Abstract
Purpose
There is currently no diagnostic test specific to Parkinson’s disease, which means that a positive diagnosis, assessments of severity, and evaluations of treatment efficacy rely heavily on evaluation scales. But obtaining scale data is time-consuming and limited in time and place. Gait is the core target in evaluation scales. Because of the inertia instrument has widely been used in healthcare institutes for gait assessment. Since the inertial device is as well embedded in every smartphone. Our objective was to explore the feasibility of using the ubiquitous smartphone to assist in the assessment of gait.
Methods
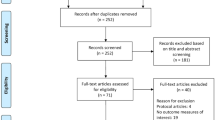
Twenty subjects were recruited in the clinical trial, which included a general gait analysis and detecting freezing of gait episodes. The gait analysis results obtained using the smartphone were compared with those obtained using an off-the-shelf inertia instrument, and the detecting freezing of gait episodes were compared with the evaluations of clinical professionals.
Results
The degree of consistency between the gait analysis results obtained using the smartphone and those obtained using the inertia instrument are ICC = 0.835, r = 0.858, and ρ = 0.846. In the detecting freezing of gait episodes, in comparing the detections by the clinical evaluators and the smartphone, the sensitivity is 90.6 ± 7.71% and specificity is 94.3 ± 8.36%.
Conclusion
The overall analyses revealed high degree of consistency between the two analysis schemes. The convenience of the ubiquitous smartphone has a great potential to enhance the frequency of gait assessment, thereby providing more data by which to assess treatment efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Parkinson’s disease (PD) was identified in 1817 by the British physician James Parkinson. PD is a progressive neurological disease involving a gradual deterioration of the substantia nigra cells in the basal ganglia of the brain. The various regions of the brain transmit signals among each other to coordinate the multiple brain functions involved in integrating thoughts, movements, emotions, and feelings. For example, in moving one’s body, the basal ganglia sends a message to the thalamus, which is then transmitted to the cerebral cortex and other regions of the brain. The transmission of these messages relies on the neurotransmitter dopamine, which is secreted by the substantia nigra cells. In cases of PD, the deterioration of these cells limits the availability of dopamine for the transmission of nerve signals. Note that the secretion of the neurotransmitter acetylcholine is mediated by dopamine levels. Thus, a decrease in the concentration of dopamine can lead to excessive acetylcholine levels, causing limb tremors and/or muscle rigidity [1].
At present, PD cannot be completely cured; with the result that treatment focuses entirely on the use of drugs or surgical interventions to ease symptoms. Most PD patients suffer from movement disorders, such as bradykinesia, stiffness, tremors, loss of balance, and loss of postural reflexes [2]. PD patients are also susceptible to disruptions in non-motor systems, resulting in micrographia, speech disorders, and/or dysphagia. Furthermore, PD has been linked to mental disorders, sleep disorders, autonomic nerve abnormalities, paresthesia, and gastrointestinal discomfort [3]. Aging, genetic factors and exposure to pesticides or industrial waste have also been shown to accelerate PD-related deterioration [4].
In today’s aging society, PD and dementia are the most common chronic neurodegenerative diseases. PD morbidity is approximately 0.1–0.2%; however, the onset of PD increases sharply with age, especially after 60 years old. The number of PD onset events per 100,000 people per year ranges from 17.4 (50–59 years) to 93.1 (70–79 years). The prevalence of PD among those over the age of 60 is approximately 1.5% [5, 6], and it has been estimated that 15% of the population over the age of 65 is affected. Note that the onset of PD can occur even before the age of 40. Currently, there are roughly 500,000 cases of PD in Europe and one million cases in the United States, with an annual growth rate of 50,000–60,000. The average life expectancy from diagnosis to death is 15 years, and mortality is more than double that in the general population [7]. As a progressive disease, PD gradually degrades one’s quality of life, because patients lose the ability to look after themselves or speak with others. By the time they reach the final stage of the disease, most PD patients are unable to eat due to dysphagia, which can result in severe weakness and concurrent aspiration pneumonia. PD brings with it a long period of pain and suffering for patients as well as their families.
