Abstract
Purpose of review
Paediatric Early Warning Systems (PEWS) are used extensively in hospitals around the world in an attempt to recognise and respond to children who are at risk of harm from deterioration. Most systems are based on the ability of physiological measurements to predict future events. Evidence supporting their use however is limited especially for important measures such as death. This review seeks to examine history and experience of PEWS and to explore recent literature for ideas that would enhance existing PEWS and new concepts that might complement the goal of recognising and responding to deterioration in hospital.
Recent findings
The largest study of PEWS, the EPOCH trial published in 2018, did not demonstrate a benefit in reducing mortality or other key indicators, from the use of the Canadian Bedside PEWS. There were several flaws that raise questions about the validity of the study; however, it also raises important issues for discussion. There have been recent studies published that propose alternative approaches to identifying deterioration including improved situation awareness and better teamwork.
Summary
We propose that it is possible to recognise and respond to early signs of deterioration in a way that reduces important outcomes; however, this will require blended approaches that embrace the complexity of the task.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
“O chestnut tree, great rooted blossomer,
Are you the leaf, the blossom or the bole?
O body swayed to music, O brightening glance,
How can we know the dancer from the dance?”
Among School Children
W.B. Yeats
Introduction
For most children, admission to hospital is a step toward improvement and recovered wellness. Families expect hospital to be a safe place, providing the best chance of getting better and although this is the case for most children, it is not the case for all. Clinicians have long been aware that some children deteriorate following admission to hospital, even after treatment has been initiated and despite regular observations, assessment, and review. The unexpected clinical deterioration or death of a child in hospital has a devastating effect on families and healthcare staff and usually leads to the investigation of preceding events in the hope of learning about how to prevent such events recurring.
In 2008, a national review of child mortality in the UK found that one in five (and potentially one in two) children who die unexpectedly in hospital has identifiable features that, if recognised and addressed earlier, could have prevented their death [1,2,3]. It is not surprising that this report and others have called for better ways of recognising and responding to the signs known to precede deterioration and death. The features that have received most attention are the changes in physiological parameters such as cardiovascular observations (heart rate, blood pressure, and capillary refill), respiratory measures (rate, effort, oxygen usage), or behavioural indicators (conscious level). In 2005, modelled on experience from adult care, a report of the first Paediatric Early Warning Score (PEWS) was published [4]. The so-called Brighton PEWS gave values, weighted on severity, across cardiovascular, respiratory, and behavioural categories that combined to create a score. The score was then matched to a set response agreed by the local nursing and medical teams. Since then, there have been many versions of PEWS enacted and published across the world based on these same principles of recognition, decision, and response. Many studies have focused on specific aspects, such as the refinement of the recognition score (single trigger or composite, trigger thresholds) also known as a “paediatric track and trigger tools” (PTTT). Other studies have focused on the response side (rapid response teams—RRTs, ICU outreach). A trend in recent years has been to recognise the whole process, from recognition to response, as a paediatric early warning scoring system or simply a PEW system, referred to as PEWS from here on [5].
There have now been several excellent PEWS narrative reviews [6,7,8] and at least three systematic reviews [9,10,•–11]. Among the conclusions of these analyses is that while PEWS may facilitate the recognition of early signs of deterioration and may improve key processes such as team work or communication, there is limited data showing effect on outcomes such as a reduction in cardiac arrest or death. The reviews highlight the fact that there is significant heterogeneity between systems, scores, scoring and triggering mechanisms, responses, and contexts making comparisons and generalizations difficult. They all highlight methodological weaknesses and the fact that most studies are from single sites, usually tertiary children’s hospitals. They also recognise the fact that PEWS being a multifaceted, complex intervention is likely to have socio-technical and cultural factors that underpin its performance in different contexts that remain poorly understood.
