Abstract
In adults, multiple sclerosis (MS) is associated with executive dysfunction, anxiety, depression, fatigue, and lowered quality of life. Similar problems may occur in pediatric MS, but the relationships between these variables have not yet been investigated. This study examined the associations among some of the most salient cognitive (executive functioning), psychological (anxiety, depression), and psychosocial (fatigue, quality of life, externalizing symptoms) factors affecting children with MS. Sixty-five patients with MS ages 6 to 18 were evaluated through the UCSF Regional Pediatric Multiple Sclerosis Center. Participants completed a neuropsychological assessment battery including the Verbal Fluency Test and Trail Making Test. Parents and children also completed rating forms assessing emotional functioning, fatigue, quality of life, and executive functioning. After controlling for significant demographic variables, higher levels of anxiety and depressive symptoms were associated with executive dysfunction on testing and self-report. In addition, higher reported executive dysfunction was associated with psychosocial difficulties, including higher levels of fatigue, worse quality of life, and more severe externalizing symptoms. The present study furthers our knowledge of the psychological and psychosocial factors associated with neurocognitive outcomes in pediatric MS. Recognition of these variables can inform medical and psychological treatment, as well as interventions in the home and community, to maximize a positive developmental trajectory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Multiple sclerosis (MS) is an autoimmune disease of the central nervous system characterized by episodes of inflammatory demyelination and gray matter atrophy (Compston and Coles 2002; Geurts and Barkhof 2008). The vast majority of MS cases occur in adulthood, but approximately 3–5% begin in childhood or adolescence. Approximately one-third of pediatric patients with MS experience cognitive impairment, which can occur even in the early stages of the disease (Amato et al. 2008; Ghezzi et al. 2010; Goretti et al. 2012; Julian et al. 2012; MacAllister et al. 2005). Similar to adults, children with MS have deficits in processing speed, complex attention, visual-motor integration, memory, executive functioning, and verbal fluency (Amato et al. 2008; Banwell and Anderson 2005; Banwell et al. 2007; Julian et al. 2012; MacAllister et al. 2005, 2007a). Some longitudinal studies of pediatric MS have found declines in cognitive performance over time (MacAllister et al. 2007b; Marin et al. 2012; Till et al. 2013), while others have revealed generally stable cognitive performance (Charvet et al. 2014).
Executive function abilities include attentional control, working memory, mental flexibility, planning, and goal-directed behavior (Delis et al. 2001) and have been found to be associated with activity of complex neural networks among the frontal lobe, parietal lobe, and subcortical structures (Alvarez and Emory 2006; Suchy 2009). Due to the diffuse nature of the neural networks underlying executive functions, they are particularly vulnerable to disruption from disease processes (Casey et al. 2005). In addition, as myelination progresses in a caudal-to-rostral pattern in neurodevelopment, the frontal systems involved in executive functions are among the last to myelinate in normal development (MacAllister et al. 2013; Rademacher et al. 1999). Thus, in addition to disrupting established brain networks, the MS disease process in children may have a particularly significant influence on the acquisition of neural circuits involved in executive functions.
Although the rates of executive dysfunction in the pediatric MS population vary widely, parent reports suggest that 19–50% of patients with MS evidence difficulty in one or more aspects of executive functioning (Holland et al. 2012; MacAllister 2010; Till et al. 2012a, b). On neuropsychological testing, children with MS have demonstrated impairment on a number of measures tapping executive functioning (Amato et al. 2008; Banwell and Anderson 2005; Blaschek et al. 2012; Charvet et al. 2014; MacAllister et al. 2005). Charvet et al. (2014) found that Forward and Backward Digit Span, a measure of attention and working memory, are among the most commonly impaired measures in pediatric MS (measured using the Wechsler Intelligence Scale for Children, 4th Edition [Wechsler 2004] or the Wechsler Adult Intelligence Scale, 4th Edition [Wechsler 2008] depending on subject age). Complex attention, or rapidly shifting attention between competing stimuli (measured by the Trail Making Test Part B; Reitan 1969), has shown the most pronounced decline over time (Marin et al. 2012). Impairments on the Modified Card Sorting Test (Nelson 1976), which measures set-shifting or mental flexibility, have also been reported in pediatric MS (Amato et al. 2008). In addition, children with MS have demonstrated impairments in self-generated organizational strategies as measured by the Rey-Osterrieth Complex Figure Copy (Banwell and Anderson 2005; Osterrieth 1944). Impairments in executive functioning impact multiple aspects of behavior and cognitive functioning, and they can limit an individual’s capacity for independence and social relationships (Jurado and Rosselli 2007).
In addition to its cognitive impact, pediatric MS influences psychological and psychosocial factors such as depression, anxiety, level of fatigue, quality of life, and behavior problems (Amato et al., 2008; MacAllister et al., 2005, 2009; Mowry et al., 2010; Till et al., 2012b). The prevalence of psychiatric disorders in childhood MS varies widely, with 30–60% of patients meeting criteria for mood disorder, anxiety disorder, attention deficit hyperactivity disorder (ADHD), or adjustment disorder (Amato et al. 2008; Boyd and MacMillan 2005; Goretti et al. 2010; MacAllister et al. 2005; Suppiej and Cainelli 2014; Thannhauser 2009; Weisbrot et al. 2014). Because onset of pediatric MS often occurs during the formative years of development in adolescence, it has the potential to change the trajectory of psychosocial development in fundamentally different ways from adults. Among patients with adult-onset MS, the psychosocial effects of the disease are thought to be related to the psychological factors associated with having a chronic illness, as well as the direct impact of the disease on fully developed brain networks responsible for emotional and behavioral regulation (Till et al. 2012a, b). Whether these mechanisms play a role in psychosocial functioning in pediatric MS remains to be determined.
