Abstract
Purpose of Review
In this manuscript, we will review core noncardiac medical management principles for the preterm infant with congenital heart disease (CHD). We describe common respiratory diseases of the newborn period, apnea of prematurity, the significance of thermoregulation, and management of hyperbilirubinemia. Taken together, these management considerations optimize neurodevelopment and growth of the infant with CHD while minimizing significant neonatal comorbidities.
Recent Findings
The comorbidities of prematurity affect both neonates with and without CHD. Respiratory distress syndrome can be a significant consequence of premature birth, and early surfactant administration is associated with decreased air leak, bronchopulmonary dysplasia (BPD), and mortality. If invasive mechanical ventilation is necessary, volume-targeted ventilation is preferred in preterm neonates with associated shorter duration of mechanical ventilation and decreased comorbidities. Recommendations for the management of hypoglycemia in infants exist, but are dependent on enteral feeding; thus, these recommendations may not be applicable to the neonate with CHD who cannot tolerate enteral feeding. Hypothermia is a common problem in premature infants and can result in high tissue oxygen demand and consumption with subsequent metabolic acidosis. Such effects can be exacerbated in the infant with CHD and may increase the risk for morbidities and mortality.
Summary
Though there have been many medical and surgical advancements in the care of preterm infants with CHD, the rates of morbidity and mortality remain high. Understanding key principles related to common complications of prematurity can be critical to improving long-term outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
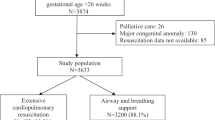
Congenital heart disease (CHD) is the most common birth defect in the newborn population. Infants with CHD are at significantly increased risk for premature delivery [1]. In infants without CHD, neonatal mortality typically decreases with each week of increasing gestational age; however, in premature infants with CHD, mortality remains high irrespective of gestational age [2]. Given the high burden of in-hospital mortality for preterm infants with CHD, it is important to understand significant sequelae of prematurity on both the cardiac and noncardiac systems. Paying close attention to key management considerations of the preterm infant may decrease common morbidities and improve overall neonatal outcomes (Fig. 1).
Respiratory distress syndrome of the newborn
Respiratory distress syndrome (RDS) is the most common pulmonary disease in the preterm neonatal period resulting in the need for assisted mechanical ventilation [3]. RDS occurs as a result of surfactant deficiency, which is either due to inadequate surfactant production or endogenous surfactant inactivation. Prematurity, lack of antenatal corticosteroids prior to preterm delivery, delivery without labor, and congenital surfactant deficiency are all factors which can limit adequate surfactant production in alveolar sacs. Meanwhile, surfactant inactivation can be seen in infants with meconium aspiration or infants of diabetic mothers.
The incidence of RDS significantly increases with the degree of prematurity. It occurs in 98% of infants born between 22 and 24 weeks gestation, 30% of infants between 28 and 34 weeks gestation, 10% of infants born at 34 weeks gestation, and only 0.3% of infants born at 39 weeks gestation [4,5,6]. RDS is a clinical diagnosis that develops shortly after birth. Classic signs include tachypnea, increased work of breathing, and progressive hypoxemia, coupled with radiographic findings of lung hypoexpansion, diffuse ground glass opacities, and air bronchograms on chest X-ray.
Surfactant deficiency results in increased surface tension throughout the pulmonary alveoli, which results in alveolar collapse [7]. This places infants at risk for diffuse lung atelectasis, impaired gas exchange, and barotrauma with positive pressure ventilation. Many neonates can be successfully managed with non-invasive respiratory support, but some may benefit from intubation and exogenous surfactant administration to reduce hypoxemia, pneumothorax, and severe respiratory failure that can result in death. Systematic reviews have demonstrated that early surfactant administration within the first 2 hours of life is associated with decreased air leak, bronchopulmonary dysplasia (BPD), and mortality [8••].