Of all the PEWS systems studied, none has been more closely evaluated than the Canadian Bedside PEWS. Over the course of several studies, the Bedside PEWS was designed, tested, and implemented [12,13,14]. In each of these studies, the Bedside PEWS seemed to advance up the validation ladder creating an optimism that the final step, a large prospective international multicentre trial, would provide firm evidence of effectiveness and validate PEWS [15]. The Evaluating Processes of care and Outcomes of Children in Hospital (EPOCH) study was reported in March 2018 [16••]. The study compared the effect of implementing the Bedside PEWS at 10 children’s hospitals with that of 11 hospitals that continued to provide care as usual in 7 countries and included 539,443 patient days. The primary outcome was all-cause hospital mortality with secondary outcomes including late admission to PICU, cardiac arrest, and PICU resource use. No significant difference in mortality was observed between the intervention and the non-intervention sites. The findings, the authors conclude, “do not support the use of this system to reduce mortality”.
Understanding EPOCH
As the largest examination of PEWS to date, EPOCH raises serious queries, including whether early detection and meaningful response is even possible. For this reason, it is important to critically consider the lessons and the limitations of the study. We believe there are two significant areas, both acknowledged by the authors, which bring the study’s findings into question, namely, the use of death as the primary outcome measure and the failure to perform any socio-technical analysis of the intervention.
Several studies, including EPOCH, have used death as a measure of effectiveness. While death is an attractive measure because of its importance and objectivity, it is also problematic because it has become a rare event in modern paediatric hospital care. Even over the short time period from when the data for the EPOCH power calculations was obtained to the completion of the study, there was a significant decrease in death rates at the study hospitals leaving the study underpowered. In a recent editorial, Chapman et al. highlight the challenge of measuring the impact of PEWS [17]. Their analysis suggests that in order to detect a 10% relative risk reduction in death, a study would require > 2 million individually randomized paediatric admissions (there were 144,539 patients in EPOCH). This effectively excludes the use of death as a practical measure for validation, at least in the short to medium term, but it also casts significant doubt over EPOCH’s findings.
The second EPOCH limitation we believe is that despite recognising that “Bedside PEWS is a complex health care intervention…embedded in social systems”, there was no evaluation of “communication or culture”. Indeed, the EPOCH study is not alone in this respect with one systematic review highlighting that the majority of studies examining PEWS and RRTs fail to examine the context, social structures, or culture in which their interventions were imbedded [9•]. The absence of any socio-technical evaluation ignores the complexity of the intervention, considering it as merely technical and neglecting the direct social processes (team work, psychological safety, communication) needed to operate the tool but also the wider organisational and cultural matrix in which the PEWS exists.
How can we know the dancer from the dance?
These limitations cast doubt on the EPOCH conclusion; however, the study also raises important questions about the models we have used to conceptualise early detection and response. The creation of prediction tools by working backwards with the characteristics of children known to have deteriorated has failed to consider additional information that might enhance detection. This involves tuning in to the “soft” intelligence that passes between staff, patients, and families from moment to moment, but which is not necessarily noticed or captured at the time unless sought. Once we start working forwards, we can also see that the conceptual models need to acknowledge the multiple direct and indirect influences on the success of such complex interventions. These include not only team training and the design of tasks but also staffing levels, appropriate work environments, and organisational culture. This creates a PEWS pyramid of dependent parts that together is able to achieve the goal of early detection and response (Fig. 1).
All of this requires the adoption of a systems view of safety which has long been appreciated in other high-risk industries and which is increasingly recognised in healthcare [18]. It also requires a shift in how we conduct research that evaluates complex interventions, becoming comfortable with the messy relationships and fuzzy lines between an intervention and the world around it.
Below we examine some of the complementary and interdependent components of the upper part of the PEWS pyramid. An in-depth examination of the components in the base of the pyramid is beyond the scope of this article but well represented within the safety literature [19].
Situation awareness
Situation awareness (SA) is a familiar concept in patient safety science and its application is a feature of High Reliability Organisations (HROs) [20]. The focus is on what is happening now, gathering and analysing information, as once this is known then good decisions can be made to probe, anticipate, respond, or escalate. This is a different model of identifying risk from those usually considered in PEWS studies and although the signals of prediction are included, they are complemented by other features that help attract attention to the present and that ensure that all means of sensing and amplifying useful information are included.