Very few studies to date have investigated the relationships among aspects of cognitive, psychological, and psychosocial functioning impacted by pediatric MS. Among children with MS who have comorbid psychiatric diagnoses, those who are diagnosed with an anxiety or mood disorder tend to show the highest frequency of cognitive impairment (Weisbrot et al. 2014). Conflicting findings have been reported with one study finding no relationship between psychological and cognitive functioning among children with MS (Goretti et al. 2012), while another study found negative correlations between anxiety/depression and executive functioning among children with MS (Holland et al. 2012). Holland and colleagues (2012) found that in pediatric MS, symptoms of anxiety are associated with poorer performance on the Trail Making Test and Digit Span, in particular the set-shifting condition of the Trail Making Test (Part B). Depressive symptoms as reported by parents on the Behavior Assessment System for Children, Second Edition (BASC-2; Reynolds and Kamphaus 2004) are similarly associated with poorer performance on these measures with the strongest associations among both Digit Span and Trail Making Test Part B in pediatric MS (Holland et al. 2012).
Several other studies have investigated cognitive functions in relation to psychosocial functioning including domains of quality of life and fatigue. Cognitive problems such as executive dysfunction in pediatric MS can negatively impact quality of life. For example, in school, students may require extra support from teachers due to cognitive difficulties, while in their social lives, children’s participation in hobbies and sports may be limited due to cognitive impairments (Amato et al. 2008, 2010). With regard to fatigue, Holland and colleagues (2012) found that higher levels of self-reported fatigue among children with MS were associated with poorer performance on Trail Making Test Parts A and B. Furthermore, Goretti and colleagues (2012) found that higher levels of self-reported cognitive fatigue in children with MS were associated with impaired performance on a problem-solving test (Tower of London Test; Shallice 1982) and that higher levels of parent-reported cognitive fatigue were correlated with impaired performance on tests of processing speed and complex attention (Trail Making Test Part B). These results suggest a relationship between cognitive fatigue and tasks requiring prolonged and effortful mental activity among children with MS. However, several other studies have failed to show an effect of fatigue on cognitive functioning (Amato et al. 2008; MacAllister et al. 2005). Regarding externalizing symptoms, while one study found that parents endorsed the presence of externalizing behaviors (e.g., hyperactivity, aggression, conduct problems) in youth with MS, only the inattention/hyperactivity index was significantly different from healthy controls (Till et al. 2012a, b). In fact, parent ratings were significantly higher for internalizing problems, such as depression and somatization, consistent with the existing literature (Charvet et al. 2016; Parrish et al. 2013; Till et al. 2012a, b).
Although limited, current research indicates that similar to adult MS, psychological issues such as anxiety and depression may be related to worse cognitive functioning in pediatric MS, specifically on tasks of executive functioning. Among adults, anxiety and depression have been shown to be independent predictors of executive dysfunction (Julian and Arnett 2009). In addition, impairments in executive functioning have been related to certain psychosocial variables such as fatigue and quality of life. Cognitive functioning has been shown to predict psychosocial functioning, especially quality of life, in adults with MS (Benedict et al. 2005). To the authors’ knowledge, no study to date has investigated the relationships between executive functioning, psychological functioning (e.g., depression, anxiety), and psychosocial functioning (e.g., fatigue, quality of life, externalizing behavior) within the same pediatric MS population. Thus, the current study aims to investigate these relationships. Consistent with previous findings in adults with MS, we hypothesized that increased anxiety and depression would be associated with greater executive dysfunction (hypothesis 1) and that greater executive dysfunction would be associated with worse psychosocial functioning (hypothesis 2).
Method
Participants
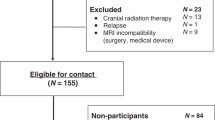
This retrospective study analyzed the performance of 65 patients with pediatric-onset relapsing-remitting MS seen at the UCSF Regional Pediatric Multiple Sclerosis Center between 2006 and 2014. The study received approval by the Palo Alto University institutional review board. Data for specific measures were available for varying subsets of the participants, with sample sizes ranging from 39 to 54. Neuropsychological testing was performed as part of routine care at the clinic and offered to consecutive patients regardless of health insurance coverage. This archival dataset was part of a larger multicenter study through the Pediatric MS Centers of Excellence established by the National MS Society (Julian et al. 2012).
Eligibility criteria for this study included participants who met criteria for a diagnosis of pediatric MS (Krupp et al. 2007) and who were younger than 18 years of age at the time of disease onset. Participants were also required to be younger than 18 years of age at the time of neuropsychological assessment, to have completed at least one measure of executive functioning, to speak and read English, and to have sufficient motor and visual capabilities to complete neuropsychological testing. Participants who had a history of developmental delay or who had received glucocorticoid treatment within 1 month of the time of neuropsychological assessment were excluded from the study.
Neuropsychological Measures
The UCSF Regional Pediatric Multiple Sclerosis Center uses a comprehensive battery addressing multiple cognitive domains. The battery varied slightly based on participant age and availability of normative data. The battery was administered by a clinical neuropsychologist or a trained and supervised psychometrician, and participants were given breaks as needed. Only those measures used for this study will be reviewed here.
Wechsler Abbreviated Scale of Intelligence (WASI)
The WASI is a screening instrument designed to provide a brief estimate of general intelligence (Wechsler 1999). The two-subtest form, consisting of vocabulary and matrix reasoning subtests, results in an FSIQ-2 Standard Score (T Score) which was used as a measure of IQ for each participant. The two-subtest form of the WASI has high loadings on a general intellectual ability factor (g) and represents both verbal/crystallized and nonverbal/fluid abilities. The average reliability coefficient for the FSIQ-2 is .96 (Wechsler 1999).