At present, there are no diagnostic tests (e.g., blood, urine, imaging, or physiological signals) specifically for PD. In the initial stages, PD is diagnosed via clinical examination. Typical symptoms include bradykinesia, akinesia, resting tremors, and rigidity [8]. Postural abnormality is another common symptom, which tends to appear in later stages. Note, however, that many PD patients are asymptomatic; i.e., they do not exhibit tremors. A clinical diagnosis of PD is evidence of at least two of the above-mentioned symptoms. Subsequent confirmation is based on the effectiveness of PD drug therapy. A variety of scales have been developed for the rating of PD symptoms. Some scales are used in research for the evaluation of treatment efficacy, whereas others are used clinically to assess disease progression and severity [9]. The Hoehn-Yahr scale and Unified Parkinson’s Disease Rating Scale (UPDRS) are used most commonly today. The Hoehn-Yahr scale is used to stage the course of PD [10], and the UPDRS is used to evaluate treatment efficacy [11]. In the initial stages (the first 10–15 years), PD patients are treated with drugs to relieve symptoms. The most common drug is levodopa, which is meant to supplement dopamine loss [4]. However, the efficacy of drugs diminishes over time, such that surgical interventions, such as deep brain stimulation (DBS) and brain lesioning, would be considered.
Dyskinesia is the main symptom of PD, and gait is the most representative item. Gait assessment can be used to screen patients with suspected PD and can also be used to monitor disease progression and evaluate the treatment efficacy. Thus, gait is the main evaluation topic on the UPDRS and the Hoehn-Yahr scale. Deep brain stimulation surgery is expensive and high-risk, and until recently, there has been no effective method by which to predict the prognosis. Recent studies however, have revealed that gait assessment can be used to predict DBS prognosis [12]. Nonetheless, gait assessment must be performed by trained clinical professionals, which is time-consuming, and is limited in time and place. As a result, the insufficient assessment is the general situation.
Microelectromechanical inertia instrument has widely been used in healthcare institutes for gait assessment [13,14,15]. Because of the inertial device is as well embedded in every smartphone. Our objective in the current study was to explore the feasibility of using a smartphone to assist in the assessment of gait in cases of PD. The ubiquity of smartphones should make it possible to perform regular gait assessments to keep track of disease progression and the efficacy of treatment.
2 Methods
PD gait assessment can be divided into general gait analysis and detecting freezing of gait (FoG) episodes. This section outlines gait assessment methods, experimental tools, and clinical trials.
2.1 General Gait Analysis
Figure 1 outlines the flow of signal data processing for general gait analysis using the inertial device embedded in smartphones to measure vertical acceleration along the sagittal plane during walking. Imported raw acceleration data first undergo signal pre-processing, which involves filtering out environmental noise and deleting signals corresponding to the start and end of the walking segment. Filtering is also performed to remove interference due to acceleration under the effects of gravity. Signal smoothing is then used to facilitate the detection of peaks. The Gaussian Continuous Wavelet Transform (GCWT) is applied to the signal, such that the valley of the resulting waveform corresponds to the time point of the initial contact (IC) of the foot (i.e., the point at which the heel strikes the ground). The GCWT is then applied again, the peak of the resulting waveform corresponding to the time point of the final contact (FC) of the foot (i.e., the point at which the toes leave the ground). Spatio-temporal integration is then used to determine the spatial positions corresponding to the time points of IC and FC [14, 15].
Once the IC and FC have been identified, it is possible to analyze gait features, including pace, rhythm, variability, asymmetry, and postural control. Gait pace includes step velocity mean, step length mean, and swing time variability. Gait rhythm includes step time mean, swing time mean, and stance time mean. Gait variability includes step velocity variability, step length variability, step time variability, and stance time variability. Gait asymmetry includes swing time asymmetry, step time asymmetry, and stance time asymmetry. Postural control includes step length asymmetry, step width mean, and step width variability. The structure of general gait analysis is shown in Fig. 2.
For a compass gait type, the center of mass (CoM) movements in the sagittal plane follow a circular trajectory during each single support phase. Then in the inverted pendulum model, the variations in height of CoM depend on step length [16]. Thus, the step length could be derived using the elevation (and variation in elevation) of the inertial device from the ground [17], as follows:
where l indicates the elevation of the inertial device above the ground (pendulum length) while the subject is standing still, and h indicates the variability in elevation while the subject is walking. The h is calculated by a double integration of vertical acceleration. To prevent integration drift, data were high-pass filtered in advance.
The step velocity is derived using step length and step time, as follows:
The degree of variability of the right and left foot data are derived from the variance of the right foot and left foot, as follows:
where Variabilityleft and right refers to the variation of the left foot and right foot, Varianceleft refers the variance of the left foot, and Varianceright refers to the variance of right foot.