Situation awareness has been central to efforts to reduce preventable adverse outcomes at Cincinnati Children’s Hospital [21]. In one study, the hospital identified several factors, in addition to the early warning score, that they believed increased the risk of deterioration or harm which included “family concerns, high-risk therapies, clinician gut feeling (a watcher), and communication” [22••]. Their key intervention, a thrice daily unit-based huddle, where risks could be identified early, escalated, and addressed, lead to a significant reduction in harm events. Huddles, also called safety briefings, are brief (< 15 min), routine, semi-structured meetings (usually standing) of healthcare staff to review and anticipate concerns and although the concept has come from high-risk industry, they have been extensively used and examined in healthcare [23].
The approach of improving SA through huddles has also been used in the UK and Ireland [24]. The clinical standards and quality improvement team in the Royal College of Paediatrics and Child Health (RCPCH) have introduced the S.A.F.E (Situation Awareness for Everyone) toolkit which is based on 4 years of learning from a large collaborative across 50 sites [25]. There is an ongoing evaluation of the impact of these interventions on several safety and quality outcomes including cardiac arrest and transfer to a higher level of care (e.g., PICU) as well as on patient and family experience [26]. There will also be an assessment of safety culture and an examination of the key team processes that contribute to the effectiveness of the huddle [27]. This is important because the Cincinnati experience demonstrated additional benefits to teams from regular huddles and working together to improve situation awareness [28, 29].
In these studies, it was observed that social, technological, and organisational inputs must combine to deliver improved SA. These findings strongly support the importance of non-technical skills in early detection of deterioration. Important too were the structured aspects of these non-technical skills such as standardised procedures to proactively identify, communicate, and plan for risk; the benefit of shared language; training to support handoffs; and continuity of care. Similar findings have been observed in efforts to improve clinical communication and handover [30]. All of these features combine to improve the efficiency of information sharing among staff, enhancing their sense of accountability and empowerment but they were also seen to strengthen the sense of community. Provost et al. in a review on the practice of huddling suggest that “huddles create time and space for conversations, enhance relationships among health care providers, and strengthen a culture of safety” [31].
Team training and human factors
One way to view the huddle is as a platform that provides the opportunity, time, and space for improved situation awareness and teamwork to occur. The research findings discussed above suggest that some of the benefit comes from simply bringing teams together for the purpose of improving safety. These studies have also identified additional team behaviours that seem to enhance this such as standard working, robust communication, and a good safety culture [27, 29]. These skills are often considered under the umbrella of team training. Most clinicians will have experienced piecemeal elements of team training within their professional groups (doctors with doctors, nurses with nurses); however, this input has been shown to be most effective when implemented as a bundled intervention that includes inter-disciplinary learning and the sustained use of teamwork practices in daily care [32]. Despite the potential synergy here, there is little evidence on the influence of specific team training on the successful application of PEWS although several bodies have called for its inclusion. The AHRQ’s (Agency for Healthcare Research and Quality, USA) TeamSTEPPS® programme [33] which offers a comprehensive team training in patient safety is recommended by the Irish PEWS National Clinical Guideline as a resource that would complement training in Ireland [34••]. A recent policy statement from the Canadian Paediatric Society has called for the optimisation of rapid response systems and teams through team training and organisational changes [35].
Despite the lack of evidence, calls for team training are reinforced by emerging literature on the barriers to effective PEWS implementation, many of which are identifying system design, communication, and human factors as key contributors. Several studies have used qualitative methods to explore the challenges of operating early warning systems. One study of nurses and physicians carried out at the Children’s Hospital of Philadelphia (CHOP) examined barriers to activating the hospital’s rapid response system identified a broad range of themes such as a lack of self-efficacy among less experienced staff, the difficulties of hierarchy, and concerns about the potential negative effects of transfer to the ICU [36]. Another study of parents and healthcare professionals from a hospital in Rome using the Bedside PEWS identified themes including staff competencies and skills; the impact of relationships and leadership; the processes identifying and responding to clinical deterioration; and the influences of organisational factors on the escalation of care [37]. All of these studies highlight the complexity of PEWS and the multitude of interacting factors that influence the outcome in addition to the track and trigger tool.
