the muscle. This profound insight not only deepens our understanding of the molecular events ensuing muscle injury but also forges new paths for the development of gene-based therapeutic interventions. Concentrating on the specific genetic aberrations linked to undesirable tissue changes facilitates the evaluation of the effectiveness of targeted therapeutic strategies, edging us closer to the establishment of more robust treatment options.
Recent scholarly work in this field has revealed distinct patterns of differential gene expression in instances of rotator cuff tears. A notable study by Tashjian et al. discerned a marked downregulation of the THSD7A gene in instances of rotator cuff tears in comparison to control groups, highlighting the potential functional significance of this gene in such pathological conditions [47]. These pivotal findings accentuate that genetic alterations are indeed a response to rotator cuff injuries. Pertaining to FAPs, such insights are invaluable for elucidating the impact of these genetic shifts on FAP cell differentiation and proliferation. Armed with this knowledge, there is potential to leverage gene therapy approaches to correct these alterations, fostering tissue repair and regeneration.
The exploration of gene modifications through gene therapy stands as a promising frontier for regenerative engineering approaches to treating rotator cuff tear injuries.
This transition towards a more personalized and precise medical paradigm constitutes a monumental stride forward, signaling the dawn of a new era in the clinical management of rotator cuff injuries.
Rotator Cuff Regenerative Engineering
High retear rates in patients following surgical repair of the rotator cuff have been mentioned previously [48]. To address this challenge, regenerative engineering has focused on utilizing cell therapy and biomaterial-based approaches [49]. Biomaterial-based approaches have been extensively investigated in preclinical studies [49]. These biomaterials, whether natural or synthetic, offer the potential to enhance the innate healing capacity of soft tissues and provide mechanical stability [49,50,51]. Consequently, various biomaterials and fabrication techniques have been employed to develop repair matrices for the treatment of the pathological phenomena associated with rotator cuff tears. In the following sections, we will briefly discuss the biomaterials and fabrication processes used in rotator cuff regenerative engineering.
Synthetic Biomaterials
Synthetic polymers are particularly appealing as materials for rotator cuff regenerative engineering because of their ability to be tailored in terms of elastic moduli, tensile strengths, and degradation rates [52]. Synthetic biomaterials are listed in Table 1. The synthetic polymers polycaprolactone (PCL), polyglycolic acid (PGA), poly(lactide-co-glycolide) (PLGA), and polylactic acid (PLA) are frequently used to fabricate matrices for rotator cuff tear treatment due to their biocompatibility—defined as the ability of a material to function in a specific application with a favorable host reaction—and biodegradability [52,53,54]. Using PCL nanofibers as a base, Tang et al. created an electroconductive nanofibrous matrix for rotator cuff regeneration by plating poly(3,4ethylenedioxythiophene):poly(styrene sulfonate) (PEDOT:PSS) nanoparticles onto the nanofibers [54]. Histological evidence proved that the nanofibrous matrix reduced muscle atrophy in a rat RCT model [54]. Using synthetic polymers, other structures appropriate for rotator cuff regeneration have been developed [55].
Limitations of Synthetic Biomaterials
Synthetic materials have proven to be feasible for rotator cuff regeneration applications; however, this class of materials has some limitations. For example, synthetic materials are biologically inert and may release acidic degradation products [56, 57]. Cell attachment, which is the ability of cells to attach to a scaffolding structure, may be limited by the use of synthetic materials [58]. Further, in severe cases of rotator cuff tears, nerve damage may be associated [59]. Regeneration of nerve tissue with synthetic materials may not be effective. For instance, in vivo silicon-based nerve conduits have been described to be limited by its inability to degrade naturally [60]. In addition, silicon-based nerve conduits have shown to induce immunogenic reactions [61]. Therefore, the use of synthetic materials may limit the healing response to damage associated with RCTs.
Natural Biomaterials
Due to their inherent biocompatibility and biodegradability, natural polymers represent a significant class of biomaterials in rotator cuff regeneration [50]. Natural polymers are listed in Table 1. Materials under the umbrella of natural materials exhibit low toxicity—the degree to which a substance can harm organisms—and a minor chronic inflammatory response [62]. Collagen, frequently employed in rotator cuff regeneration, has several advantageous qualities, including encouraging cell adhesion, proliferation, and consequently tissue regeneration [63]. Another natural polymer utilized to rejuvenate RCTs, particularly tendons, is chitosan [64]. Chitosan is a biocompatible and biodegradable substance that can encourage cellular migration and proliferation [65]. However, natural polymers are limited by their mechanical properties. When compared to native tendons, natural polymers, such as collagen and fibrin, have reduced tensile strength and elasticity, which may limit the ability of the regenerated tissue to endure the mechanical demands of the shoulder joint [66]. Furthermore, depending on the source and processing techniques, the mechanical properties of natural polymers may vary, making it challenging to obtain consistent and optimum performance [67, 68].
