Abstract
Purpose of review
Clinical decision support systems (CDSS) are tools, ideally embedded within electronic health systems, that can facilitate clinicians utilizing best practices and individual patient data to improve outcomes. While various iterations of CDSS have existed for years (including on paper-based charting systems), the past decade has seen an explosion of these systems. This review highlights some recent trends in CDSS, including where improvement in patient outcomes was achieved, as well as areas where the benefits were not realized.
Recent findings
Overall, three categories of CDSS improving patient safety have been analyzed. These include reduction in adverse events relating to medications, helping facilitate antimicrobial stewardship, and the identification and treatment of pediatric sepsis. In each of these areas, CDSS has been generally shown to improve patient safety to varying degrees. Occasional studies have shown no improvement or worsening outcomes, although this is often due to poor training of clinicians with the technology rather than a flaw with the technology itself. Most CDSS research has been unable to show improvements in tangible outcomes such as mortality rates, but this is often secondary to the fact that these outcomes are rare in the pediatric context and thus showing improvements is challenging.
Summary
CDSS is a simple term to describe a heterogenous group of interventions, designed to improve patient care using technology. In this review, the evidence shows that it can improve adherence to antimicrobial guidelines, minimize medication errors, and improve identification of pediatric sepsis. Like any new system, when implemented cautiously, with ample time for education of staff and troubleshooting, it can improve patient safety; however, if not implemented with sufficient forethought, it may not improve safety and can indeed cause its own adverse events.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
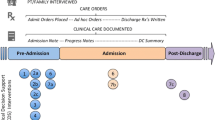
Clinical decision support systems (CDSSs) are information tools, ideally embedded within electronic health systems (EHS), designed to facilitate best clinical practices based on current standards and patient-specific data. Established by Bates and colleagues (2003), the “ten commandments” for effective clinical decision support outline the requirements of a computerized CDSS for it to be efficacious [1], especially considering changes and improvements in medical diagnostics and therapeutics. Ramnarayan and Britto broke down functions of CDSS into eight use cases: alert, diagnosis, reminder, suggestion, interpretation, prediction, critique, and assistance [2] (see Table 1, adapted from their work).
CDSS has been often cited as a facilitator of improved patient safety, especially in the pediatric context [3]. Weight-based medication-dosing errors, and delayed recognition and treatment of sepsis are common areas of practice where CDSS promises to improve pediatric patient outcomes. In this paper, we will review the evidence supporting the integration of CDSS in the pediatric population. Focusing on improvements in the ordering and prescribing of medication, proper antimicrobial usage and stewardship, reduction of adverse events, and superior prediction and detection in sepsis, we will argue that there is supporting evidence to recommend the thoughtful development, integration, testing, and continuing evaluation of CDSS in the pediatric context to improve patient safety.
Computerized physician order entry, CDSS, and adverse events
The provision and prescribing of improper medication can result in adverse outcomes in children. Woods et al. (2005) reported a rate of 1% in adverse events, representing over a thousand patients in their retrospective analysis [4]. However, adverse events as result of medication errors have been reported as high as 10% when the focus is specifically on outpatient and discharged patients [5]. Due to their small body habitus and unique physiology, neonates are particularly susceptible to medication errors when compared with larger children and adults.
In the pursuit of improving outcomes for the pediatric population, it must be identified where it is possible for CDSS to appropriately fit into the workflow. It is also imperative to assess what additional utility CDSS brings to clinical encounters, especially in environments already using CPOE (computerized physician order entry). Typically, CPOE systems are implemented preceding that of CDSS tools. CPOE at the most basic level enables a consistent ordering workflow and prescription formatting preventing common errors such as insufficient information or illegibility as seen with handwritten prescriptions [6]. The further integration of CDSS into CPOE can alert the user to further medication dosing considerations and possible “drug-drug” interactions.
A systematic review by Van Rosse and colleagues (2009) assessed the potential of CPOE systems to reduce adverse events, independent of CDSS. However, a nonsignificant and heterogeneously distributed reduction in adverse drug events was observed leading to the notion that overall mortality is not affected by the use of CPOE. Although CPOE lowers the rate of errors specific to medication prescriptions, to what effect this has on adverse events and therefore improvements in patient safety and better clinical outcomes is not conclusive [7]. One study by Upperman et al. (2005) demonstrated no change in the rate of potential adverse drug events following the implementation of CPOE in the Children’s Hospital of Pittsburgh. Yet when the results were stratified in categories attributing to an outcome of patient harm or no harm, it was found that there was a substantial decrease in the incidence of harmful adverse drug events despite no significant change in total adverse drug events [8].