The lungs of preterm infants have poor compliance and low functional residual capacity (FRC) as a result of structural immaturity, innate surfactant deficiency, and a highly compliant chest wall [9]. To maintain FRC, optimize pulmonary gas exchange, and minimize the incidence of ventilator-associated lung injury, initiation of nasal continuous positive airway pressure (CPAP) is recommended immediately after birth. The goal of noninvasive positive pressure ventilation is to limit hypoxemia (in neonates without cyanotic heart disease, goal SpO2 90–95% with an FiO2 requirement < 50%), hypercarbia (goal PaCO2 45–65), work of breathing, and barotrauma (avoid high PEEP, for example no greater than 6–7 cm H2O in late preterm infants) [7, 10]. If this cannot be achieved with CPAP, then intubation and surfactant administration is recommended. Volume-targeted ventilation is associated with shorter duration of mechanical ventilation and decreased comorbidities in preterm infants and is the preferred mode of ventilation when possible [11••, 12]. Ventilator settings should target physiologic tidal volumes of 4–6 ml/kg titrated appropriately to avoid high peak inspiratory pressures (generally PIP > 25), a sufficient PEEP to maintain FRC and adequate oxygenation, respiratory rates 30–60 breaths per minute, and short inspiratory times of 0.3–0.35 s [10].
RDS in a premature neonate with cyanotic heart disease or single ventricle physiology poses additional complexities in management. For example, in the premature neonate with single ventricle physiology, the ratio of pulmonary and systemic blood flow (Qp:Qs) must be balanced. Estimates of shunt fraction are made via oximetry (arterial and mixed venous saturation, with the assumption of pulmonary vein saturation). However, in the premature neonate with RDS who presents with pulmonary vein desaturation due to poor pulmonary gas exchange, accurate estimation of shunt fraction via oximetry cannot be achieved without an invasive measure of pulmonary vein saturation. Moreover, in the premature single ventricle neonate with RDS, pulmonary vein desaturation will contribute to significant systemic hypoxemia due to the mixing of atrial blood.
Apnea of prematurity
Apnea of prematurity (AOP) commonly occurs in preterm infants, and its incidence is inversely correlated with gestational age and birth weight. Nearly all infants with birth weight < 1000 g and gestational age < 28 weeks experience AOP. Rates drop to 85% at 30 weeks gestation and to 20% at 34 weeks gestation [13]. Apnea is defined as a pause in breathing for > 20 seconds or a pause of > 10 seconds that is associated with bradycardia (heart rate < 100 beats per minute) and oxygen desaturation events [14]. AOP is a limited disease process which resolves over time as the preterm infant matures. In most cases, resolution occurs by 36 weeks postmenstrual age [15].
Apnea can be categorized as central, obstructive, or mixed. Central apnea involves a cessation of breathing due to insufficient respiratory drive in the central nervous system (CNS). It can result from developmental immaturity, CNS injury including intracranial hemorrhage and hypoxic-ischemic encephalopathy, seizures, medication use (magnesium sulfate, opiates, benzodiazepines, and barbiturates), and hypoxia triggering respiratory depression [16]. Obstructive apnea occurs as a result of airway obstruction, generally from immature pharyngeal tissue, hypotonic airways, nasal occlusion or laryngospasms. Mixed apnea results from a combination of central and obstructive processes and comprises the majority of apneic episodes in preterm infants [13].
If left untreated, AOP can have significant long-term impacts on neurodevelopment, retinopathy of prematurity (ROP), BPD, and infant mortality. This is thought to be related to the cumulative effects of chronic, intermittent hypoxia that occurs over time as a result of desaturation events secondary to apnea [14]. While many studies have demonstrated a signal for worse neurodevelopmental outcomes with prolonged hypoxemia and apnea, a causative link remains unclear since prematurity and other associated comorbidities also contribute significantly to neurodevelopmental outcomes. Though preterm infants are at increased risk for sudden infant death syndrome (SIDS), AOP does not increase the risk of SIDS in early infancy. This is because AOP generally resolves before the postmenstrual age that SIDS occurs. The average age of SIDS in preterm and term infants is 47 weeks and 53 weeks postmenstrual age, respectively, and AOP usually resolves before term-corrected gestational age [13].
Methylxanthines are the pharmacologic mainstay of therapy for AOP. Caffeine is specifically the methylxanthine of choice because of its more potent central nervous system effects, wide therapeutic index, low risk for toxicity, and longer half-life [17]. Caffeine stimulates the medullary respiratory centers, increases sensitivity to carbon dioxide, and enhances diaphragmatic function. Cumulatively, its effects increase minute ventilation and reduce hypoxic respiratory depression, limiting the occurrence of apnea [18]. There is currently no standardized consensus on dosing or duration for caffeine therapy. Initial studies on caffeine use in preterm infants for AOP were performed with a loading dose of 20 mg/kg and maintenance doses of 5 mg/kg/day [19•]. Subsequent studies confirmed that higher maintenance doses of 10 mg/kg/day were safe to use for prolonged periods of time [20]. As such, a single 20 mg/kg loading dose followed by maintenance doses of 5–10 mg/kg/day is now widely accepted as common practice. If infants continue to experience apneic episodes on lower doses of daily maintenance therapy, providers may give a mini loading dose of 10 mg/kg caffeine followed by uptitration of the maintenance dose. Since the incidence of AOP is low after 34 weeks with general resolution by 36 weeks, caffeine therapy is generally discontinued within this time frame [21]. Providers should monitor infants closely for apneic episodes and ensure infants are event-free after discontinuation of therapy. Given the long half-life of caffeine, infants are typically monitored for 5–8 days after caffeine cessation to ensure the drug is completely metabolized and cleared. If apnea persists after 36 weeks gestation, alternate causes of apnea should be explored.