Graphene Applications in Regenerative Engineering: Addressing Muscle Atrophy and Fatty Expansion in Rotator Cuff Injuries
Graphene has recently attracted significant attention in regenerative engineering applications due to its exceptional mechanical, electrical, and thermal properties [69]. One of the most promising applications of graphene is in the development of engineered matrices for the treatment of muscle atrophy and fat accumulation. Graphene-based materials have shown promising results in enhancing muscle regeneration by promoting cell growth and differentiation, leading to the formation of new muscle tissue and repairing damaged muscle fibers [69].
Fatty expansion of the rotator cuff involves changes in lipid metabolism, inflammation, and oxidative stress [48]. Several studies have investigated the potential of graphenic materials in treating fatty degeneration in muscle. Graphene oxide (GO), a graphene derivative, has proven to reduce lipid accumulation in muscle tissue. Furthermore, GO treatment has been found to reduce inflammation in muscle tissue. Inflammation is a factor associated with fatty expansion in muscle, and the reduction in inflammation is associated with decreased lipid accumulation.
Graphene-based nanocomposites have also shown promise in reducing fatty expansion in muscle [70]. A study conducted on mice showed that a graphene-based nanocomposite could reduce lipid accumulation in muscle tissue by up to 60%. The study also found that the graphene-based nanocomposite could increase muscle strength and function, indicating that it may be a potential material utilized in the treatment of myopathies such as rotator cuff tears [71]. A recent report utilized a graphene electrospun nanofibrous matrix in a rat model of chronic massive rotator cuff tears [72]. The study’s results showed that using the graphene matrix promoted muscle regeneration and decreased fatty expansion in muscle tissue [72]. The treated group showed a significant increase in muscle fiber size and muscle strength compared to the control group [72]. The graphene matrix was found to improve muscle function by promoting angiogenesis, which is the formation of new blood vessels and reducing fibrosis, which is the formation of scar tissue [72]. The study also found that the graphene matrix had no adverse effects on the rats and was well-tolerated [72]. This suggests using a graphene matrix could be a safe and effective approach for treating chronic massive rotator cuff tears [72].
Electrospinning Applications for RCTs
Since the work of Laurencin et al. in 2002, tissue regeneration applications have utilized electrospinning as a fabrication method for polymer-based matrices [73]. The outflow of polymeric solution from the nozzle initiates the electrospinning process [3]. The polymer solution is dispensed from the nozzle tip, where electrostatic, mechanical, and gravitational forces combine to form a droplet [3]. A polymer stream emerges when the droplet’s surface tension is insufficient to dissipate the electrostatic charge [3]. The production of nanofibers and lengthening of the erupting stream are caused by solvent evaporation as it moves toward a collection platform.
Regenerative engineering approaches to treating RCTs have utilized electrospinning to produce nanofibrous matrices. Due to nanofiber’s biomimetic capabilities combined with their inherent nano-related characteristics, such as their high surface-to-volume ratio, adjustability, and flexibility, electrospun nanofibers have been used in the treatment rotator cuff tear-related symptoms such as muscle atrophy and fat expansion [52, 66]. The Laurencin group utilized the electrospinning platform to synthesize an electroconductive nanofibrous matrix using (PEDOT: PSS) nanoparticles coated on PCL nanofibers and demonstrated its ability to reduce muscle atrophy [74]. Huang et al. developed a nanofibrous matrix composed of electrospun polyurethane and lithium containing mesoporous silicon nanoparticles that reduced fat accumulation in a rotator cuff injury model [55].
Advancements in 3D Printing for Rotator Cuff Tear Rehabilitation: Tailoring Tissue Engineering and Regenerative Strategies
3D printing technology has emerged as a transformative tool in the field of tissue engineering, offering novel solutions for the rehabilitation of rotator cuff tears (RCTs). By enabling the precise fabrication of synthetic tissues with customizable mechanical characteristics and complex structural compositions, this technology facilitates the creation of regulated microenvironments that are conducive to rotator cuff regeneration.
Utilization of Heterogeneous Materials
The capability of 3D printers to handle a variety of biomaterials allows for the production of objects with heterogeneous structures, meeting the intricate demands of rotator cuff regeneration, given that the anatomical structure encompasses ligament, bone, and muscle, each with distinct properties and functions [75]. The integration of diverse materials within a single print job enables the development of interfaces with varying properties, potentially improving the integration of the engineered tissue with the native rotator cuff environment.