Delis-Kaplan Executive Function System (D-KEFS) Trail Making Test
The D-KEFS Trail Making Test (Delis et al. 2001) is designed to measure the following component processes of executive function: visual scanning, number sequencing, letter sequencing, number-letter switching, and motor speed. This test is an iteration of the Halstead-Reitan Trail-Making Test Part A and B, which demonstrate adequate test-retest reliability (Levine et al. 2004) and construct validity (Strauss et al. 2006). The Trail Making Test Part B has been found to be particularly sensitive to impairment in pediatric MS (MacAllister et al. 2005; Till et al. 2012a, b). For the present study, the completion time on the number-letter switching condition of the D-KEFS Trail Making Test (the equivalent of Trail Making Test Part B) was used as a performance-based measure of executive function.
Delis-Kaplan Executive Function System (D-KEFS) Verbal Fluency Test
The D-KEFS Verbal Fluency Test (Delis et al. 2001) measures fluent productivity in the verbal domain and is believed to assess facets of executive functioning such as self-initiation, working memory, and processing speed (Strauss et al. 2006). The participant produces words that begin with a specific letter, then names words belonging to a particular semantic category, and then switches between two different semantic categories. In this study, the total number of correct responses on the switching condition, with reliability coefficients ranging from .51 to .73 (Delis et al. 2001), was used as a performance-based measure of executive functioning.
Self-report measures
Behavior Rating Inventory of Executive Function (BRIEF)
The BRIEF (Gioia et al. 2000) is a rating scale designed to measure real world executive functioning and includes self- and parent-report versions, which demonstrate satisfactory internal consistency ranging from .80 to .98. Test-retest correlations for the Global Executive Composite, Behavioral Regulation Index, and the Metacognition Index are .86, .84, and .88, respectively (Gioia et al. 2000). In this study, the Global Executive Composite T scores for both the self- and parent-reports were used as report-based measures of executive functioning.
Behavior Assessment System for Children, Second Edition (BASC-2)
The BASC-2 (Reynolds and Kamphaus 2004) is a rating scale designed to facilitate the classification of a variety of emotional and behavioral disorders in children ages 2 through 25 and to facilitate intervention planning. Participants completed the Self-Report of Personality and parents completed the Parent Rating Scales. The Depression subscale T score on both the self- and parent-report was used as a measure of depression, while the anxiety subscale T score on the self- and parent-report was used as a measure of anxiety. Anxiety and depression subscales on the BASC-2 have demonstrated internal consistency and reliability for children and adolescents (α = .79 to .88 for anxiety; α = .87 to .93 for depression). They have also shown strong internal consistency in the pediatric MS population (Till et al. 2012a, b) and have been studied in relation to executive functioning in the past (Holland et al. 2012). The Externalizing Problems Composite T score on the parent-report was used as a measure of externalizing behavior and also shows strong internal consistency in the pediatric MS population (Till et al. 2012a, b). Given that externalizing problems have not been examined in depth in the pediatric MS population, the Externalizing Problems Composite T score (which includes hyperactivity, aggression, and conduct problems) was chosen to identify whether this domain warrants further examination without increasing type I error.
Pediatric Quality of Life Inventory, Version 4.0 (PedsQL)
The PedsQL (Varni et al. 1999) is a modular instrument for measuring health-related quality of life in healthy children and adolescents, as well as those who have medical conditions (Varni et al. 2002). Both patients and their parents completed the PedsQL 4.0 Generic Core Scales and the Multidimensional Fatigue Scale (MFS). The Total Scale Score on the PedsQL Parent- and Self-Reports were used as measures of parent- and self-reported quality of life, respectively. The PedsQL 4.0 Generic Core Scales demonstrates strong internal consistency (α = .83 for child self report and α = .86 for parent proxy-report; Varni et al. 1999) and has been shown to be sensitive to quality of life issues in pediatric cancer, cerebral palsy, cardiac disease, and pediatric MS (Mowry et al. 2010; Varni et al. 2002).
The PedsQL Multidimensional Fatigue Scale (MFS; Varni et al. 1999) is a specific module of the Pediatric Quality of Life Inventory, Version 4.0. It was designed as a generic symptom-specific instrument to measure fatigue in pediatric patients as well as healthy school and community populations (Varni et al. 1999). The 18-item scale results in three subscales: (1) general fatigue, (2) sleep/rest fatigue, and (3) cognitive fatigue. The Parent- and Self-Report Total Scale Scores were used as measures of fatigue based on previous research suggesting that the item content reflects the components of fatigue commonly assessed by physicians treating pediatric patients with MS (Holland et al. 2012). The MFS Total Scale Score demonstrates strong internal consistency for both the self- (α = .89) and parent-report (α = .92; Varni et al. 2002).
Sociodemographic and Clinical Variables
Sociodemographic variables extracted for the purposes of this study included sex, race, mother and father’s education level, and age at neuropsychological evaluation. Clinical variables included diagnosis, age at symptom onset (years), disease duration (years), and disability as measured by the Expanded Disability Status Scale (EDSS; Kurtzke 1983).
Statistical Analyses
The data were analyzed using the Statistical Package for Social Sciences (SPSS, Version 20, released in 2011). Raw scores were used for analyses with the exception of the WASI, BRIEF, and BASC-2, which were analyzed using T scores. In addition, the MFS and PedsQL were analyzed using composite scores.