There is controversial evidence that the introduction of CPOE into the workflow can paradoxically increase mortality in the pediatric ICU [9]. However, upon criticism by Van Rosse et al. (2009), several factors leading to this singular increase in mortality were highlighted including issues with patient registration, increased time to enter orders, drug relocation, technical difficulties and network compatibility, and a potential reduction in verbal interactions among the health care team. Other studies conducted in pediatric critical care, but in different tertiary care facilities and with longer post implementation analysis periods, found mortality rates unchanged [10, 11].
The additional impact of CDSS when introduced to environments operating with CPOE in the clinical workflow is best exemplified by Kadmon et al. (2009), in which the use of CPOE did not significantly reduce medication error rates and as a result, potential adverse events, until CDSS (specifically weight-based calculation adjustments) was incorporated [12]. The utility of CDSS is shown in this example in which even a limited decision support can improve outcomes more so than CPOE alone, but it remains critical that both systems are incorporated in a careful manner to provide optimal treatment to patients.
CDSS and medication dosing
The pediatric population is prone to medication errors along the entire prescribing continuum—from ordering and dispensing to administering and therapeutic monitoring. The majority of medication errors occur during the ordering phase of medication administration [13••] and there are several aspects of prescription ordering for children that contribute toward these errors. Dosing for all ages typically is based on standard weights but because of the dramatic differences in weight and surface area within pediatrics, errors are common. Medication errors have been reported to be three times higher in pediatrics compared with adults and account for 20% of all incident reports within single institutions [14]. In the USA, where a combination of imperial and standard measurements exists, the calculation of weight-based medications based off pounds instead of kilograms creates opportunity for misinterpretation and error [15]. Exact corrected gestational age may also play a role when considering the adjustment for neonates [16]. In addition, many medications are not licensed for pediatric use; formulations may not yet be available and therefore prescribing “off-label” is common for children [17].
The most common of medication errors are “10-fold” errors, which may happen during medication ordering or preparation/administration. These occur due to misplaced decimals, tailing zeroes, and illegible prescriptions [18]. Omitted or missed doses are the second most common medication error in pediatrics [19]—the rate of these errors has been reported in the literature from 2.4 to 13% of all doses scheduled [20]. The prevalence of these potential errors tends to be increased in the emergency department (ED) setting due to the fast-paced nature of clinical care and more limited opportunity for prescription monitoring or double checking by nurses or pharmacists [13••]. Medication error rates in the ED, as reported in a pediatric tertiary care network, range from 10 to 31% [13••].
The implementation of CDSS on medication dosing has had its share of successes and challenges. Following the conversion from written prescriptions to electronic prescribing with a basic CDSS in an acute tertiary care pediatric hospital in the UK, there was a reduction in dosing errors from 2.2 to 1.2% of all prescription orders [16]. Handwriting discrepancies and misinterpretation of dosing units (ex. micrograms and milligrams) were eliminated. In the outpatient and discharge patient units, potential serious adverse events as a result of medication errors were eliminated. Notably, the CDSS was relatively limited in this setting—without full weight-based dosing calculation or treatment recommendation. It was evident that the use of technological order-entry systems leads to better structure and eradicates the issue of illegibility, contributing significantly to the reduction in medication prescription errors.
While other examples of CDSS implementation with varying levels of functionality have reduced or fully eliminated prescriptions with insufficient or illegible information [6, 16], incorrect dosing calculations [13••, 21, 22], and dose omissions [6], these systems have also generated novel problems. Examples include mis-selection of prescription types in timing or frequency [16], and incorrect infusion rates or dosage options [6] selected from drop down menus. There is consensus in the literature that at this time, CDSS systems cannot reliably mitigate errors in knowledge, such as compensating for renal or hepatic impairment, and therefore the expertise of the physician and comprehension of the medical intervention are still critical [16]. This highlights an important reminder that these “tools” must be used as aids and not as replacements for critical thinking when making clinical decisions.