Application of PLGA in 3D Printed Structures for RCT Repair
Polylactic-co-glycolic acid (PLGA), a well-established synthetic biomaterial, has demonstrated its viability in 3D printing applications pertinent to RCT rehabilitation. Chen et al. successfully utilized 3D-printed PLGA scaffolds as a matrix to house mesenchymal stem cells, which were genetically modified to overexpress bone morphogenic protein-12 (BMP-12) [53]. This innovative approach aimed to expedite the healing process at the critical bone-tendon interface, showing the potential of 3D printing in enhancing the efficacy of cellular therapies for RCT repair.
In a similar vein, Jiang et al. created a 3D-printed scaffold using PLGA, integrating it with cell-laden collagen-fibrin hydrogels [75]. Their comprehensive assessment of the scaffold’s biocompatibility, conducted both in vitro and in vivo, has established a robust foundation for future research, confirming the feasibility of 3D-printed PLGA structures in the context of rotator cuff repair.
Addressing RCT-Related Symptoms
While these advancements highlight the potential of 3D printing in RCT rehabilitation, the specific impact of these technologies on RCT-related symptoms such as fat expansion and muscle atrophy requires further investigation. Preliminary evidence suggests that healing at the bone-tendon interface can alleviate pathological changes associated with RCTs [76]. This provides a preliminary basis for exploring 3D-printed structures as a viable fabrication method for scaffolds in RCT repair, although comprehensive evaluations are needed to substantiate these findings and optimize the technology for clinical application.
In conclusion, the integration of 3D printing in the domain of RCT rehabilitation signifies a significant step forward, offering innovative solutions and paving the way for personalized and effective treatment strategies. Continued research and development in this area are imperative to fully unlock the potential of 3D printing in transforming RCT treatment and improving patient outcomes.
Future Directions
As previously discussed, fibroadipogenic progenitor cells (FAPs) possess the potential to differentiate into either fibrotic or adipogenic cell types. Gaining a comprehensive understanding of these differentiation pathways opens avenues for the modulation of FAPs, with the goal of mitigating fat accumulation and potentially preventing lipotoxic-muscle atrophy in cases of torn rotator cuff. Insulin-resistant white adipocytes, for instance, are implicated in fat accumulation, and novel strategies such as photo biomodulation laser therapy have shown promise in ameliorating these effects in high-fat diet–induced scenarios[77].
Beyond non-pharmaceutical interventions, pharmaceutical avenues, particularly those explored within the realm of diabetes mellitus research, also present potential for influencing insulin signaling and, consequently, FAP behavior [78]. Furthermore, the strategic integration of regenerative engineering principles, employing scaffolds and mechanically stimulating exercises, has demonstrated efficacy in aligning myotubes, reducing fat accumulation, and enhancing collagen production by stem cells [72, 79].
With a view toward skeletal muscle regeneration, constructs incorporating PLGA and stem cells have emerged as significant players, underscored by the importance of the “secretome” in modulating the regenerative environment [80]. Herein lies the innovation of synthetic artificial stem cells (SASC), designed to emulate the secretome and guide tissue regeneration, presenting a versatile solution applicable to a spectrum of conditions including rotator cuff tears [81].
Concluding Remarks
In conclusion, this review underscores the necessity to transition our terminology from the traditional “fat infiltration” to the more accurate descriptor, “fat expansion,” when detailing the fatty alterations seen in rotator cuff tears. The phenomenon of fat accumulation in the context of rotator cuff tears is more accurately described as “fat expansion.” Our examination into the world of fibroadipogenic progenitor cells (FAPs) has revealed their critical role in these pathological outcomes, providing paradigm shifts that can recalibrate our therapeutic strategies. A significant revelation is the emerging correlation between insulin resistance in adipocytes, which are believed to originate from FAPs, and the muscle atrophy observed in patients suffering from RCTs. This insight not only widens our comprehension of the intricacies of RCT pathology but also offers potential avenues for treatment.
The integration of regenerative engineering treatment strategies holds promise for addressing the pathological alterations associated with rotator cuff tears. By harnessing the capabilities of stem cell science, biomimicry, biomaterials, and physical modulation, we stand on the cusp of a new era in therapeutic interventions for rotator cuff injuries. Furthermore, the groundbreaking progress in regenerative engineering, especially in the realm of rotator cuff tendon tears, has been spotlighted. This pioneering field promises not just to enhance our treatment modalities, but potentially transform them, by targeting and mitigating the pathological changes that have, for so long, plagued surgical outcomes. These advancements not only offer a pathway to improved patient outcomes but also lay the groundwork for future research endeavors aimed at refining and optimizing treatment modalities for rotator cuff tears and related musculoskeletal conditions.
Data Availability
No datasets were generated or analyzed for the writing of this manuscript.
References
Post M, Silver R, Singh M. Rotator cuff tear: diagnosis and treatment. Clin Orthop. 1983;173:78–91.
Freedman BR, Mooney DJ, Weber E. Advances toward transformative therapies for tendon diseases. Sci Translational Med. 2022;14:eabl8814. https://doi.org/10.1126/scitranslmed.abl8814.