Caffeine not only reduces the occurrence of apnea, but has been shown to decrease the incidence of BPD in the preterm population and the length of time on ventilatory support [22]. The importance of this finding cannot be emphasized enough as currently, there are no other treatments known to decrease rates of BPD among neonates.
AOP can be complicated and/or exacerbated by the use of alprostadil infusions in premature neonates with CHD that are ductal dependent for either systemic or pulmonary blood flow. Alprostadil is known to cause apnea (but with decreased incidence in lower doses) such that neonates with ductal-dependent lesions may often require mechanical ventilation for apnea. [23, 24] The alprostadil-associated apnea may be difficult to differentiate from AOP. Nevertheless, it is important to acknowledge that the incidence of AOP is low beyond 34 weeks and, therefore, apnea in a neonate greater than 34 weeks with ductal-dependent CHD is more likely the result of alprostadil, rather than AOP.
Hypoglycemia
Hypoglycemia is a common metabolic derangement that occurs in the neonatal period. All infants—from healthy term infants to sick preterm infants—experience a drop blood glucose concentrations after birth as a part of normal physiologic transition from the intrauterine to extrauterine environment [25]. In utero, the fetus receives a steady supply of glucose from the placenta. After birth, the umbilical cord is clamped, and the infant no longer receives a continuous exogenous supply of glucose. This results in a transient and often asymptomatic period of hypoglycemia for most infants during the first 24–48 hours of life [26•]. The physiologic nadir is generally observed around 2–3 h after birth with serum glucose levels declining as low as 20–30 mg/dL [27, 28]. This triggers the release of key regulatory hormones that are responsible for gluconeogenesis such as catecholamines, glucagon, and corticosteroids [29]. This helps regulate and maintain euglycemia in the neonate.
A subset of infants are at risk for prolonged hypoglycemia, which is generally defined as hypoglycemia that persists past 72 h of age. Neonatal hypoglycemia is most commonly seen in infants who are small for gestational age (SGA) or who have intrauterine growth restriction (IGUR), infants of diabetic mothers (IDM), infants who are large for gestational age (LGA), premature infants, and infants with perinatal stress [28]. SGA and IUGR infants have decreased glycogen stores and less adipose tissue for glucose storage, decreasing their ability to produce endogenous glucose via gluconeogenesis after birth [25]. IDM are exposed to prolonged hyperglycemia in utero as glucose crosses the placenta. This results in increased insulin production which persists after birth, resulting in an overall hyperinsulinemic state [30]. As insulin lowers blood glucose levels, hyperinsulinism results in hypoglycemia. Prematurity predisposes neonates to develop hypoglycemia due to limited glycogen and fat stores, poor gluconeogenesis pathways, increased metabolic demands and peripheral glucose utilization, and immature counter-regulatory responses to hypoglycemia [29]. Infants who experience perinatal stress include those with fetal distress prior to birth, perinatal ischemia/hypoxia, maternal preeclampsia/eclampsia, sepsis, and hypothermia. Due increased metabolic demand after birth and a dysregulated insulin secretion pattern in response to perinatal stress (known as hypoglycemic hyperinsulinism), these infants experience prolonged neonatal hypoglycemia [25].
Despite its prevalence, there is little consensus on the definition of hypoglycemia in the neonate. The American Academy of Pediatrics (AAP) has arbitrarily defined hypoglycemia as a blood glucose value of less than 47 mg/dL (2.61 mmol/L) based on limited evidence regarding neurodevelopmental outcomes [26•, 28, 29, 31, 32]. Infants with risk factors for neonatal hypoglycemia should be screened in the first 1–2 h after birth with serial subsequent monitoring for the first 12–24 h of life, or until the hypoglycemia resolves. All infants with clinical symptoms of hypoglycemia should be screened, treated, and monitored closely. The most common signs include tremors, jitteriness, weak or high-pitched cry, tachypnea, apnea, cyanosis, seizures, lethargy, and hypotonia [28].
