Abstract
Comorbidity and symptom overlap are common among psychiatric disorders of childhood. Consequently, differential diagnosis is often a challenge. This study addresses the diagnostic utility of the BASC-3 in differential diagnosis of autism spectrum disorders (ASD) versus ADHD using demographically similar samples of children who had undergone comprehensive diagnostic studies prior to the BASC-3 being administered. Results indicated that the BASC-3 Parent and Teacher rating scales, primarily the Atypicality, Withdrawal, Developmental Social Disorders, and Autism Probability Index scores, were both sensitive and accurate to ASD and differentiated this disorder with strong accuracy from ADHD and did so as well and in some instances better than longer assessments. The Hyperactivity and Attention Problems scales did not add to this differentiation, also pointing out the need for comprehensive assessment using omnibus scales such as BASC-3 in differential diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Comorbidity and symptom overlap are common among psychiatric disorders of childhood (Frick et al. 2020). Consequently, differential diagnosis is often a challenge, which in turn hinders accurate treatment planning and treatment efficacy. The high comorbidity rate among children affected by both ASD and ADHD serves as an exemplar of the challenges of differential diagnosis in child psychopathology (Rodriguez-Seijas et al. 2019).
Furthermore, recent research has demonstrated that the comorbidity of ADHD and ASD persists into adulthood (Solberg et al. 2019a, b). At the same time, however, this same research highlights the importance of differential diagnosis. For example, individuals with ADHD were found to be three times more likely than those with ASD to suffer a substance use disorder.
The presence of Intellectual Disability (ID) further complicates differential diagnosis of ADHD from ASD as this condition often co-occurs with both syndromes. In a sample of over 2000 children with ASD, over 18% also had ID (Levy et al. 2010; Tonnsen et al. 2016), and 3.5% of children and adolescents with ID also have ADHD, which is similar to the 3.9% in children and adolescents without ADHD (Platt et al. 2018).
The research literature cited documents the difficulties clinicians face when disentangling the diagnoses, symptom overlap, and symptom differentiation when evaluating children and adolescents referred for both ADHD and ASD symptomatology. Thus, the current study seeks to address this clinical challenge by determining whether or not widely used parent and teacher rating scales can aid this task. The specific aims of this investigation were to (a) determine whether or not the Parent and Teacher Rating Scales of the BASC-3 could be used to differentiate ADHD from ASD accurately and (b) identify the BASC-3 obtained scores that were most useful for making this clinical differentiation. The BASC-3 holds promise for making this diagnostic differentiation because of prior research indicating that this measure has functioned well to diagnose ASD in young children (Bradstreet et al. 2017) and ADHD in children and adolescents (Reynolds and Kamphaus 2015).
Methods
Subjects
The clinical sample in this study consists of 118 children diagnosed with autism spectrum disorders (ASD) and 118 children diagnosed with attention-deficit/hyperactivity disorder (ADHD). The children were evaluated for participation who met the specified inclusion criteria by trained recruiters and independent examiners from various schools and clinical settings (this process is described in detail in the BASC-3 professional Manual; Reynolds and Kamphaus 2015). For the ADHD as well as the ASD samples, information on IQ was not available. Information regarding subtypes of ADHD represented in the clinical sample was not available, and future studies may wish to address this shortcoming. The ADHD group has demographically similar characteristics as the ASD group with respect to the age, parents’ education level, gender, and ethnicity. Table 1 presents the demographic characteristics of the two groups. For parent education level (i.e., the highest school grade completed by the child’s mother), Level 1 indicates grade 11 or less, Level 2 for high school graduate, Level 3 for 1 to 3 years of college or technical school, and Level 4 for 4 years of college or more. For race/ethnicity, AA represents African American, HI for Hispanic, OT for Asian and Other, and WH for White.
Measure
Child (ages 6 through 11) and Adolescent (ages 12 through 21) forms of the Behavior Assessment System for Children-Third Edition (BASC-3) Parent Rating Scales (PRS) and Teacher Rating Scales (TRS) are used (Reynolds and Kamphaus 2015). The PRS and TRS each provide a comprehensive measure of a child’s adaptive and problem behaviors in community/home and school settings, respectively. Both forms contain descriptors of behaviors that informants rate on a four-point scale of frequency, ranging from Never to Almost Always (i.e., 0 = Never, 1 = Sometimes, 2 = Often, and 3 = Almost Always).
Psychological profiles with strong theoretical relationships to ASD symptomology on BASC-3 include the Developmental Social Disorders, Atypicality, and Withdrawal scales. The Developmental Social Disorders content scale provides a global indication of deficits in social skills, communication, interests, and activities, and an elevated score may indicate the presence of any symptoms reflective of ASD. The Atypicality clinical scale measures a child’s tendency to behave in ways that are considered odd and unusual. The Withdrawal clinical scale measures a child’s tendency to avoid contact and to lack interest in making contact in social settings as well as children who do not attach well to others. Previous BASC research has shown that Atypicality and Withdrawal scale scores are markedly elevated in children diagnosed with an ASD (Volker et al. 2009). The Autism Probability Index (AUI), a completely actuarially derived index, which is new to the BASC-3, was also selected for analysis. The AUI provides an indication of the similarity between the obtained behavioral ratings and the ratings of children identified as having an ASD.