Other possible covariates that were considered in the analyses included sex, race, parent education level, age at testing, age at symptom onset, disease duration, disease severity, and IQ. When these variables correlated with any of the dependent variables, they were controlled for in the analyses. Prior to conducting regression analyses, preliminary correlations were performed in order to determine the zero-order relationships between predictors and variables of interest in an effort to confirm the absence of spurious relationships. Preliminary correlations between continuous variables were assessed using the Pearson correlation coefficient, and correlations involving discrete variables (e.g., disease severity) were assessed with the non-parametric Spearman rank correlation coefficient. Hierarchical regression analyses were then conducted for each of the two main hypotheses to determine predictors of executive and psychosocial functioning. To ensure that assumptions of the linear regression model were met, we examined our predictors for absence of multicollinearity and found that all variables met this assumption.
Results
Sample Demographics and Descriptive Statistics
Participant demographics for the 65 children and adolescents with multiple sclerosis (25 boys and 40 girls) are presented in Table 1. Mean age of participants at the time of testing was 14.61 years (SD = 3.01, range 6.5–18.0) with mean disease duration of 2.26 years (SD = 2.10, range .08–10.95). Descriptive statistics for the variables of interest are presented in Table 2.
Hypothesis 1
Preliminary Pearson correlations were conducted in order to determine the zero-order relationships among anxiety, depression, and executive functioning. As shown in Table 3, the Trail Making Test and Verbal Fluency Test were both significantly correlated with parent-reported anxiety. The BRIEF Self-Report was strongly correlated with self-reported anxiety, as well as self- and parent-reported depression. The BRIEF Parent-Report was significantly correlated with parent-reported anxiety and depression.
Hierarchical and simultaneous regression analyses were then conducted to assess the unique variance that anxiety and depression contributed to executive functioning (see Table 4). After controlling for significant patient and disease factors, parent-reported anxiety accounted for an additional 7% of the variance in executive functioning as measured by the Trail Making Test (p = .031) but did not contribute significantly to executive functioning as measured by the Verbal Fluency Test (p = .648). In a simultaneous regression, self-reported anxiety, self-reported depression, and parent-reported depression explained 61% of the variance on the BRIEF Self-Report (p < .001), with only self-reported depression (β = .55, p < .001) and parent-reported depression (β = .28, p = .047) showing significant contributions to the model. In another regression, after controlling for disease duration, parent-reported anxiety and depression accounted for an additional 54% of the variance in executive functioning as measured by the BRIEF Parent-Report (p < .001); however, only parent-reported depression significantly contributed to the model (β = .85, p < .001).
Hypothesis 2
Two-tailed preliminary Pearson correlations were conducted in order to determine the zero-order relationships among psychosocial variables (fatigue, quality of life, externalizing symptoms) and executive functioning. As shown in Table 5, performance-based measures of executive functioning (Trail Making Test and Verbal Fluency) were not significantly correlated with any psychosocial variables. Self-reported executive function (BRIEF Self-Report) was significantly correlated with self- and parent-reported fatigue (MFS Self- and Parent-Report), as well as self- and parent-reported quality of life (PedsQL Self- and Parent-Report). Parent-reported executive function was significantly correlated with self- and parent-reported fatigue (MFS Self- and Parent-Report), parent-reported quality of life (PedsQL Parent-Report), and parent-reported behavior problems (BASC-2 Externalizing Problems).
Table 6 displays the hierarchical and simultaneous regression analyses that were then conducted to assess the unique variance that each measure of executive functioning contributed to each psychosocial variable. After controlling for significant patient and disease factors, the BRIEF Self- and Parent-Report accounted for an additional 51% of the variance in self-reported fatigue as measured by MFS Self-Report (p < .001). In a separate regression, the BRIEF Parent- and Self-Report accounted for an additional 41% of the variance in parent-reported fatigue as measured by the MFS Parent-Report (p < .001). Regarding quality of life, the BRIEF Self-Report accounted for an additional 37% of the variance on self-reported quality of life as measured by the PedsQL Self-Report (p < .001). In a simultaneous regression, the BRIEF Self- and Parent-Report significantly explained 51% of the variance on the PedsQL Parent-Report (p < .001), but only the BRIEF Parent-Report (β = −.60, p < .01) showed a significant contribution to the model. Lastly, the BRIEF Parent-Report significantly explained 67% of the variance for the BASC-2 Externalizing Problems (p < .001).
Discussion
We report that anxiety and depression are associated with aspects of executive dysfunction in a population of pediatric MS patients, as measured by performance-based and self-report measures, providing partial support for our first hypothesis. Specifically, anxiety was related to one performance-based measure of executive functioning (Trail Making Test), while depression was related to self-report measures of executive functioning but not performance-based measures. These findings on performance-based measures of executive functioning are generally consistent with previous studies that have found correlations among these variables. This includes Holland and colleagues’ (2012) study, which found that parent-reported anxiety significantly correlated with the Trail Making Test A and B but not the D-KEFS Verbal Fluency Test. However, they also found that parent-reported depression significantly correlated with the Trail Making Test A and B, which the current study did not find. This discrepancy may be due to the use of different Trail Making Tests, as well as differences in sample characteristics. Taken together, our findings suggest that anxiety is more associated with performance on executive functioning tasks than is depression.
In contrast with performance-based measures of executive functioning, self-report measures of executive functioning (BRIEF Self- and Parent-Report) showed significant relationships with depression but not anxiety. Depressive symptoms are associated with increased symptom reporting in individuals with medical disorders (Ciechanowski et al. 2003). Thus, in the current study, the presence of depressive symptoms could have resulted in an increased perception and/or reporting of executive function deficits, even if these deficits are fairly mild on objective neuropsychological testing. On the other hand, it is possible that depressive symptoms are more strongly associated with executive dysfunction in a real-world setting (such as problems with initiation, task monitoring, planning, and organization) than performance on measures given in a highly structured neuropsychological testing environment. From a neurobiological perspective, abnormal functioning of the hypothalamic-pituitary-adrenal axis plays a role in depressive symptomatology, and it is also associated with structural changes in the frontal cortex (Weinstock 2008). Thus, it is possible that depression could impact executive functions mediated by the frontal cortex (Schmitt et al. 2012), which may manifest more strongly in the real world than in a controlled testing environment.