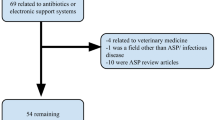
CDSS and antimicrobial stewardship
Antibiotic resistance is a recognized issue and antimicrobials are the most prescribed medicines in pediatrics with 37–61% of hospitalized patients receiving these medications. It has been estimated that 20–50% of these prescriptions are potentially unnecessary or inappropriate, leading to increased risks of antibiotic resistance, dosing toxicity, medication side effects, and a rise in health care costs [23•]. Antimicrobial stewardship (ASP) principles advocate for prescribing the optimal antibiotics when clinically indicated using the optimal dose, route, and duration to maximize patient outcomes and minimize resistance.
Clinical decision support has been identified as a potential tool to encourage ASP [24]. The implementation of a CDSS has been demonstrated by Webber et al. [24] to be rapidly integrated into the routine clinician workflow without significant disruption. Effective use of a CDSS relies on consultations with the health care professionals operating the system, as without consistent feedback to the technology design teams, interference in the workflow can manifest [24, 25].
The most common reason for prescribing antibiotics in children is to treat acute otitis media (AOM). A 2013 study investigating the capability of a CDSS found increased adherence to AOM guidelines, including optimal antibiotic selection, but there was no difference in total antibiotic prescribing [26]. It was postulated that CDSS does not effectively convince physicians to withhold treatment; rather, providers are more likely to adjust the selection or modify course based on the support. This is important as switching from broad spectrum antibiotics to more targeted therapies can reduce the probability of acquiring resistance.
This idea is reinforced by other studies such as those investigating acute respiratory illnesses (ARIs), when CDSS was incorporated into the workflow. Antibiotics are often inappropriately prescribed to treat ARIs in pediatrics considering most of these infections are viral, so it is of interest whether CDSS influence the overall prescribing of these medications as well as the preference for broad or narrow spectrum drugs. In a study of both adults and children, Mainous et al. (2013) identified a modest effect and no effect respectively on the inappropriate prescribing of antibiotics following CDSS implementation; however, there is a significant increase in the use of narrow spectrum antibiotics and resulting decrease in broad spectrum antibiotics in both groups [27]. Similar findings were highlighted by Litvin and colleagues (2013) as the intervention did alter the use of antibiotics for ARIs but dramatically reduced broad spectrum empiric treatments [28]. Notably, the heterogeneity in antibiotic prescription is a common theme and despite the use of CDSS with embedded standards and guidelines, providers are likely to be influenced by external factors such as patient concerns and expectations, as well as disagreement with when antibiotics are indicated or disputing guidelines on when narrow spectrum antibiotics should be first-line treatment.
The success of CDSS interventions is dependent on the incremental change in clinical practice from users, specifically the incorporation of CDSS into the workflow. Linder et al. (2009) failed to show any improvements in prescribing, but upon further analysis, it was found that only 6% of clinical encounters actually utilized CDSS [29]. In following other infectious diseases treated with antibiotics, the treatment of community-acquired pneumonia did not change in a study conducted in an Australian pediatric hospital [30]. The authors had commented on the treatment guidelines for uncomplicated pneumonia and the restricted nature in which broad spectrum antibiotics are used for this condition, and the use of CDSS did not further reduce the already-low rates of broad spectrum use. The emerging evidence supports the potential of CDSS systems to reduce health care costs and refine antimicrobial use, but careful implementation and accommodating user feedback are critical to preventing disruptions in the workflow.
CDSS and pediatric sepsis
Sepsis is a complex clinical syndrome with a definition that has evolved, most recently best classified in children the pediatric logistic organ dysfunction scale (PELOD-2). In terms of treatment, research has shown that the factors contributing to poor outcomes revolve around time to treatment or delay in therapy, and aggressiveness of fluid resuscitation and antibiotic administration [31•]. However, timely recognition of pediatric sepsis has proved to be more challenging than identifying septic adults, generally attributed to the fact that that many children present without hypotension (often in a state of compensated shock) [32•], making rapid identification more challenging.
Pediatric sepsis recognition tools and treatment protocols, especially those in the context of the emergency department, are associated with reduced time to initiation of antibiotics and fluid administration, thereby positively affecting outcomes such as overall length of stay and reducing morbidity and mortality [33,34,35]. The emergence of CDSS in the context of pediatric sepsis is worth evaluation for comparison with and combined with physician clinical judgment. In a study by Balamuth et al. (2016), physician judgment to detect sepsis had a higher specificity but lower sensitivity when compared with an algorithm alert based on relevant information entered [36]. When the methods were used together in which sepsis could only be ruled out if both methods were negative, the sensitivity was higher than any method alone. The authors then tested this in a more realistic fashion in which the physician would agree or refute the alert triggered by the decision support and found that through this sequential approach, specificity was higher than any other approach. The best practice considering these results is dependent on the priorities of a given institution. The practices resulting in higher sensitivity will ensure that cases are not missed.
