Abstract
For the development of fall prevention programs, the dynamic postural control of elderly persons under conditions when their senses are perturbed needs to be investigated. The present study investigates the manner in which elderly persons respond to external perturbations when their visual and somatic senses are disturbed. The subjects included 4 healthy older adults and 6 young adults. In the experiment, external perturbation was introduced through a platform that was movable in four directions (forward, backward, right, and left). The effects of sensory disturbance created by wearing translucent goggles and standing on a soft floor were examined. The responses were measured in terms of the center of pressure (COP) on the force plate, the electromyographic (EMG) activity, and the joint angle from video analysis. The COP analysis showed that the older group, especially in the presence of sensory disturbances, required a longer time than that for the younger group to return to an erect standing position after external perturbations (recovery time). The EMG indicated that the older group used the articular muscles of the knee to respond to postural perturbations involving up-and-down movements. The recovery time is a characteristic parameter of the response to external perturbations in the presence of sensory disturbances, and thus a potentially useful indicator in evaluating balance ability. The increases in knee muscle’ activities were due to reduced ankle joint torque, which is presumably one of the causes of the prolonged recovery time. These findings could be applied to the development of fall prevention training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Falling can cause serious physical and psychological injury to older people, requiring a long recovery period. Because falling is often caused by unexpected external perturbations [1], the dynamic postural control ability of older people should be evaluated. Analysis of dynamic postural control commonly uses floor translational or tilting perturbations [2]. Dynamic postural control is closely associated with motion and sensation, and therefore the influence of the sensory system needs to be considered.
Several previous studies have reported postural control analyses in the presence of altered sensory conditions. Horak et al. reported that healthy younger people show no significant increase in postural sway when the conditions of their visual and somatic sensations are perturbed [3]. Meyer et al. reported that interruption of a single sensory input does not lead to a significant increase in postural sway [4]. Younger people have been shown to be capable of using sensory- reweighting as a reliable sensory source for postural control. In contrast, older people have been reported to show a delay in sensory- reweighting in comparison to that of younger people in the presence of an altered visual input [5]. Deterioration in sensory- reweighting, along with a decline in sensory function, leads to postural instability.
Thus, sensation perturbations can be used to effectively analyze the influence of the sensory system on the postural control of older people. However, there are few reports about postural control of older people exposed to external floor perturbations in the presence of sensory disturbances. The present study thus investigates the postural control mechanism of older people in response to external perturbations with their visual and somatic sensations perturbed to find characteristic parameters. The results will clarify the involvement of sensation and motion in postural control in older people, and help the development of fall prevention approaches.
2 Materials and Methods
2.1 Subjects
The subjects were 4 healthy older adults (all male; age: 69.5 ± 4.5 years; height: 162.0 ± 8.5 cm; weight: 57.5 ± 3.5 kg) and 6 young adults (4 men and 2 women; age: 21.8 ± 1.6 years; height: 167.3 ± 9.3 cm; weight 60.2 ± 5.8 kg). The subjects had no neurological disorders or orthopedic history in their lower limbs. Subjects were given a carefully written explanation of the experimental purpose, method, and privacy protection in advance of the experiment. They submitted their written informed consent to participate in this study. This study was approved by the Ethical Committee of The University of Tokyo.
2.2 Stimulus Parameters
Using an electrically operated platform, a dynamic translation perturbation was applied in four directions: forward, backward, right, and left. Each perturbation stimulus had a 1.9-s duration and a 0.18-m displacement.
2.3 Procedure
The subjects were asked to stand on the platform with their arms crossed to maintain an upright posture with the feet approximately shoulder-width apart. After the subjects were allowed to practice the procedure several times, perturbations were applied at random intervals between 5 and 10 s after the start of the measurement session to prevent anticipatory control. Data obtained when the perturbation caused a step or steps of the lower limbs were excluded. In such cases, the trial was started over. A physical therapist stood laterally near the subject and was prepared to support the subject if necessary to ensure each subject’s safety.