Our second hypothesis—that executive functioning would be associated with psychosocial functioning (including fatigue, quality of life, and externalizing symptoms)—was partially upheld. The most notable exception was that performance-based measures of executive functioning (Trail Making Test, Verbal Fluency Test) were not associated with any measures of psychosocial functioning, while report-based measures were. In particular, the finding that performance on tests of executive functioning is not related to fatigue is generally consistent with a growing number of studies (Carroll et al. 2015). Several pediatric (Amato et al. 2008; MacAllister et al. 2005) and adult MS studies (Krupp and Elkins 2000; Morrow et al. 2009; Paul et al. 1998; Schwartz et al. 1996) have shown that self-reported fatigue is not strongly correlated with neuropsychological test performance. Two other studies have found partially conflicting results, showing that higher levels of parent- and self-reported cognitive and general fatigue were associated with impaired performance on the Trail Making Test B (Goretti et al. 2012; Holland et al. 2012) but not on the Verbal Fluency Test. The choice of MFS subscales used in analyses may explain why these findings partially conflict with the current study, as we measured fatigue using the fatigue total score rather than the general or cognitive fatigue subscales.
With regard to other psychosocial variables, the current study also indicates a relationship between report-based measures of executive functioning and quality of life and externalizing symptoms, which has not yet been examined in the research to date. One explanation for this finding is that report-based measures are affected by issues of recall and response bias, and they may be more likely to show correlations with one another (Prince et al. 2008). This explanation is supported by the fact that the BRIEF Self-Report correlated most highly with self-report measures of psychosocial functioning, while the BRIEF Parent-Report correlated most highly with parent questionnaires of psychosocial functioning. Despite these caveats, the current findings can also be understood by the multi-faceted representation of executive function afforded by the BRIEF and its potential for greater ecological validity when compared to the performance-based measures of executive functioning (Trail Making Test, Verbal Fluency Test) used in this study. Previous research has suggested that performance-based measures of executive functioning may not be sensitive to executive dysfunction in everyday life because the cognitive processes being measured are overly specific (Mangeot et al. 2002; Silver 2000). By contrast, the BRIEF was specifically developed to encompass executive dysfunction as it manifests children’s day-to-day activities (Gioia et al. 2000). Given the broad scope of the BRIEF, it is logical that it would be an important predictor of psychosocial functioning (i.e., how a child functions within his/her social environment). More specifically, it makes sense that aspects of executive functioning in daily life—including the ability to plan, organize, and complete tasks, shift from one task to another, and regulate emotional responses appropriately—would be related to a child’s level of fatigue, quality of life, and disruptive behaviors.
Overall, results related to our second hypothesis suggest that while tests of executive functioning may have more limited applicability in predicting how a child with MS will function in his/her daily life, self-report measures (which more accurately capture real-world executive deficits) are more closely related to everyday psychosocial functioning. Therefore, when designing a neuropsychological battery for children with MS, it may be beneficial to consider the strong association of the BRIEF with psychosocial functioning (particularly for externalizing symptoms), especially when areas of psychosocial functioning are a concern. However, it is also important to note that while these findings are currently understood within the context of a pediatric MS population, it is not yet possible to conclude whether or not these results are disease-specific. It is possible that the associations revealed by this study might also be found in a healthy population or in any population with a chronic illness, which provides an interesting line of further inquiry.
There are several limitations to the present study, including the relatively short disease duration of the sample (mean = 2.37 years), which may have resulted in restriction of range, as well as the use of self-report measures, which are affected by threats to validity, particularly those occurring due to response bias (De Los Reyes and Kazdin 2005; Prince et al. 2008). Although the study sample was large (N = 65), the sample sizes for each neuropsychological measure and self-report questionnaire were smaller, resulting in lower power. In addition, due to the retrospective nature of this study, data on the presence of other neurological and non-neurological disorders (other than developmental delay) were not available, which may limit the applicability of our findings to the MS population. The analyses also did not include other sociodemographic and clinical variables that may influence neuropsychological performance in children, including parent language status, use of disease-modifying therapies or other medications, and aspects of disease burden as measured by magnetic resonance imaging (MRI). Future research should endeavor to control for these additional variables. Additionally, while set-shifting is an important component of executive functioning, our measures did not directly address other components of executive functioning (e.g., initiation, maintenance, etc.) that may be relevant to psychosocial functioning. Future research may also consider individually examining the specific components of the BASC-2 Externalizing Problems Composite (i.e., hyperactivity, aggression, and conduct problems) to determine their differential contributions to executive functioning. Another consideration in the interpretation of these findings is the directionality of hypotheses. In an effort to build upon existing findings of mood predicting cognition and cognition predicting psychosocial functioning in adults with MS, we maintained the directions of these findings in the current study hypotheses. However, a recent study by Charvet and colleagues (2016) found that cognitive functioning predicted psychological functioning in pediatric MS. Future studies should seek to clarify the directionality of the relationships between these variables. Finally, given the cross-sectional design of this study, future research should examine these hypotheses over time. A longitudinal design could outline causal mechanisms that would enhance our understanding of not only which factors influence each other, but also which factors would serve as the best targets for intervention.
Despite these limitations, to the authors’ knowledge, this is one of the largest studies to date that has examined cognitive, psychological, and psychosocial factors in a pediatric MS population. We present the unique finding that higher levels of depressive symptoms are associated with greater reported problems with executive functioning in daily life in this population. In addition, our findings reveal that perceived executive deficits are associated with higher levels of fatigue, lower quality of life, and greater externalizing problems. These results also suggest that self-report measures of executive functioning are better related to psychosocial factors in the pediatric MS population than neuropsychological tests of executive functioning, which emphasizes the importance of including self-report measures when assessing this population.