Variability in gait features is derived from the standard deviation (SD) in data pertaining to walking, for example,
Symmetry between the left foot and right foot is derived from the averages of the left foot and right foot, for example,
where Asymmetryleft and right refers to the absolute difference between the averages of the left foot Averageleft and the right foot Averageright.
Figure 3 presents a schematic illustration showing the derivation of gait analysis results, where the blue wave indicates raw walking data; the green wave is derived from the initial GCWT (following data integration and smoothing) with the valley corresponding to the IC time point; and the red wave is derived from the second GCWT with the peak corresponding to the FC time point. The IC and FC time points of the left foot and right foot are differentiated by the sign of angular velocity along the vertical axis after filtering.
2.2 FoG Detection
When PD patients stand or walk normally, the power spectrum of vertical acceleration along the sagittal plane is distributed mainly in the loco band (0.5–3 Hz). FoG episodes produce a significant spectral component referred to as the freeze band (3–8 Hz) [15, 18]. A FoG episode can be detected using a 256-point Hamming sliding window for the filtering of vertical acceleration data with a data shift of 40 points per slide movement. Data captured from each window data undergo processing via fast Fourier transform (FFT) to calculate the power spectral density (PSD). Trapezoidal integration is then performed respectively on the freeze band and the loco band. The sum of the integration results of the two frequency bands are referred to as the energy index (EI) [15], and the integration of the freeze band divided by the integration of the loco band is referred to as the freezing index (FI). Freezing threshold FIth and energy threshold EIth are used to determine the occurrence of FoG episodes. FIth and EIth vary from person to person and must therefore be obtained via practical testing. Step cadence (SC) is determined from the second harmonic in the spectrum. Human gait is a periodic phenomenon, and the number of steps per unit time is the second harmonic in the walking spectrum [19]. The process of FoG episode detection is illustrated in Fig. 4.
The following criteria are used to detect FoG episodes:
where \(\wedge\) is the AND logical operator. When FI(i) and EI(i) of the ith data window both exceed the critical values FIth and EIth, then Criterion 1 is true. When the SC of three consecutive window frames (i − 2, i − 1, i) are not equal, Criterion 2 is true. A progressive increase in the SC of three consecutive window frames (i − 2, i − 1, i) indicates an increase in the walking steps, such that Criterion 3 is true. The FoG episode begins at
where \(\vee\) is the OR logical operator. The FoG episode ends at
The PSD of a FoG episode is shown in Fig. 5, the PSD of normal walking is shown in Fig. 6, the PSD of standing still is shown in Fig. 7, and the accumulation of the aforementioned three PSDs is shown in Fig. 8. Most of the energy of FoG episodes and normal walking is distributed in the range of 0–40 Hz. Standing still implies little or no movement; therefore, most of the PSD can be attributed to noise with most of the energy distributed below 0.5 Hz. Note also that the total energy involved in standing still is significantly lower than that of FoG episodes and normal walking. The cumulative PSD can be used to distinguish instances of standing still, where FIth and EIth are the average values plus the standard deviation estimated for a subject standing still for 20 s.
2.3 Experimental Tools
This study requires a smartphone that is small, light, and computationally powerful. The following experiments were performed using a Sony™ Xperia XZ F8331 (146 × 72 × 8.1 mm; 161 g) with a powerful quad-core processor (2 × 2.15 GHz Kryo and 2 × 1.6 GHz Kryo), the Qualcomm MSM8996 Snapdragon 820 chipset, an Adreno 530 graphics processor, and 3 GB RAM/ 32 GB ROM. The operating system was Android 8.0 (Oreo). Note that this smartphone also features a solid aluminum back and frame shell with a wear-resistant Corning Gorilla Glass 4 screen. The embedded inertial device is the Bosch BMI160 MEMs chip, comprising a 16-bit three-axis accelerometer and three-axis gyroscope. The sensing range of the accelerometer is ± 2 g, ± 4 g, ± 8 g, and ± 16 g. The sensing range of the gyroscope is ± 125°/s, ± 250°/s, ± 500°/s, ± 1000°/s, and ± 2000°/s.
The gait analysis results obtained using the smartphone were compared with those obtained using an XsensTM MTw Awinda, which is widely applied in clinical experiments. FoG detection results were evaluated by clinical professionals, who sought to identify FoG episodes by examining video segments from the same analysis sessions.
2.4 Clinical Trials
The sample size of this trial (n = 20) was in line with the recommendations of the Lee Silverman Voice Treatment [20, 21]. In this study, type-I error α was set to 0.05, statistical power was set to 80%, and the withdrawal rate was estimated at 20%.