Human factor principles have been applied to the design of observation charts for early warning systems [38]. It is only recently however that human factors is being used to consider the entire process of recognition, decision, and response within the context that makes up an early warning system [39]. This perspective along with the application of tools such as the Systems Engineering Initiative for Patient Safety (SEIPS [40]) model of work system and patient safety is likely to provide new ideas for future PEWS [41].
The future of PEWS
We see the future of PEWS as the improvement and integration of three key processes with a deep appreciation of the system in which they exist (Fig. 2):
- 1)
Recognition (prediction tools and enhanced situation awareness)
- 2)
Decision (improved decision aides and team decision-making)
- 3)
Response (optimal response to (a) rescue and (b) evaluate and manage ongoing risk)
The emergence of affordable wearables for continuous monitoring combined with “big data” analytics will significantly improve the potential for prediction, situation awareness, and early recognition [42, 43]. The inclusion of additional clinical information from electronic records could personalize risk assessment and strengthen both recognition and decision-making functions [44]. These technological advances will only deliver provided they are fully integrated into human systems, with their dependence on communication and culture; otherwise, the volume of information could be overwhelming and end up being counterproductive [45].
The role of patients and families in PEWS needs to be evaluated further. In the Irish PEWS, we have included a low-level score (0 or 1) for parent or clinician concern. This ensures bedside staff engage with a parent or family to ask if there is anything worrying them in addition to the fact that their child is in hospital, every time that observations are taken. Communicating with families about their unique role is vital and is supported by good parent information [46]. Future research is needed to examine how best to optimize this essential partnership.
The black box of decision-making in PEWS needs to be explored. We believe there is much to learn from a better understanding of the balance between clinical judgement/autonomy and mandatory actions, including the potential influence of organisational cultures (Table 1) on these decisions. There is also a need to learn more about how risk is dealt with following activation of PEWS as most children will not require resuscitation or transfer to PICU, but many will have ongoing needs, and will continue to have derangements in physiological measures with elevated scores. The modification of parameters, thresholds, or responses is utilised in many PEWS models, but this function is not well examined.
Finally, we need to better understand response. Most of the research on PEWS and rapid response teams comes from Children’s Hospitals where it may be possible to resource a dedicated team. In smaller centres, however, it is likely that the responders will be from an on-call medical team with a different set of skills and response options. This research needs to examine the burden on hospitals, especially critical care facilities, of providing an early warning system as this is important for sustainability.
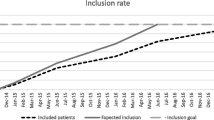
Research on these three processes needs to move in unison as too much of the learning has been from looking backwards, from known deterioration, rather than forwards. The Paediatrics Utilisation and Mortality Avoidance (PUMA) Study which is ongoing in UK is a novel study and the first of its kind to incorporate “a functions-based approach” with the aim of improving patient safety and reduction in mortality [47••]. This study aims to examine the messiness of designing, implementing, and improving a PEWS system in different settings, including paediatric wards in district general hospitals, through more organic approaches. These approaches, including quality improvement, are seeking to establish the structures and processes that support early detection of deterioration or safety rather than rigidly implementing standard components. This allows situation awareness, human factors, and team training to be used in addition to vital sign-based alerts if considered favourably by local teams. The study is underpinned by a number of theoretical frameworks to examine socio-technical factors and extract the learning needed to inform a national programme. The study is using mortality as an outcome; however, the research protocol openly acknowledges the fact that they may not have sufficient numbers to demonstrate an impact. In light of this, several other clinical outcomes are suggested including cardiac arrest and escalation to a higher level of care (PICU/HDU) as well as safety metrics. In due course, if a national programme for the UK is agreed and implemented, it may be possible to support the validation of PEWS by examining mortality data over time using routinely collected data [48].