The Attention Problems and Hyperactivity clinical scales were used to assess a subset of core ADHD symptoms. The Attention Problems scale measures an inability to maintain attention and the tendency to be easily distracted from tasks requiring attention. The Hyperactivity scale assesses the hyperactivity and impulsivity aspects of ADHD. ADHD Probability Index (ADI) provides an indication of the similarity between the obtained behavioral ratings and the ratings of children identified as having ADHD. Since the items included in this index are not limited to attention problems and hyperactivity, it is of interest to examine its power in discriminating ASD from ADHD groups.
Extensive psychometric properties of the selected scales are reported in the BASC-3 Manual (Reynolds and Kamphaus 2015). Most alpha coefficients are above .85 for all ages. Concurrent validity as indicated by the correlation between similar BASC-3 and Autism Spectrum Rating Scales (ASRS; Goldstein and Naglieri 2010) scales is reported as moderate to high.
Procedures
To compare ability of the selected BASC-3 profiles to the discriminate between the ASD and ADHD profiles, taking into account various model assumptions and theoretical framework, v logistic regression models were applied to examine the relationship between the scales selected and clinical diagnosis. Each model’s resulting area under the Receiver Operating Characteristics Curve (AUC) is reported. In addition, using the predicted probability .60 as the cut point, the predictive accuracy is obtained as indicated by the percentage of the correct prediction, the false-positive (FP) prediction errors, and the false-negative (FN) errors.
In addition, independent t tests and Cohen’s d effect size are calculated to validate the statistical and clinical significance of the score differences between the two groups. Since norms using ADHD groups are available in BASC-3, these tests are conducted using both general combined norms and clinical norms established using ADHD sample.
Results
Table 2 presents the logistic models’ results for the PRS and TRS. The sensitivity of the models including ASD scales is above .80. The prediction accuracy rate is around .72, and FP rate is low. On the other hand, the models including ADHD scales in diagnosis of ASD do not show discrimination with AUC being around .50, and high false-negative rate.
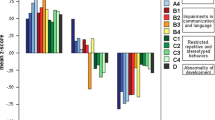
Tables 3 and 4 show consistent results using general combined and clinical norms. First, the ASD and ADHD groups show significant differences in all ASD-related scales with the effect sizes ranging from − 1.1 to − 1.5. A large number of t tests are reported in these tables; however, the majority of the differences seen on the key scales investigated were significant at the p < .01 level, and the effect sizes, reported in these same tables, are substantial and of even greater importance in diagnostic decision-making than traditional statistical significance testing. Second, the two groups demonstrate negligible variations in Attention Problems and Hyperactivity scales. Except for the PRS, the differences between the two groups are insignificant with small effect sizes (d = − .01 to − .02). This suggests ADHD indicators do not differentiate the ASD and ADHD groups well.
Conclusions
One way to help clinicians meet the challenges of differential diagnosis is to create improved assessment methods and procedures. Considerable attention, for example, was paid improving the item content, that is, content validity of the BASC-3 over the previous edition of the BASC (Reynolds and Kamphaus 2015). Items were added to assess more fully the complete range of symptoms associated with ASD, new empirically derived scales were created to provide the clinician with more options for making differential diagnoses of ASD, and existing BASC clinical scales were re-analyzed with new items to ensure greater homogeneity of construct assessment. This latter procedure resulted in increases in internal consistency coefficients for most scales. The current results, demonstrating considerably improved differential validity for ASD and ADHD syndromes, may be explained by using these construct assessment improvements in the revision process.
For now, the BASC-3 ASD-related diagnostic scales show considerable promise for two purposes, (1) diagnosis of ASD and (2) differential diagnosis of ADHD and ASD. Clinicians may have further confidence in these findings due to the fact that the same results were found for relatively large clinical and general normative samples. Both parent and teacher ratings’ of the behavioral profiles using the content and clinical scales of the BASC-3 have the potential for ASD-sensitive and ASD-specific screening. The Autism Probability Index is also highly sensitive to the presence of ASD but has somewhat less specificity. Compared to the far lengthier ADOS-2, while the differences are considered by us to be small, the BASC-3 performed overall at a higher level of accuracy with this clinical sample than has been reported in an updated study of the diagnostic accuracy of the ADOS-2 in a referred sample. In a large clinical sample of children and adolescents (N = 1080, age 1.7 to 20.5), updated actuarial diagnostic algorithms were derived in-sample to determine the “best” possible diagnostic algorithms associated with ASD for the ADOS-2. The revised, best algorithms resulted in values of sensitivity = .85 and specificity = .86 (Kamp-Becker et al. 2017). These algorithms were improved over the original ADOS-2 Manual algorithms but also the algorithms pertained especially to cases with core autism, and to girls. Kamp-Becker et al.’s results also suggested less effective diagnostic differentiation for children and adolescents with internalizing disorders and conduct disorder. The BASC-3 scales show superior sensitivity to the detection of ASD when it is present with only small sacrifices to specificity, or the detection of the absence of ASD in referral samples that are also fraught with children where ADHD is a key differentiator. The practical efficacy of the BASC-3 scales in terms of both clinician time and costs offer a clear alternative to lengthier assessments with no loss of diagnostic accuracy. Further research however is suggested to look at combining the results of BASC-3 with assessments such as the ADOS-2 in hopes that the combined assessment results can further improve the accuracy of what can be life changing diagnostic decisions for children and their families. The use of IQ as a moderator variable in differential diagnosis in referral samples also may be a fruitful area for future research on discriminating persons with ASD (or the detection of comorbidities of various forms) from persons with disorders that have overlapping symptoms. The interpretation of test scores and particularly the application of diagnostic labels must be considered in context of the referral base and base rates of various disorders, which can vary considerably by setting (i.e., see discussion by Reynolds (2016)).