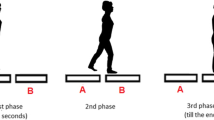
To elicit sensory disturbance, translucent goggles which blurred the field of view of the subjects (goggles condition) and a soft mat (AIREX, Air ex AG, Switzerland) (mat condition) were used. Perturbation was applied under the following four conditions: normal condition (open eyes, no mat); mat condition (open eyes, standing on the mat); goggles condition (wearing goggles, no mat), mat + goggles condition (wearing goggles and standing on the mat) (Fig. 1). Normal goggles with lenses covered by translucent film were used. The thickness of the mat was 58 mm and the hardness corresponded to rubber C7 in Japanese Industrial Standards K7312.
2.4 Data Collection
Center of pressure (COP), electromyographyc (EMG) activity, and joint angle data were obtained using previously described techniques [6]. Figure 2 shows the experimental set up of this study. To analyze the movement of the COP, a force plate (Kyowa Electronic Instruments Ltd., Tokyo, Japan) was placed onto the platform. The sampling rate was 1,000 Hz (converted to 100 Hz for analysis). A utility telemeter (NEC Corp., Tokyo, Japan) was used to measure EMG activity at a sampling frequency of 1,000 Hz to evaluate muscle activity under an unstrained condition. For EMG measurements, the target muscles were the right tibialis anterior muscle, the right medial head of the gastrocnemius muscle, the right rectus femoris (RRF) muscle, the right biceps femoris (RBF) muscle, both sides of the gluteus medius muscle, both sides of the rectus abdominis muscle, and both sides of the spinal erector. The EMG signals were normalized by the EMG magnitude in the isometric contraction at the maximum muscle power. This value was determined in advance using resistance applied by the examiner. Particular attention was given to the fixation, except for the target areas, using Bohannon’s method, so that the greatest muscle power was elicited [7]. For three-dimensional motion analysis, a motion measurement system (Frame-DIAS: DKH Ltd., JPN) was used. The sampling frequency of each camera was set at 120 Hz. At the measurement points, 14-mm-diameter infrared reflective markers were placed. The measurement points were the acromion, lower ends of the sternum, the anterior and posterior superior iliac spine, the greater trochanter, knee joint center, the lateral malleolus, the heel, and the fifth metatarsal head. The platform speed was confirmed using an accelerometer and the Frame-DIAS (Fig. 2). The platform, utility telemeter, and motion measurement system were synchronized and operated simultaneously.
2.5 Data Analysis
COP parameters under perturbation were calculated, and the total COP path length and COP latency (time from perturbation to start of COP motion) were analyzed. In addition, COP parameters were qualitatively analyzed. For EMG data analysis, biological information analysis software (Bimutas II, Kissei Comtec Co. Ltd., Tokyo, Japan) was used. After high-pass filtering (20 Hz) and full-wave rectification smoothing (simple moving average of 201 points to 1,000-Hz sampling), signals were normalized by the peak amplitude in the isometric contraction of maximum power. The muscle latency time was defined as the period between two time points: T1 and T2, where T1 is the time when the perturbation was applied, and T2 is the time when muscle activity started. T1 and T2 were identified as the times when the marker on the platform started to move and when the EMG amplitude exceeded 3 standard deviations of its baseline, respectively [8]. The amount of muscle activity was evaluated using the time-integrated value of muscle discharge in the perturbation. For three-dimensional angle changes calculation, Frame-DIAS was used. The angle changes of the trunk, hip, knee, and ankle joint in the sagittal and frontal planes were analyzed. The definitions of joint angles are given in the Appendix. The angle produced by the first and second vector was calculated for each part. The mean value of all subjects was calculated by quantifying the angle change as the difference between the angle in the upright position before perturbation and the angle in the upright position under a steady state after perturbation had ceased.
2.6 Statistical Analysis
The differences in each parameter of COP, angle change, and muscle activity between two groups were compared using the t test. A p value of < 0.05 was considered statistically significant. All statistical analyses were conducted using SPSS20.0 software (SPSS, Tokyo, Japan).
3 Results
3.1 Cop
No significant age-dependent difference was found in total COP path length in the four directions or four conditions. Similarly, no significant age- or condition-dependent difference was found in COP latency in the four directions or four conditions, indicating that older people respond to external perturbations without delay. Figures 3a–d show the time from the end of the external perturbation to COP reversal (recovery time). Older people required a significantly longer time for the following conditions: (1) mat and (2) goggles conditions while moving forward; (1) mat, (2) goggles and (3) mat + goggles conditions while moving backward; (1) goggles and (2) mat + goggles conditions in right translation; and (1) normal, (2) mat, (3) goggles, and (4) mat + goggles conditions in left translation.