Over the past few years, artificial intelligence and machine learning have taken off in the healthcare sector. A data-driven approach, utilizing advancements in machine learning, teaches a “neural network” to recognize symptomology along the spectrum of sepsis. This type of CDSS integrates data so that the criteria and classification rules are constructed by the algorithm itself using several informative inputs to not only indicate whether a patient is septic or not but also provide further stratification into sepsis, severe sepsis, or septic shock. This data has included new vital sign thresholds based off the pediatric SIRS [37], temperature with age-adjusted heart rate and respiratory rate integration [38], temperature and temporal blood cultures [39], and integration of temperature, desaturation, heart rate, respiratory rate, and bradycardia (RALIS) [40, 41]. CDSS incorporated with machine learning has demonstrated its superior performance over typical scoring scales [31•] and has demonstrated high sensitivity (~ 86%) and specificity (99%) in identifying pediatric sepsis [32•]. However, in this study, when clinician judgment and CDSS work in conjunction, sensitivity was augmented to 99% [36]. The utility of CDSS in identifying pediatric sepsis continues to be assessed, especially in practice where decision support is used to help guide educated clinical judgment. The incorporation of machine learning in this field may result in more refined criteria of which to accurate and efficiently clinically assess patients. However, considering these technologies are data-driven, and improved by individual-specific data, they function optimally in clinical settings with long records of comprehensive information such as the ICU.
Commentary and critique of CDSS
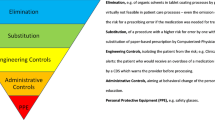
The utility of CDSS has been demonstrated in multiple clinical areas; however, it is imperative that users do not treat this tool as a panacea or utilize a “one-size-fits-all” model. There is data to suggest positive outcomes in outpatient and discharged patient groups, yet no significant change in the inpatient units [16]. The criticism facing CDSS integration into the discussed medical practices among others falls into the following categories: clinician education on the systems, health care team input in the creation of CDSS, and the prevalence of alert fatigue and subsequent excess of overriding.
The implementation of CDSS can reduce and even eliminate common errors in the realm of medication ordering, but in the process can introduce new problems not previously encountered. Computer errors ranging from incorrect selections on drop-down menus, duplicated orders, and order set/keypad entry errors are all common issues associated with CPOE and CDSS. The solution proposed to these situations typically follows that users are requested to be more careful and diligent (i.e., educational interventions); however, these are not reliable measures to ensure safety. Follow-up by the recipients of the orders is also recommended if conflict arises. This is especially critical in the presence of knowledge-based errors—problems that a CDSS system may not prevent but merely mitigate—so providers on both sides of the orders must remain diligent in the use of support tools.
A limiting factor in health care providers properly using CDSS is the varying level of familiarity with the respective software. Few examples in the literature reference specific training periods or introductory sessions as part of their methodology and when they do occur formally, only a single educational session is routinely mentioned [6, 9, 10]. This point was addressed in regard to other technologies like CPOE by Van Rosse et al. (2009), acknowledging that a single 2- to 4-h session is not enough time to become proficient with a system, especially in the instance where users were trained 3 months prior to implementation [9]. In some studies, there was an attempt to address this lack of training through the ambiguous notion that ongoing training will be provided as needed [6, 10]. This makes the comparison in physician proficiency between studies difficult.
One of the neglected aspects of implementation concerns the absence of health care professional insight in the initial designing of this technology. Through inclusion of the physicians, pharmacists, nurses, and other healthcare providers in the development of these technologies, fellow users will be more inclined to operating systems that are properly tailored to their profession.