Saveh-Shemshaki N, Nair LS, Laurencin CT. Nanofiber-based matrices for rotator cuff regenerative engineering. Acta Biomaterialia. 2019;94:64–81. https://doi.org/10.1016/j.actbio.2019.05.041.
Laron D, Samagh SP, Liu X, Kim HT, Feeley BT. Muscle degeneration in rotator cuff tears. J Shoulder Elbow Surg. 2012;21:164–74. https://doi.org/10.1016/j.jse.2011.09.027.
Lemos DR, Babaeijandaghi F, Low M, Chang C-K, Lee ST, Fiore D, et al. Nilotinib reduces muscle fibrosis in chronic muscle injury by promoting TNF-mediated apoptosis of fibro/adipogenic progenitors. Nat Med. 2015;21:786–94. https://doi.org/10.1038/nm.3869.
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty infiltration of disrupted rotator cuff muscles. Rev Rhum Engl Ed. 1995;62(6):415–22.
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;(304):78–83.
Longo UG, Mazzola A, Magrì F, Catapano S, De Salvatore S, Carotti S, et al. Histological, radiological and clinical analysis of the supraspinatus tendon and muscle in rotator cuff tears. BMC Musculoskelet Disord. 2023;24:127. https://doi.org/10.1186/s12891-023-06237-9.
Sevivas N, Serra SC, Portugal R, Teixeira FG, Carvalho MM, Silva N, et al. Animal model for chronic massive rotator cuff tear: behavioural and histologic analysis. Knee Surg Sports Traumatol Arthrosc. 2015;23:608–18. https://doi.org/10.1007/s00167-014-3441-3.
Kim HM, Galatz LM, Lim C, Havlioglu N, Thomopoulos S. The effect of tear size and nerve injury on rotator cuff muscle fatty degeneration in a rodent animal model. J Shoulder Elbow Surg.2012;21(7):847–58. https://doi.org/10.1016/j.jse.2011.05.004.
Meyer GA, Gibbons MC, Sato E, Lane JG, Ward SR, Engler AJ. Epimuscular fat in the human rotator cuff is a novel beige depot. Stem Cells Transl Med. 2015;4:764–74. https://doi.org/10.5966/sctm.2014-0287.
Agha O, Diaz A, Davies M, Kim HT, Liu X, Feeley BT. Rotator cuff tear degeneration and the role of fibro-adipogenic progenitors. Ann NY Acad Sci. 2021;1490:13–28. https://doi.org/10.1111/nyas.14437.
Singh A, Gibbons MC, Anakwenze OA, Cheng T, Azimi H, Schenk S, Ward SR. Histological quantification of chronic human rotator cuff muscle degeneration. J Shoulder Elbow Surg.2016;25(10): E336–7. https://doi.org/10.1016/j.jse.2016.07.070.
Arrighi N, Moratal C, Clément N, Giorgetti-Peraldi S, Peraldi P, Loubat A, et al. Characterization of adipocytes derived from fibro/adipogenic progenitors resident in human skeletal muscle. Cell Death Dis. 2015;6:e1733–e1733. https://doi.org/10.1038/cddis.2015.79.
Chavez JA, Summers SA. Lipid oversupply, selective insulin resistance, and lipotoxicity: molecular mechanisms. Biochim Biophys Acta. 2010;1801:252–65. https://doi.org/10.1016/j.bbalip.2009.09.015.
Vishvanath L, Gupta RK. Contribution of adipogenesis to healthy adipose tissue expansion in obesity. J Clin Invest. 2019;129:4022–31. https://doi.org/10.1172/JCI129191.
Wang Y, Shyh-Chang N. Sphingolipids mediate lipotoxicity in muscular dystrophies. Life Medicine. 2022;1:273–5. https://doi.org/10.1093/lifemedi/lnac015.
Laurencin CT, Khan Y, Regenerative engineering. Sci Transl Med. 2012;4:160ed9. https://doi.org/10.1126/scitranslmed.3004467.
Shemshaki NS, Kan HM, Barajaa M, Otsuka T, Lebaschi M, Mishra N, Nair LS, Laurencin CT. Muscle degeneration in chronic massive rotator cuff tears of the shoulder: addressing the real problem using a graphene matrix. Proc Natl Acad Sci. 2022;119(33):e2208106119. https://doi.org/10.1073/pnas.2208106119.
Monga I, Kaur K, Dhanda SK. Revisiting hematopoiesis: applications of the bulk and single-cell transcriptomics dissecting transcriptional heterogeneity in hematopoietic stem cells. Brief Funct Genomics. 2022;21(3):159–76. https://doi.org/10.1093/bfgp/elac002.