In asymptomatic infants at risk for hypoglycemia, the initial management is feeding initiation with maternal breast milk, donor breast milk or formula, depending on parental preference [33]. If normoglycemia is not attained or feeds cannot be initiated, then IV glucose should be administered with the goal of maintaining plasma glucose levels 40–50 mg/dL per the AAP [26•]. The Pediatric Endocrine Society recommends blood glucose levels of > 50 mg/dL in first 48 h and > 60 mg/dL thereafter [34]. IV glucose can be administered in a concentrated bolus or via a continuous infusion. Some studies have shown that dextrose boluses can worsen hypoglycemia by triggering a state of transient hyperinsulinism, thus favoring the use of continuous IV glucose infusions in treatment [35]. Providers should target an initial glucose infusion rate (GIR) of 6–8 mg/kg/min in preterm, low birth weight and SGA/IUGR infants, and a GIR of 4–6 mg/kg/min in term and IDM infants [29]. Figure 2 below provides a framework for screening and management of infants most at risk for neonatal hypoglycemia.
The association between hypoglycemia and poor neurodevelopmental outcomes is well documented which is why recognition and treatment of hypoglycemia is critical. Infants who present with seizures secondary to hypoglycemia are at risk for severe neurodevelopmental abnormalities, coma, or even death [26•]. Newborns with congenital hyperinsulinism or other genetic hypoglycemic disorders are at risk for permanent brain injury, especially if they experience prolonged hypoglycemia [31]. With regards to infants who experience transient hypoglycemia after birth, some studies have shown decreased academic achievement in childhood [36], and others have shown increased risk of low executive function and visual-motor impairment [37], but these long-term outcomes have not been validated in more recent studies [38, 39]. Thus, further studies are needed to determine the relationship between transient neonatal hypoglycemia and impaired neurodevelopment.
The management of hypoglycemia in premature neonates with CHD may pose additional difficulties if either (1) the patient is unable to tolerate enteral feedings or (2) there is concern for systemic tissue oxygen delivery and intestinal blood flow related to restricted systemic blood flow. The AAP guidelines for the management of hypoglycemia focus primarily on oral feeding; however, the complexities of infants with critical CHD may require an emphasis on intravenous glucose supplementation or prolonged enteral tube feeding via a nasogastric or transpyloric tube.
Hypothermia
Per the World Health Organization, the normal core temperature for neonates should be 36.5–37.5 °C. Therefore, hypothermia is defined as a body temperature below 36.5 °C [40]. Preterm infants are at high risk for hypothermia due to a large surface area-to-weight ratio, evaporative heat loss with skin immaturity, low intrinsic fat stores, and immature hypothalamic function resulting in abnormal thermoregulation [5]. Hypothermia is a common complication among preterm infants, and multiple studies have demonstrated a prevalence of more than 50% during initial hospitalization [41, 42].
Hypothermia is a significant cause of morbidity and mortality among premature infants. There is a clear dose–response relationship between the degree of hypothermia and the risk of mortality [40]. Risk factors for hypothermia in the neonate include maternal hypertension, maternal hypothermia, chorioamnionitis, prolonged rupture of membranes, low 5-min APGAR score, low birth weight, prematurity, respiratory distress syndrome, perinatal hypoxia, and need for resuscitation at birth [43, 44]. Given the numerous risk factors, high prevalence, and high mortality associated with hypothermia, thermoprotective strategies have been implemented in the initial resuscitation of the preterm infant per the Neonatal Resuscitation Program (NRP) to minimize the occurrence of hypothermia. This includes wrapping the infant in a plastic bag without drying, use of a thermal mattress and radiant warmer, increasing delivery room temperature, and immediate placement of a hat for all infants less than 32 weeks gestation [45, 46].
Medical comorbidities associated with hypothermia are significant. Hypothermia delays the normal transition from fetal to neonatal circulation and triggers a hypermetabolic state that breaks down brown fat stores to create heat and maintain body temperature. This results in high oxygen tissue and nutrient consumption, metabolic acidosis, hypoglycemia, and additional fluid and electrolyte imbalances that can lead to multiorgan dysfunction and even death [47, 48••]. Hypothermia is also associated with a series of adverse clinical outcomes including sepsis, coagulopathy, hypotension and shock, and intraventricular hemorrhage (IVH) [49, 50]. Hypothermia can often be the initial presenting symptom of severe illness in the neonate—specifically infections including pneumonia, meningitis, and sepsis. Thorough examination and workup are absolutely critical if new hypothermia develops, or infants are not able to maintain their core temperature despite adequate growth and development.