The criteria for the inclusion of subjects were as follows:
-
1
Over 20 years old (legal age),
-
2
Typical PD patient,
-
3
In 2‒4 PD Hoehn-Yahr stages,
-
4
Ability to walk independently (i.e., without assistance from others),
-
5
No comorbidity of mental or intellectual impairment (i.e., ability to understand instructions during the trial).
The criteria for the exclusion of subjects were as follows:
-
1
Atypical PD patient,
-
2
Impaired intelligence, confusion, depression, and/or loss of motivation,
-
3
Acute illness or disease of the central or peripheral nervous system, which could potentially affect walking,
-
4
Orthopedic or internal medical problems potentially affecting walking,
-
5
Vulnerable groups, such as prisoners, indigenous people, pregnant women, or mental patients.
Throughout the experiment, an elastic band was used to fix both the MTw Awinda and the smartphone adjacent to the center of the body mass, which is behind the navel against the second lumbar spine (L2). Participants performed a timed up and go test (TUG), which involved walking in a straight line and then turning back. Note that from the perspective of signal processing, this routine would produce large fluctuations in velocity at the starting and ending points. Thus, we extended the walking distance (normally 3 m) to 5 m, with the aim of ensuring stable velocity for a sufficient duration, as shown in Fig. 9. During the FoG episode detection test, FoG episodes were induced by placing additional obstacles on the walking pathway.
3 Results
The clinical trial was approved by the Clinical Trial Center, National Taiwan University Hospital, and all subjects provided written informed consent. As shown in Table 1, the demographic background information of the subjects included age, gender, duration of suffering from PD, duration of FoG occurrence, Hoehn-Yahr stage, evaluation of the UPDRS part III, evaluation of the New Freezing of Gait Questionnaire (N-FOGQ), and evaluation of Mini-Mental State Examination (MMSE).
The gait analysis items used to compare the performance of the proposed smartphone and the MTw Awinda were as follows: step count, step time, stride time, stance time, swing time, step length, and step velocity. The measured number of steps obtained using the smartphone was 100% consistent with the results from the MTw Awinda. After verifying the normal distribution of results from the Shapiro–Wilk test, the experiment data were analyzed in terms of level of agreement (LoA): mean, standard deviation, intraclass correlation coefficient (ICC), correlation coefficient analysis (r), Spearman correlation coefficient analysis (ρ), and ± 95% confidence interval analysis, as shown in Table 2.
Independent t-test tests and analysis of variance (ANOVA) were used to analyze the between-group differences. The relatively small number of subjects limited the effects of data reorganization; therefore, Bonferroni correction was not performed [22]. In accordance with the recommendations of Hartmann and Portney [23, 24], the degree of consistency was defined in terms of ICC, r, or ρ, as follows: excellent (> 0.900), good (0.750‒0.899), medium (0.500‒0.749), and inconsistent (< 0.500). The results in Table 2 illustrate the high degree of consistency between the gait analysis result obtained using the smartphone and those obtained using the MTw Awinda. The averages of ICC, r, and ρ are 0.835, 0.858, and 0.846, respectively. Figure 10 compares the time-series of step counts obtained using the MTw Awinda and the smartphone.
The detection of FoG episodes depends on two types of movement disorders: akinetic and tremoric. Note that at least one FoG episode was identified during the test session of each subject, and a total of 39 FoG episodes (#FoG) were identified among all subjects. Note also that three evaluators with clinical experience participated in the analysis, and their results presented high inter-rater agreement. There was a clear consensus with regard to the time points corresponding to the start and end of the FoG episodes (ICC > 0.82). The smartphone detected only 35 #FoG (89.7%). The detection sensitivity and specificity of the clinical evaluators and smartphone were respectively derived as follows:
where Phone FRs indicates the #FoG detected by the smartphone, Clinic FRs indicates the #FoG identified by clinical evaluators, and NFRs refer to non-FoG periods. The analysis results are detailed in Table 3. We also compared the measurements obtained by the evaluators and the smartphone. The average times were as follows: evaluators (6.50 ± 2.36 s.) and smartphone (6.20 ± 2.40 s.). The consistency between the two data sets was as follows: ICC = 0.972, r = 0.971, and ρ = 0.947. Overall, the above analysis revealed outstanding consistency between the two analysis schemes.