Boldt C. What is tumor-infiltrating lymphocyte (TIL) therapy? MD Anderson Cancer Center; Cancerwise. 2021(4). https://www.mdanderson.org/cancerwise/what-is-tumor-infiltrating-lymphocyte-til-therapy--6-things-to-know.h00-159460056.html.
Perrin J, Capitao M, Mougin-Degraef M, Guérard F, Faivre-Chauvet A, Rbah-Vidal L, Gaschet J, Guilloux Y, Kraeber-Bodere F, Cherel M, Barbet J. Cell tracking in cancer immunotherapy. Front Med (Lausanne). 2020;7:34. https://doi.org/10.3389/fmed.2020.00034.
Hartwell MJ, Harold RE, Sweeney PT, Seitz AL, Marra G, Saltzman MD. Imbalance in axial-plane rotator cuff fatty infiltration in posteriorly worn glenoids in primary glenohumeral osteoarthritis: An MRI-based Study. Clin Orthop Relat Res. 2021;479(11):2471–9. https://doi.org/10.1097/CORR.0000000000001798.
Werthel JD, Boux de Casson F, Walch G, Gaudin, P, Moroder, P, Sanchez-Sotelo, J, Chaoui, J, Burdin, V. Three-dimensional muscle loss assessment: a novel computed tomography-based quantitative method to evaluate rotator cuff muscle fatty infiltration. J Shoulder Elbow Surg. 2022;31(1):165–74. https://doi.org/10.1016/j.jse.2021.07.029.
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. https://doi.org/10.1016/S1058-2746(99)90097-6.
Xu J, Liu B, Qiao Y, Ye Z, Su W, Zhao J. The 3-dimensional fatty infiltration in the overall supraspinatus can be predicted by localized sectional accumulation units: a cross-sectional study in patients with atraumatic small-to-massive rotator cuff tears. JBJS. 2023;105:380. https://doi.org/10.2106/JBJS.22.00767.
Davis DL, Kesler T, Gilotra MN, Almardawi R, Hasan SA, Gullapalli RP, et al. Quantification of shoulder muscle intramuscular fatty infiltration on T1-weighted MR images: a viable alternative to the Goutallier classification system. Skeletal Radiol. 2019;48:535–41. https://doi.org/10.1007/s00256-018-3057-7.
Addison O, Marcus RL, Lastayo PC, Ryan AS. Intermuscular fat: a review of the consequences and causes. Int J Endocrinol. 2014;2014:309570. https://doi.org/10.1155/2014/309570.
Uezumi A, Fukada S, Yamamoto N, Takeda S, Tsuchida K. Mesenchymal progenitors distinct from satellite cells contribute to ectopic fat cell formation in skeletal muscle. Nat Cell Biol. 2010;12:143–52. https://doi.org/10.1038/ncb2014.
Joe AWB, Yi L, Natarajan A, Le Grand F, So L, Wang J, et al. Muscle injury activates resident fibro/adipogenic progenitors that facilitate myogenesis. Nat Cell Biol. 2010;12:153–63. https://doi.org/10.1038/ncb2015.
Contreras O, Rossi FMV, Theret M. Origins, potency, and heterogeneity of skeletal muscle fibro-adipogenic progenitors—time for new definitions. Skeletal Muscle. 2021;11:16. https://doi.org/10.1186/s13395-021-00265-6.
Hansen JB, Kristiansen K. Regulatory circuits controlling white versus brown adipocyte differentiation. Biochem J. 2006;398:153–68. https://doi.org/10.1042/BJ20060402.
Stumm J, Vallecillo-García P, Vom Hofe-Schneider S, Ollitrault D, Schrewe H, Economides AN, et al. Odd skipped-related 1 (Osr1) identifies muscle-interstitial fibro-adipogenic progenitors (FAPs) activated by acute injury. Stem Cell Research. 2018;32:8–16. https://doi.org/10.1016/j.scr.2018.08.010.
Liu X, Ning AY, Chang NC, Kim H, Nissenson R, Wang L, et al. Investigating the cellular origin of rotator cuff muscle fatty infiltration and fibrosis after injury. Muscles Ligaments Tendons J. 2016;6:6–15. https://doi.org/10.11138/mltj/2016.6.1.006.
Shirasawa H, Matsumura N, Shimoda M, Oki S, Yoda M, Tohmonda T, et al. Inhibition of PDGFR signaling prevents muscular fatty infiltration after rotator cuff tear in mice. Sci Rep. 2017;7:41552. https://doi.org/10.1038/srep41552.
Davies MR, Liu X, Lee L, Laron D, Ning AY, Kim HT, et al. TGF-β small molecule inhibitor SB431542 reduces rotator cuff muscle fibrosis and fatty infiltration by promoting fibro/adipogenic progenitor apoptosis. PLoS ONE. 2016;11:e0155486. https://doi.org/10.1371/journal.pone.0155486.