This study also encourages further examination of cognitive, psychological, and psychosocial outcomes in pediatric MS in identifying targets for intervention. For example, the current findings suggest that targeting depression, anxiety, fatigue, and quality of life in pediatric MS may contribute to improvements in executive functioning, and vice versa. This lays the groundwork for future intervention-focused research.
In addition, the current findings emphasize the need for regular monitoring by neuropsychology as part of a multidisciplinary team. In formulating appropriate recommendations for this population, neuropsychologists should consider the psychological and psychosocial difficulties that may be influencing executive functioning both on testing and in the child’s daily life. This study’s finding that the BRIEF Self- and Parent-Report are strong predictors of psychosocial difficulties suggests that this may be a useful measure to use in this population, not only in evaluating executive dysfunction but also in understanding the broader impact this has on the child’s daily life.
While clinical information easily gleaned from a medical chart (such as age of onset, disease duration, and disease severity) may relate to certain aspects of cognitive functioning, the findings of this study suggest that this information will not necessarily provide accurate predictions about how the child may be functioning on a psychosocial level. This, too, emphasizes the importance of regular use of screens for detecting psychosocial difficulties, including the MFS and PedsQL.
Detection of impairments in psychological, psychosocial, and executive function can be used to inform development of educational planning (e.g., school accommodations, school placement) that will help maximize educational opportunities. In addition, awareness of the psychosocial effects of pediatric MS can help guide interventions within the home and the community in order to facilitate a positive developmental trajectory.
Lastly, this study furthers our clinical understanding of the ways in which pediatric MS is similar and distinct from adult-onset MS. As understood within the life course model of disease formation, the biological and psychosocial factors that interact throughout the life course may influence disease risk in different ways depending on the particular period in development during which they occur (Ben-Shlomo and Kuh 2002; Dennis 2000). In pediatric MS, demyelination and inflammation occur during formative years, and therefore have the potential to disrupt typical development (MacAllister et al. 2013). As a result, the disease can have profound impacts on cognitive development and psychosocial functioning in childhood. This study contributes to our understanding of MS throughout the lifespan, suggesting that relationships among executive, psychosocial, and psychological functioning that have been found in adults may also be found in children with the disease. However, it remains unknown how these relationships may change as these children age. Thus, further studies are needed to characterize the functioning of patients with pediatric-onset MS once they reach adulthood.
References
Alvarez, J. A., & Emory, E. (2006). Executive function and the frontal lobes: a meta-analytic review. Neuropsychology Review, 16(1), 17–42.
Amato, M. P., Goretti, B., Ghezzi, A., Lori, S., Zipoli, V., Portaccio, E.,…Trojano, M. (2008). Cognitive and psychosocial features of childhood and juvenile MS. Neurology, 70(20), 1891–1897.
Amato, M. P., Goretti, B., Ghezzi, A., Lori, S., Zipoli, V., Portaccio, E.,…Trojano, M. (2010). Cognitive and psychosocial features in childhood and juvenile MS: Two-year follow-up. Neurology, 75(13), 1134–1140.
Banwell, B. L., & Anderson, P. E. (2005). The cognitive burden of multiple sclerosis in children. Neurology, 64(5), 891–894.
Banwell, B., Ghezzi, A., Bar-Or, A., Mikaeloff, Y., & Tardieu, M. (2007). Multiple sclerosis in children: clinical diagnosis, therapeutic strategies, and future directions. Lancet Neurology, 6(10), 887–902.
Benedict, R. H., Wahlig, E., Bakshi, R., Fishman, I., Munschauer, F., Zivadinov, R., & Weinstock-Guttman, B. (2005). Predicting quality of life in multiple sclerosis: accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. Journal of the Neurological Sciences, 231(1), 29–34.
Ben-Shlomo, Y., & Kuh, D. (2002). A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology, 31, 285–293.
Blaschek, A., Van’s Gravesande, K. S., Heinen, F., Pritsch, M., Mall, V., & Calabrese, P. (2012). Neuropsychological aspects of childhood multiple sclerosis: an overview. Neuropediatrics, 43(4), 176–183.
Boyd, J. R., & MacMillan, L. J. (2005). Experiences of children and adolescents living with multiple sclerosis. Journal of Neuroscience Nursing, 37(6), 334–342.
Carroll, S., Chalder, T., Hemingway, C., Heyman, I., & Moss-Morris, R. (2015). Understanding fatigue in paediatric multiple sclerosis: a systematic review of clinical and psychosocial factors. Developmental Medicine and Child Neurology, 58(3), 229–239.
Casey, B. J., Tottenham, N., Liston, C., & Durston, S. (2005). Imaging the developing brain: what have we learned about cognitive development? Trends in Cognitive Science, 9(3), 104–110.
Charvet, L. E., O’Donnell, E. H., Belman, A. L., Chitnis, T., Ness, J. M., Parrish, J.,…Krupp, L. B. (2014). Longitudinal evaluation of cognitive functioning in pediatric multiple sclerosis: Report from the US Pediatric Multiple Sclerosis Network. Multiple Sclerosis Journal, 20(11), 1502–1510.
Charvet, L., Cersosimo, B., Schwarz, C., Belman, A., & Krupp, L. B. (2016). Behavioral symptoms in pediatric multiple sclerosis: relation to fatigue and cognitive impairment. Journal of Child Neurology.
Ciechanowski, P. S., Katon, W. J., Russo, J. E., & Hirsch, I. B. (2003). The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. General Hospital Psychiatry: Psychiatry, Medicine and Primary Care, 25(4), 246–252.