3.2 Muscle Activity
No significant age-dependent difference was found in muscle latency in the four directions or with the four conditions. The measurement results of the amount of muscle activity are shown in Figs. 4a–d under normal conditions and Figs. 5a–d with the mat + goggles condition. No significant age-dependent difference was found under normal conditions. However, for the mat + goggles condition, older people showed significantly more activity of the RRF and RBF during backward translation, and higher activity of the RRF and RBF in right and left translations, but the difference in the level of the activities between the older and the younger groups was not significant. Older people did show significantly less activity of the right gastrocnemius RGA in right and left translations.
Muscle activities under mat + goggles condition for a forward, b backward, c right, and d left translations. R TA right anterior tibialis, R GA right gastrocnemius, R RF right rectus femoris, R BF right biceps femoris, R/L GM right/left gluteus medius, R/L A right/left rectus abdominis, R/L ES right/left spine erector
3.3 Angle Change
Table 1 shows the angular changes. The average changes in the ankle and knee joints under the mat and mat + goggles conditions were larger than those under the normal condition with forward and backward translation. No differences in sensory conditions were observed for average angle change in right or left translation. Under the normal condition, younger people showed a significantly greater change in trunk angle than did older people in forward, backward and right translations. No significant difference was found in other parts of the body.
4 Discussion
The COP analysis shows that under sensory disturbance, the older group had more difficulty in stopping body sway in comparison to the younger group. As the agonist muscles used to stop the sway are ankle muscles, those muscles must work properly. According to a previous report, older people have difficulty with eccentric contraction of limb muscles [9]. In eccentric contraction, the muscles contract while the muscle length is simultaneously extended. This contraction requires a very high level of control as compared to concentric contraction. In addition, older people have difficulty relaxing the antagonist muscle because of decreased reciprocal inhibition [10]. A combination of these factors can hinder smooth eccentric contraction. Maki et al. examined the activity of the tibialis anterior and the gastrocnemius of older people in the presence of translational external perturbations, reporting a strong tendency toward simultaneous contraction [11]. Maki et al. reported that when deprived of visual information, older people simultaneously contract the agonistic and antagonistic muscles to stiffen their bodies [12]. Thus, older people have difficulty coordinating muscle contractions. In the presence of sensory disturbances, they tend to increase the degree of simultaneous contraction. The diminished coordination of muscles resulting from the above factors makes it difficult for older people to respond to external perturbations. They thus require substantial time to stop their body sway. The time required for older people to stop their body sway can serve as an index of their adaptability to sensory disturbances.
The muscle activity analysis shows that older people tended to strongly activate the muscles of the femoral region as compared to younger people. According to several reports, the postural control of older people on a hard floor depends on hip strategy [13, 14]. Horak et al. reported that older people largely depend on hip strategies because their use of ankle strategies is limited to a very small range [15]. The authors presume that older people experience reduced ankle joint torque. In our experiment, older people may have possibly used the simultaneous contraction of the knee muscles for postural control in order to compensate for the reduced ankle joint torque. This can be presumed to be caused by increased vertical perturbation while using a mat. Thus, our study shows that in addition to the muscles of the ankle and hip joints, older people strongly activate the articular muscles of the knee in responding to postural perturbation involving up-and-down movements.
5 Conclusion
This study examined the dynamic postural control ability of older people exposed to external floor perturbations to find characteristic parameters when visual and somatic sensations are perturbed. Four conditions were set for sensory disturbances by combining visual sensory disturbance (wearing semi-transparent goggles) and plantar sensory disturbance (standing on a soft mat). The COP displacement was measured with a force plate, muscle latency and activity of the trunk and lower extremity muscles were measured with EMG, and angular changes of the trunk and lower extremity joints were measured using a video device. COP analysis shows that older people required a longer time than that of younger people to return to an erect standing position after the end of external perturbations (recovery time) in the presence of sensory disturbances. This recovery time is a characteristic parameter in the response to external perturbations in the presence of sensory disturbances, and is thus a potentially useful indicator for evaluating balance training with external perturbations. Muscle activity analysis found that older people used the articular muscles of the knee to respond to postural perturbations involving up-and-down movements, presumably as compensatory action due to reduced ankle joint torque. These findings indicate the influence of sensory disturbance on the postural control of older people and would be very useful for the development of fall prevention approaches.