Alert fatigue is a commonly cited frustration with CDSS systems. Alert fatigue can lead to the overriding of alerts and other functions within the CDSS and has been reported as high as 96% in extreme cases [13••]. Other studies have recorded lower overriding rates [22, 42, 43], but the pattern is still a concern and there has been debate weighing the abundance of false or unnecessary alerts against the alerts that cannot be missed and keep patients safe. “Misfires” are not the only reason for overriding though—the electronic rules or eRules set by the program software teams govern how and when alerts are triggered within a CDSS system. A study by Kirkendall and colleagues (2014) evaluated eRules through comparison with a gold standard of medication-dosing guidelines formed by an aggregate of five separate traditional and respected sources. In assessing the accuracy of the vendor-supplied rules, it was found that only one out of every two eRules lined up exactly with the gold standard dosing guidelines [44]. As previously noted, unique requirements for the pediatric population like weight-based dosing augment the complexity of care and therefore any tool used to support that care. This heterogeneity in medication prescription makes it difficult for program vendors of CDSS to align their software with the standards used in a particular clinic, again highlighting the vulnerabilities of the pediatric population. This emphasizes the importance of end-user feedback when designing, testing, and implementing CDSS systems in the pediatric context.
Conclusion
The use of CDSS in pediatric care has merit in supporting medication use, encouraging adherence to antibiotic guidelines, preventing adverse events, and detecting/predicting sepsis. As discussed, the potential of deleterious outcomes following the introduction of this support system is relatively small, but further investigation must continue to determine benefits in specific settings. CDSS systems rely upon a base of an EHR with CPOE, and end-user familiarity with any given system. It must be emphasized that CDSS is not a replacement for physician knowledge or clinical judgment but, as seen in the realms of medical diagnosis and treatment discussed, is another tool in the clinician toolbox in order to conduct best clinical practices. Careful execution is critical when it comes to using CDSS in any medical encounter, with the overall goal of reducing adverse outcomes. Overall, CDSS can support patient safety efforts; however, it must be done with appropriate planning, resources, and evaluation frameworks in place.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, et al. Ten commandments for effective clinical decision support: making the ... J Am Med Informatics Assoc [Internet]. 2003;10(6):523–30. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12925543.
Ramnarayan P, Britto J. Paediatric clinical decision support systems. Arch Dis Child. 2002;87:361–2.
Lehmann CU, Kim GR. Computerized provider order entry and patient safety. Pediatr Clin N Am. 2006;53(6):1169–84.
Woods D, Thomas E, Holl J, Altman S, Brennan T. Adverse events and preventable adverse events in children. Pediatrics. 2005;115(1):155–60.
Impicciatore P, Choonara I, Clarkson A, Provasi D, Pandolfini C, Bonati M. Incidence of adverse drug reactions in paediatric in/out-patients: a systematic review and meta-analysis of prospective studies. Br J Clin Pharmacol. 2001;52(1):77–83.
Warrick C, Naik H, Avis S, Fletcher P, Franklin BD, Inwald D. A clinical information system reduces medication errors in paediatric intensive care. Intensive Care Med. 2011;37(4):691–4.
Van Rosse F, Maat B, Rademaker CMA, Van Vught AJ, Egberts ACG, Bollen CW. The effect of computerized physician order entry on medication prescription errors and clinical outcome in pediatric and intensive care: a systematic review. Pediatrics. 2009;123(4):1184–90.
Upperman JS, Staley P, Friend K, Neches W, Kazimer D, Benes J, et al. The impact of hospitalwide computerized physician order entry on medical errors in a pediatric hospital. J Pediatr Surg. 2005;40(1):57–9.
Han YY, Carcillo JA, Venkataraman ST, Clark RSB, Watson RS, Nguyen TC, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005;116(6):1506–12.
Del Beccaro MA, Jeffries HE, Eisenberg MA, Harry ED. Computerized provider order entry implementation: no association with increased mortality rates in an intensive care unit. Pediatrics. 2006;118(1):290–5.
Keene A, Ashton L, Shure D, Napoleone D, Katyal C, Bellin E. Mortality before and after initiation of a computerized physician order entry system in a critically ill pediatric population. Pediatr Crit Care Med. 2007;8(3):268–71.
Kadmon G, Bron-Harlev E, Nahum E, Schiller O, Haski G, Shonfeld T. Computerized order entry with limited decision support to prevent prescription errors in a PICU. Pediatrics. 2009;124(3):935–40.
•• Benjamin L, Frush K, Shaw K, Shook JE, Snow SK. Pediatric medication safety in the emergency department. Pediatrics. 2018;141(3) This review highlights the top areas of improvement in the care of children in the emergency department. The opportunities for improving medication safety focus on weight-based dosing, standardized dosing, the optimization of computerized physician order entry using clinical decision support, and enhancing training across all medical professions in the systematic dispensing and administering of medications in the ED.