Hyperbilirubinemia
Neonatal hyperbilirubinemia is very common and occurs in approximately 80% of all newborn infants. Hyperbilirubinemia is more likely to occur with increasing degree of prematurity. For example, late preterm infants are two times more likely than term infants to develop hyperbilirubinemia requiring treatment and are likely to have more prolonged bilirubin level elevations with higher peak concentrations [51]. Hyperbilirubinemia clinically presents with jaundice which refers to a yellowish discoloration of the skin, sclera, and mucous membranes.
When assessing an infant with hyperbilirubinemia, it is important to distinguish whether the jaundice is physiologic or pathologic. This distinction is key to guiding the urgency of treatment and further workup. Jaundice should be considered pathological if any of the following criteria are met [52]:
-
Elevated total serum bilirubin (TsB) in the first 24 h of life
-
TsB is greater than 95%ile based on age-specific bilirubin normograms
-
Rate of rise in TsB by more than 5 mg/dL/day or more than 0.2 mg/dL/h
-
Jaundice persists past 2 weeks in full term infants
-
Conjugated hyperbilirubinemia is present (direct bilirubin level > 1.0 mg/dL if TsB is ≤ 5.0 mg/dL OR direct bilirubin level > 20% of TsB)
Causes of unconjugated pathologic hyperbilirubinemia include immune-mediated hemolytic disease due to ABO or Rh incompatibility or non-immune-mediated hemolysis from RBC membrane or enzyme defects. Significant hemorrhage at birth (subgaleal hemorrhage or intracranial hemorrhage) or trauma at birth (cephalohematoma or extensive bruising) can also result in significant hyperbilirubinemia. In rare cases, genetic syndromes, such as Crigler-Najjar and Gilbert syndrome, that cause enzymatic defects impairing bilirubin clearance will result in pathologic unconjugated hyperbilirubinemia [53]. Conjugated hyperbilirubinemia is always a reflection of cholestatic disease and signals impaired hepatobiliary function in the neonate [54].
Physiologic jaundice accounts for nearly 75% of neonatal hyperbilirubinemia cases and is extremely common. Unconjugated bilirubin levels generally peak by 48–96 h of age with resolution of hyperbilirubinemia by 2 weeks of life [53]. The etiology for physiologic jaundice is multifactorial, and its occurrence is transient and limited to the neonatal period. Neonates have larger red blood cell (RBC) mass and shorter RBC life spans. Bilirubin is produced from the breakdown of fetal hemoglobin after birth, contributing to hyperbilirubinemia. The clearance of bilirubin is also immature after birth due to delayed maturation of the liver enzyme needed to conjugate bilirubin to make it water-soluble for excretion. Infants also have increased enterohepatic circulation which allows bilirubin to be reabsorbed from the small intestine instead of being excreted [55]. Among premature infants or sick term infants who have delayed enteral feeding, the process of increased enterohepatic circulation is worsened and results in more prolonged hyperbilirubinemia. This is important for providers to understand so they can properly identify which infants warrant more frequent screening and potential need for phototherapy.
Screening infants for hyperbilirubinemia is important due to the damaging effects of unconjugated bilirubin on the central nervous system. Unconjugated bilirubin is not bound to albumin in the serum and can freely cross the blood brain barrier. It can then deposit in multiple structures of the brain and cause bilirubin-induced neurological dysfunction (BIND) which can lead to bilirubin encephalopathy or kernicterus [5, 56]. Phototherapy and exchange transfusions—the mainstays of therapy for unconjugated hyperbilirubinemia—both facilitate the removal of unconjugated bilirubin from the serum, thus decreasing the risk for BIND. Phototherapy has been shown to routinely decrease TsB levels that would result in escalation of care and reduce the need for exchange transfusions [52, 57]. The thresholds for phototherapy recommended by the AAP are far below the levels at which there is a risk for bilirubin neurotoxicity, making it a safe and effective form of treatment for a common neonatal disease.
The evaluation and management of hyperbilirubinemia applies to all neonates, including those with CHD. However, specific attention should be directed at the evaluation of hyperbilirubinemia in the CHD patient who is not planned for immediate post-natal neonatal surgery. In neonates who proceed to congenital heart surgery in the first week of life, the need for phototherapy may be obviated by the use of cardiopulmonary bypass which, in effect, results in total exchange transfusion via the blood priming, red blood cell recovery methods, and ultrafiltration performed during cardiopulmonary bypass.