Conclusion
Patient safety is often described as an emergent phenomenon, materializing from the actions and interactions of multiple components inside the complex system of healthcare [49]. What is also noted is the difficulty of predicting how change in one part of the system might influence another, or the whole. Recognising and responding to deterioration are a complex endeavour and were never likely to have a single or simple solution. Tools and technology have a significant contribution to make; however, they must enhance and integrate with the people and cultures that share the system. Utilisation of research and improvement methods that appreciate the complexity of the problem and the solutions are necessary to make progress. Seeking and blending learning from disciplines such as human factors, models such as SEIPS, or approaches such as Safety I (learning how come work goes wrong) and Safety II (learning how come work goes right) is required to meet the challenge of complexity [50•]. Finally, organisations and leaders much acknowledge that many of the critical success factors that address deterioration are shared with other safety and quality goals, such as reducing medication harm, improving handover or patient flow, and even enhancing patient and staff experience. Identifying and improving the essential behaviours and skills that underpin so many challenges could create a prize much greater than just improving the tragedy of preventable in hospital deterioration.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pearson GA. Why children die: a pilot study. London: CEMACH; 2008.
Confidential Enquiry into Maternal and Child Health (CEMACH). Why children die—a pilot study. London: CEMACH; 2008.
Wolfe I, Macfarlane A, Donkin A, et al. Why young children die: death in infants, children and young people in the UK Part A. Royal College of Paediatrics and Child Health, 2016.
Monaghan A. Detecting and managing deterioration in children. Paediatr Nurs. 2005;17:32–5.
Pearson G, Duncan H. Early warning systems for identifying sick children. Paediatr Child Health. 2011;21(5):230–3.
Roland D. Paediatric early warning systems: myths and muses. Paediatr Child Health. 2017;27(5):242–6.
Chapman SM, Maconochie IK. Early warning scores in paediatrics: an overview. Arch Dis Child. 2019;104(4):395–9. https://doi.org/10.1136/archdischild-2018-314807.
Chapman SM, Wray J, Oulton K, Pagel C, Ray S, Peters MJ. ‘The score matters’: wide variations in predictive performance of 18 paediatric track and trigger systems. Arch Dis Child. 2017;102:487–95.
• Lambert V, Matthews A, MacDonell R, et al. Paediatric early warning systems for detecting and responding to clinical deterioration in children: a systematic review. BMJ Open. 2017;7:e014497. Systematic Review highlighting the deficit of studies considering socio-technical and organizational aspects of PEWS.
Chapman SM, Wray J, Oulton K, Peters MJ. Systematic review of paediatric track and trigger systems for hospitalised children. Resuscitation. 2016;109:87–109.
Trubey R, Huang C, Lugg-Widger FV, Hood K, Allen D, Edwards D, et al. Validity and effectiveness of paediatric early warning systems and track and trigger tools for identifying and reducing clinical deterioration in hospitalised children: a systematic review. BMJ Open. 2019;9:e022105. https://doi.org/10.1136/bmjopen-2018-022105.
Parshuram CS, Hutchison J, Middaugh K. Development and initial validation of the Bedside Paediatric Early Warning System score. Crit Care. 2009;13(4):R135.
Parshuram CS, Bayliss A, Reimer J, Middaugh K, Blanchard N. Implementing the Bedside Paediatric Early Warning System in a community hospital: a prospective observational study. Paediatr Child Health. 2011;16(3):e18–22.
Parshuram CS, Duncan HP, Joffe AR, Farrell CA, Lacroix JR, Middaugh KL, et al. Multicentre validation of the bedside paediatric early warning system score: a severity of illness score to detect evolving critical illness in hospitalised children. Crit Care. 2011;15(4):R184. https://doi.org/10.1186/cc10337.
Parshuram CS, Dryden-Palmer K, Farrell C, et al. Evaluating processes of care and outcomes of children in hospital (EPOCH): study protocol for a randomized controlled trial. Trials. 2015;16:245.