Wong ICK, Wong LYL, Cranswick NE. Minimising medication errors in children. Arch Dis Child. 2009;94(2):161–4.
Shaw KN, Lillis KA, Ruddy RM, Mahajan P V., Lichenstein R, Olsen CS, Chamberlain JM, for the Pediatric Emergency Care Applied Research Network Reported medication events in a paediatric emergency research network: sharing to improve patient safety. Emerg Med J 2013;30(10):815–819.
Jani YH, Barber N, Wong ICK. Republished error management: paediatric dosing errors before and after electronic prescribing. Postgrad Med J. 2011;87(1030):565–8.
Conroy S, North C, Fox T, Haines L, Planner C, Erskine P, et al. Educational interventions to reduce prescribing errors. Arch Dis Child. 2008;93(4):313–5.
Wong ICK, Ghaleb MA, Franklin BD, Barber N. Incidence and nature of dosing errors in paediatric medications: a systematic review. Drug Saf. 2004;27(9):661–70.
Patient Safety Observatory. Safety in doses: medication safety incidents in the NHS. Natl Patient Saf Agency [Internet]. 2007;9–12. Available from: http://www.nrls.npsa.nhs.uk/resources/?EntryId45=59822
National Patient Safety Agency. Rapid response report NPSA/2010/RRR009: reducing harm from omitted and delayed medicines in hospital. 2010;(February):1–14.
Lehmann CU, Kim GR, Gujral R, Veltri MA, Clark JS, Miller MR. Decreasing errors in pediatric continuous intravenous infusions. Pediatr Crit Care Med. 2006;7(3):225–30.
Sethuraman U, Kannikeswaran N, Murray KP, Zidan MA, Chamberlain JM. Prescription errors before and after introduction of electronic medication alert system in a pediatric emergency department. Acad Emerg Med. 2015;22(6):714–9.
• Donà D, Barbieri E, Daverio M, Lundin R, Giaquinto C, Zaoutis T. et al.Implementation and impact of pediatric antimicrobial stewardship programs: a systematic scoping review. Antimicrob Resist Infect Control. 2020;9:3 This review assesses the implementation of pediatric antimicrobial stewardship programs and the associated improvements in health outcomes. Pediatric ASPs have a significant impact on antimicrobial use, healthcare cost, and antimicrobial resistance in both inpatient and outpatient settings. It continues to be of interest how more data collection and coordination between systems will lead to more precise effects on healthcare systems and as a result, patient care.
Webber EC, Warhurst HM, Smith SS, Cox EG, Crumby AS, Nichols KR. Conversion of a single-facility pediatric antimicrobial stewardship program to multi-facility application with computerized provider order entry and clinical decision support. Appl Clin Inform. 2013;4(4):556–68.
Hum RS, Cato K, Sheehan B, Patel S, Duchon J, DeLaMora P, et al. Developing clinical decision support within a commercial electronic health record system to improve antimicrobial prescribing in the neonatal ICU. Appl Clin Inform. 2014;5(2):368–87.
Forrest CB, Fiks AG, Bailey LC, Localio R, Grundmeier RW, Richards T, et al. Improving adherence to otitis media guidelines with clinical decision support and physician feedback. Pediatrics. 2013;131(4).
Mainous AG, Lambourne CA, Nietert PJ. Impact of a clinical decision support system on antibiotic prescribing for acute respiratory infections in primary care: quasi-experimental trial. J Am Med Inform Assoc. 2013;20(2):317–24.
Litvin CB, Ornstein SM, Wessell AM, Nemeth LS, Nietert PJ. Use of an electronic health record clinical decision support tool to improve antibiotic prescribing for acute respiratory infections: the ABX-TRIP study. J Gen Intern Med. 2013;28(6):810–6.
Linder JA, Schnipper JL, Tsurikova R, Yu T, Volk LA, Melnikas AJ, et al. Documentation-based clinical decision support to improve antibiotic prescribing for acute respiratory infections in primary care: a cluster randomised controlled trial. Inform Prim Care. 2009;17(4):231–40.
Mostaghim M, Snelling T, McMullan B, Ewe YH, Bajorek B. Impact of clinical decision support on empirical antibiotic prescribing for children with community-acquired pneumonia. J Paediatr Child Health. 2019;55(3):305–11.