Compston, A., & Coles, A. (2002). Multiple sclerosis. The Lancet, 359(9313), 1221–1231.
De Los Reyes, A., & Kazdin, A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131(4), 483–509.
Delis, D. C., Kaplan, E., & Kramer, J. H. (2001). Delis-Kaplan executive function system. Psyctests.
Dennis, M. (2000). Childhood medical disorders and cognitive impairment: biological risk, time, development, and reserve. In K. O. Yeates, M. D. Ris, & H. G. Taylor (Eds.), Pediatric neuropsychology: research, theory, and practice (pp. 3–22). New York: Guilford Press.
Geurts, J. G., & Barkhof, F. (2008). Grey matter pathology in multiple sclerosis. Lancet Neurology, 7(9), 841–851.
Ghezzi, A. A., Goretti, B. B., Portaccio, E. E., Roscio, M. M., & Amato, M. M. (2010). Cognitive impairment in pediatric multiple sclerosis. Neurological Sciences, 31(Suppl. 2), S215–S218.
Gioia, G. A., Isquith, P. K., Guy, S. C., & Kenworthy, L. (2000). Behavior rating inventory of executive function. Lutz: Psychological Assessment Resources.
Goretti, B., Ghezzi, A., Portaccio, E., Lori, S., Zipoli, V., Razzolini, L.,…Amato, M. P. (2010). Psychosocial issues in children and adolescents with multiple sclerosis. Neurological Sciences, 31(4), 467–470.
Goretti, B., Portaccio, E., Ghezzi, A., Lori, S., Moiola, L., Falautano, M.,…Amato, M. P. (2012). Fatigue and its relationships with cognitive functioning and depression in paediatric multiple sclerosis. Multiple Sclerosis, 18(3), 329–334.
Holland, A., Graves, D., Greenberg, B., & Harder, L. (2012). Fatigue, emotional functioning, and executive dysfunction in pediatric multiple sclerosis. Child Neuropsychology, 20(1), 71–85.
Julian, L. J., & Arnett, P. A. (2009). Relationships among anxiety, depression, and executive functioning in multiple sclerosis. The Clinical Neuropsychologist, 23(5), 794–804.
Julian, L., Serafin, D., Charvet, L., Ackerson, J., Benedict, R., Braaten, E.,…Krupp, L. (2012). Cognitive impairment occurs in children and adolescents with multiple sclerosis: Results from a United States network. Journal of Child Neurology, 28(1), 102–107
Jurado, M. B., & Rosselli, M. (2007). The elusive nature of executive functions: a review of our current understanding. Neuropsychology Review, 17(3), 213–233.
Krupp, L. B., & Elkins, L. (2000). Fatigue and declines in cognitive functioning in multiple sclerosis. Neurology, 55(7), 934–939.
Krupp, L. B., Banwell, B., & Tenembaum, S. (2007). Consensus definitions proposed for pediatric multiple sclerosis and related disorders. Neurology, 68(Suppl. 2), S7–S12.
Kurtzke, J. (1983). Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology, 33(11), 1444–1452.
Levine, A. J., Miller, E. N., Becker, J. T., Selnes, O. A., & Cohen, B. A. (2004). Normative data for determining significance of test-retest differences on eight common neuropsychological instruments. The Clinical Neuropsychologist, 18(3), 373–384.
MacAllister, W. S. (2010). Multiple sclerosis in children and adolescents: Neurocognitive disorders. In D. Riva & C. Njiokiktjien (Eds.), Brain lesion localization and developmental functions: Basal ganglia, connecting systems, cerebellum, mirror neurons (pp. 81–88). Montrouge, France: John Libbey Eurotext.
MacAllister, W. S., Belman, A., Milazzo, M., Weisbrot, D., Christodoulou, C., Scherl, W.,… Krupp, L. (2005). Cognitive functioning in children and adolescents with multiple sclerosis. Neurology, 64(8), 1422–1425.
MacAllister, W. S., Boyd, J. R., Hollans, N. J., Milazzo, M. C., & Krupp, L. B. (2007a). The psychosocial consequences of pediatric multiple sclerosis. Neurology, 68(Suppl. 2), S66–S69.
MacAllister, W. S., Christodoulou, C., Milazzo, M., & Krupp, L. (2007b). Longitudinal neuropsychological assessment in pediatric multiple sclerosis. Developmental Neurobiology, 32(2), 625–644.
MacAllister, W. S., Christodoulou, C., Troxell, R., Milazzo, M., Block, P., Preston, T.,…Krupp, L. (2009). Fatigue and quality of life in pediatric multiple sclerosis. Multiple Sclerosis, 15(12), 1502–1508.
MacAllister, W. S., Christodoulou, C., Milazzo, M., Preston, T. E., Serafin, D., Krupp, L. B.,…Harder, L. (2013). Pediatric multiple sclerosis: What we know and where are we headed? Child Neuropsychology, 19(1), 1–22.
Mangeot, S., Armstrong, K., Colvin, A. N., Yeates, K. O., & Taylor, H. G. (2002). Long-term executive function deficits in children with traumatic brain injuries: assessment using the behavior rating inventory of executive function (BRIEF). Child Neuropsychology, 8(4), 271–284.
Marin, S., Banwell, B., & Till, C. (2012). Cognitive trajectories in 4 patients with pediatric-onset multiple sclerosis: serial evaluation over a decade. Journal of Child Neurology, 28(12), 1577–1586.
Morrow, S. A., Weinstock-Guttman, B., Munschauer, F. E., Hojnaki, D., & Benedict, R. H. (2009). Subjective fatigue is not associated with cognitive impairment in multiple sclerosis: cross-sectional and longitudinal analysis. Multiple Sclerosis, 15(8), 998–1005.