•• Parshuram CS, et al. Canadian critical care trials group and the EPOCH investigators. Effect of a pediatric early warning system on all-cause mortality in hospitalized pediatric patients: the EPOCH randomized clinical trial. JAMA. 2018;319(10):1002–12. Large multisite randomised study comparing outcomes between sites using PEWS with sites providing usual care. Conclusion was that there was no effect on mortality. The study was under powered and failed to perform any socio-technical evaluation of the intervention bringing the conclusion into question however it raises important issues.
Chapman SM, Wray J, Oulton K, Peters MJ. ‘Death is not the answer’: the challenge of measuring the impact of early warning systems. Arch Dis Child. 2019;104:210–1.
Cheung R, Roland D, Lachman P. Reclaiming the systems approach to paediatric safety. Arch Dis Child. 2019:archdischild-2018-316401. https://doi.org/10.1136/archdischild-2018-316401.
Vincent C. Patient Safety. 2nd ed: BMJ Books, Wiley Blackwell; 2011.
Wickens CD. Situation awareness: review of Mica Endsley’s 1995 articles on situation awareness theory and measurement. Hum Factors. 2008;50(3):397–403.
Brady PW, Wheeler DS, et al. Situation awareness: a new model for predicting and preventing patient deterioration. Hosp Pediatrics. 2014;4:143.
•• Brady PW, Muething S, Kotagal U, et al. Improving situation awareness to reduce unrecognized clinical deterioration and serious safety events. Pediatrics. 2013;131(1):e298–308. https://doi.org/10.1542/peds.2012-1364. Study showing benefit of using huddles to improve situation awareness and teamwork leading to a reduction in inpatient deterioration.
Ryan S, Ward M, Vaughan D, et al. Do safety briefings improve patient safety in the acute hospital setting? A systematic review. J Adv Nurs. 2019. https://doi.org/10.1111/jan.13984.
SAFE—situation awareness for everyone programme, RCPCH. https://www.rcpch.ac.uk/resources/situation-awareness-everyone-safe-resource-introduction.
Stapley E, Sharples E, Lachman P, et al. Factors to consider in the introduction of huddles on clinical wards: perceptions of staff on the SAFE programme. Int J Qual Health Care. 2017:1–6.
Deighton J, Edbrooke-Childs J, Stapley E, Sevdalis N, Hayes J, Gondek D, et al. Realistic evaluation of situation awareness for everyone (SAFE) on paediatric wards: study protocol. BMJ Open. 2016;6:e014014.
Edbrooke-Childs J, Hayes J, Sharples E, Gondek D, Stapley E, Sevdalis N, et al. Development of the huddle observation tool for structured case management discussions to improve situation awareness on inpatient clinical wards. BMJ Qual Saf. 2018;27(5):365–72.
Goldenhar LM, Brady PW, Sutcliffe KM, Muething SE. Huddling for high reliability and situation awareness. BMJ Qual Saf. 2013;22:899–906.
Brady PW, Goldenhar LM. A qualitative study examining the influences on situation awareness and the identification, mitigation and escalation of recognised patient risk. BMJ Qual Saf. 2014;23:153–61.
Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–12. https://doi.org/10.1056/NEJMsa1405556.
Provost SM, Lanham HJ, Leykum LK, et al. Health care huddles: managing complexity to achieve high reliability. Health Care Manage Rev. 2015;40(1):2Y12.
Weaver SJ, Dy SM, Rosen MA. Team-training in healthcare: a narrative synthesis of the literature. BMJ Qual Saf. 2014;23:359–72.
TeamSTEPPS®, Agency for Healthcare Research and Quality (AHRQ), Rockville, MD. https://www.ahrq.gov/teamstepps/index.html (accessed May 20th 2019).
•• National Clinical Effectiveness Committee - National Guideline No. 12: The Irish Paediatric Early Warning System. https://health.gov.ie/wp-content/uploads/2017/02/NCG-12-PEWS-full-report-V21.pdf. The Irish national clinical guideline on PEWS produced using the GRADE framework. The guideline recommends the use of an early warning score in combination with enhanced family input, teamwork and increased situation awareness.