Conclusions
Prematurity adds significant complexity and risk for noncardiac complications in neonates with CHD. Management of respiratory diseases, apnea of prematurity, thermoregulation, and hyperbilirubinemia are specialized in premature infants, further adding complexity. It is important to understand how these problems are managed, as standard, in premature neonates but, also, important to understand how these management issues are affected by CHD (Fig. 1). Understanding these key therapeutic principles may be critical in improving the long-term outcomes of premature neonates with CHD.
Data Availability
No datasets were generated or analysed during the current study.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Reddy RK, McVadon DH, Zyblewski SC, Rajab TK, Diego E, Southgate WM, et al. Prematurity and congenital heart disease: a contemporary review. NeoReviews. 2022;23(7):e472–85.
Norman M, Håkansson S, Kusuda S, Vento M, Lehtonen L, Reichman B, et al. Neonatal outcomes in very preterm infants with severe congenital heart defects: an international cohort study. J Am Heart Assoc. 2020;9(5):e015369.
Clark RH. The epidemiology of respiratory failure in neonates born at an estimated gestational age of 34 weeks or more. J Perinatol. 2005;25(4):251–7.
Ekhaguere OA, Okonkwo IR, Batra M, Hedstrom AB. Respiratory distress syndrome management in resource limited settings-current evidence and opportunities in 2022. Front Pediatr. 2022;10: 961509.
Karnati S, Kollikonda S, Abu-Shaweesh J. Late preterm infants - changing trends and continuing challenges. Int J Pediatr Adolesc Med. 2020;7(1):36–44.
Htun ZT, Hairston JC, Gyamfi-Bannerman C, Marasch J, Duarte Ribeiro AP. Antenatal corticosteroids: extending the practice for late-preterm and scheduled early-term deliveries? Children. 2021;8(4):272. https://doi.org/10.3390/children8040272.
Yadav S, Lee B, Kamity R. Neonatal respiratory distress syndrome. StatPearls Publishing; 2023.
•• Ng EH, Shah V. Guidelines for surfactant replacement therapy in neonates. Paediatr Child Health. 2021;26(1):35–49. Systematic review demonstrates early surfactant administration within the first 2 hours of life is associated with decreased air leak, bronchopulmonary dysplasia (BPD), and mortality.
Schmolzer GM, Kumar M, Pichler G, Aziz K, O’Reilly M, Cheung PY. Non-invasive versus invasive respiratory support in preterm infants at birth: systematic review and meta-analysis. Centre for Reviews and Dissemination (UK); 2013.
Bronicki RA, Benitz WE, Buckley JR, Yarlagadda VV, Porta NFM, Aganga DO, et al. Respiratory care for neonates with congenital heart disease. Pediatrics. 2022;150(Supplement 2):e2022056415H.
•• Klingenberg C, Wheeler KI, McCallion N, Morley CJ, Davis PG. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst Rev. 2017;10(10):CD003666. Volume-targeted ventilation is associated with shorter duration of mechanical ventilation and decreased comorbidities in preterm infants and is the preferred mode of ventilation when possible.
Peng W, Zhu H, Shi H, Liu E. Volume-targeted ventilation is more suitable than pressure-limited ventilation for preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2014;99(2):F158–65.
Eichenwald EC, Watterberg KL, Aucott S, Benitz WE, Cummings JJ, Goldsmith J, et al. Apnea of prematurity. Pediatrics. 2016;137(1):e20153757.
Williamson M, Poorun R, Hartley C. Apnoea of prematurity and neurodevelopmental outcomes: current understanding and future prospects for research. Front Pediatr. 2021;9:755677.
Pergolizzi J, Kraus A, Magnusson P, Breve F, Mitchell K, Raffa R, et al. Treating apnea of prematurity. Cureus. 2022;14(1):e21783.
Zhao J, Gonzalez F, Mu D. Apnea of prematurity: from cause to treatment. Eur J Pediatr. 2011;170(9):1097–105.
Henderson-Smart DJ, De Paoli AG. Methylxanthine treatment for apnoea in preterm infants. Cochrane Database Syst Rev. 2010;(12):CD000140.
Kumar VHS, Lipshultz SE. Caffeine and clinical outcomes in premature neonates. Children. 2019;6(11):118. https://doi.org/10.3390/children6110118.