Lee C, Agha O, Liu M, Davies M, Bertoy L, Kim HT, et al. Rotator cuff fibro-adipogenic progenitors demonstrate highest concentration, proliferative capacity, and adipogenic potential across muscle groups. J Orthop Res. 2020;38:1113–21. https://doi.org/10.1002/jor.24550.
Han X. Lipidomics: developments and applications. J Chromatogr B Analyt Technol Biomed Life Sci. 2009;877:2663. https://doi.org/10.1016/j.jchromb.2009.07.007.
Flück M, Ruoss S, Möhl CB, Valdivieso P, Benn MC, von Rechenberg B, et al. Genomic and lipidomic actions of nandrolone on detached rotator cuff muscle in sheep. J Steroid Biochem Mol Biol. 2017;165:382–95. https://doi.org/10.1016/j.jsbmb.2016.08.005.
Rutkowski JM, Stern JH, Scherer PE. The cell biology of fat expansion. J Cell Biol.2015;208(5):501–12. https://doi.org/10.1083/jcb.201409063.
Tamilarasan KP, Temmel H, Das SK, Al Zoughbi W, Schauer S, Vesely PW, et al. Skeletal muscle damage and impaired regeneration due to LPL-mediated lipotoxicity. Cell Death Dis. 2012;3:e354–e354. https://doi.org/10.1038/cddis.2012.91.
Reggio A, De Paolis F, Bousselmi S, Cicciarelli F, Bernardini S, Rainer A, et al. A 3D adipogenesis platform to study the fate of fibro/adipogenic progenitors in muscular dystrophies. Dis Model Mech. 2023;16:dmm049915. https://doi.org/10.1242/dmm.049915.
Liu X, Liu M, Lee L, Davies M, Wang Z, Kim H, et al. Trichostatin A regulates fibro/adipogenic progenitor adipogenesis epigenetically and reduces rotator cuff muscle fatty infiltration. J Orthop Res. 2021;39:1452–62. https://doi.org/10.1002/jor.24865.
Iio R, Manaka T, Takada N, Orita K, Nakazawa K, Hirakawa Y, et al. Parathyroid hormone inhibits fatty infiltration and muscle atrophy after rotator cuff tear by browning of fibroadipogenic progenitors in a rodent model. Am J Sports Med. 2023;51:3251–60. https://doi.org/10.1177/03635465231190389.
Lee C, Liu M, Agha O, Kim HT, Liu X, Feeley BT. Beige fibro-adipogenic progenitor transplantation reduces muscle degeneration and improves function in a mouse model of delayed repair of rotator cuff tears. J Shoulder Elbow Surg. 2020;29:719–27. https://doi.org/10.1016/j.jse.2019.09.021.
Lee C, Liu M, Agha O, Kim HT, Feeley BT, Liu X. Beige FAP transplantation improves muscle quality and shoulder function after massive rotator cuff tears. J Orthop Res. 2020;38:1159–66. https://doi.org/10.1002/jor.24558.
Tashjian RZ, Kim SK, Roche MD, Jones KB, Teerlink CC. Genetic variants associated with rotator cuff tearing utilizing multiple population-based genetic resources. J Shoulder Elbow Surg. 2021;30:520–31. https://doi.org/10.1016/j.jse.2020.06.036.
Gladstone JN, Bishop JY, Lo IKY, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719–28. https://doi.org/10.1177/0363546506297539.
Washington KS, Shemshaki NS, Laurencin CT. The role of nanomaterials and biological agents on rotator cuff regeneration. Regen Eng Transl Med. 2021;7:440–9. https://doi.org/10.1007/s40883-020-00171-1.
Hee CK, Dines JS, Dines DM, Roden CM, Wisner-Lynch LA, Turner AS, et al. Augmentation of a rotator cuff suture repair using rhPDGF-BB and a type I bovine collagen matrix in an ovine model. Am J Sports Med. 2011;39:1630–40. https://doi.org/10.1177/0363546511404942.
Ratner BD. A pore way to heal and regenerate: 21st century thinking on biocompatibility. Regenerative Biomaterials. 2016;3:107–10. https://doi.org/10.1093/rb/rbw006.
Zhao S, Su W, Shah V, Hobson D, Yildirimer L, Yeung KWK, et al. Biomaterials based strategies for rotator cuff repair. Colloids Surf, B. 2017;157:407–16. https://doi.org/10.1016/j.colsurfb.2017.06.004.
Chen P, Cui L, Chen G, You T, Li W, Zuo J, et al. The application of BMP-12-overexpressing mesenchymal stem cells loaded 3D-printed PLGA scaffolds in rabbit rotator cuff repair. Int J Biol Macromol. 2019;138:79–88. https://doi.org/10.1016/j.ijbiomac.2019.07.041.