4 Discussion
The primary differences between the smartphone and the MTw Awinda are the sampling rate and tasking mode of the kernel processor. It is possible to set the sampling rate of the inertial device embedded in a smartphone to match that of the MTw Awinda; however, the MTw Awinda operates in single tasking mode, while the smartphone operates in multitasking mode. This allows the MTw Awinda to maintain a constant sampling rate and frequency resolution while calculating the gait spectrum. The system resources of smartphones are controlled by the Android operating system, in which background programs share resources and priority is given to programs that are responsible for core tasks, such as the real-time clock and phone standby. Thus, smartphones cannot ensure that sampling of the embedded inertial device proceeds at a constant rate. These fluctuations can have a direct effect on the spectral resolution, which is crucial to determining the occurrence of FoG episodes. This problem could be alleviated by using a more powerful processor or reducing the number of programs running in the background. In this study, we initially assessed the Sony™ Xperia and Samsung™ Galaxy smartphones, both of which feature quad-core processors. We then discovered that the Galaxy tends to have a larger number of proprietary apps running in the background and sharing more system resources; therefore, we opted for the Sony device in the above experiments. Gait detection performance could also be improved by reducing the computational load on the smartphone. In the above experiments, we sought to optimize measurement performance by restoring the phone to its factory settings, deleting all pre-installed apps, and closing all built-in apps, such as GPS and synchronizer. The resulting measurement results did not differ significantly from those obtained from the MTw Awinda; however, it is unlikely that the same benchmarks could be achieved using a typically configured smartphone.
It should also be noted that the clinical evaluators would be able to use their extensive experience in interpreting the body language of subjects, such as facial expressions and body movements. In contrast, smartphones depend entirely on objective variations in gait, while disregarding FoG episodes of short duration and underestimating the duration of FoG episodes. As a result, clinical evaluators tend to be more sensitive than is smartphone.
The results of this experiment revealed that most of the situations involving FoG episodes occurred during changes in routine (e.g., walking initiation, turning, approaching the ending point, or passing through the midway obstacles), which is in line with general clinical symptoms. We also found that the symptoms (akinetic, tremoric), FoG forms (trembling, shuffling, akinetic), Hoehn and Yahr stages, or gender did not diverge from the measurements obtained using the smartphone or the MTw Awinda.
Finally, it should be noted that our focus in this study was on engineering issues. The role of gait assessment in clinical diagnosis has not been fully elucidated. The means by which gait analysis (e.g., FoG detection and its duration) contribute to clinical diagnosis and the degree of accuracy required for this analysis will have to be examined in the future.
The system developed in this study could greatly enhance the convenience and frequency of PD gait assessment, thereby providing more data by which to assess treatment efficacy.
Change history
11 September 2020
Following the publication of the article by Tang et al. [1], inappropriate and missing citations were discovered. To make the article more comprehensive and complete, the authors propose to publish a correction. And the authors would like to apologize for any inconvenience caused to the readers by these changes in the paper. The corresponding corrections are shown below:
References
Latash, M. L. (2008). Postural control and locomotion in Parkinson’s disease. Neurophysiological basis of movement (pp. 325–326). Illinois: Champaign.
Lees, A. J., Hardy, J., & Revesz, T. (2009). Parkinson’s disease. Lancet, 373(9680), 2055–2066. https://doi.org/10.1016/S0140-6736(09)60492-X.
Chaudhuri, K. R., & Schapira, A. H. (2009). Non-motor symptoms of Parkinson’s disease: Dopaminergic pathophysiology and treatment. Lancet Neurology, 8(5), 464–474. https://doi.org/10.1016/S1474-4422(09)70068-7.
Environmental Factors and Parkinson’s. National Parkinson Foundation. Retrieved from https://www.parkinson.org/understanding-parkinsons/what-is-parkinsons/Environmental-Factors-and-Parkinsons
Bower, J. H., Maraganore, D. M., McDonnell, S. D. K., & Rocca, W. A. (1999). Incidence and distribution of parkinsonism in Olmsted County, Minnesota, 1976–1990. Neurology, 52(6), 1214–1220.
de Rijk, M. C., Breteler, M. M., Graveland, G. A., Ott, A., Grobbee, D. E., van der Meché, F. G., et al. (1995). Prevalence of Parkinson’s disease in the elderly: the Rotterdam Study. Neurology, 45(12), 2143–2146.
Katzenschlager, R., Head, J., Schraq, A., Ben-Shlomo, Y., Evans, A., & Lees, A. J. (2008). Fourteen-year final report of the randomized PDRG-UK trial comparing three initial treatments in PD. Neurology, 71(7), 474–480.