• Moschino L, Zivanovic S, Hartley C, Trevisanuto D, Baraldi E, Roehr CC. Caffeine in preterm infants: where are we in 2020? ERJ Open Res. 2020;6(1). https://doi.org/10.1183/23120541.00330-2019. Review of the causes and management of apnea of prematurity.
Puia-Dumitrescu M, Smith PB, Zhao J, Soriano A, Payne EH, Harper B, et al. Dosing and Safety of off-label use of caffeine citrate in premature infants. J Pediatr. 2019;211:27-32.e1.
Abdel-Hady H, Nasef N, Shabaan AE, Nour I. Caffeine therapy in preterm infants. World J Clin Pediatr. 2015;4(4):81–93.
Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A, et al. Caffeine therapy for apnea of prematurity. N Engl J Med. 2006;354(20):2112–21.
Singh Y, Mikrou P. Use of prostaglandins in duct-dependent congenital heart conditions. Arch Dis Child Educ Pract Ed. 2018;103(3):137–40.
Ohara T, Ogata H, Fujiyama J, Murata Y, Abe J, Kakuta K, et al. Effects of prostaglandin E1 infusion in the pre-operative management of critical congenital heart disease. Tohoku J Exp Med. 1985;146(2):237–49.
Abramowski A, Ward R, Hamdan AH. Neonatal hypoglycemia. StatPearls Publishing; 2023.
• Thompson-Branch A, Havranek T. Neonatal hypoglycemia. Pediatr Rev. 2017;38(4):147–57. AAP recommendations on the management of infant hypoglycemia emphasize oral feeding as treatment; these recommendations may be of limited utility in the neonate with congenital heart disease who is not able to tolerate enteral feeding.
Güemes M, Rahman SA, Hussain K. What is a normal blood glucose? Arch Dis Child. 2016;101(6):569–74.
Committee on Fetus and Newborn, Adamkin DH. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics. 2011;127(3):575–9.
Sharma A, Davis A, Shekhawat PS. Hypoglycemia in the preterm neonate: etiopathogenesis, diagnosis, management and long-term outcomes. Transl Pediatr. 2017;6(4):335–48.
Stanescu A, Stoicescu SM. Neonatal hypoglycemia screening in newborns from diabetic mothers--arguments and controversies. J Med Life. 2014;7 Spec No. 3(Spec Iss 3):51–2.
Rozance PJ. Hypoglycemia in the newborn and neurodevelopmental outcomes in childhood. JAMA. 2022;327(12):1135–7.
Lucas A, Morley R, Cole TJ. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ. 1988;297(6659):1304–8.
Rozance PJ, Wolfsdorf JI. Hypoglycemia in the newborn. Pediatr Clin North Am. 2019;66(2):333–42.
Thornton PS, Stanley CA, De Leon DD, Harris D, Haymond MW, Hussain K, et al. Recommendations from the pediatric endocrine society for evaluation and management of persistent hypoglycemia in neonates, infants, and children. J Pediatr. 2015;167(2):238–45.
Kutamba E, Lubega S, Mugalu J, Ouma J, Mupere E. Dextrose boluses versus burette dextrose infusions in prevention of hypoglycemia among preterms admitted at Mulago Hospital: an open label randomized clinical trial. Afr Health Sci. 2014;14(3):502–9.
Kaiser JR, Bai S, Gibson N, Holland G, Lin TM, Swearingen CJ, et al. Association between transient newborn hypoglycemia and fourth-grade achievement test proficiency: a population-based study. JAMA Pediatr. 2015;169(10):913–21.
McKinlay CJD, Alsweiler JM, Anstice NS, Burakevych N, Chakraborty A, Chase JG, et al. Association of neonatal glycemia with neurodevelopmental outcomes at 4.5 years. JAMA Pediatr. 2017;171(10):972–83.
Shah R, Dai DWT, Alsweiler JM, Brown GTL, Geoffrey Chase J, Gamble GD, et al. Association of neonatal hypoglycemia with academic performance in mid-childhood. JAMA. 2022;327(12):1158–70.
Edwards T, Alsweiler JM, Crowther CA, Edlin R, Gamble GD, Hegarty JE, et al. Prophylactic oral dextrose gel and neurosensory impairment at 2-year follow-up of participants in the hPOD randomized trial. JAMA. 2022;327(12):1149–57.