• Le S, Hoffman J, Barton C, Fitzgerald JC, Allen A, Pellegrini E, et al. Pediatric severe sepsis prediction using machine learning. Front Pediatr. 2019;7(October):1–8 This study investigates the use of machine learning in detecting sepsis compared with traditional scoring methods and finds that the former demonstrates superior performance in predicting severe sepsis onset. The system utilizing machine learning performed superior to PELOD-2 at 1 and 4h pre-onset and superior to SIRS at 0, 1, and 4h pre-onset, and excelled in other metrics as well. The early identification and subsequent treatment of pediatric of sepsis is essential in improving patient outcomes.
• Das C, Lucia MS HK and TJ. Improving recognition of pediatric severe sepsis in the emergency department: contributions of a vital sign based electronic alert and bedside clinician identification. Ann Emerg Med. 2017;70(6):759–768.e2. This quality improvement intervention conducted in a pediatric ED evaluated the performance of a sepsis recognition process including an electronic sepsis alert and bedside assessment. The alert demonstrated good sensitivity and high specificity for severe sepsis and when clinician identification was integrated for the patients that were negative for an alert, sensitivity improved.
Weiss SL, Fitzgerald JC, Balamuth F, Alpern ER, Lavelle J, Chilutti M, et al. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med. 2014;42(11):2409–17.
Joe Brierley, MD, Joseph A. Carcillo, MD, Karen Choong, MD, Tim Cornell, MD, Allan DeCaen, MD, Andreas Deymann, MD, Allan Doctor, MD, Alan Davis, MD, John Duff, MD, Marc-Andre Dugas, MD, Alan Duncan, MD, Barry Evans, MD, Jonathan Feldman, MD, Kathryn Felm J. Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock Am Coll Crit Care Med 2015;40(2):1291–1296.
Davis AL, Carcillo JA, Aneja RK, Deymann AJ, Lin JC, Nguyen TC, et al. The American College of Critical Care Medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: executive summary. Pediatr Crit Care Med. 2017;18(9):884–90.
Balamuth F, Alpern ER, Grundmeier RW, Chilutti M, Weiss SL, Fitzherald JC, et al. Comparison of two sepsis recognition methods in a pediatric emergency department. Acad Emerg Med. 2015;22(11):1298–306.
Sepanski RJ, Godambe SA, Mangum CD, Bovat CS, Zaritsky AL, Shah SH. Designing a pediatric severe sepsis screening tool. Front Pediatr. 2014;2(JUN).
Cruz AT, Williams EA, Graf JM, Perry AM, Harbin DE, Wuestner ER, et al. Test characteristics of an automated age- and temperature-adjusted tachycardia alert in pediatric septic shock. Pediatr Emerg Care. 2012;28(9):889–94.
Vidrine RM, Zackoff M, Pfeiffer S, Paff Z, Seger B, Stalets E, et al. Predicting severe sepsis in the pediatric ICU. Pediatr Qual Saf. 2019;4(3):e155.
Mithal LB, Yogev R, Palac HL, Kaminsky D, Gur I, Mestan KK. Vital signs analysis algorithm detects inflammatory response in premature infants with late onset sepsis and necrotizing enterocolitis. Early Hum Dev. 2018;117(312):83–9.
Gur I, Markel G, Nave Y, Vainshtein I, Eisenkraft A, Riskin A. A mathematical algorithm for detection of late-onset sepsis in very-low birth weight infants: 2014;51:647–650.
Jani YH, Barber N, Wong ICK. Characteristics of clinical decision support alert overrides in an electronic prescribing system at a tertiary care paediatric hospital. Int J Pharm Pract. 2011;19(5):363–6.
Stultz JS, Nahata MC. Appropriateness of commercially available and partially customized medication dosing alerts among pediatric patients. J Am Med Inform Assoc. 2014;21(E2):35–42.
Kirkendall ES, Andrew Spooner S, Logan JR. Evaluating the accuracy of electronic pediatric drug dosing rules. J Am Med Inform Assoc. 2014;21(E2).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Patient Safety
Rights and permissions
About this article
Cite this article
Saddler, N., Harvey, G., Jessa, K. et al. Clinical Decision Support Systems: Opportunities in Pediatric Patient Safety. Curr Treat Options Peds 6, 325–335 (2020). https://doi.org/10.1007/s40746-020-00206-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-020-00206-3