Tang X, Saveh Shemshaki N, Vernekar VN, Prabhath A, Kuyinu E, Kan H-M, et al. The treatment of muscle atrophy after rotator cuff tears using electroconductive nanofibrous matrices. Regen Eng Transl Med. 2021;7:1–9. https://doi.org/10.1007/s40883-020-00186-8.
Huang K, Su W, Zhang X, Chen C, Zhao S, Yan X, et al. Cowpea-like bi-lineage nanofiber mat for repairing chronic rotator cuff tear and inhibiting fatty infiltration. Chem Eng J. 2020;392:123671. https://doi.org/10.1016/j.cej.2019.123671.
Dai W, Kawazoe N, Lin X, Dong J, Chen G. The influence of structural design of PLGA/collagen hybrid scaffolds in cartilage tissue engineering. Biomaterials. 2010;31:2141–52. https://doi.org/10.1016/j.biomaterials.2009.11.070.
Laurencin C, Khan Y, El-Amin SF. Bone graft substitutes. Expert Rev Med Devices. 2006;3:49–57. https://doi.org/10.1586/17434440.3.1.49.
Yamaguchi M, Shinbo T, Kanamori T, Wang P, Niwa M, Kawakami H, et al. Surface modification of poly(l-lactic acid) affects initial cell attachment, cell morphology, and cell growth. J Artif Organs. 2004;7:187–93. https://doi.org/10.1007/s10047-004-0267-7.
Kim HM, Dahiya N, Teefey SA, Keener JD, Galatz LM, Yamaguchi K. Relationship of tear size and location to fatty degeneration of the rotator cuff. J Bone Joint Surg Am. 2010;92:829–39. https://doi.org/10.2106/JBJS.H.01746.
Arslantunali D, Dursun T, Yucel D, Hasirci N, Hasirci V. Peripheral nerve conduits: technology update. Med Devices (Auckl). 2014;7:405–24. https://doi.org/10.2147/MDER.S59124.
Wang Y, Zhang Y, Li X, Zhang Q. The progress of biomaterials in peripheral nerve repair and regeneration. J Neurorestoratol. 2020;8:252–69. https://doi.org/10.26599/JNR.2020.9040022.
Wang D, Zhang X, Huang S, Liu Y, Fu BS, Mak KK, et al. Engineering multi-tissue units for regenerative medicine: bone-tendon-muscle units of the rotator cuff. Biomaterials. 2021;272:120789. https://doi.org/10.1016/j.biomaterials.2021.120789.
Roßbach BP, Gülecyüz MF, Kempfert L, Pietschmann MF, Ullamann T, Ficklscherer A, et al. Rotator cuff repair with autologous tenocytes and biodegradable collagen scaffold: a histological and biomechanical study in sheep. Am J Sports Med. 2020;48:450–9. https://doi.org/10.1177/0363546519892580.
Willbold E, Wellmann M, Welke B, Angrisani N, Gniesmer S, Kampmann A, Hoffmann A, Cassan D, Menzel H, Hoheisel AL, Glasmacher B, Reifenrath J. Possibilities and limitations of electrospun chitosan‐coated polycaprolactone grafts for rotator cuff tear repair. J Tissue Eng Regen Med. 2020;14(1):186–97. https://doi.org/10.1002/term.2985.
Melamed E, Beutel BG, Robinson D. Enhancement of acute tendon repair using chitosan matrix. Am J Orthop (Belle Mead NJ). 2015;44(5):212–6.
Zheng Z, Ran J, Chen W, Hu Y, Zhu T, Chen X, et al. Alignment of collagen fiber in knitted silk scaffold for functional massive rotator cuff repair. Acta Biomater. 2017;51:317–29. https://doi.org/10.1016/j.actbio.2017.01.041.
Van Kampen C, Arnoczky S, Parks P, Hackett E, Ruehlman D, Turner A, et al. Tissue-engineered augmentation of a rotator cuff tendon using a reconstituted collagen scaffold: a histological evaluation in sheep. Muscles Ligaments Tendons J. 2013;3:229–35.
Derwin KA, Badylak SF, Steinmann SP, Iannotti JP. Extracellular matrix scaffold devices for rotator cuff repair. J Shoulder Elbow Surg. 2010;19:467–76. https://doi.org/10.1016/j.jse.2009.10.020.
Aleemardani M, Zare P, Seifalian A, Bagher Z, Seifalian AM. Graphene-based materials prove to be a promising candidate for nerve regeneration following peripheral nerve injury. Biomedicines. 2021;10:73. https://doi.org/10.3390/biomedicines10010073.
Shin SR, Li Y-C, Jang H, Khoshakhlagh P, Akbari M, Nasajpour A, et al. Graphene-based materials for tissue engineering. Adv Drug Deliv Rev. 2016;105:255–74. https://doi.org/10.1016/j.addr.2016.03.007.