Abiramalatha T, Ramaswamy VV, Bandyopadhyay T, Pullattayil AK, Thanigainathan S, Trevisanuto D, et al. Delivery room interventions for hypothermia in preterm neonates: a systematic review and network meta-analysis. JAMA Pediatr. 2021;175(9):e210775.
Bhatt DR, White R, Martin G, Van Marter LJ, Finer N, Goldsmith JP, et al. Transitional hypothermia in preterm newborns. Adv Neonatal Care. 2010;10(5 Suppl):S15–7.
Medoff Cooper B, Holditch-Davis D, Verklan MT, Fraser-Askin D, Lamp J, Santa-Donato A, et al. Newborn clinical outcomes of the AWHONN late preterm infant research-based practice project. J Obstet Gynecol Neonatal Nurs. 2012;41(6):774–85.
Dang R, Patel AI, Weng Y, Schroeder AR, Lee HC, Aby J, et al. Incidence of neonatal hypothermia in the newborn nursery and associated factors. JAMA Netw Open. 2023;6(8):e2331011.
Demtse AG, Pfister RE, Nigussie AK, McClure EM, Ferede YG, Tazu Bonger Z, et al. Hypothermia in preterm newborns: impact on survival. Glob Pediatr Health. 2020;7:2333794X20957655.
Ringer SA. Core concepts: thermoregulation in the newborn, part ii: prevention of aberrant body temperature. NeoReviews. 2013;14(5):e221–6.
Wyckoff MH, Wyllie J, Aziz K, de Almeida MF, Fabres JW, Fawke J, et al. Neonatal life support 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A156–87.
Miller SS, Lee HC, Gould JB. Hypothermia in very low birth weight infants: distribution, risk factors and outcomes. J Perinatol. 2011;31(Suppl 1):S49-56.
•• Ting JY, Synnes AR, Lee SK, Shah PS, Canadian Neonatal Network and Canadian Neonatal Follow-Up Network. Association of admission temperature and death or adverse neurodevelopmental outcomes in extremely low-gestational age neonates. J Perinatol. 2018;38(7):844–9. Hypothermia triggers a hypermetabolic state to break down brown fat stores to create heat and maintain body temperature. This results in high oxygen tissue and nutrient consumption, metabolic acidosis, hypoglycemia, and additional fluid and electrolyte imbalances that can lead to multiorgan dysfunction and even death.
Mank A, van Zanten HA, Meyer MP, Pauws S, Lopriore E, Te Pas AB. Hypothermia in preterm infants in the first hours after birth: occurrence, course and risk factors. PLoS ONE. 2016;11(11):e0164817.
Liu H, Li J, Guo J, Shi Y, Wang L. A prediction nomogram for neonatal acute respiratory distress syndrome in late-preterm infants and full-term infants: a retrospective study. eClinicalMedicine. 2022;50:101523. https://doi.org/10.1016/j.eclinm.2022.101523.
Sarici SU, Serdar MA, Korkmaz A, Erdem G, Oran O, Tekinalp G, et al. Incidence, course, and prediction of hyperbilirubinemia in near-term and term newborns. Pediatrics. 2004;113(4):775–80.
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114(1):297–316.
Ansong-Assoku B, Shah SD, Adnan M, Ankola PA. Neonatal jaundice. Stat Pearls Publishing; 2023.
Fawaz R, Baumann U, Ekong U, Fischler B, Hadzic N, Mack CL, et al. Guideline for the evaluation of cholestatic jaundice in infants: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2017;64(1):154–68.
Mitra S, Rennie J. Neonatal jaundice: aetiology, diagnosis and treatment. Br J Hosp Med. 2017;78(12):699–704.
Shapiro SM. Definition of the clinical spectrum of kernicterus and bilirubin-induced neurologic dysfunction (BIND). J Perinatol. 2005;25(1):54–9.
Bhutani VK, Stark AR, Lazzeroni LC, Poland R, Gourley GR, Kazmierczak S, et al. Predischarge screening for severe neonatal hyperbilirubinemia identifies infants who need phototherapy. J Pediatr. 2013;162(3):477-482.e1.
Author information
Authors and Affiliations
Contributions
P.V. and J.K. both wrote the manuscript text and prepared the figures.
Corresponding author
Ethics declarations
Conflict of Interest
Pavika Varma declares that she has no conflict of interest. John S. Kim declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiology/CT Surgery
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Varma, P., Kim, J.S. Medical Management Considerations of Premature Infants with Congenital Heart Disease. Curr Treat Options Peds 10, 39–51 (2024). https://doi.org/10.1007/s40746-024-00294-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-024-00294-5