References
Shapiro, A., & Melzer, I. (2010). Balance perturbation system to improve balance compensatory responses during walking in old persons. Journal of NeuroEngineering and Rehabilitation, 7, 32.
Maeda, Y., Tanaka, T., Nakajima, Y., & Shimizu, K. (2011). Analysis of postural adjustment responses to perturbation stimulus by surface tilts in the feet-together position. Journal of Medical and Biological Engineering, 31, 301–305.
Horak, F. B., Nashner, L. M., & Diener, H. C. (1990). Postural strategies associated with somatosensory and vestibular loss. Experimental Brain Research, 82, 167–177.
Meyer, P. F., Oddsson, L. E., & De Luca, C. J. (2004). The role of plantar cutaneous sensation in unperturbed stance. Experimental Brain Research, 156, 505–512.
Jeka, J. J., Allison, L. K., & Kiemel, T. (2010). The dynamics of visual reweighting in healthy and fall-prone older adults. Journal of Motor Behavior, 42, 197–208.
Y. Maeda, T. Toshiaki, Y. Nakajima, T. Miyasaka, T. Izumi and N. Kato (2100). Dynamic postural adjustments in stance in response to translational perturbation in the presence of visual and somatosensory disturbance. Journal of Medical and Biological Engineering (in press).
Bohannon, R. W. (1986). Test-retest reliability of hand-held dynamometry during a single session of strength assessment. Physical Therapy, 66, 206–209.
Fortiedr, P. A. (1994). Use of spike triggered of muscle activity to quantify inputs to motoneuron pools. Journal of Neurophysiology, 72, 248–265.
Enoka, R. M. (1996). Eccentric contractions require unique activation strategies by the nervous system. Journal of Applied Physiology, 81, 2339–2346.
Hortobágyi, T., Olmo, M. F., & Rothwell, J. C. (2006). Age reduces cortical reciprocal inhibition in humans. Experimental Brain Research, 171, 322–329.
Maki, B. E., & Ostrovski, G. (1993). Scaling of postural responses to transient and continuous perturbation. Gait Posture, 1, 93–104.
Maki, B. E., & Fernie, G. R. (1988). A system identification approach to balance testing. Progress in Brain Research, 76, 297–306.
Manchester, D., Woollacott, M., Zederbauer-Hylton, N., & Marin, O. (1989). Visual, vestibular and somatosensory contributions to balance control in the older adults. Journals of Gerontology, 44, M118–M127.
Gu, M. J., Schultz, A. B., Shepard, N. T., & Alexander, N. B. (1996). Postural control in young and elderly adults when stance is perturbed: dynamics. Journal of Biomechanics, 29, 319–329.
Horak, F. B., Shupert, C. L., & Mirka, A. (1989). Components of postural dyscontrol in the elderly: review. Neurobiology of Aging, 10, 727–738.
Acknowledgments
This study was supported by a Grant-in-Aid for Scientific Research of the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Appendix: Definition of Angle Change
Appendix: Definition of Angle Change
Body part | Direction of movement | First vector | Second vector | |
|---|---|---|---|---|
Sagittal plane | ||||
Ankle joint | Dorsiflexion, plantar flexion | Heel to fifth metatarsal head | Knee to lateral malleolus | |
Knee joint | Flexion, extension | Greater trochanter to knee | Knee to lateral malleolus | |
Hip joint | Flexion, extension | Anterior superior iliac spine to the greater trochanter | Greater trochanter to knee | |
Trunk | Flexion, extension | Acromion to anterior superior iliac spin | Anterior superior iliac spine to greater trochanter | |
Frontal plane | ||||
Ankle joint | Lateral bending | Heel to fifth metatarsal head | Knee to lateral malleolus | |
Hip joint | Lateral bending | Right knee to left knee | Right knee to right greater trochanter | |
Trunk | Lateral bending | Right greater trochanter to right acromion | Right acromion to left acromion | |
Rights and permissions
About this article
Cite this article
Maeda, Y., Tanaka, T., Nakajima, Y. et al. Age-related Changes in Dynamic Postural Control Ability in the Presence of Sensory Perturbation. J. Med. Biol. Eng. 35, 86–93 (2015). https://doi.org/10.1007/s40846-015-0009-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-015-0009-8