References
Bradstreet, L. E., Juechter, J. I., Kamphaus, R. W., Kerns, C. M., & Robins, D. L. (2017). Using the BASC-2 parent rating scales to screen for autism spectrum disorder in toddlers and preschool-aged children. Journal of Abnormal Child Psychology., 45, 359–370. https://doi.org/10.1007/s10802-016-0167-3.
Frick, P. J., Burns, C., & Kamphaus, R. W. (2020). Clinical assessment of child and adolescent personality and behavior (4th ed.). New York: Springer.
Goldstein, S., & Naglieri, J. A. (2010). Autism Spectrum Rating Scales. Toronto: Multi- Health Systems Inc..
Kamp-Becker, I., Langmann, A., Stehr, T., Poustka, L., & Becker, K. (2017). Diagnostic accuracy of the ADOS-2 taking account of gender effects. ZKinder Jugendpsychiatry and Psychotherapy., 45(3), 193–207. https://doi.org/10.1024/1422-4917/a000492.
Levy, S. E., Giarelli, E., Lee, L., Schieve, L. A., Kirby, R. S., Cunniff, C., Nicholas, J., Reaven, J, & Rice, C. (2010). Autism Spectrum Disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. Journal of Developmental & Behavioral Pediatrics., 31, 267–275.
Platt, J. M., Keyes, K. M., McLaughlin, K. A., Kaufman, A. S. (2018). Intellectual disability and mental disorders in a US population representative sample of adolescents. Psychological Medicine., 49(6), 952–961.
Reynolds, C. R. (2016). Contextualized evidence and empirically based testing and assessment. Clinical Psychology: Science and Practice, 33(4), 410–416. https://doi.org/10.1111/cpsp.12181.
Reynolds, C. R., & Kamphaus, R. W. (2015). Behavior assessment system for children (3rd ed.). Bloomington: Pearson.
Rodriguez-Seijas, C., Gadow, K. D., Rosen, T. E., Kim, H., Lerner, M. D., & Eaton, N. R. (2019). A transdiagnostic model of psychiatric symptom co-occurrence and autism spectrum disorder. Autism Research. https://doi.org/10.1002/aur.2228.
Solberg, B. S., Zayats, T., Posserud, M.-B., Halmøy, A., Engeland, A., Haavik, J., & Klungsøyr, K. (2019a). "Patterns of psychiatric comorbidity and genetic correlations provide new insights into differences between attention-deficit/hyperactivity disorder and autism spectrum disorder": Erratum. Biological Psychiatry, 86(8), 647. https://doi.org/10.1016/j.biopsych.2019.07.025.
Solberg, B. S., Zayats, T., Posserud, M.-B., Halmøy, A., Engeland, A., Haavik, J., & Klungsøyr, K. (2019b). Patterns of psychiatric comorbidity and genetic correlations provide new insights into differences between attention-deficit/hyperactivity disorder and autism spectrum disorder. Biological Psychiatry, 86(8), 587–598. https://doi.org/10.1016/j.biopsych.2019.04.021.
Tonnsen, B. L., Boan, A. D., Bradley, C. C., Charles, J., Cohen, A., & Carpenter, L. A. (2016). Prevalence of autism spectrum disorders among children with intellectual disability. American Journal of Intellectual and Developmental Disabilities, 121(6), 487–500.
Volker, M. A., Smerbeck, A. M., Toomey, J., & Rodgers, J. D. (2009). BASC-2 PRS profiles for students with high-functioning autism spectrum disorders. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-009-0849-6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
We have a conflict of interest to disclose. Xuechun Zhou and Jianjun Zhu are employed by the publisher of the BASC-3, NCS Pearson. Cecil R. Reynolds and R.W. Kamphaus are co-authors of the BASC-3.
Additional information
Accepted by Dr. Arthur MacNeill Horton Jr. as Guest Action Editor
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, X., Reynolds, C., Zhu, J. et al. Differentiating Autism from ADHD in Children and Adolescents Using BASC-3. J Pediatr Neuropsychol 6, 61–65 (2020). https://doi.org/10.1007/s40817-020-00082-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40817-020-00082-7