Cheng A, Mikrogianakis A. Canadian paediatric society position statement. Rapid response systems for paediatrics: suggestions for optimal organization and training. Paediatr Child Health. 2018;23:51–7.
Roberts KE, Bonafide CP, Weirich Paine C, et al. Response system barriers to calling for urgent assistance despite a comprehensive pediatric rapid response system. Am J Crit Care. 2014;23:223–9.
Gawronski O, Parshuram C, Cecchetti C, Tiozzo E, Ciofi degli Atti ML, Dall’Oglio I, et al. Qualitative study exploring factors influencing escalation of care of deteriorating children in a children’s hospital. BMJ Paediatr Open. 2018;2(1):e000241.
Christofidis MJ, Hill A, Horswill MS, Watson MO. A factors approach to observation chart design can trump health professionals’ prior chart experience. Resuscitation. 2013;84(5):657–65.
Lyons PG, Edelson DP, Churpek MM. Rapid response systems. Resuscitation. 2018;128:191–7.
Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56(11):1669–86.
Chua WL, See MTA, Legido-Quigley H, et al. Factors influencing the activation of the rapid response system for clinically deteriorating patients by frontline ward clinicians: a systematic review. Int J Qual Health Care. 2018;30(6):492.
Health Information and Quality Authority, Ireland. Health technology assessment of the use of information technology for early warning and clinical handover systems, 2015. https://www.hiqa.ie/sites/default/files/2017-01/HTA-of-use-of-information-technology-for-early-warning-and-clinical-handover-systems.pdf.
Halpern NA. Early warning systems for hospitalized pediatric patients. JAMA. 2018;319(10):981–2.
Rothman MJ, Tepas JJ 3rd, Nowalk AJ, et al. Development and validation of a continuously age-adjusted measure of patient condition for hospitalized children using the electronic medical record. J Biomed Inform. 2017;66:180–93.
Bonafide CP, Roland D, Brady PW. Rapid response systems 20 years later: new approaches, old challenges. JAMA Pediatr. 2016;170(8):729–30. https://doi.org/10.1001/jamapediatrics.2016.0398.
Shine 2012: Listening to you. Final report. https://www.health.org.uk/improvement-projects/quantifying-parental-concern-to-strengthen-their-voice (accessed 08/06/19).
•• Thomas-Jones E, Lloyd A, Roland D, et al. A prospective, mixed-methods, before and after study to identify the evidence base for the core components of an effective Paediatric Early Warning System and the development of an implementation package containing those core recommendations for use in the UK: paediatric early warning syste—utilisation and mortality avoidance—the PUMA study protocol. BMC Pediatrics. 2018;18:244. https://doi.org/10.1186/s12887-018-1210-z. An important ongoing study protocol examining a broad range of interventions to reduce inpatient deterioration.
Clarke GM, Conti S, Wolters AT. et al, Evaluating the impact of healthcare interventions using routine data. BMJ. 365:l2239.
Emanuel L, Berwick D, Conway J, et al. What exactly is patient safety? In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in patient safety: new directions and alternative approaches (vol. 1: assessment). Rockville (MD): Agency for Healthcare Research and Quality; 2008. Advances in Patient Safety.
• Braithwaite J, Wears RL, Hollnagel E. Resilient health care: turning patient safety on its head. Int J Qual Health Care. 2015;27(5):418–20. Paper introducing the key concepts of resilience in healthcare and Safety II, the ability to learn from understanding why work goes right.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
John Fitzsimons declares that he has no conflict of interest. Michaela Pentony declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Patient Safety
Rights and permissions
About this article
Cite this article
Fitzsimons, J., Pentony, M. Paediatric Early Warning Systems in 2019: What We Know and What We’ve Yet to Learn. Curr Treat Options Peds 5, 315–325 (2019). https://doi.org/10.1007/s40746-019-00176-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-019-00176-1