Li J, Yang S, Yu J, Cui R, Liu R, Lei R, et al. Lipid- and gut microbiota-modulating effects of graphene oxide nanoparticles in high-fat diet-induced hyperlipidemic mice. RSC Adv. 2018;8:31366–71. https://doi.org/10.1039/C8RA06058D.
Saveh Shemshaki N, Kan H-M, Barajaa M, Otsuka T, Lebaschi A, Mishra N, et al. Muscle degeneration in chronic massive rotator cuff tears of the shoulder: addressing the real problem using a graphene matrix. Proc Natl Acad Sci U S A. 2022;119:e2208106119. https://doi.org/10.1073/pnas.2208106119.
Li W-J, Laurencin CT, Caterson EJ, Tuan RS, Ko FK. Electrospun nanofibrous structure: a novel scaffold for tissue engineering. J Biomed Mater Res. 2002;60:613–21. https://doi.org/10.1002/jbm.10167.
Tang X, Saveh-Shemshaki N, Kan H-M, Khan Y, Laurencin CT. Biomimetic electroconductive nanofibrous matrices for skeletal muscle regenerative engineering. Regen Eng Transl Med. 2020;6:228–37. https://doi.org/10.1007/s40883-019-00136-z.
Jiang X, Wu S, Kuss M, Kong Y, Shi W, Streubel PN, et al. 3D printing of multilayered scaffolds for rotator cuff tendon regeneration. Bioactive Materials. 2020;5:636–43. https://doi.org/10.1016/j.bioactmat.2020.04.017.
Huynh T, Kim JT, Dunlap G, Ahmadi S, Wolchok JC. In vivo testing of an injectable matrix gel for the treatment of shoulder cuff muscle fatty degeneration. J Shoulder Elbow Surg. 2020;29:e478–90. https://doi.org/10.1016/j.jse.2020.03.038.
Silva G, Ferraresi C, de Almeida RT, Motta ML, Paixão T, Ottone VO, et al. Infrared photobiomodulation (PBM) therapy improves glucose metabolism and intracellular insulin pathway in adipose tissue of high-fat fed mice. Lasers Med Sci. 2018;33:559–71. https://doi.org/10.1007/s10103-017-2408-2.
Li M, Chi X, Wang Y, Setrerrahmane S, Xie W, Xu H. Trends in insulin resistance: insights into mechanisms and therapeutic strategy. Sig Transduct Target Ther. 2022;7:1–25. https://doi.org/10.1038/s41392-022-01073-0.
Peng Y, Li X, Wu W, Ma H, Wang G, Jia S, Zheng C. Effect of mechanical stimulation combined with platelet-rich plasma on healing of the rotator cuff in a murine model. Am J Sports Med. 2022;50(5):1358–68. https://doi.org/10.1177/03635465211073339.
Kubo Y, Hoffmann B, Goltz K, Schnakenberg U, Jahr H, Merkel R, et al. Different frequency of cyclic tensile strain relates to anabolic/catabolic conditions consistent with immunohistochemical staining intensity in tenocytes. Int J Mol Sci. 2020;21:1082. https://doi.org/10.3390/ijms21031082.
Shah S, Esdaille CJ, Bhattacharjee M, Kan H-M, Laurencin CT. The synthetic artificial stem cell (SASC): shifting the paradigm of cell therapy in regenerative engineering. Proc Natl Acad Sci. 2022;119:e2116865118. https://doi.org/10.1073/pnas.2116865118.
Han S, Sun J, He S, Tang M, Chai R. The application of graphene-based biomaterials in biomedicine. Am J Transl Res. 2019;11:3246–60.
Wu SY, An SS, Hulme J. Current applications of graphene oxide in nanomedicine. Int J Nanomedicine. 2015;10(Spec Iss):9–24. https://doi.org/10.2147/IJN.S88285.
Acknowledgements
We would like to thank our funding agency: NIH Building Infrastructure Leading to Diversity (BUILD) UTEP/NIH /2TL4GM118971. Original images were created using BioRender.
Funding
NIH Building Infrastructure Leading to Diversity (BUILD) UTEP/NIH /2TL4GM118971.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Significance
Muscle atrophy and fat accumulation complicate current therapeutic approaches to treating rotator cuff tears. Understanding and acknowledging the true pathological contributors to rotator cuff tears is critical for developing regenerative engineering treatment strategies for rotator cuff tears.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merriman Jr, M.A., Chapman, J.H., Whitfield, T. et al. Fat Expansion Not Fat Infiltration of Muscle Post Rotator Cuff Tendon Tears of the Shoulder: Regenerative Engineering Implications. Regen. Eng. Transl. Med. (2023). https://doi.org/10.1007/s40883-023-00324-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40883-023-00324-y