Jankovic, J. (2008). Parkinson’s disease: Clinical features and diagnosis. Journal of Neurology, Neurosurgery and Psychiatry, 79(4), 368–376. https://doi.org/10.1136/jnnp.2007.131045.
Professional Training. National Parkinson Foundation. Retrieved from https://www.parkinson.org/Professionals/Professional-Resources/Screening-Instruments
Goetz, C. G., Poewe, W., Rascol, O., Sampaio, C., Stebbins, G. T., Counsell, C., et al. (2004). Movement disorder society task force report on the Hoehn and Yahr staging scale: Status and recommendations. Movement Disorders, 19(9), 1020–1028.
Goetz, C. G., Tilley, B. C., Shaftman, S. R., Stebbins, G. T., Fahn, S., Martinez-Martin, P., et al. (2008). Movement disorder society-sponsored revision of the unified Parkinson’s disease rating scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Movement Disorders, 23(15), 2129–2170.
Lilleeng, B., Gjerstad, M., Baardsen, R., Dalen, I., & Larsen, J. P. (2015). Motor symptoms after deep brain stimulation of the subthalamic nucleus. Acta Neurologica Scandinavica, 131(5), 298–304. https://doi.org/10.1111/ane.12342.
Del Din, S., Godfrey, A., & Rochester, L. (2015). Validation of an accelerometer to quantify a comprehensive battery of gait characteristics in healthy older adults and Parkinson’s disease: Toward clinical and at home use. IEEE Journal of Biomedical and Health Informatics, 20(3), 838–847. https://doi.org/10.1109/JBHI.2015.2419317.
Godfrey, A., Lara, J., Munro, C. A., Wiuff, C., Chowdhury, S. A., Del Din, S., et al. (2015). Instrumented assessment of test battery for physical capability using an accelerometer: A feasibility study. Physiological Measurement, 36(5), N71–83.
Moore, S. T., MacDougall, H. G., & Ondo, W. G. (2008). Ambulatory monitoring of freezing of gait in Parkinson’s disease. Journal of Neuroscience Methods, 167(2), 340–348.
Zijlstra, W., & Hof, A. (1997). Displacement of the pelvis during human walking: Experimental data and model predictions. Gait & Posture, 6(3), 249–262. https://doi.org/10.1016/s0966-6362(97)00021-0.
Zijlstra, W., & Hof, A. L. (2003). Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait & Posture, 18(2), 1–10. https://doi.org/10.1016/s0966-6362(02)00190-x.
Auvinet, B., Berrut, G., Touzard, C., Moutel, L., Collet, N., Chaleil, D., et al. (2002). Reference data for normal subjects obtained with an accelerometric device. Gait Posture, 16(2), 124–134.
Moore, S. T., Yungher, D. A., Morris, T. R., Dilda, V., MacDougall, H. G., Shine, J. M., et al. (2013). Autonomous identification of freezing of gait in Parkinson’s disease from lower-body segmental accelerometry. Journal of NeuroEngineering and Rehabilitation, 10, 19. https://doi.org/10.1186/1743-0003-10-19.
Ramig, L. O., Countryman, S., O’Brien, C., Hoehn, M., & Thompson, L. (1996). Intensive speech treatment for patients with Parkinson’s disease: Short-and long-term comparison of two techniques. Neurology, 47(6), 1496–1504.
Ramig, L. O., Countryman, S., Thompson, L. L., & Horii, Y. (1995). Comparison of two forms of intensive speech treatment for Parkinson disease. Journal of Speech and Hearing Research, 38(6), 1232–1251.
Armstrong, R. A. (2014). When to use the Bonferroni correction. Ophthalmic and Physiological Optics, 34(5), 502–508. https://doi.org/10.1111/opo.12131.
Hartmann, A., Luzi, S., Murer, K., de Bie, R. A., & de Bruin, E. D. (2009). Concurrent validity of a trunk tri-axial accelerometer system for gait analysis in older adults. Gait & Posture, 29(3), 444–448. https://doi.org/10.1016/j.gaitpost.2008.11.003.
Portney, L. G., & Watkins, M. P. (2015). Foundations of clinical research: Applications to practice. Pennsylvania: F.A. Davis Company.
Acknowledgements
This study was supported by the Ministry of Science and Technology, Taiwan, under Grant MOST 107-2221-E-130-005.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang, ST., Tai, CH., Yang, CY. et al. Feasibility of Smartphone-Based Gait Assessment for Parkinson’s Disease. J. Med. Biol. Eng. 40, 582–591 (2020). https://doi.org/10.1007/s40846-020-00551-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-020-00551-6