Mowry, E., Julian, L., Im-Wang, S., Chabas, D., Galvin, A., Strober, J., & Waubant, E. (2010). Health-related quality of life is reduced in pediatric multiple sclerosis. Pediatric Neurology, 43(2), 97–102.
Nelson, H. E. (1976). A modified card sorting test sensitive to frontal lobe defects. Cortex, 12(4), 313–324.
Osterrieth, P. A. (1944). Le test de copie d’une figure complex: contribution à l’étude de la perception et de la mémoire. Archives de Psychologie, 30, 286–356.
Parrish, J. B., Weinstock-Guttman, B., Smerbeck, A., Benedict, R. H. B., & Yeh, E. A. (2013). Fatigue and depression in children with demyelinating disorders. Journal of Child Neurology, 28(6), 713–718.
Paul, R. H., Beatty, W. W., Schneider, R., Blanco, C. R., & Hames, K. A. (1998). Cognitive and physical fatigue in multiple sclerosis: relations between self-report and objective performance. Applied Neuropsychology, 5(3), 143.
Prince, S. A., Adamo, K. B., Hamel, M. E., Hardt, J., Connor Gorber, S., & Tremblay, M. (2008). A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. International Journal of Behavioral Nutrition and Physical Activity.
Rademacher, J., Engelbrecht, V., Burgel, U., Freund, H., & Zilles, K. (1999). Measuring in vivo myelination of human white matter fiber tracts with magnetization transfer MR. NeuroImage, 9(4), 393–406.
Reitan, R. (1969). Manual for administration of neuropsychological test batteries on adults and children. Bloomington: Indiana University Press.
Reynolds, C. R., & Kamphaus, R. W. (2004). Behavior assessment system for children (2nd ed.). Toronto: Pearson Canada Assessment Inc.
Schmitt, A. J., Miller, J., & Long, K. (2012). Executive functioning profiles of children who display inattentive and overactive behavior in general education classrooms. The School Psychologist, 66(3). Retrieved from http://www.apadivisions.org/division-16/publications/newsletters/school-psychologist/index.aspx
Schwartz, C., Coulthard-Morris, L., & Zeng, Q. (1996). Psychosocial correlates of fatigue in multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 77(2), 165–170.
Shallice, T. (1982). Specific impairments of planning. Philosophical Transactions of the Royal Society of London B, 298, 199–209.
Silver, C. H. (2000). Ecological validity of neuropsychological assessment in childhood traumatic brain injury. The Journal of Head Trauma Rehabilitation, 15(4), 973–988.
Strauss, E., Sherman, E. M. S., & Spreen, O. (2006). A compendium of neuropsychological tests: Administration, norms, and commentary (3rd ed.). New York: Oxford University Press.
Suchy, Y. (2009). Executive functioning: overview, assessment, and research issues for Non-neuropsychologists. Annals of Behavioral Medicine, 37(2), 106–116.
Suppiej, A., & Cainelli, E. (2014). Cognitive dysfunction in pediatric multiple sclerosis. Neuropsychiatric Disease and Treatment, 10, 1385–1392.
Thannhauser, J. E. (2009). Grief-peer dynamics: understanding experiences with pediatric multiple sclerosis. Qualitative Health Research, 19(6), 766–777.
Till, C., Ho, C., Dudani, A., García-Lorenzo, D., Collins, D., & Banwell, B. (2012a). Magnetic resonance imaging predictors of executive functioning in patients with pediatric-onset multiple sclerosis. Archives of Clinical Neuropsychology, 27(5), 495–509.
Till, C., Udler, E., Ghassemi, R., Narayanan, S., Arnold, D., & Banwell, B. (2012b). Factors associated with emotional and behavioral outcomes in adolescents with multiple sclerosis. Multiple Sclerosis, 18(8), 1170–1180.
Till, C., Racine, N., Araujo, D., Narayanan, S., Collins, D., Aubert-Broche, B.,…Banwell, B. (2013). Changes in cognitive performance over a 1-year period in children and adolescents with multiple sclerosis. Neuropsychology, 27(2), 210–219.
Varni, J. W., Seid, M., & Rode, C. (1999). The PedsQL: measurement model for the pediatric quality of life inventory. Medical Care, 37(2), 126–139.
Varni, J. W., Burwinkle, T. M., Katz, E. R., Meeske, K., & Dickinson, P. (2002). The PedsQL in pediatric cancer. Cancer, 94(7), 2090–2106.
Wechsler, D. (1999). Wechsler abbreviated scale of intelligence (WASI). San Antonio: The Psychological Corporation.
Wechsler, D. (2004). Wechsler intelligence scale for children - fourth edition (WISC-IV). San Antonio: Pearson Assessments.
Wechsler, D. (2008). Wechsler adult intelligence scale - fourth edition (WAIS-IV). San Antonio: Pearson Assessments.
Weinstock, M. (2008). The long-term behavioural consequences of prenatal stress. Neuroscience & Biobehavioral Reviews, 32(6), 1073–1086.
Weisbrot, D. M., Charvet, L., Serafin, D., Milazzo, M., Preston, T., Cleary, R.,…Krupp, L. (2014). Psychiatric diagnoses and cognitive impairment in pediatric multiple sclerosis. Multiple Sclerosis, 20(5), 588–593.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
For this type of study, formal consent is not required.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Rights and permissions
About this article
Cite this article
Nunan-Saah, J., Posecion, L., Paulraj, S.R. et al. Executive Functioning in Pediatric Multiple Sclerosis: Considering the Impact of Emotional and Psychosocial Factors. J Pediatr Neuropsychol 3, 206–217 (2017). https://doi.org/10.1007/s40817-017-0033-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40817-017-0033-4